Abstract
The aim of this study was to define the influence of whiplash injuries on the perceived condition of health 3 years after injury. We evaluated remaining symptoms and the use of health services. Insurance companies provided reports and medical certificates from traffic accidents in Finland in 1998, for those injured who had agreed to take part in the study. Participants in the 1-year follow-up study answered a self-report questionnaire. Three years after the whiplash-causing accident, 11.8% of participants reported that injury symptoms had caused their health to deteriorate significantly as compared with before the accident. Neck pain was the most common single symptom, reported by 14.6% of respondents. The severity of the initial symptoms according to the WAD classification is reflected in the subject’s self-perception of health after 3 years. A remarkable 10–17% of respondents still used health services regularly because of the symptoms. Although some of the injured had improved in the long term, some reported that their health condition was worse after 3 years than at the 1-year follow-up. The percentage of respondents reporting a significant health deterioration remains unchanged 3 years after the whiplash injury. These findings illuminate the importance of early recognition of risk factors for long-term disability and the primary treatment and rehabilitation procedures.
Keywords: Whiplash injury, Traffic accidents, Prognosis, Rehabilitation
Introduction
The incidence of whiplash-associated disorders after traffic accidents appears to be increasing, although the total number of traffic-accident injuries is slightly decreasing [8]. A considerable number of injured have prolonged symptoms. It has been noted that as much as 50% of those with whiplash injuries had residual symptoms 17 years after the accident [2]. Other studies show a general prevalence of neck pain and severe headaches in individuals with a history of neck injury from a car collision [4]. A history of whiplash injury apparently not only increases risk of future neck pain, but also other health complaints and psychological complications. It is thus associated with adverse effects on everyday activities [1, 9]. However, data on incidence of chronic symptoms after whiplash vary widely from country to country [6]. Despite intensive studies, the causes of long-term disability remain unknown [8]. Our previous study noted that in Finland nearly 10% of those who suffered a whiplash injury in a traffic accident felt that their health was significantly worse at the 1-year follow-up than before the accident [10]. The WAD (whiplash associated disorders) classification presented by the Quebec Task Force [13] predicted the duration of work disability and the long-term health damage caused by the injury [10]. In the present study we were interested in how the injured managed 3 years after the trauma. The aim was to define the impact of the whiplash injury on the perceived condition of health in the long term, the remaining symptoms and need for health services.
Materials and methods
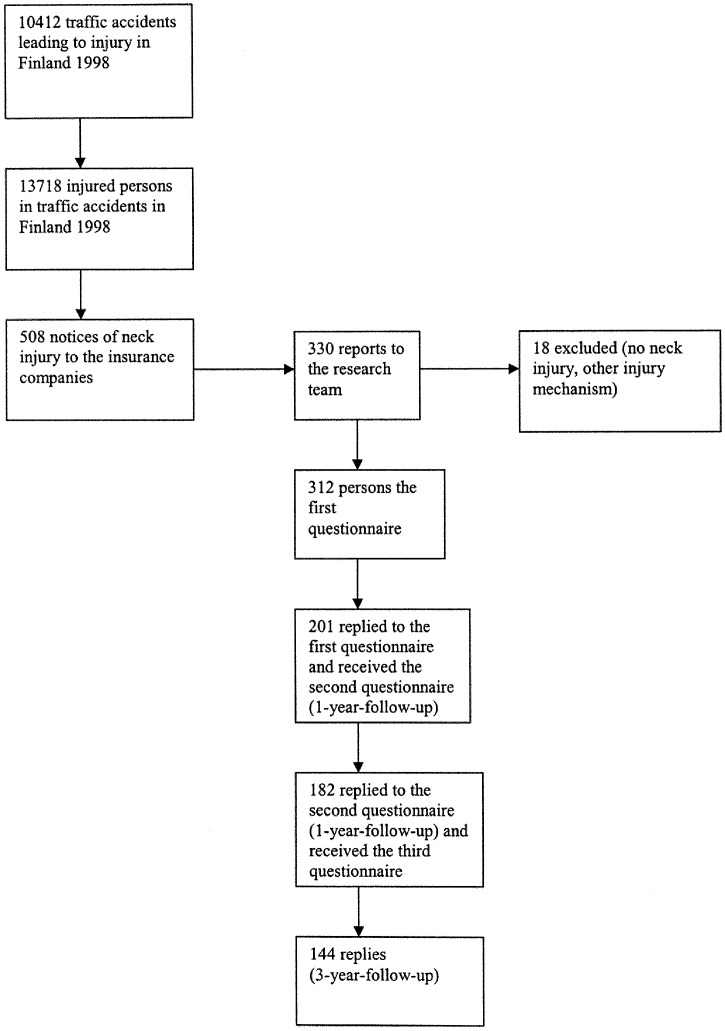
We gathered information from traffic accidents that occurred in Finland in 1998. After an insurance company received notification of a traffic accident-related neck injury, it requested the injured person’s permission to send the relevant personal data and medical certificates to us, for use in the study. A WAD classification was made on the basis of the medical certificate, according to the classification presented by the Quebec Task Force (Table 1). Our first forms were promptly sent to the injured. With self-report questionnaires, we collected demographic data, details about the accident and symptoms related to the subject’s injury and state of health. We also used generally accepted, validated questionnaires concerning state of mind (Beck’s depression index) [17], general psychic stress (general health questionnaire) [12] and subjective estimate of the disability caused by neck pain (neck disability index) [11]. One year after the accident, a new self-report questionnaire was sent to those who had answered the first form. Subsequently, these respondents received a follow-up questionnaire 3 years after the accident, asking for subjective evaluation of the neck injury’s effect on health compared to the situation before the accident, the remaining main symptoms, use of health services and length of possible work disability due to the injury. As shown in Fig. 1, 201 people (64%) answered the first questionnaires, 182 (91%) returned the 1-year follow-up questionnaire and 144 (79%) returned the 3-year questionnaire.
