Abstract
There are few articles in the literature concerning anterior instrumentation in the surgical management of spinal tuberculosis in the exudative stage. So we report here 23 cases of active thoracolumbar spinal tuberculosis treated by one-stage anterior interbody autografting and instrumentation to verify the importance of early reconstruction of spinal stability and to evaluate the results of one-stage interbody autografting and anterior instrumentation in the surgical management of the exudative stage of throracolumbar spinal tuberculosis. Twenty-three patients, including two children (9 and 15 years old, respectively) and 21 adults with thoracolumbar spinal tuberculosis were treated surgically. T9 to L4 spinal segments were affected, and MRI/CT showed evident collapse of the vertebrae because of tuberculous destruction and paravertebral abscess. Neurological deficits were found in 15 patients. Before surgery, patients received standard anti-tuberculosis chemotherapy for 2 to 3 weeks. Under general endotracheal anaesthesia, the patients were placed in right recumbent positions, and a transthoracic, lateral extracavitary or extrapleural approach was chosen according to the tuberculosis lesion segment. After exposure, the tuberculous lesion region, including the collapsed vertebrae and in-between intervertebral disc, was almost completely resected in order to release the segmental spinal cord. Then, autologous iliac, rib or fibular graft was harvested to complete interbody fusion, and an anterior titanium-alloy plate-screw system was used to reconstruct the stability of the affected segments. Anti-tuberculosis chemotherapy was continued for at least 9 months, and the patients were supported with thoracolumbosacral orthosis for 6 months after surgery. All patients were followed up for an average of 2 years. All 23 cases were healed without chronic sinus formation or any recurrence of tuberculosis during the follow-up period. Spinal fusion occurred at a mean of 3.8 months after surgery. Of all patients with neurological deficits, 14 patients showed obvious improvement; only one patient with Frankel C lesion remained unchanged, but none of the patients got worse. During the follow-up period, a mean of 18 degrees of kyphosis correction was achieved after surgery in the adult group. Moderate progressive kyphosis because of this procedure fusion occurred postoperatively in a 9-year-old child after 2 1/2 years; another 15-year-old child did not demonstrate this phenomenon. Except for the early loosening of one screw in two cases (which did not affect the reconstruction of spinal stability), no other complications associated with this procedure were found during follow-up. Early reconstruction of spinal stability plays an important role in the surgical management of spinal tuberculosis. One-stage anterior interbody autografting and instrumentation in the surgical management of the exudative stage of spinal tuberculosis show more advantages in selected patients, but supplementary posterior fusion should be considered to prevent postoperative kyphosis when this procedure is performed in children.
Keywords: Spinal tuberculosis, Anterior interbody fusion, Instrumentation, Spinal instability
Introduction
Tuberculosis continues to be the leading cause of death from infectious disease in the world, and it is causing more widespread concern than ever before [10]. The Fourth National Epidemiological Sampling Survey of Tuberculosis in China in 2000 showed that the prevalence of active pulmonary tuberculosis, smear positive pulmonary tuberculosis and bacteriological positive pulmonary tuberculosis is 367/100,000, 122/100,000 and 160/100,000, respectively [15]. Spinal tuberculosis, the most common pattern of extrapulmonary tuberculosis, also has increased rapidly around the world in recent years, especially in the undeveloped and developing countries [13]. The entire region of the human spine can be infected by Mycobaterium tuberculosis, occurring mostly in the thoracolumbar region. Patients with spinal tuberculosis often have evident collapse of vertebrae because of tuberculous destruction resulting in kyphosis and neurological deficits. It is beleived that aggressive surgical treatment should be adopted in the management of indicated patients with spinal tuberculosis [3]. But there is no consensus about one-stage anterior instrumentation, whether is should be applied or not. Recently, some authors have emphasized the importance of early reconstruction of spinal stability in the management of spinal tuberculosis, but there are only a few articles on this issue [9, 17]. We therefore report here a group of 23 cases with the exudative stage of thoracolumbar spinal tuberculosis treated by one-stage anterior interbody autografting and instrumentation. The aim of this clinical study is not only to verify the importance of early reconstruction of spinal stability, but also to evaluate the results of this method.
