Abstract
Background
Minimally invasive augmentation techniques of vertebral bodies have been advocated to treat osteoporotic vertebral body compression fractures (VBCFs). Kyphoplasty is designed to address both fracture-related pain as well as kyphotic deformity usually associated with fracture. Previous studies have indicated the potential of this technique for reduction of vertebral body height, but there has been little investigation into whether this has a lasting effect. The current study reports on our experience and the one-year results in 27 kyphoplasty procedures (24 patients) for osteoporotic VBCFs.
Results
All but one patient experienced pain relief following the procedure (on VAS 1–10)—with a lasting effect over the follow-up period in 25 cases. An average vertebral kyphosis reduction of 47.7% was achieved with no loss of reduction after one year. The potential for reduction was statistically related to the pre-operative amount of kyphosis, the level treated, and the age of the fracture, but not to the age of the patient. During follow-up, one fracture adjacent to a treated level was observed. Pain relief was not related to the amount of reduction.
Conclusion
Kyphoplasty is an effective treatment of VBCFs in terms of pain relief and durable reduction of deformity. Whether spinal realignment results in an improved long-term clinical outcome remains to be investigated.
Keywords: Spine, Osteoporosis, Kyphoplasty, PMMA
Introduction
Vertebral body compression fractures (VBCFs) are a common and often debilitating expression of osteoporosis. Patients may suffer from acute episodes of pain as well as chronic pain problems due to the resulting spinal deformities, as the natural history of osteoporotic vertebral fractures is often accompanied by kyphotic collapse of the affected segment. Osteoporotic kyphosis has an adverse effect on the mobility of patients, quality of life and even the rate of survival [3, 11, 19]. Also, the risk of pain and disability increases progressively with the number and severity of vertebral deformities [18].
Conservative management of VBCFs includes analgesics, bed rest, and external bracing. However, some patients do not respond to these therapies in either terms of pain relief or progression of deformity. More invasive surgical procedures such as internal fixation and stabilisation are not the optimal treatment for the majority of patients due to their usually advanced age and associated comorbidities, as well as technical factors such as limited holding power of implants in osteoporotic bone [24]. An ideal therapy should address both fracture-related pain and the associated spinal deformity in a minimally invasive fashion.
During the last few years, percutaneous cement augmentation of the fractured vertebral bodies (vertebroplasty) has been highly advocated as a treatment for focal back pain on the basis of osteoporotic VBCFs [5]. Rapid regression of pain has been found in 80–90% of treated patients, with a long-lasting effect in a similar rate of patients [1, 6, 9, 16]. However, vertebroplasty does not address the associated spinal malalignement as it “freezes” the deformity.
Kyphoplasty is a minimally invasive procedure that aims to address both the fracture pain and the kyphotic deformity. During the procedure, tamps are positioned inside the vertebral body through a working cannula under fluoroscopic control. The tamps are inflated, thereby lifting the endplates and creating a cavity, which, following tamp removal, is filled with bone cement to maintain reduction. In comparison to vertebroplasty, more viscous cement may be introduced with less pressure, thereby decreasing the risk of cement extrusions [17].
A few very short-term studies have reported on clinical results after kyphoplasty, indicating significant pain relief in combination with an initial reduction of local bony kyphosis by 33–50% [7, 14]. There has been little investigation into whether pain relief and particularly reduction of vertebral height are lasting effects. The current study reports on our experience and the one-year results in 27 kyphoplasty procedures (24 patients) for osteoporotic VBCFs.
Materials and methods
Technique
Patients were positioned prone on a radiolucent operating table. Under image intensifier control, eight-gauge 6-inch bone marrow biopsy needles (Manan Trapsystem, MDTech, Gainesville, FL, USA) were percutaneously placed through stab incisions into the fractured vertebral body. After transpedicular positioning, the needles were exchanged over a guidewire for a working cannula.
Inflatable bone tamps (Kyphon, Wezembeek-Oppem, Belgium) were then placed into the vertebral bodies bilaterally. Inflation of the balloons was controlled radiologically and by manometric parameters until the vertebral body height was restored or a pressure of 300psi was reached (maximum certified pressure of balloons). After deflation and withdrawal of the balloons, the remaining vertebral body cavity was slowly filled under fluoroscopic control with PMMA cement (Palacos E-flow, Essex Chemie) corresponding to the combined volume of the inflated balloons.
After the cement had hardened, the working cannulas were removed and the stab incisions closed. After recovery from anaesthesia, patients were allowed to mobilise according to their complaints without any external bracing. Any cement leaks from the vertebral bodies were recorded at surgery or on post-operative radiographs.
Patients
The study included 24 patients (12 male, 12 female) with a follow-up of one year. Overall, 27 vertebral bodies were augmented (Table 1). The average age of the patients was 65.5 years (range 34–79 years). Twenty interventions were performed under intubation, and 4 patients were operated on with local anaesthetic in combination with IV sedation. As the cases described represent our early experience with this technique, we usually recommended surgery under general anaesthesia.
Table 1.
