Abstract
The purpose of the study was to compare conventional versus minimally invasive extraperitoneal approach for anterior lumbar interbody fusion (ALIF). Fifty-six consecutive patients with spondylolisthesis, lumbar instability, or failed back syndrome were treated with ALIF between 1991 and 2001. The patients were retrospectively evaluated and divided in two groups: Group 1, consisting 33 patients, was treated with ALIF using the conventional retroperitoneal approach, and Group 2, consisting of 23 patients, was operated with the minimally invasive muscle-splitting approach for ALIF. The groups were comparable as regards age, indication of fusion, and diagnosis. All patients in both groups had fusion with autologous iliac crest grafts and posterior instrumentation with posterolateral fusion in the same sitting. Clinical evaluation was done by two questionnaires: the North American Spine Society (NASS) Lumbar Spine Outcome Assessment Instrument and the Nottingham Health Profile (NHP). Fusion rate was evaluated radiologically. Mean clinical follow-up was 5.5 years. There was no statistical difference in the occurrence of complications with both approaches nor with the fusion rates of 92% in group 1 and 84% in group 2 respectively. The minimally invasive extraperitoneal approach for ALIF was associated with significantly less intraoperative blood loss, operation time, and length of the skin incision. In addition, this approach showed significant improvement in postoperative back pain in comparison to the conventional approach for ALIF.
Keywords: ALIF, Conventional, Minimally invasive, Lumbar spine
Introduction
Anterior lumbar interbody fusion (ALIF) was originally described for surgical management of Pott’s disease of the spine [1]. In 1932, Capener described the first ALIF for treating spondylolisthesis [4]. Since then, ALIF has evolved into an effective surgical treatment option for a variety of lumbar degenerative disorders, including degenerative disc disease, low-grade spondylolisthesis, and posterior pseudoarthrosis. Today, segmental fusions along with intervertebral disc removal account for the majority of spine surgeries [2].
In 1960, Harmon described a left extraperitoneal approach to the lumbar spine [15]. This was met by initial criticism from Stauffer and Coventry who condemned this approach, as it involved “too much surgical trauma to the patient” [36]. However, subsequent reports established growing popularity of the extraperitoneal approach with satisfactory results [12, 37]. Fraser et al. described a wide, muscle-splitting extraperitoneal approach to the lumber spine [11]. This was improved upon by Mayer in 1996 by using a smaller incision combined with a muscle-splitting exposure [24]. Zucherman in 1995 presented the first report using the laparoscopic approach in the ALIF [40]. Thus, with increasing popularity of ALIF, minimally invasive techniques were developed with the aim of decreasing postoperative morbidity, reducing hospitalization time, and shortening rehabilitation time.
Several reports in the literature document the advantages of ALIF in combination with posterior instrumentation for the management of spondylolisthesis, lumbar degenerative disc disease with instability, and failed back surgery syndrome (FBSS) [3, 7, 11, 19, 26, 28]. Available approaches for ALIF are the conventional extraperitoneal approach [15], the minimally invasive extraperitoneal approach [24], and the laparoscopic-assisted ALIF [40]. The surgical approach used should be designed to obtain the best spinal fusion. For this reason, it is important to have comparative studies so that the treating surgeon, knowing the advantages and risk factors, can select the optimal surgical approach. A comparison of mini-open laparotomy with laparoscopic ALIF has been presented in several reports [32, 39]; however we could find no report in the literature where outcomes of ALIF using the conventional and minimally invasive extraperitoneal approaches are compared.
From 1991 to 1996, ALIF was performed at our center using the conventional extraperitoneal approach described by Harmon [15]. From 1996 to date, we have been using the minimally invasive extraperitoneal approach for lumbar spine fusion [24]. In this report, we present a retrospective comparative study in ALIF procedures using either the conventional or a minimally invasive muscle-splitting retroperitoneal approach. Data regarding operative parameters, length of hospital stay, surgical-approach-associated complications, radiological parameters, and clinical outcome parameters in two comparable patient groups treated by the same surgical team are presented.
