Abstract
The surgical management of post-traumatic thoracolumbar kyphosis remains controversial. The need for combined procedures is subject to debate, especially for post-traumatic kyphosis after simple type A fractures. The aim of this retrospective study was to evaluate radiographic findings, patient satisfaction and clinical outcome after mono-segmental surgical treatment using an anterior procedure alone (group 1, n=10 patients) and using a one-stage combined anterior and posterior procedure (group 2, n=15 patients) for post-traumatic thoracolumbar kyphosis after simple type A fractures. The main indication for surgery was pain. There were no statistically significant differences between the patients in the two groups concerning age, cause of injury, time interval between trauma and surgery, preoperative kyphosis and preoperative back pain score. For all these 25 patients, complete follow-up data were available for retrospective evaluation. The median follow-up was 17 years in group 1 and 8 years in group 2. Radiographic documentation and classification was made on the basis of standing antero-posterior and lateral views and computed tomographic scans. Fractures were categorized according to the Magerl classification. Kyphotic deformity was assessed on lateral radiographs using the Cobb method. Kyphosis angles were measured preoperatively, directly postoperatively, and at final follow-up. For clinical evaluation, the back pain scoring system of Greenough and Fraser was used. Patients were requested to score their status prior to trauma, preoperatively and at follow-up. The Wilcoxon test was used for statistical analysis (P<0.05 is significant). In all cases radiographic union was achieved. Median kyphosis in group 1 was corrected from 23° preoperatively to 12° postoperatively (P<0.01) and was 11° at follow-up. Median kyphosis in group 2 was corrected from 21° pre-operatively to 12° postoperatively (P<0.01) and was 12° at follow-up. The median back score in group 1 changed from 66 points before the trauma to 23 points (P<0.01) preoperatively and 35 points at follow-up (P<0.01). The median back score in group 2 changed from 67 points before the trauma to 20 points (P<0.01) preoperatively and 38 points at follow-up (P<0.01). In group 2, four patients had complaints due to annoying prominence of the dorsal instrumentation. In all these cases the dorsal instrumentation was removed. Statistical analysis in this series of ten patients with anterior spondylodesis compared with 15 patients with combined one-stage spondylodesis did not reveal objective advantages of the combined procedure as far as the outcome of radiographic correction of kyphosis or patient outcome is concerned. It is therefore concluded that in cases of post-traumatic thoracolumbar kyphosis after simple type A fractures, mono-segmental correction using an anterior procedure alone, with spondylodesis, is the surgical procedure of choice.
Keywords: Thoracolumbar, Post-traumatic, Anterior approach, Combined approach, Kyphosis, Clinical outcome
Introduction
Post-traumatic deformities can be observed in cases of conservative or inadequate surgical treatment of spinal injuries [2, 10, 21, 25, 26]. The Magerl et al. classification of thoracolumbar spinal injuries [18] recognizes three injury types. The classification reflects a progressive scale of morphological damage by which the degree of instability is determined. Only minor and functionally unimportant injuries with slight tissue destruction may heal without consequences. In more serious injuries, a secondary post-traumatic deformity may develop. Pain, progressive deformity, neurological damage or increasing neurological deficit and skin problems are the main indications for surgery.
Anterior, posterior, or combined anterior and posterior procedures have been advocated by different authors and show various degrees of success [1, 3, 7, 8, 10, 11, 12, 13, 14, 15, 16, 19, 20, 22, 24, 25,26]. On the basis of biomechanical considerations such as the load-sharing concept and tension-band principle, reconstruction of the anterior column with dorsal compression osteosynthesis instrumentation is the treatment of choice [10, 17, 25]. A combined approach in one stage has the preference in comparison with a staged procedure [23]. The need and indications for combined procedures, however, are still subject to debate, especially for post-traumatic thoracolumbar kyphosis after simple type A fractures. For all post-traumatic thoracolumbar kyphosis cases, surgical treatment by an anterior procedure alone was initially performed at our clinic. From 1988 onwards, mainly on the basis of biomechanical considerations [10, 17, 25], combined procedures were performed.