Materials and methods
General description
From March 1997 to February 2000, 23 patients (14 male, 9 female) received surgical treatment for thoracolumbar spinal tuberculosis at our department of Nanfang Hospital, Guangzhou, China. The patients included two children (9 and 15 years old, respectively) and 21 adults (range: 19 to 58 years, with an average of 40.8 years). The T9 to L4 vertebrae were affected in all patients of this group, an average of 2.5 vertebrae in each patient, who presented symptoms of back pain or low back pain, but only 11 of them had mild to moderate tuberculous toxic reaction. The duration of symptoms before surgery was 3 months to 1 year. MRI/CT showed all patients had evident collapse of the vertebral body, compression of the spinal cord and paravertebral abscess. These image demonstrations matched the conditions for selection of the anterior procedure. The Cobb’s angle of kyphosis before the operation was 28°±14° in the adult group. In a 9-year-old child with T12-L2 tuberculosis, severe kyhosis (48°), compression of the spinal cord and huge psao abscess formation were noted (Fig. 1), and another 15-year-old patient did not develop obvious kyphosis. The neurological examination according to the Frankel classification showed the Frankel B lesion in 2, C in 5, D in 8 and E in 8 patients.
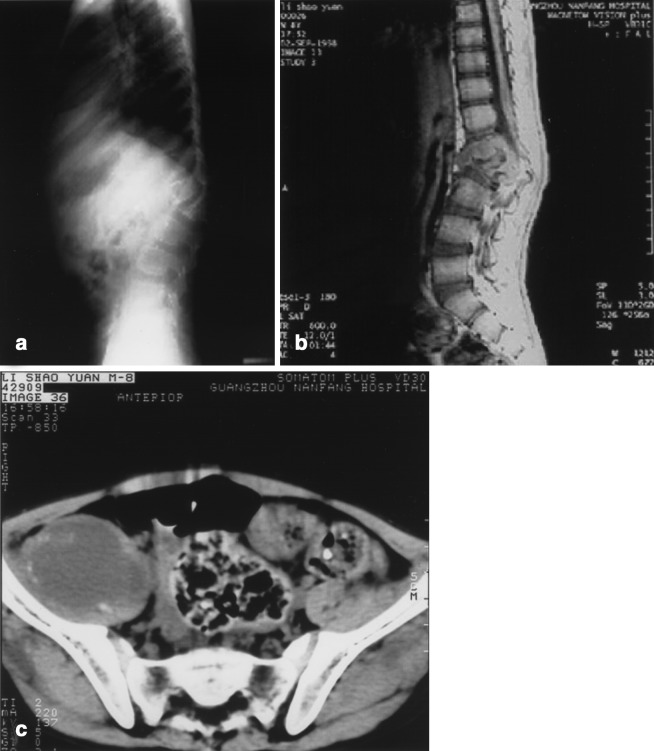
Fig. 1.
T11-L1 tuberculosis in a 9-year-old patient. A Lateral X-ray film shows severe kyphosis (48°) resulting from tuberculous destruction of the affected spine. B Sagittal MRI demonstrates compression of the spinal cord in this child with Frankel C neurological deficit. C Huge abscess of the right psao is confirmed by CT scanning
Preoperative preparation
All patients received routine chest X-rays and sputum examinations for the tubercle bacillus, but all were found to be without open tuberculosis or acute miliary pulmonary tuberculosis. All patients received standard anti-tuberculous chemotherapy by oral administration of isoniazid (300 mg per day), rifampin (450 mg per day) and/or ethambutol (1,200 mg per day), and intramuscular streptomycin (0.75 g per day for adults and 0.5 g for children) for 2 to 3 weeks before surgery.