Methods
Patient selection and definition of groups
Fifty-six consecutive patients, who had been treated with an anterior lumbar interbody fusion over a 10-year period from January 1991 to January 2001 at the Department of Orthopaedic Surgery, University of Innsbruck, were evaluated in this retrospective study. All patients included in the study had single- or two-level ALIF using autologous iliac crest dowel grafts. Furthermore, every patient had a posterolateral fusion and a dorsal stabilization with instrumentation (Moss-Miami/CD instrumentation). Indications for surgery were spondylolisthesis, symptomatic instability in degenerative disc disease, or FBSS. FBSS was defined when at least one of the following criteria is observed: (a) equal or more pain after surgery; (b) unsuccessful surgery or no postoperative improvement; and (c) decreased ability to work postoperatively [34]. The FBSS patients in this collective had undergone previous laminectomy/hemilaminectomy, discectomies, or attempted lumbar fusions (either anteroposterior fusion or just posterior fusion). Patients were divided into two groups according to the type of surgical approach for ALIF:
Group 1 consisted of 33 patients treated with ALIF using the conventional retroperitoneal approach as described by Harmon [15]. The mean age at operation was 49.4 (range 32–63) years. The diagnoses were spondylolisthesis (17), degenerative disc disease with instability (three), and FBSS (13). Twenty-eight patients underwent a single-level fusion (21 at L4–5; four at L3–4, and three at L2–3), and five underwent two-level fusions (three at L3–5 and two at L1–3). CD-instrumentation was used for posterior stabilization in 23 patients and Moss-Miami instrumentation in 10 patients.
Group 2 consisted of 23 patients treated with a minimally invasive muscle-splitting approach as described by Mayer [24]. The mean age at operation was 51.7 (range 33–67) years. Diagnoses were spondylolisthesis (11), degenerative disc disease with instability (five) and FBSS (seven). In 21 cases, single-level fusion (17 at L4–5, three at L3–4, and one at L2–3), and in two cases, two-level fusion (L3–5) was performed. As posterior implants, the CD instrumentation was used in 19 patients and Moss-Miami instrumentation in four patients.
Surgical approaches
Conventional extraperitoneal approach as described by Harmon
The center of the disc space to be fused is marked on the skin under fluoroscopic control in the left lateral abdominal region. The skin incision is centered above this projection in an oblique direction parallel to the fibers of the external oblique abdominal muscle. The retroperitoneal space is accessed by splitting the external oblique abdominal muscle in the direction of its fiber orientation and cauterizing the internal oblique and transverse abdominal muscles across the direction of their fiber orientation. Under blunt dissection of the retroperitoneal space, the lumbar spine is exposed. Care is taken to preserve the common iliac vessels. For a safe left-to-right retraction, the ligation of segmental vessels is occasionally necessary. After verifying the correct disc space level under fluoroscopic control, the disc is removed and the bone dowels are inserted [15]. At our institute, autologous iliac crest bone grafts are harvested prior to preparing the retroperitoneal approach through the same skin incision.
Minimally invasive approach as described by Mayer
The skin incision is made after marking the disc space in the left lateral abdominal region and is followed by retrieving the autologous iliac crest dowels through the same opening. The retroperitoneal space is accessed by a blunt, muscle-splitting approach. Each muscular layer, the external oblique, the internal oblique, and the transverse abdominal muscle, is dissected in the direction of its fibers. The retroperitoneal dissection and the exposure and fusion of the lumbar spine are performed as described for the conventional approach. We have not used a self-retaining retractor frame to expand the surgical window as proposed by Mayer [24].
Patient Evaluation
Operative and radiological parameters
Data showing surgical time, blood loss, skin incision length, and complications were collected. The radiographic fusion rate was assessed by using anteroposterior and lateral plain radiographs. The radiographs were observed for trabecular bridging across the bone graft, radiolucent areas between the implant and the vertebral body, migration of the implant, signs of inflammatory reaction or resorption of the bone graft, and development of pseudoarthrosis.