The aim of this retrospective study was to evaluate radiographic findings, patient satisfaction and clinical outcome after mono-segmental surgical treatment using an anterior procedure alone and using a one-stage combined anterior and posterior procedure for post-traumatic thoracolumbar kyphosis after simple type A fractures.
Materials and methods
Between January 1984 and May 1996, 25 consecutive patients were surgically treated for symptomatic post-traumatic thoracolumbar kyphosis after simple type A fractures. Fractures were categorized according to the Magerl classification [18]. We defined as simple type A fractures: impaction fractures (type A.1.1 fractures), wedge impaction fractures (type A.1.2 fractures) and incomplete burst fractures (type A.3.1 fractures) with no or minor narrowing (<10%) of the spinal canal. The deformation of the vertebral body in these fractures is due to compression of the cancellous bone rather than to fragmentation [18]. The posterior column is intact [18]. Narrowing of the spinal canal did not occur or was minor. There were no neurological injuries. For all these 25 consecutive patients, complete follow-up data were available for retrospective evaluation. The main indication for surgery in all 25 patients was pain that did not respond to conservative treatment. Either a mono-segmental anterior procedure alone (group 1, n=10 patients) or a combined mono-segmental anterior and posterior fusion (group 2, n=15 patients) without anterior or posterior decompression of the spinal canal was performed in these patients. Patients were excluded from the study if they had post-traumatic kyphosis due to vertebral body collapse (type A.1.3 fractures), split fractures (type A.2), burst-split fractures (type A.3.2), complete burst fractures (type A.3.3), type B injuries and type C injuries. Patients with a follow-up of less than 5 years and patients who needed multi-level anterior or posterior fusions with or without anterior and posterior decompression of the spinal canal were also excluded.
The aim of the operative treatment was complete correction of the post-traumatic spinal deformity and reduction of the associated back pain.
Surgical technique
The patients in group 1 were operated between January 1984 and September 1986. Anterior release, excision of the intervertebral disc, correction of the kyphosis and a mono-segmental stabilization was performed using an iliac crest bone graft and anterior osteosynthesis with the single-rod Slot-Zielke system (Fig. 1a,b). The patients in group 2 were operated between April 1988 and May 1996. A one-stage combined mono-segmental anterior stabilization with the Slot-Zielke system and posterior fusion with CD instrumentation (hook construction) was carried out in seven patients. In a further six patients, a one-stage combined mono-segmental anterior stabilization with the Slot-Zielke system and posterior fusion with the DKS system (pedicle-screw construction) was performed (Fig. 2a,b). The Miami-Moss system was used in two patients for anterior and posterior fusion (pedicle-screw construction). Pedicle-screw construction was the implant of choice [25]. A hook construction was used if there was a serious anterior bone loss of the damaged vertebra and solid fixation and placement of the pedicle screws could not be guaranteed. Postoperatively, all patients were mobilized in a light-weight brace for up to 3 months. The senior author (H.D.B.) operated all patients.
Fig. 1.