Surgical procedure
The surgery was performed under general endotracheal anaesthesia, with the retropleural or transthorac approach used for the thoracic region and the retroperitoneal approach for the thoracolumbar and lumbar region. Normally, the approach was from the severely damaged side of the spine. If the patient had bilateral psoas abscess, sample drainage of the abscess was performed on the other side. After exposure, segmental vessels were carefully ligated. If the paravertebral abscess was so large that drainage from a stab incision was necessary to help judge the margin of the lesion foci, then the discs above and below the affected vertebral bodies were identified and resected with curettes, rongeurs and a high-speed air drill down to bleeding normal bone. This excision extended cranially and caudally until healthy bleeding cancellous bone was exposed to the dura mater. Slots were made in healthy bleeding bone of the vertebral bodies above and/or below the affected ones. After radical resection of the involved spine, distraction was carried out in between adjacent normal vertebrae to correct the prior kyphosis, and the spinal defect was measured. The resultant gap was repaired with suitable-length bone grafts using the technique of Hodgson and Stock [7]. Bone grafts were harvested from the iliac crest, rib or fibula in this procedure, and fibular grafts were often indicated in child patients. After interbody autografting, an anterior spinal Z-plate(Sofamor-Danek Co.) system or K-plate system (STABLE Surgical Implant Co., Ltd., Guangdong, China) was used to span the healthy vertebral body above and below the defect. After careful hemostasis, a quantity of normal saline was used for space irrigation to eliminate residual tuberculous tissue. Then, 3 to 4 g of streptomycin was put in the operated area, and a local drainage tube was inserted routinely before the incision was closed. If a transthoracic approach was adopted or pleura were torn open during the procedure, closed drainage of the pleural cavity should be made.
Postoperative treatment
In the 1st week after surgery, the patients were regularly examined for physical status, drainage characteristics and operation-related complications. If no complication of bleeding persisted, the drainage tube was pull out after 72 h, and preventive antibiotics for control of mixed infections were administered as soon as the surgery was completed. At the 1st week after surgery, isoniazid was administered intravenously to minimize the dissemination of tuberculosis. This standard anti-tuberculosis chemotherapy lasted for at least 9 months after surgery. The patients were instructed to notice any adverse reaction of antituberculous agents. One or two weeks after surgery, the patient could sit on the bed or walk around under the effective support of thoracolumbosacral orthosis, and this orthsis support was maintained for 6 months. All patients were X-rayed and the erythrocyte sedimentation rate, hepatic function, etc., were examined at 1-month intervals. They were followed up for 1 to 4 years (average 2 years).
Results
Autogenous fibular graft was used in a 9-year-old patient (Fig. 2), iliac graft in 18 patients, and rib graft in 4 (including another 15-year-old patient). All 23 patients healed without chronic sinus formation or any recurrence of tuberculosis. Spinal fusion at the interface that showed in radiological films occurred at a mean of 3.8 months after surgery (Fig. 3). Of the patients with neurological deficit, 14 improved to Frankel E, and only one case with Frankel C remained unchanged. In the adult group of 21 cases, a mean of 18 degrees of kyphosis correction was achieved, and most of patients (17) resumed their original work during follow-up. As for the 9-year-old patient, who recovered very soon and returned to primary school 10 months after surgery, postoperative MRI scanning showed excellent decompression of the spinal cord and correction of kyphosis after the procedure(Fig. 4). One and half years after the procedure, this child underwent a second operation to remove anterior implants because one screw loosened (Fig. 5). Moderate kyphosis was found 2 1/2 years after the primary operation (Fig. 6). But for another 15-year-old patient, no progressive kyphois due to solid anterior fusion was noted. Except for the early loosening of one screw of the Z-plate fixation system in two cases (which did not affect the reconstruction of spinal stability), no other complications associated with this procedure were found in any of the other cases.
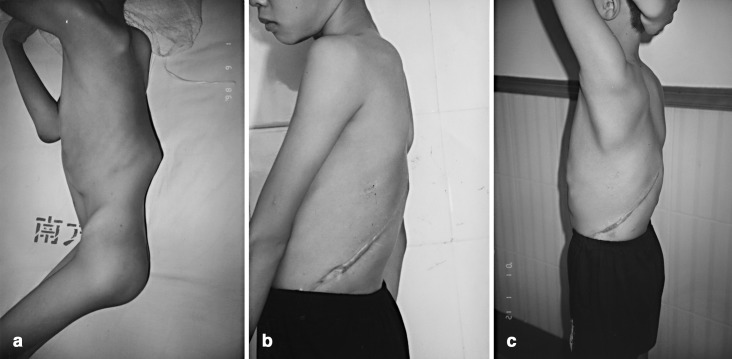
Fig. 2.