Clinical parameters
To evaluate clinical outcomes, patients received two questionnaires, the North American Spine Society (NASS) Lumbar Spine Outcome Assessment Instrument, and the Nottingham Health Profile (NHP):
The NASS Lumbar Spine Outcome Assessment Instrument: This is a disease-specific questionnaire and is applied to determine the health status of patients with chronic back pain [8]. The translation and validation of a German version of the NASS questionnaire was published in 1999 [28]. The German NASS questionnaire contains 17 items for patients with lumbar spine disorders. Two questions concern back pain directly, nine deal with pain-related disability, and six concern neurogenic symptoms. The 17 NASS items are split into two scales, the pain and disability scale and the neurogenic symptoms scale. Each question was scaled 1 (not at all) to 6 (extremely).
NHP: The NHP was developed in the -late 1970s in Great Britain. It is an instrument for self-assessment of health-related quality of life [16]. Since the mid-1980s, the use of this instrument has also increased in other countries, and in 1992 an authorized German translation was published [19]. The NHP is made up of 38 yes-or-no-type questions that cover six dimensions of subjective health. The subscales are energy, pain, emotional reaction, sleep, social isolation, and physical mobility. The results of each subscale are standardized from 0 to 100, with high scores indicating reduction in quality of life.
Statistical analysis
Statistical analysis and evaluation of operative and radiological parameters and clinical questionnaires were performed. The differences observed between the two groups were analyzed using the chi-square test and the Mann-Whitney U test. Probability values of less than 0.05 were considered statistically significant.
Results
The mean length of the postoperative clinical follow-up period was 5.5 (range 1.5–11) years.
Operative and radiological parameters
Surgical time, intraoperative blood loss, and skin incision length are summarized in Table 1. We found that group 2 showed significantly better results concerning surgical time, blood loss, and incision length. In group 1, plain radiographs were available for review in all 33 cases involving 38 levels. In group 2, one patient had to be excluded because no radiographs were available. Therefore, 22 cases involving 24 levels were evaluated in this group. Plain radiographs were taken in a postoperative period from 6 to 96 (mean 26) months. In group 1, we found a fusion rate of 92% compared to 84% in group 2 (p=0.288). A radiographic fusion could be diagnosed after 8 (range 6–12) months. In group 1, pseudoarthrosis developed in two single-level fusion patients (one each at L3–4 and L4–5) and in one double-level fusion patient (L3–5). In group 2, pseudoarthrosis developed in four patients with single-level fusion (two at L4–5, one at L3–4, and one at L2–3).
Table 1.
Comparison of surgical time, blood loss, and skin incision length
| Group 1 (n=33) conventional approach |
Group 2 (n=23) minimal-invasive |
p value | |
| Surgical time (min) | 126.0 (range 79–190) | 100.5 (range 47–150) | 0.012 |