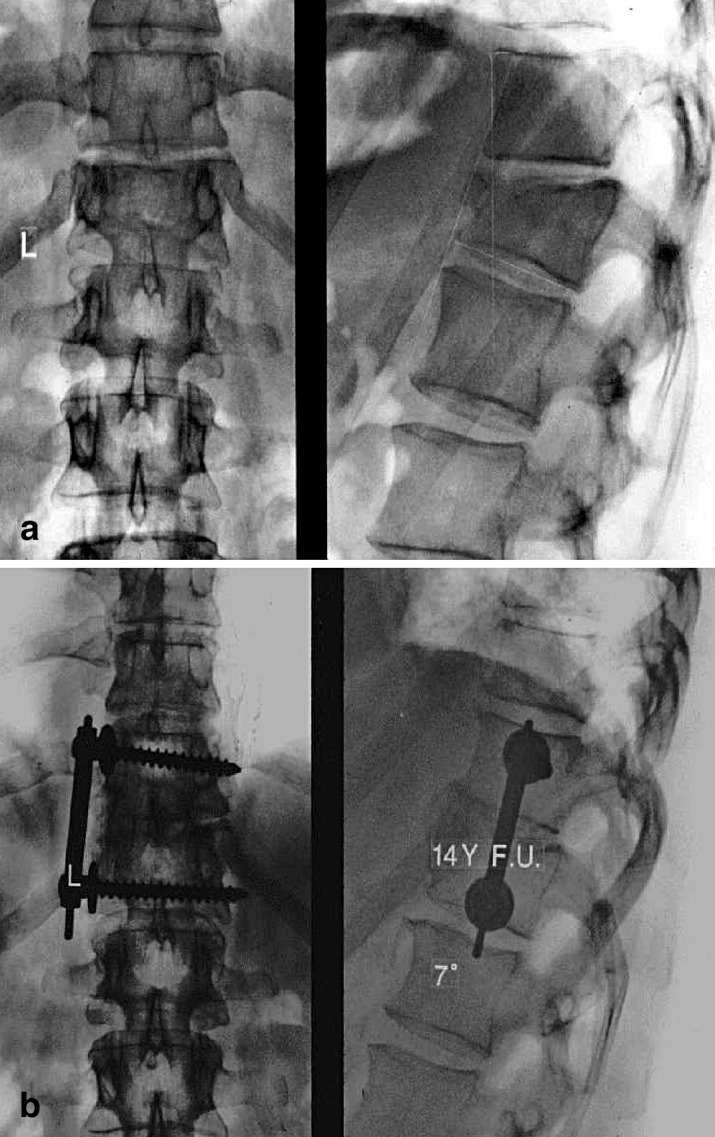
Example of a group 1 patient (mono-segmental anterior procedure alone). a Preoperative antero-posterior (AP) and lateral radiographs of a 37-year-old man with a post-traumatic kyphosis of 22° after a simple type A fracture of T12, with a Greenough and Fraser back pain score of 25 points. b The patient at 14 years follow-up after a mono-segmental anterior reconstruction and stabilization with a Slot-Zielke device. The kyphosis is now 7°, and the Greenough and Fraser score 38 points
Fig. 2.
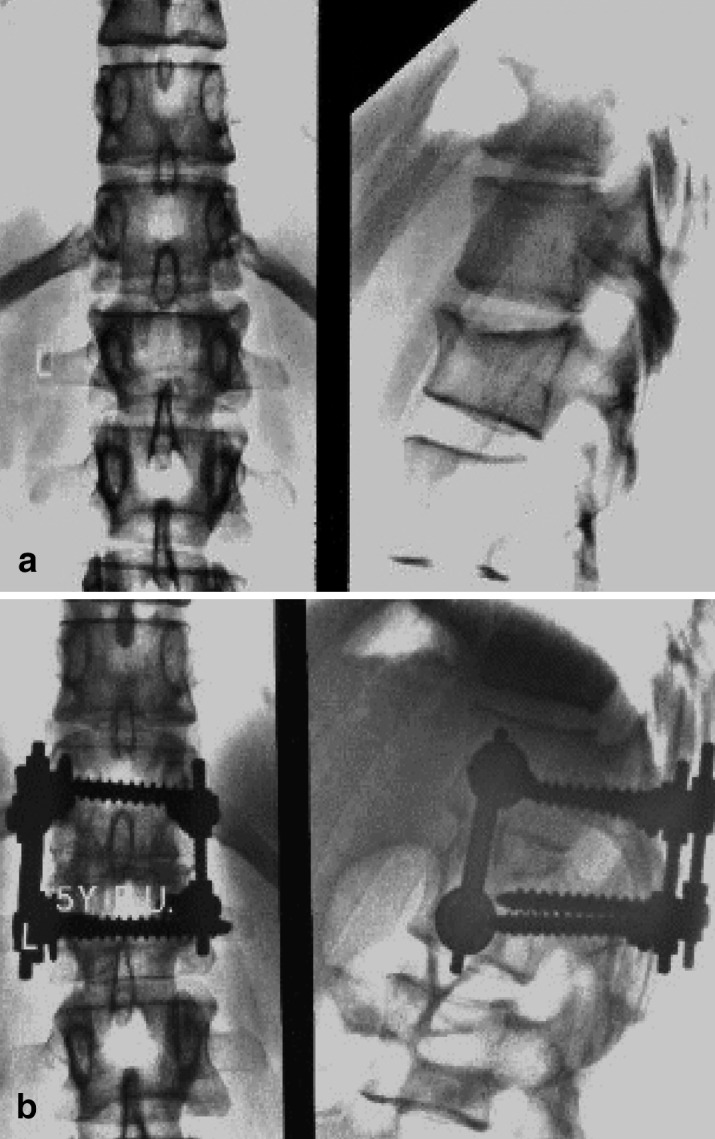
Example of a group 2 patient (mono-segmental combined one-stage anterior and posterior procedure). a Preoperative AP and lateral radiograph of a 27-year-old woman with a post-traumatic kyphosis of 17°, after a simple type A fracture of L1, with a Greenough and Fraser back pain score of 15 points. b The patient at 5 years follow-up after a combined mono-segmental anterior reconstruction and stabilization with Slot-Zielke device and posterior DKS system. Kyphosis is now 10° and the Greenough and Fraser back pain score 50 points
Radiological evaluation
Radiographic documentation and classification was made on the basis of standing anterior-posterior (AP) and lateral views, and computed tomographic (CT) scans. Magnetic resonance imaging was not carried out. The AP and lateral views and CT scans were also scored by an independent consultant radiologist. Fractures were categorized according to the Magerl classification [18]. Kyphotic deformity was assessed on lateral radiographs using the Cobb method. Kyphosis angles were measured preoperatively, directly postoperatively, and at final follow-up, between the superior endplate of the vertebra above the wedged vertebra and the inferior endplate of the vertebra below. All scoliotic angles were measured by the Cobb method on the AP preoperative, postoperative and follow-up radiographs.