Autogenous fibular graft was used in this child patient for interbody fusion. The X-ray shows primary repair of the fibular defect with demineralized allogenous bone matrix at 1 month after surgery (A) and excellent remodeling 10 months later (B)
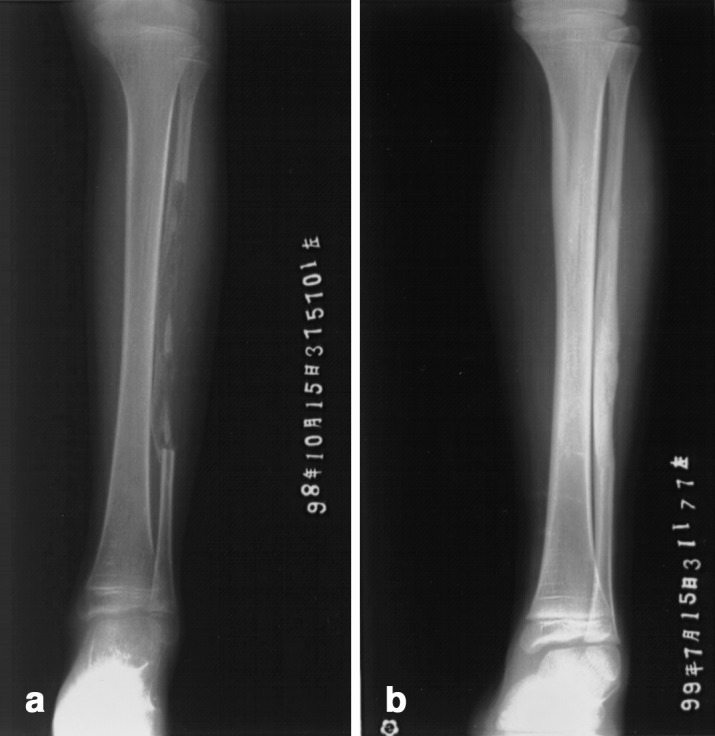
Fig. 3.
L3–4 tuberculosis in a 56-year-old patient (A). Bilateral psao abscesses are seen in CT scanning (B). The patient received one-stage anterior resection, interbody autografting with iliac crest and Z-plate instrumentation. X-ray taken 4 months later shows bone fusion at the interface (C)
Fig. 4.

MRI shows satisfactory release of the spinal cord and correction of kyphosis after operation in the child patient described in Fig. 1
Fig. 5.
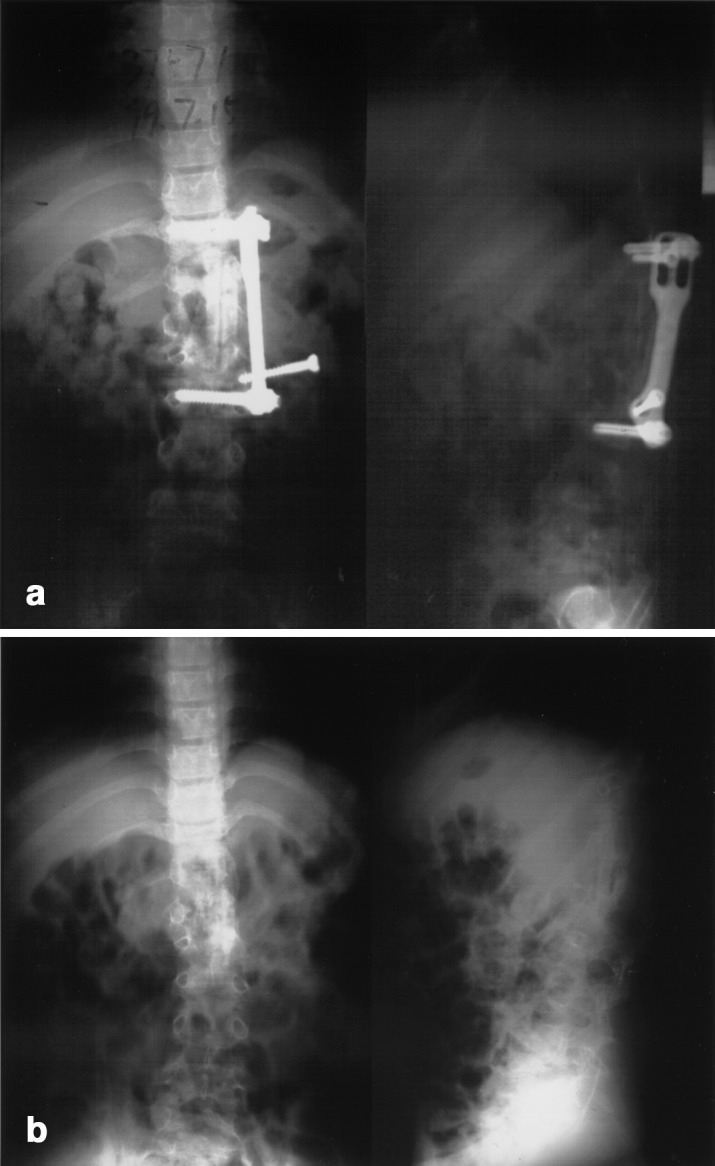
The child patient described in Fig. 1 underwent surgery a second time 1 1/2 years after the initial operation to remove the anterior implant because one screw loosened (A). Kyphosis is not evident at the time after the second operation (B)
Fig. 6.
Photographs of the child patient described in Fig. 1 show severe kyphosis before the initial operation (A), less evident kyphosis before the second operation (B) and moderate progressive kyphosis developed 2 years after the second operation (C)
Discussion
Due to classic description of spinal tuberculosis by Pervical Pott in 1779, it is generally accepted that spinal tuberculosis is the most dangerous pattern of bone and joint tuberculosis because of its ability to cause bone destruction, deformity and paraplegia. Tuberculosis of the spine is an unstable lesion that tends to progress at least until there is