Table 1.
Clinical classification of whiplash-associated disorders by the Quebec Task Force
| Grade | Clinical presentation |
|---|---|
| 0 | No complaint about neck, no physical signs |
| I | Complaint of neck pain, stiffness or tenderness; no physical signs |
| II | Neck complaint and musculoskeletal signs* |
| III | Neck complaint and neurological signs** |
| IV | Neck complaint and fracture or dislocation |
*Decreased range of motion or point tenderness
**Decreased or absent tendon reflexes, weakness, sensory deficits
Fig. 1.
The composition of the research material
Pearson’s Chi-square test was used to evaluate the statistical correlation between WAD classification, age, gender and marital status with change of health after the whiplash injury.
Results
According to WAD classification, there were 2 (1.4%) WAD 0, 68 (47.2%) WAD I, 57 (39.6%) WAD II, 15 (10.4%) WAD III and 1 (0.7%) WAD IV cases in this material. One case could not be classified due to missing medical data. Age and sex distribution and other socio-demographic data are presented in Table 2. Sixty-eight people (47.2%) reported that the whiplash injury did not affect their health after 3 years; 59 (41%) reported that it slightly impaired their health and 17 (11.8%) reported that their health was significantly worse than before the accident, due to symptoms deriving from whiplash. Neck pain was the most common symptom reported, by 21 respondents (14.6%); 7 (4.9%) identified headache as their major complaint, and 6 (4.2%) identified upper extremities as the main problem. A large majority reported suffering two or more symptoms. Most often the symptoms were neck pain combined with headache, symptoms of upper extremities, dizziness and neck stiffness.
Table 2.
Socio-demographic characteristics of respondents at time of accident
| Mean age (years) | |
| Female | 39.3 (SD 13.9) |
| Male | 46.5 (SD 14.2) |
| Gender (n) | |
| Female | 92 (63.9%) |
| Male | 52 (36.1%) |
| Marital status (n) | |
| Single | 20 (13.9%) |
| Married | 95 (55.9%) |
| Widowed | 16 (10.9%) |
| Divorced | 4 (2.8%) |
| Unknown | 9 (6.3%) |
| Education (n) | |
| Primary school | 34 (23.6%) |
| Secondary school | 59 (40.9%) |
| High school graduate | 41 (28.5%) |
| Unknown | 10 (6.9%) |
Of those who said the whiplash injury had significantly impaired their health in the 1-year follow-up, 24% reported managing better after 3 years, and 10.7% said they managed worse. Seventeen people (11.8%) reported using pain medication at least weekly due to whiplash-related symptoms; 12 (8.3%) used neck a collar, two of these (1.4%) at least weekly. During the past year, 24 people (16.7%) had physiotherapeutic treatment for whiplash-related symptoms and six (4.2%) had physiotherapy more than 16 times. Four people (2.8%) had been in a multimodal rehabilitation evaluation. Six (4.2%) reported taking sick leave during the last year because of the injury. Six (4.2%) reported taking sick leave over 6 months during the 3-year follow up. Nine people (6.3%) still had unresolved insurance claims. The WAD classification was significantly reflected (p<0.05) in the impairment of health (Table 3). Gender, age, marital status and education did not significantly correlate with the perceived change of health after 3 years.
Table 3.