The size of the spinal canal was determined by CT. The mid-sagittal diameters of the spinal canal at the injury level were compared with the average of the same diameter at one level proximal and one level distal to the injury, and expressed as a percentage of narrowing.
Patient outcome
Patients were requested to fill out a questionnaire including the back pain scoring system of Greenough and Fraser [9] to score their status prior to the trauma, preoperatively and at follow-up. The score is derived from 13 factors including pain, activities of daily living, employment, and sporting ability. The score ranges from 0 to 75 points and is classified as an excellent (>65 points), good (>50 points), fair (>30 points) or poor (<30 points) result. Retrospective evaluation has been shown by Fischer et al. to be a reliable tool for measuring patient outcome, even when used a long time after the treatment [6].
Statistical analysis
Kyphosis angles [4] and patient back pain scores [9] are reported as medians (5th–95th percentiles), and P-values were calculated using the Wilcoxon signed rank test. A P-value of <0.05 was considered significant.
Results
For all 25 patients, 11 women and 14 men, complete follow-up data were available for retrospective evaluation (Table 1). All individual patient data are listed in Table 2. The two groups were comparable with regard to age (36 vs 35 years), cause of injury, time interval between trauma and surgery (16 vs 18 months), preoperative kyphosis (23° vs 21°), and pre-injury back pain score (66 vs 67 points). The average follow-up was 17 years in group 1 and 8 years in group 2.
Table 1.