| Blood loss (ml) | 600.0 (range 300–2000) | 260.0 (range 100–800) | <0.001 |
| Skin incision length (cm) | 31.6 (range 15–50) | 12.0 (range 7–24) | <0.001 |
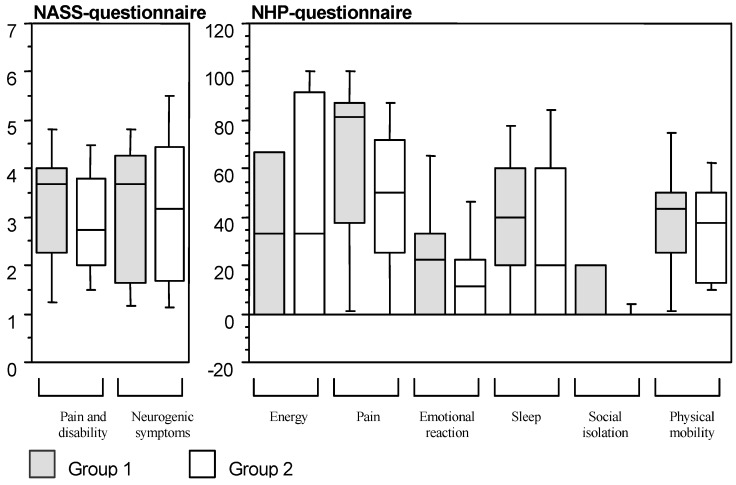
Clinical parameters-NASS and NHP questionnaires
Of all patients, 87.5% (26 in group 1 and all 23 in group 2) answered the questionnaire. Results of the NASS Outcome Instrument and the NHP are summarized in Fig. 1 and Table 2. Results of the NASS subscales showed no statistical difference between the two groups. A mean value of 3–3.3 in subscales “pain and disability” and “neurogenic symptoms” means that these symptoms and impediments occur occasionally. Although the results of the NHP questionnaire were slightly better in group 2, the difference between both groups was not statistically significant, except in the subscale “pain” (p=0.027). The two different surgical approaches did not influence the clinical outcome. Also, gender, age, and radiological fusion did not have significant effects on the clinical outcome.
Fig. 1.
Results of the North American Spine Society (NASS) Lumbar Spine Outcome Assessment Instrument and the Nottingham Health Profile (NHP) related to the two different surgical approaches. Group 1: Anterior lumbar interbody fusion (ALIF) with conventional approach (n=26). Group 2: ALIF with minimally invasive approach (n=23). The 17 NASS items are split into two scales, the pain and disability scale and the neurogenic symptoms scale. Each question scaled 1 (not at all) to 6 (extremely). NHP subscales are energy, pain, emotional reaction, sleep, social isolation, and physical mobility. Results of each subscale are standardized from 0 to 100, with high scores indicating reduction in quality of life
Table 2.
North American Spine Society (NASS) Lumbar Spine Outcome Assessment Instrument and the Nottingham Health Profile (NHP) questionnaires; mean values and significance
| Group 1 (n=33) conventional approach |
Group 2 (n=23) minimally invasive |
p value | |
| NASSa subscales | |||
| Lumbar pain and disability | 3.3 | 3.0 | 0.28 |
| Neurogenic symptoms | 3.3 | 3.2 | 0.75 |
| NHPb subscales | |||
| Energy | 42.3 | 37.7 | 0.52 |
| Pain | 65.4 | 46.7 | 0.02* |
| Emotional reaction | 22.7 | 15.5 | 0.19 |
| Sleep | 37.7 | 34.8 | 0.62 |
| Social isolation | 6.2 | 3.5 | 0.13 |
| Physical mobility | 39.4 | 38 | 0.78 |
Mean values expressed: * significant
a NASS Lumbar Spine Outcome Assessment Instrument
b NHP
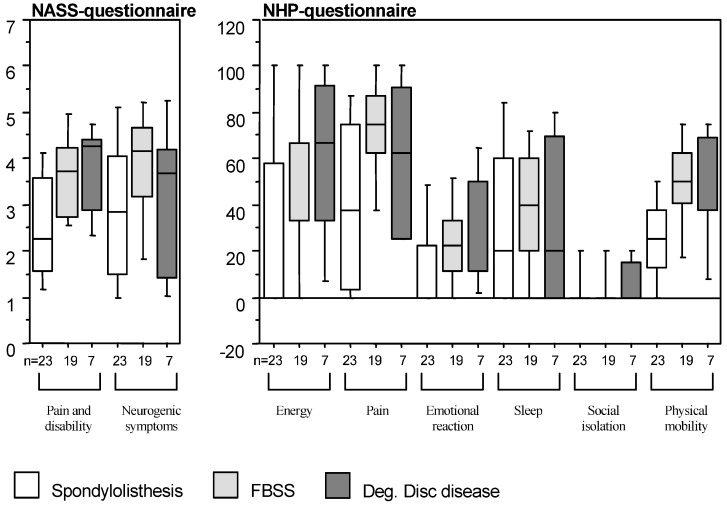
The questionnaires showed significant differences between both groups when related to indication for fusion. Fig. 2 shows the subscale results according to the different indications. In the NASS subscale “lumbar pain and disability”, there were statistical differences between the spondylolisthesis and the FBSS groups (p=0.006) as well as the spondylolisthesis and the degenerative disc disease group (p=0.026). In the NASS subscale “neurogenic symptoms”, significant differences were found between the spondylolisthesis and the FBSS group (p=0.044). Compared with the FBSS group, the spondylolisthesis group also presented significantly better results in the NHP dimensions “energy” (p=0.042), “pain” (p=0.008), and “physical mobility” (p=0.002).