Correlation between WAD classification and perceived change in health 3 years after injury (p<0.05, Pearson Chi-square)
| Perceived change in health after 3 years | WAD 0 (%) | WAD I (%) | WAD II (%) | WAD III (%) | WAD IV (%) | Missing WAD data (%) | Total (%) |
|---|---|---|---|---|---|---|---|
| No change | 2 (100) | 36 (52.9) | 24 (42.1) | 6 (40.0) | 0 | 0 | 68 (47.2) |
| Slightly impaired | 0 | 27 (39.7) | 27 (47.4) | 5 (33.3) | 0 | 0 | 59 (41.0) |
| Significantly impaired | 0 | 5 (7.4) | 6 (10.5) | 4 (26.7) | 1 (100) | 1 (100) | 17 (11.8) |
Discussion
Our results show that the proportion of people who experience significant health deterioration compared with before their accidents remains unchanged 3 years after the accident. These findings are in good accordance with several other long follow-up studies [2, 14]. In our material, WAD classification was significantly associated with poor outcome after 3 years. This supports the results of Suissa et al, in that initial-symptom severity—for example, of upper extremities—can predict chronic symptoms after whiplash injury [15]. We consider this finding interesting, because several studies have found that the WAD classification or the severity or multiplicity of initial symptoms did correlate with late symptoms and disability [7, 16]. Although it is often reported that women and older patients have worse outcomes [5, 14], we found no difference between gender and age and the perceived change of health after 3 years.
Whiplash-related costs rise considerably with chronic symptoms [13], the majority related to prolonged sick leave and use of health services. Our study also found people with long work disability during the three-year follow-up, and some had been on sick-leave during the past year. The level of use of other health services, e.g., medication and physiotherapy, is remarkable. In addition, insurance claims can remain unresolved after the three years.
Our results show that, although some people with prolonged disability after a whiplash injury improve after a long time, there is a significant number of people who perceive their health to be worse after 3 years, compared to at the 1-year follow-up. This raises the question of whether other factors, apart from the primary physical injury, may have an effect on the perceived state of health, as also suggested by Castro et al in their experimental study [3].
Although most previous long-term follow-up studies are retrospective in design; ours is prospective. The disadvantage is that the responders form only a small part (144/508, 30%) of all the neck injuries reported to insurance companies in 1998. However, 79% of those taking part in the 1-year follow-up responded to the 3-year follow-up questionnaire. Naturally, there is a danger of a selection bias. However, in our study the prognosis in the long term seems reasonably better than in some other long-term follow-up studies [2, 7, 14].
Conclusions
Our findings suggest that physical and structural factors are not necessarily definitive when the disability lengthens. Although some of the injured improve in the long-term follow-up, the proportion of those who perceive that their health is significantly worse after the whiplash injury remains at the same level. The symptoms vary, with neck pain dominating. A remarkable number of people need regular pain medication and physiotherapy. However, the subjective experience of the disability is an inevitable factor to take into account when planning rehabilitation procedures. Because the proportion of long-term disability remains unchanged, even 3 years after the whiplash injury, it is important to find tools to identify people likely to suffer from prolonged symptoms, in order to improve the possibility of early treatment and rehabilitation.
Acknowledgement
This work was supported financially by the Finnish Motor Insurers’ Centre.
References
- 1.Berglund Jour Clin Epidemiol. 2001;54:851. doi: 10.1016/S0895-4356(00)00369-3. [DOI] [PubMed] [Google Scholar]
- 2.Bunketrop Eur Spine J. 2002;11:227. doi: 10.1007/s00586-002-0393-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castro Int J Legal Med. 2001;114:316. doi: 10.1007/s004140000193. [DOI] [PubMed] [Google Scholar]
- 4.Cote Accid Anal Prev. 2000;32:151. doi: 10.1016/S0001-4575(99)00117-7. [DOI] [PubMed] [Google Scholar]
- 5.Cote Spine. 2001;26:E445. doi: 10.1097/00007632-200110010-00020. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari Clin Exp Rheumatol. 1999;17:321. [PubMed] [Google Scholar]
- 7.Hildingsson Acta Orthop Scand. 1990;61:357. doi: 10.3109/17453679008993536. [DOI] [PubMed] [Google Scholar]
- 8.Lovell Injury. 2002;33:97. doi: 10.1016/S0020-1383(01)00111-5. [DOI] [PubMed] [Google Scholar]
- 9.Mayou Psychosom Med. 1997;59:578. doi: 10.1097/00006842-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Miettinen Clin Exp Rheumatol. 2002;20:399. [PubMed] [Google Scholar]
- 11.Pietrobon Spine. 2002;27:515. doi: 10.1097/00007632-200203010-00012. [DOI] [PubMed] [Google Scholar]
- 12.Scmitz Acta Psychiatr Scand. 1999;100:462. doi: 10.1111/j.1600-0447.1999.tb10898.x. [DOI] [PubMed] [Google Scholar]
- 13.Spitzer Spine. 1995;20:S1. [Google Scholar]
- 14.Squires J Bone Joint Surg. 1996;78B:955. doi: 10.1302/0301-620X78B6.1267. [DOI] [PubMed] [Google Scholar]
- 15.SuissaEur Spine J 2001104411276835 [Google Scholar]
- 16.Söderlund Int J Rehabil Res. 1999;22:77. doi: 10.1097/00004356-199906000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Varjonen Nord J Psychiatry. 1997;51:331. [Google Scholar]