Comparison of patients and outcome in group1 (anterior) versus group 2 (anterior and posterior) stabilization. Values are presented as median (5–95%percentile) unless stated otherwise
| Group 1 | Group 2 | |
|---|---|---|
| No. of patients | 10 | 15 |
| Age (years) | 36 (26–45) | 35 (22–49) |
| Sex (n) | 8 male, 2 female | 5 male, 10 female |
| Interval trauma surgery (months) | 16 (10–27) | 18 (7–46) |
| Follow-up (years) | 17 (15–18) | 8 (6–12) |
| Fracture level (n) | ||
| Thoracic (T1-T10) | 3 | 2 |
| Thoracolumbar (T11-L1) | 5 | 11 |
| Lumbar (L2-L5) | 2 | 2 |
| Kyphosis | ||
| Preoperative | 23° (14°–42°) | 21° (10°–36°) |
| Postoperative | 12° (1°–38°) | 12° (0°–28°) |
| Follow-up | 11° (7°–41°) | 12° (2°–28°) |
| Back pain score a | ||
| Pre-injury | 66 (40–74) | 67 ( 41–75) |
| Preoperative | 23 (10–37) | 20 (5–39) |
| Follow-up | 35 (7–68) | 38 (21–60) |
a Back pain scored according to Greenough and Fraser [9]
Table 2.
Individual data of all patients in group 1 (anterior only) and group 2 (combined anterior and posterior)
| Patient No. | Age | Sex | Instrumentation | Interval from injury to surgery | Kyphosis | Follow-up | Fracture level | Patient scorea | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (years) | (months) | Preop | Postop | Follow-up | (months) | Pre-injury | Preoperative | At follow-up | ||||
| Group 1 | ||||||||||||
| 1 | 29 | M | Zielke | 31 | 20° | 2° | 9° | 209 | L2 | 69 | 31 | 10 |
| 2 | 36 | M | Zielke | 22 | 35° | 16° | 25° | 202 | L1 | 73 | 5 | 31 |
| 3 | 31 | M | Zielke | 10 | 35° | 30° | 34° | 206 | T7 | 69 | 27 | 67 |
| 4 | 23 | M | Zielke | 12 | 47° | 45° | 47° | 202 | T8 | 66 | 42 | 69 |
| 5 | 38 | F | Zielke | 17 | 16° | 1° | 11° | 196 | L1 | 33 | 19 | 2 |
| 6 | 37 | M | Zielke | 17 | 22° | 4° | 7° | 189 | T12 | 66 | 25 | 38 |
| 7 | 36 | M | Zielke | 11 | 35° | 20° | 11° | 184 | L1 | 57 | 21 | 24 |
| 8 | 50 | M | Zielke | 16 | 13° | 2° | 7° | 180 | L2 | 75 | 17 | 54 |
| 9 | 30 | M | Zielke | 12 | 24° | 13° | 16° | 200 | T11 | 59 | 25 | 63 |
| 10 | 37 | F | Zielke | 16 | 16° | 11° | 11° | 214 | T8 | 49 | 20 | 19 |
| Group 2 | ||||||||||||
| 1 | 18 | F | Zielke/CD | 18 | 20° | 7° | 14° | 140 | L1 | 73 | 39 | 66 |
| 2 | 24 | F | Zielke/CD | 14 | 5° | 2° | 5° | 144 | L2 | 75 | 24 | 58 |
| 3 | 41 | M | Zielke/CD | 66 | 35° | 32° | 36° | 124 | T8 | 73 | 40 | 41 |
| 4 | 31 | F | Zielke/CD | 14 | 31° | 22° | 25° | 164 | T12 | 69 | 9 | 45 |
| 5 | 48 | F | Zielke/CD | 10 | 22° | 15° | 18° | 123 | T12 | 75 | 9 | 30 |
| 6 | 27 | M | Zielke/CD | 27 | 38° | 26° | 22° | 112 | T6 | 62 | 25 | 44 |
| 7 | 50 | M | Zielke/DKS | 6 | 30° | 14° | 18° | 100 | T12 | 17 | 16 | 36 |
| 8 | 44 | M | Zielke/CD | 15 | 20° | 15° | 15° | 102 | L1 | 66 | 4 | 21 |
| 9 | 30 | F | Zielke/DKS | 8 | 34° | 12° | 12° | 100 | T11 | 67 | 9 | 26 |
| 10 | 32 | F | Miami/Miami | 28 | 21° | 11° | 8° | 80 | T12 | 75 | 5 | 21 |
| 11 | 27 | F | Zielke/DKS | 25 | 17° | 12° | 10° | 87 | L1 | 75 | 15 | 50 |
| 12 | 48 | F | Zielke/DKS | 38 | 14° | 10° | 10° | 80 | L1 | 60 | 35 | 23 |
| 13 | 35 | F | Zielke/DKS | 26 | 22° | 12° | 12° | 72 | T11 | 63 | 20 | 38 |