Fig. 2.
Results of the North American Spine Society (NASS) Lumbar Spine Outcome Assessment Instrument and the Nottingham Health Profile (NHP) related to the different indications. FBSS failed back surgery syndrome
Complications
Complications encountered were vascular injuries, sympathetic dysfunction, injury of the lateral femoral cutaneus nerve, ileus, deep venous thrombosis (DVT), superficial wound infection, and dislocation of the iliac bone graft. The incidence of each of these events is summarized in Table 3. One patient in group 1 had a laceration of the left common iliac vein. The second patient had substantial blood loss due to a torn lumbar vein. In group 2, there were also incidences of lacerations of the left common iliac vein and a segmental artery. Both injuries could be ligated with endoclips. In both groups, 9% of patients complained about a sympathetic dysfunction, with one leg being drier and colder than the other (p=0.959). In group 1, 12% of patients, and in group 2, 4% of patients reported postoperative hyperesthesia in the area of the left lateral cutaneus nerve of the thigh (p=0.316). Three patients (9%) in group 1 developed a postoperative weakness of the left abdominal muscles. Abdominal muscle weakness was not seen after the minimally invasive approach in group 2. One patient in group 2 developed superficial wound infection at the posterior instrumentation site, which resolved with intravenous antibiotics; no operative debridement was necessary, and suture removal was uneventful. There was no significant difference in the incidence of complications in both study groups.
Table 3.
Complications after anterior lumbar interbody fusion (ALIF) with posterior instrumentation in both study groups
| Complications | Group 1 (n=33) conventional approach |
Group 2 (n=23) minimally invasive |
| Intraoperative | ||
| Vascular injuries | 2 | 2 |
| Postoperative | ||
| Paralytic Ileus | 2 | 2 |
| Deep venous thrombosis | 1 | 0 |
| Dislocation of the iliac bone graft | 1 | 0 |
| Superficial wound infection | 0 | 1 |
| Weakness of left abdominal muscles | 3 | 0 |
| Sympathetic dysfunction | 3 | 2 |
| Lateral femoral cutaneus nerve injury | 4 | 1 |
| Total | 16 (48.5%) | 8 (34.8%) |
Discussion
The patient collective presented in this report consists of two comparable age-matched groups of ALIF operations where the same group of surgeons used either the conventional or the minimally invasive extraperitoneal approach to the lumbar spine. In addition, autologous iliac crest grafts were used for interbody fusion in both the groups with posterior instrumentation and posterolateral fusion in all cases.
