Abstract
To date, only three cases of artificial disc prosthesis dislocation have been reported in the literature. We present in detail two additional cases of prosthesis dislocation and discuss the surgical interventions undertaken that resulted in a good clinical outcome in both patients.
Keywords: Artificial disc prosthesis, Total disc replacement, Degenerative disc disease, Spinal fusion, Low-back pain
Introduction
Of late, total disc replacement has been increasingly used for the treatment of degenerative disc disease, with recent evidence suggesting that it may be a suitable alternative to spinal fusion [2, 4, 5, 6]. Artificial disc prostheses have been available since 1984, with more than 13,000 implanted over the last decade [3]. The use of these prostheses has generally been successful, with only three cases of prosthesis dislocation being reported in the literature [2, 3]. This is the first time that a full case report has been reported highlighting two cases of prosthesis dislocation and the approaches taken to resolve this dislocation. However, the success rate of total disc arthroplasty is still controversial [1].
Case reports
Case 1
A 44-year-old male truck driver with a history of several years of low-back pain and sciatica was referred to our clinic in October 2001. The patient’s pain was exacerbated with work and failed to respond to conservative treatment with pain killers, a back brace and an intensive rehabilitation program. A magnetic resonance imaging (MRI) examination revealed foraminal stenosis and disc degeneration Modic II changes at the L5-S1 level. Electromyography confirmed right lumbar radiculopathy at L5. In June 2002, the patient underwent a total disc replacement using the medium-sized PRODISC implant (Spine Solution, New York, NY, USA). The surgical procedure was uneventful with no immediate postoperative complications and the patient’s pain was significantly reduced with an Oswestry score improvement of 60% (Figs. 1, 2).
Fig. 1.
Postoperative control of Prodisc II prosthesis, AP view
Fig. 2.

Postoperative control of Prodisc II prosthesis, lateral view
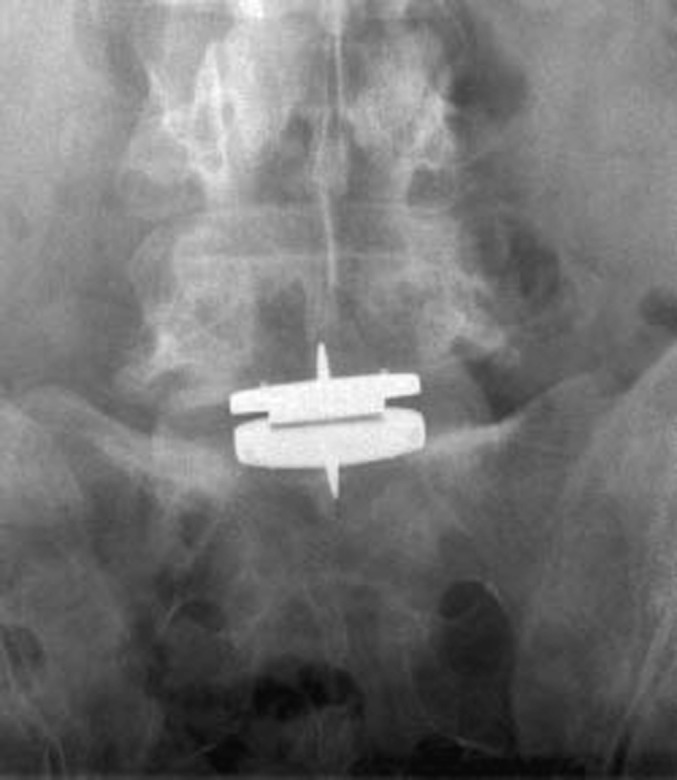
However, 4 months after implantation the patient began to experience severe acute low-back pain. Radiographs revealed that the patient was suffering from a dislocation of the prosthesis with an anterior dislocation of the polyethylene (PE) inlay (Fig. 3).
Fig. 3.

Control at 4 months: dislocation of PE inlay
Because of the the severity of the pain, it was decided to remove the prosthesis using a transperitoneal approach. Unfortunately, it was not possible to replace the prosthesis with a new implant owing to destruction of the anterior part of the endplate at L5 following the removal of the prosthesis. Consequently, an anterior lumbar interbody infusion (ALIF) was performed using a Union carbon cage and a Pyramid anterior plate (Medtronic Sofamor Danek, Memphis, Tenn., USA) (Fig. 4).
Fig. 4.