sound bony fusion. Bone fusion of the vertebrae is thought to be the most reliable evidence of healing of spinal tuberculosis [3]. To achieve this aim, many treatment methods have been developed, chemotherapy alone and chemotherapy combined with surgical management.
Tuberculosis is a generalized disease entity, and chemotherapeutic agents remain the cornerstone of treatment for spinal tuberculosis. A study in Korea by the Medical Research Council Working Party found that chemotherapy alone is efficacious for spinal tuberculosis, even when myelopathy or obvious bone destruction is present [11]. They reported that good clinical recovery was attained in 92% of patients and that complete or partial fusion with a mean increase of kyphosis of less than 18° by 36 months was obtained in 84% of patients. But many authors recommend that the treatment of spinal tuberculosis should be decided individually for each patient on the basis of the extent of the disease [17]. For severe spinal tuberculosis, the collapse of many vertebrae resulting in spinal instability can undoubtedly increase kyphosis formation and prolong the conservative treatment period and bed-rest time if chemotherapy is adopted alone. Moreover, the adverse effects of antituberculous chemotherapeutic agents cannot be underestimated. Altman et al. [1] reported that complications secondary to chronic chemotherapy occurred in two of their six patients who were children, one developing permanent deafness from treatment with intramuscularly administered streptomycin and another requiring a liver transplant for hepatoxicity because of long-term isoniazid therapy.