| 14 | 36 | M | Miami/Miami | 18 | 20° | 0° | 3° | 70 | L2 | 51 | 29 | 34 |
| 15 | 36 | F | Zielke/DKS | 14 | 12° | 0° | 0° | 73 | T12 | 61 | 21 | 53 |
a Greenough and Fraser back pain score [9]
Radiographic evaluation results
Median kyphosis in group 1 was corrected from 23° preoperatively (range 14°–42°) to 12° postoperatively (range 1°–38°) (P<0.01), and was 11° (range 7°–41°) at follow-up. Median kyphosis in group 2 was corrected from 21° preoperatively (range 10°–36°) to 12° (range 0°–28°) postoperatively (P<0.01), and was 12° (range 2°–28°) at follow-up (Table 1). In all cases, radiographic union was achieved.
In the AP views no scoliotic angles of more then 5° were measured on the preoperative, postoperative or follow-up AP radiographs.
Patient outcome results
The median back pain score in group 1 changed from 66 points (range 40–74 points) before the trauma to 23 points (range 10–37 points) preoperatively (P<0.01), and 35 points (range 7–68 points) at follow-up (P<0.01). Median back pain score in group 2 changed from 67 points (range 41–75 points) before the trauma to 20 points (range 5–39 points) preoperatively (P<0.01), and 38 points (range 21–60 points) at follow-up (P<0.01) (Table 1). The median hospital stay was 19 days in group 1 (range 13–21 days) and 15 days in group 2 (range 11–19 days). In both groups 80% of the patients reported that, considering the long-term results, they would agree to undergo the operation again.
Statistical analysis
Statistical analysis in this series of ten patients with anterior spondylodesis compared with 15 patients with combined one-stage spondylodesis did not reveal objective advantages of the combined procedure as far as the outcome of radiographic correction of kyphosis and patient outcome is concerned.
Complications
Only one serious early complication (pneumonia) occurred in group 1. There were no neurological complications. In group 2 four patients had complaints due to annoying prominence of the dorsal instrumentation. In all these cases the dorsal instrumentation was removed.
Discussion
The aim of this retrospective study was to evaluate radiographic findings, patient satisfaction and clinical outcome after surgical treatment with a mono-segmental anterior procedure alone and with a one-stage mono-segmental combined anterior and posterior procedure for post-traumatic thoracolumbar kyphosis after simple type A fractures.
Reproducibility of fracture classification systems in general has been a matter of controversy. Blauth et al. [5] reported an interobserver agreement of the Magerl classification to be 67% (41–91%). For the A type fractures the interobserver reliability was found to be over 90% [5]. Use of MRI and better definition of the distinctive properties of the three different types may enhance the reproducibility of the classification scheme [21]. Radiographic documentation and classification according to Magerl in this study was made on the basis of standing AP and lateral views and CT scans. MRI scans were not available at the time the first patients in this study were treated.