Revision surgery, fusion with carbon interbody cage and autologus bone and anterior Pyramid plate
The patient recovered quickly from surgery with no postoperative complications. To date, the patient’s pain has been significantly reduced with an Oswestry score improvement of 40%.
Case 2
A 57-year-old woman who had undergone an operation for a disc hernia at the L5-S1 level 18 years previously began to experience low-back pain during 1998. Conservative treatment with nonsteroidal anti-inflammatory drugs and participation in a back school program, which teaches people with back problems how to control their back pain through correctly performing activities of daily living, failed to provide adequate pain relief. Radiographs and a computed tomography (CT) scan revealed no deformity of the facet joints and no evidence of canal stenosis. A brace test was positive and an MRI examination revealed Modic I changes in the L5 and S1 endplates. In May 2001, the patient underwent a total disc replacement using the medium-sized PRODISC II implant. The surgical procedure was uneventful with no postoperative complications. Pain was relieved following the procedure with the patient’s Oswestry score improving from 44 to 10%. However, 1 month after implantation the patient began to experience severe low-back pain, which was treated with analgesics by the general practitioner. Radiographs detected L5-S1 listhesis (grade 1) and evidence of polyethylene inlay dislocation. However, as the patient was now free of pain 6 weeks later with an Oswestry score of 14%, it was decided that regular monitoring of the patient would be sufficient. At a 16-month check-up the patient was still in good condition and was not complaining of back pain; the Oswestry score was 16%. The listhesis appeared stable and there was no evidence of peri-implant lysis, leading us to conclude that a spontaneous fusion had occurred. Nineteen months after the surgery the back pain worsened (Oswestry score 24%) and because of a risk of metallosis in relation with micromotion, it was decided that the patient should undergo surgery. Consequently, posterior fixation with pedicular screws and posterolateral graft fusion were performed 20 months after the initial PRODISC insertion. The surgical procedure was uneventful and the patient experienced significant pain relief.
Discussion
Artificial disc prostheses, which are indicated for the treatment of back pain related to degenerative disc disease, can be implanted at the lumbar levels L2-3, L3-4, L4-5 and L5-S1 [2, 4, 6]. The use of disc prostheses has shown good results in the short term [2, 5, 6], although mid- and long-term data are still lacking and there havebeen no prospective randomized studies comparing this procedure with the “gold standard” lumbar fusion [1]. Studies have shown significant improvement in pain relief along with improvement in pain intensity, walking distance, and lumbar mobility [2, 4, 6]. Moreover, intra- and postoperative morbidity appears to be dramatically reduced compared to lumbar-fusion procedures [3].
PRODISC II, which has been in clinical use since 1999, is an alternative prosthesis with an improved design, enabling implantation through a minimally invasive anterior approach. It is a modular system consisting of two metallic endplates and an inlay made out of polyethylene (PE). The PE inlay is fixed in the lower endplate by a snap-lock mechanism. To accommodate patient anatomy, there are three endplate sizes (small, medium, and large), three heights of the PE component (10, 12, and 14 mm), and two lordosis angles (6 and 11 deg).
Despite being a complex procedure, only three cases of prosthesis dislocation have previously been documented. Mayer et al. [4] reported an anterior dislocation of the PE inlay with PRODISC, which occurred in a patient 5 weeks postoperatively, causing an increase in pain. This was the result of a technical error during implantation when the PE inlay was not completely snapped into the inferior endplate. The PE was removed and replaced, which resulted in a reduction in pain. Van Ooij et al. [5] also reported two cases of dislocation with the Charité disc prosthesis, caused by slow anterior migration and settling of the prosthesis, which were revised with spinal-fusion surgery.
The two cases of prosthesis dislocation reported here were specific to the implantation process, during which the PRODISC was implanted too anteriorly. This occurred as the instruments provided for implantation do not allow exact placement of the prosthesis. In particular, the distraction block is only available in one depth and cannot be adapted for the larger patient or those with large vertebrae. In addition, several limitations have been observed with the instruments provided for implantation. The design of the probe, with its fixed top, prevents the prosthesis from being inserted in the correct posterior position. Insertion of the inlay can be problematic as the distraction opening is not of an adequate size nor is it parallel. Finally, fixation of the inlay in the metallic endplate is not always stable owing to the fact that the lip is only 1 mm and can be easily damaged during insertion. As a result, the inlay cannot always be completely snapped into the metallic endplate, which along with the presence of shear forces, increases the likelihood of dislocation.
In conclusion, this report highlights two cases of PRODISC dislocation within 3 months of surgery. Both dislocations were caused by the PRODISC being implanted too anteriorly and the presence of shear forces caused by this anterior position. The authors suggest that the incidence of prosthesis dislocation could be reduced if the PE inlay had a strong attachment to the lower endplate and by the manufacturers providing a more comprehensive range of tools for implantation. Some modifications to the currently available instruments may improve the implantation procedure to allow for optimal positioning of the implant.
References
- 1.DeEur Spine J 20031210812709847 [Google Scholar]
- 2.Mayer Eur Spine J. 2002;11:S124. doi: 10.1007/s00586-002-0446-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Ooij A (2002) Analysis of 21 patients with clinically failed Charité disc prosthesis. Eur Spine J [Suppl 2], abstract 47
- 4.Mayer Eur Spine J. 2002;11:S85. doi: 10.1007/s00586-002-0445-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeegers Eur Spine J. 1999;8:210. doi: 10.1007/s005860050160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GriffithSpine 19841918427973983 [Google Scholar]