Although chemotherapy is the mainstay in the management of spinal tuberculosis, surgical procedures are still important. Until now, debridement of tuberculous foci or drainage of the cold abscess alone has proved to be unreliable, not offering enough stability of the spine and not having a long-term advantage over ambulant chemotherapy alone [3]. Anterior radical surgery with chemotherapy has been advocated as the treatment of choice [7], but the patient has to remain immobilized with a body cast or to stay in bed for a prolonged period of time. This immobilization cannot absolutely eradicate the motion of the local infected region, especially in young patients who need a lot of daily nursing care. And it will introduce unnecessary morbidity, especially in severely infected cases or in patients with poor compliance with the medication. There are still some complications with this surgical treatment, such as kyphotic deformity progression and graft failure [2, 8]. It is agreed that the insertion of strut grafts in the space after debridement of the affected vertebral bodies provides insufficient support anteriorly [4, 12]. So in the literature a few authors have introduced single stage or double stage posterior instrumentations, such as the Harrington rod or pedicle screw system, to reconstruct spinal stability and to prevent these complications. The clinical results are certainly preferred, strongly supporting that reconstruction of spinal stability is very important in the management of spinal tuberculosis in selected cases [5, 9, 14].
In our series, we report 23 cases with thoracolumbar spinal tuberculosis in the exudative stage treated by one-stage anterior interbody autografting and instrumentation. Some authors expressed their concerns about the risk of introducing a foreign body in infectious diseases. According to Oga et al. [16], both clinical and microbiological results suggest that there were no cases of persistence or recurrence of infection after posterior instrumentation surgery, and there was little Mycobacterium tuberculosis adherent to the stainless steel and only a little adherent biofilm observed. Yilmaz et al. [17] reported that 22 patients who had tuberculosis of the spine with moderate-to-severe localized kyphosis and 16 patients who had more than two involved levels had stabilization with anterior instrumentation. They found that there was no recurrence of spinal tuberculosis during an average of 2 years and 5 months of follow-up. In their report, 22 patients who had involvement of one or two levels had an average correction of the deformity of 64 percent, and 16 patients who had more than two levels of involvement had an average correction of 81 percent. But only 8 of 22 patients in their report were diagnosed as having active spinal tuberculosis. In our group, all patients had evident paravertebral abscess and erosion of spinal vertebrae, which indicated they were all at the exudative stage of spinal tuberculosis. Even for the relatively short follow-up period (range 1–4 years) in our clinical study, the results are encouraging. All patients healed without chronic sinus formation or recurrence. It also indicates that anterior instrumentation is safer and more effective in the management of exudative thoracolumbar spinal tuberculosis with regard to the quality of life, kyphosis correction and bone fusion. It can be concluded from our study and other reports that early reconstruction of spinal stability plays an important role in the treatment of active spinal tuberculosis [4, 14, 17].
In our experience, one-stage anterior resection, interbody autografting and instrumentation in the surgical treatment of selected patients with thoracolumbar spinal tuberculosis are advantageous in several aspects. This procedure can allow direct exposure of the pathological site of spinal tuberculosis in most cases and permits effective resection of almost all damaged vertebrae, involving disc tissues and tuberculous granuloma. “Resection” instead of “radical resection” is used in this procedure because it is very difficult to achieve the goal of radical surgery in treatment of spinal surgery. We believe that almost complete resection of pathological structures can effectively release the spinal cord at the involving level and to some extent decrease the quantity of chemotherapeutic agents and the duration of chemotherapy. Under effective strut autografting with iliac crest, fibular or rib bone, partial to complete correction of kyphosis can be obtained in the exudative stage of spinal tuberculosis. Undoubtedly, early anterior instrumentation can directly provide stability for the involving spinal segments, which would prevent strut graft slippage or failure and create a favorable environment for bony fusion. Postoperatively, the patient can resume daily activity without limitation under thoracolumbosacral orthosis. Compared to the two-stage surgery, a single stage surgery can shorten the treatment period, improve the quality of life and is more cost-effective. Finally, we prefer the titanium fixation system, which we adopted in this group, considering that instrumentation of the titanium system can allow the patient to undergo MRI and CT examinations postoperatively. In our experience, MRI is a very useful means to observe any recurrence, healing or bony fusion of spinal tuberculosis for postoperative follow-up.
We agree with Yilmaz et al. [17] that the treatment decision should be made individually. The indications for anterior radical surgery of spinal tuberculosis (Hong Kong procedure) is commented on in many articles [3, 7, 8, 17]. The procedure described is indicated in patients who need anterior radical surgery, direct decompression of the spinal cord and early reconstruction of spinal stability. Some authors believe that anterior instrumentation should be used only in patients involving more than two levels, but we believe that interbody fusion plus anterior instrumentation has an advantage over strut graft insertion alone. In any event, it should be kept in mind that the use of anterior instrumentation alone is possible only if the posterior elements are intact.