In this report, the minimally invasive approach clearly achieved better results compared to the conventional approach as far as incision length, blood loss, and surgery time were concerned. The length of the skin incision depended naturally on patient size as well as the number of fusioned levels [11]. For the minimally invasive approach, incisions between 6 and 20 cm have been reported [9, 39]. In one case in this study, in the minimally invasive group, a skin incision measuring 24 cm was necessary in an adipose patient. Such a long incision may not seem fitting for the term “minimally invasive.” It does apply, however, when one considers that a comparative incision by the conventional approach would have to be approximately 50 cm long. A self-retaining spreader frame allowed a skin incision of only 4 cm in the minimally invasive approach by Mayer. The retraction frame is screwed into vertebral bodies to be fused. With this system, skin, muscles, and the retroperitoneal space are spread apart in order to have a sufficient surgical view of the intervertebral space [24]. This technique permits a very small skin incision; however, a second incision is required to obtain the autologous iliac crest dowel. Since we do not have this special frame, we preferred to take slightly bigger incisions with the advantage that this allowed us to harvest bone grafts from the anterior iliac crest through the same incision. Thus, we did not need to make an additional incision for bone graft acquisition, as described by Mayer.
Average blood loss using the conventional approach in group-1 was 600 ml, which is similar to that reported in literature [20, 25]. The 260 ml average blood loss in group 2 was significantly less compared to group 1. Other reports using the minimally invasive approach have also reported 200–300 ml blood loss [9, 32, 38]. Mayer stated an average blood loss of less than 70 ml. However, since he used a separate incision for procuring bone grafts, the blood loss caused during harvesting bone grafts is not calculated in the total blood loss [24].
Average duration of surgery for group 1 was 126 min. This is comparable to the reported range of 117–142 min by conventional ALIF [9, 38, 39]. The minimally invasive approach in group 2 was not only significantly faster (100.5 min) in comparison to group 1 but also below the average surgical times reported in the literature using the minimally invasive approach for ALIF [9, 32, 39]. The 111 min reported by Mayer do not include the time required to obtain the autologous bone graft [24].
Anterior lumbar interbody fusion alone has been cited to have fusion rates between 56 and 80% [10, 17, 23, 36]. By combining the anterior lumbar interbody fusion with posterior instrumentation, the pseudoarthrosis rate decreases substantially [3, 7]. Many reports have documented high fusion rates (88–100%) and low pseudoarthrosis rates using anteroposterior fusion [13, 20, 23, 24, 35]. A fusion rate of 92% in group 1 (conventional approach) of this study is similar to that in other series with anterior-posterior fusion. The marginally lower fusion rate of 84% in group 2 in our report was not statistically significant in comparison to group 1.
Complication rates for ALIF are in general low, and those for the conventional and minimally invasive approach reported in separate studies are comparable. We also found insignificant differences in the complication rates in our two study groups. The dangers involved in the anterior approach in general are injury to vascular structures, the sympathetic chain, and the hypogastric plexus. Vascular injuries are prone to occur in presence of anatomical variations, scarred tissue, or when the disc space is exposed too far laterally. Massive blood loss can result, particularly when large vessels are lacerated. One patient in group 1 lost 2,000 ml of blood after a lumbar vein was torn from the inferior vena cava. Similar acute massive blood losses have been reported to occur occasionally with both conventional and minimally invasive approaches during ALIF [14, 21, 25, 29, 31, 39].
The danger of injuring the hypogastric plexus, which in men may result in retrograde ejaculation, is small when operating by the retroperitoneal approach but cannot be completely excluded. Reported incidence of retrograde ejaculation in men who had undergone fusion by retroperitoneal approach is 1–10% [29, 32, 35, 36, 39]. This takes place especially when monopolar diathermy or microdiathermy is used instead of endoclips [32]. In this study, there was no incidence of sexual dysfunction. No sexual dysfunctions were reported by Penta et al. and DeWald et al. in minimal-invasive approaches [9, 27]; nor by Hacker and Kozak et al. by the conventional approaches [14, 20]. In a prospective study, Sasso et al. documented that a transperitoneal approach to the lumbar spine L4-S1 has a 10-times greater chance of causing retrograde ejaculation in men than a retroperitoneal approach for anterior lumbar interbody fusion [33]. Sympathetic dysfunction where the patients complained that one leg felt drier and colder than the other was observed in 9% of patients in both groups of this study. This falls within the reported incidence of 4–10% with minimally invasive approaches and 5–16% with conventional approaches for ALIF [14, 29, 38].