Post-traumatic deformities can be observed with both conservative and inadequate surgical treatment of spinal injuries. The deformity is often associated with pain. The pain may emanate from the site of the deformity itself, the injured disc level, a bony nonunion, or from the lordotic compensation above and below the deformity site, where added stresses are placed on the respective facet joints. In patients with associated neurological complications, post-traumatic tethered cord due to dural adhesions, myelo-degeneration and post-traumatic syringomyelia can cause severe pain [10]. Often the precise origin of pain is difficult to identify [26]. The kyphosis is often fixed and rigid, and correction is difficult. In the presence of healed and contracted anterior soft tissue, surgical correction by posterior spinal fusion alone is in most cases not sufficient for the angular post-traumatic kyphosis [25, 26]. Finally, the spinal cord cannot be adequately decompressed through the posterior approach because the offending compression is located anteriorly [25, 26], although decompression was not necessary in the present series. If surgery is restricted to an anterior approach, correction of a deformity is often hindered by posterior structures. After fractures and dislocations, there may be ankylosis or bony obstacles with the danger of cord impingement. In addition, the bending moment that remains after anterior correction may be one of the major causes of the failures that occur when ventral surgery is performed exclusively. The combination of circumspinal decompression and safe correction of the vertebral column in a single posterior approach was advocated by Heinig [11], who described a closing wedge osteotomy. This procedure was later modified by Gertzbein and Harris [8] for the correction of post-traumatic kyphosis. Heinig [11] performed his procedure in both neurologically intact individuals and patients with neurological deficits. However, Gertzbein and Harris [8] outlined their treatment algorithm only for, and limited their procedure to, patients without neurological deficits. They stated that an anterior procedure is warranted to ensure complete decompression in the patient with a progressive neurological deficit or a persistent incomplete neurological deficit in the presence of a kyphotic deformity. Gertzbein and Harris [8] limited their procedure to corrections of approximately 30°–40°. If the kyphosis is corrected by more than 40° in these closing wedge osteotomy procedures, the spinal cord may become too long for the shortened vertebral column and may be curved or even kinked and potentially damaged.
Kawahara et al. [14] described a technique of circumspinal decompression and correction osteotomy using a single posterior approach for the correction of angular kyphotic deformity. Anterior decompression of the spinal cord is possible by costotransversectomy. Patients with or without neurological deficits are included as suitable candidates for the procedure [14].
On the basis of biomechanical considerations such as the load sharing concept and tension band principle, reconstruction of the anterior column with dorsal compression osteosynthesis instrumentation is the treatment of choice [10, 17, 20, 25]. There is a consensus that both anterior and posterior factors should be managed for a sufficient restoration of alignment to obtain fusion in rigid kyphosis in various pathologic conditions [10, 17, 20, 25]. Because anterior and posterior spinal structures are involved, Harms and Stolze [10, 25] argued that the strategy of choice for the correction of rigid angular post-traumatic kyphosis is a dorso-ventro-dorsal procedure in order to achieve lasting correction and secure fusion. After a thorough circumferential release, the angular kyphosis can be easily corrected and permanently fixed.
The need and indications for combined procedures, however, are still subject to debate [12, 15, 16], especially for post-traumatic thoracolumbar kyphosis after simple type A fractures with mild kyphosis and no posterior ankylosis or bony obstacles. The initial trauma mechanism did not affect the posterior column. In our series, narrowing of the spinal canal did not occur or was minor. There were no neurological injuries, and it was not necessary to perform an anterior or posterior decompression of the spinal canal. In these patients, a posterior in situ fusion with instrumentation [8] can be considered, but because the injury is located primarily in the anterior and middle column, we preferred an anterior mono-segmental or a one-stage combined mono-segmental procedure.
Kostuik and Matsusaki [15, 16] have reported the successful results of anterior decompression and stabilization with the use of anterior instrumentation for post-traumatic kyphosis. Kaneda [12] reported that anterior decompression and fusion associated with anterior instrumentation is suitable for patients with low-grade post-traumatic kyphosis with neurological deficits. However, these studies [12, 15, 16] did not compare the results with the combined procedure and did not report a long-term follow-up.