Just as Fountain et al. [5] reported, progressive kyphosis occurred in children with spinal tubersulosis after solid anterior fusion. We also observed this phenomenon in a 9-year-old child. Besides overgrowth of the posterior elements in fused segments, early removal of anterior instrumentation could not be excluded as a cause because to some extent effective anterior instrumentation can help balance overgrowth of the posterior elements biomechanically. We did not find evident progressive kyphosis in this child during 1 1/2 years of follow-up before removal of the instrumentation. But this suggests that supplemental posterior fusion should be recommended sooner or later for a biomechanical balance between anterior and posterior spinal elements if the procedure described is used in children.
The timing of this procedure is another issue. In our experience, this procedure can be performed when the patient’s general condition has improved and the erythrocyte sedimentation rate (ESR) shows a decreasing trend. Giving the patient standard anti-tuberculosis chemotherapy for 2 to 3 weeks before surgery is a routine treatment. In case of a large paravertebral abscess, it is difficult to get ESR to a normal range. If lacking effective blood concentration monitoring of chemotherapeutic agents, the trend of ESR to continue to drop is a useful marker for specifying the timing of surgery.
Conclusions
In summary, our results confirm that one-stage anterior interbody autografting and instrumentation show more advantages in selected patients because they can provide sufficient segmental stability of the affected spine, good correction of kyphotic deformity and promotion of bony fusion. Combined with standard chemotherapy, early reconstruction of spinal stability plays an important role in surgical management of spinal tuberculosis. Regular chemotherapy and spinal stability maintenance are the prime strategy for treatment of any spinal tuberculosis, and they cannot be separated from each other. Another posterior fusion should be supplemented in children with severe spinal tuberculosis to prevent progressive kyphosis following this procedure. Although the preliminary result is encouraging, we plan long-term follow-up for this procedure to further assess its application in the treatment of spinal tuberculosis.
Footnotes
This article was presented at the Conference of Eurospine 2001, Gothenburg, Sweden.
References
- 1.Altman Clin. 1996;Orthop:225. doi: 10.1097/00003086-199604000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Bailey J Bone Joint Surg Am. 1972;54A:1633. [PubMed] [Google Scholar]
- 3.Boachie-Adjei Orthop Clin North Am. 1996;27:95. [PubMed] [Google Scholar]
- 4.Faraj J Bone Joint Surg Am. 2001;83A:463. doi: 10.2106/00004623-200103000-00027. [DOI] [PubMed] [Google Scholar]
- 5.Fountain J Bone Joint Surg Am. 1975;57A:1104. [PubMed] [Google Scholar]
- 6.Guven Spine. 1994;19:1039. doi: 10.1097/00007632-199405000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Hodgson J Bone Joint Surg Am. 1960;42:295. [Google Scholar]
- 8.Kemp J Bone Joint Surg Br. 1973;55:715. [PubMed] [Google Scholar]
- 9.LeeJ Neurosurg 19999116310505499 [Google Scholar]
- 10.Mankin Curr Opin Orthop. 2001;12:489. doi: 10.1097/00001433-200112000-00010. [DOI] [Google Scholar]
- 11.Medical J Bone Joint Surg Br. 1973;55:678. [PubMed] [Google Scholar]
- 12.MedicalBr J Surg 1974618534611574 [Google Scholar]
- 13.Moon Spine. 1977;22:1791. doi: 10.1097/00007632-199708010-00022. [DOI] [PubMed] [Google Scholar]
- 14.Moon Spine. 1995;20:1910. doi: 10.1097/00007632-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 15.National Chin J Tuberculos Respir Dis. 2002;25:3. [Google Scholar]
- 16.Oga Spine. 1993;18:1890. doi: 10.1097/00007632-199310000-00028. [DOI] [PubMed] [Google Scholar]
- 17.Yilmaz J Bone Joint. 1997;Surg:1261. [Google Scholar]