The incidence of a postoperative ileus after ALIF has been cited between 0–11% [9, 27, 29, 32, 35, 38, 39]. The ileus incidence in our collective was in the same range, with spontaneous appearance of peristalsis on the third to fourth postoperative day in all cases. DVT occurrences vary from no or few incidences to 4.5% [27, 29, 32]. In this study, one patient in the conventional approach (group 1) demonstrated DVT. This was managed conservatively with antithrombotic medications and ultrasound control examinations; a spontaneous resolution was observed. Postoperative wound infections after ALIF have been cited to be between 1 and 2% [27, 32, 36]. We had one superficial postoperative infection in the minimally invasive group at the posterior instrumentation site, which resolved with antibiotics.
In one case in our study, the impacted bone graft dislocated. The graft in L4–5 in a patient in group 1 who underwent a double-level fusion L3–5 was noted to be dislocated 1.5–2 cm anteriorly on immediate postoperative radiographs. A pseudoarthrosis resulted at this level. The patient refused reoperation. Today, the patient has a poor clinical outcome and is not satisfied with the result of the operation. Other authors describe dislocated bone grafts in 1–2% of cases where the patients submitted to subsequent reoperation. However, no statement is made in these reports concerning the clinical outcome in these cases [25, 28, 29]. Le Huec et al., in a biomechanical cadaveric study, documented that supplementation of the ALIF with an anterolateral plate provided significant additional stabilization in all directions [22]. We did not use supplemental plate fixation in our cases; it is possible that this complication could have been avoided if additional anterior plating was used. Very seldom yet reported complications of anterior spinal fusions are thrombotic occlusions of the distal aorta [5], iliac artery [21, 31], retroperitoneal fibrosis [6], and an acute postoperative pancreatitis [30]. None of them were encountered in our study.
In a recent paper, Kaiser compared retrospectively the minimally invasive and the laparoscopic approach for ALIF [18]. Although the outcomes were more or less the same in his report, there was a complication of retrograde ejaculation in 45% of the laparoscopic group versus 6% in the minimally invasive group. They further state in their report “on the basis of our data and previously published reports, we have essentially abandoned laparoscopic ALIF. We rely primarily on the mini-open (minimally invasive) laparotomy whenever we perform an ALIF.” Based on this, and on the fact that the chances of retrograde ejaculation are 10 times more with a transperitoneal approach than an retroperitoneal one, we believe that the retroperitoneal minimally invasive approach is the best option when performing ALIF.
To our knowledge, this study is the first report comparing the conventional extraperitoneal approach with the minimally invasive approach for ALIF. In our experience, ALIF can be performed with a minimally invasive extraperitoneal approach without increasing risks of complications or rates of pseudoarthrosis. In addition, the minimally invasive approach involves smaller incisions, less surgical exposure time, and less intraoperative bleeding, and is associated with significant improvement in postoperative back pain in comparison to the conventional approach for ALIF.