Complete correction of the deformity, reaching the neutral position or a mild lordosis, was the goal of surgery. In neither group were we able to achieve this goal in the majority of the patients. In all cases radiographic union was achieved. In our opinion, the achievement of a solid fusion is of great importance for patient satisfaction. In this long-term follow-up study, kyphosis and back pain score at follow-up did not turn out to be better in the combined group.
Conclusion
In both groups, operative correction led to a long-lasting improvement in kyphosis and patient outcome, although the original pre-trauma level was not reached.
We may therefore conclude that in cases of post-traumatic thoracolumbar kyphosis after simple type A fractures, mono-segmental anterior correction alone, with spondylodesis, is the surgical procedure of choice.
References
- 1.AcarogluEur Spine J 19965568689418 [Google Scholar]
- 2.BeenSpine 199116702003240 [Google Scholar]
- 3.Been Acta Neurochir. 1999;141:349. doi: 10.1007/s007010050003. [DOI] [PubMed] [Google Scholar]
- 4.Bernhardt Spine. 1989;14:717. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Blauth Orthopade. 1999;28:662. doi: 10.1007/s001320050397. [DOI] [PubMed] [Google Scholar]
- 6.Fischer JAMA. 1999;282:1157. doi: 10.1001/jama.282.12.1157. [DOI] [PubMed] [Google Scholar]
- 7.Floman Clin Orthop. 1982;164:110. [PubMed] [Google Scholar]
- 8.Gertzbein Spine. 1992;17:374. doi: 10.1097/00007632-199203000-00025. [DOI] [PubMed] [Google Scholar]
- 9.GreenoughSpine 199217361531553 [Google Scholar]
- 10.HarmsEur Spine J 1992114220054929 [Google Scholar]
- 11.Heinig JA (1984) Egg shell procedure. In: Luque ER (ed) Segmental spinal instrumentations. Slack, Thorofare, pp 221–320
- 12.Kaneda K (1991) Anterior approach and Kaneda instrumentation for lesions of the thoracic and lumbar spine. In: Bridwell K, DeWald RL (eds) The textbook of spinal surgery. JB Lippincott, Philadelphia, pp 959–990
- 13.Kao-WhaSpine 19931819098235882 [Google Scholar]
- 14.Kawahara Spine. 2001;26:391. doi: 10.1097/00007632-200102150-00016. [DOI] [PubMed] [Google Scholar]
- 15.KostuikSpine 1990151692353252 [Google Scholar]
- 16.Kostuik Spine. 1989;14:379. doi: 10.1097/00007632-198904000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Lowery GL, Harms J (1997) Principles of load sharing. In: Bridwell KH, DeWald RL (eds) The textbook of spinal surgery, 2nd edn. Lippincott-Raven, Philadelphia, pp 155–165
- 18.Magerl Eur Spine J. 1994;3:184. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 19.Malcolm J Bone Joint Surg Am. 1981;63:891. [PubMed] [Google Scholar]
- 20.McAfee J Bone Joint Surg Am. 1985;67:89. [PubMed] [Google Scholar]
- 21.Oner Eur Spine J. 2002;3:235. doi: 10.1007/s00586-001-0364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberson Spine. 1985;10:307. doi: 10.1097/00007632-198505000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Shing-Sheng Spine. 1996;21:2260. doi: 10.1097/00007632-199610010-00016. [DOI] [PubMed] [Google Scholar]
- 24.Shufflebarger Spine. 1990;16:930. doi: 10.1097/00007632-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Stoltze Orthopade. 1999;28:731. doi: 10.1007/s001320050403. [DOI] [PubMed] [Google Scholar]
- 26.Vaccaro Spine. 2001;15:111. doi: 10.1097/00007632-200112151-00019. [DOI] [Google Scholar]