References
- 1.Albee JAMA. 1911;57:885. [Google Scholar]
- 2.Andersson BJ (1995) Epidemiology. In: Weinstein JN, Rydevik BL, Sonntag VH (eds) Essentials of the spine. Raven, New York, pp 1–10
- 3.BarnesJ Neurosurg 200195111453405 [Google Scholar]
- 4.Capener Br J Surg. 1932;19:374. [Google Scholar]
- 5.Castro J Spinal Disord. 2000;13:538. doi: 10.1097/00002517-200012000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Chan Clin Radiol. 1983;34:331. doi: 10.1016/s0009-9260(83)80354-7. [DOI] [PubMed] [Google Scholar]
- 7.Christensen Int Orthop. 1997;21:176. doi: 10.1007/s002640050145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daltroy Spine. 1996;21:741. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 9.DeWaldAm Surg 199965619915535 [Google Scholar]
- 10.Flynn J Bone Joint Surg Am. 1979;61:1143. [PubMed] [Google Scholar]
- 11.Fraser J Bone Joint Surg Br. 1982;64:44. doi: 10.1302/0301-620X.64B1.6461662. [DOI] [PubMed] [Google Scholar]
- 12.Fujimaki Clin Orthop. 1982;165:164. [PubMed] [Google Scholar]
- 13.Grob Arch Orthop Trauma Surg. 1991;111:20. doi: 10.1007/BF00390187. [DOI] [PubMed] [Google Scholar]
- 14.Hacker Spine. 1997;22:660. doi: 10.1097/00007632-199703150-00017. [DOI] [PubMed] [Google Scholar]
- 15.Harmon Clin Orthop. 1960;18:169. [Google Scholar]
- 16.Hunt J Epidemiol Community Health. 1980;34:281. doi: 10.1136/jech.34.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ishihara J Spinal Disord. 2001;14:91. doi: 10.1097/00002517-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 18.KaiserNeurosurgery 2002519712182440 [Google Scholar]
- 19.Kohlmann Soz Praventivmed. 1997;42:175. doi: 10.1007/BF01300568. [DOI] [PubMed] [Google Scholar]
- 20.Kozak Spine. 1990;15:322. doi: 10.1097/00007632-199004000-00014. [DOI] [PubMed] [Google Scholar]
- 21.KulkarniEur Spine J 2003124812592547 [Google Scholar]
- 22.Le Eur Spine J. 2002;11:130. doi: 10.1007/s005860100316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linson Spine. 1991;16:143. [PubMed] [Google Scholar]
- 24.Mayer Spine. 1997;22:691. doi: 10.1097/00007632-199703150-00023. [DOI] [PubMed] [Google Scholar]
- 25.O’BrienClin Orthop 19862031912937594 [Google Scholar]
- 26.Ogon M, Maurer H, Wimmer C, Landauer F, Sterzinger W et al (1997) Minimally invasive approach and surgical procedure in the lumbar spine. Orthopäde 26:553–561 [DOI] [PubMed]
- 27.Penta Spine. 1997;22:2429. doi: 10.1097/00007632-199710150-00021. [DOI] [PubMed] [Google Scholar]
- 28.Pose Z Orthop. 1999;137:437. doi: 10.1055/s-2008-1037387. [DOI] [PubMed] [Google Scholar]
- 29.Rajaraman J Neurosurg. 1999;91:60. doi: 10.3171/spi.1999.91.1.0060. [DOI] [PubMed] [Google Scholar]
- 30.Rajaraman Eur Spine J. 2000;9:171. doi: 10.1007/s005860050230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raskas Clin Orthop. 1997;338:86. doi: 10.1097/00003086-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Regan JJ, Yuan H, McAfee PC (1999) Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery. A prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine. 24:402–411 [DOI] [PubMed]
- 33.Sasso Spine. 2003;28:1023. doi: 10.1097/00007632-200305150-00013. [DOI] [PubMed] [Google Scholar]
- 34.Seelig Z Orthop. 1989;127:346. doi: 10.1055/s-2008-1044674. [DOI] [PubMed] [Google Scholar]
- 35.Slosar Spine. 2000;25:722. doi: 10.1097/00007632-200003150-00012. [DOI] [PubMed] [Google Scholar]
- 36.Stauffer J Bone Joint Surg Am. 1972;54:756. [PubMed] [Google Scholar]
- 37.Takahashi Spine. 1990;15:1211. doi: 10.1097/00007632-199011010-00022. [DOI] [PubMed] [Google Scholar]
- 38.Wimmer Orthopade. 1997;26:563. doi: 10.1007/s001320050124. [DOI] [PubMed] [Google Scholar]
- 39.Zdeblick Spine. 2000;25:2682. doi: 10.1097/00007632-200010150-00023. [DOI] [PubMed] [Google Scholar]
- 40.ZuchermanSpine 1995220298578381 [Google Scholar]