Data of the treated patients: initials, age of the patient, sex, level treated, age of the fracture (pre-operative symptoms), pre-operative vertebral kyphosis, reduction achieved, and correction in percent
| No | Pat | Age | Sex | Level | Age of fracture (days) | Kyph pre-op (°) | Red (°) | Red % |
|---|---|---|---|---|---|---|---|---|
| 1 | WY | 72 | F | T10 | 60 | 10 | 0 | 0 |
| 2 | WY | 72 | F | L2 | 60 | 11 | 4 | 36 |
| 3 | HE | 62 | M | T7 | 40 | 17 | 8 | 47 |
| 4 | HE | 62 | M | T10 | 40 | 21 | 8 | 38 |
| 5 | SH | 77 | M | T12 | >180 | 17 | 3 | 18 |
| 6 | StH | 78 | F | L1 | 40 | 11 | 1 | 9 |
| 7 | StH | 78 | F | L2 | 40 | 10 | 6 | 60 |
| 8 | BS | 62 | F | L1 | 30 | 22 | 10 | 45 |
| 9 | MH | 76 | M | L1 | 10 | 10 | 7 | 70 |
| 10 | KH | 45 | M | T10 | 7 | 20 | 9 | 45 |
| 11 | HG | 75 | F | L1 | 3 | 20 | 9 | 45 |
| 12 | NK | 71 | M | L2 | 11 | 12 | 8 | 67 |
| 13 | HM | 79 | F | T11 | 30 | 16 | 6 | 38 |
| 14 | HE | 75 | M | L2 | 10 | 10 | 6 | 60 |
| 15 | FF | 52 | M | T5 | 22 | 14 | 0 | 0 |
| 16 | CE | 72 | F | L3 | 2 | 10 | 10 | 100 |
| 17 | MC | 65 | F | L1 | 2 | 18 | 6 | 33 |
| 18 | FH | 58 | M | L4 | 4 | 8 | 7 | 88 |
| 19 | WU | 34 | M | L1 | 3 | 14 | 5 | 36 |
| 20 | KH | 66 | M | T12 | 20 | 28 | 18 | 64 |
| 21 | KR | 77 | F | T12 | 90 | 17 | 8 | 47 |
| 22 | FE | 61 | F | L1 | 4 | 20 | 17 | 85 |
| 23 | SE | 53 | F | T12 | 40 | 36 | 12 | 34 |
| 24 | ZC | 63 | M | L1 | 16 | 22 | 10 | 45 |
| 25 | SW | 55 | M | L1 | 7 | 22 | 10 | 45 |
| 26 | BA | 74 | F | L1 | 7 | 16 | 10 | 63 |
| 27 | PN | 71 | F | L1 | 60 | 26 | 18 | 69 |
Indications for the intervention were osteoporotic VBCFs causing focal pain with a kyphosis of 10° minimum or an increase of deformity under initial mobilisation. Most patients did not have any further imaging (CT, MRI, bone scan) prior to the intervention. Several patients could not recall a specific incident as the beginning of their focal pain, and could only give an estimate (e.g. 40 days). In one case (no. 5, SH) the fracture was classified as “old” (>180 days).
Standing films were used to measure kyphosis of the fractured vertebral body as the angulation between both endplates. In some patients, pre-op standing films could not be obtained due to their pain. In these cases measurements were taken from the available supine films. Pre-op films were compared to controls after 2–3 months, 5–6 months, and after one year.
After defining the anatomic landmarks in collaboration, the measurements were taken independently by two different observers (their average serving as the final result). The interobserver reliability was assessed using the Kappa test with a 0.81 agreement. The focal back pain in all patients was determined by VAS scores (from 0 “no pain” to 10 “worst imaginable pain”) pre-operatively and at the follow-up investigations.
Statistics
Multiple regression analysis was conducted to determine the relative importance of the possible independent factors (age, gender, treated level, fracture age and pre-operative kyphosis) as predictors of the final achieved fracture reduction. A stepwise, forward-selection, multiple regression analysis was computed with fracture correction as the dependent variable, using Statistica 6.0 software (StatSoft, Tulsa, OK, USA), with a significance level set at p =0.05.
Results
Twenty-one patients had sustained fractures on the basis of a primary osteoporosis with minimal trauma. The average age in this group was 68 years. Two younger patients suffered from Bechterew’s disease (no. 10, KH, age 45) and osteogenesis imperfecta respectively (no. 19, WU, age 34). One additional patient suffered from steroid-induced secondary osteoporosis (no. 20, KH, age 66). The same patient had to be treated surgically for a bleeding ulcer two days post kyphoplasty. All other interventions were performed without any perioperative or postoperative complications.
Local cement leaks were observed in nine vertebrae (in three patients towards the disc space and in six patients lateral to the vertebral body). None of these findings seemed to have clinical sequelae. During follow-up, the cement plug seemed to have shifted anteriorly in one vertebra, but no loss of reduction or pathological movement could be detected.
All patients could be mobilised within the first 24 h after surgery. Twenty-one patients were hospitalised for 1–3 days. Due to additional injuries, three patients stayed for a maximum of 11 days. In 16 cases kyphoplasty was performed as an isolated procedure, whereas in 8 patients the adjacent levels above and below the kyphoplasty were reinforced with vertebroplasty during the same surgery. Indications for a combined procedure were advanced stage of osteoporosis as well as significant overall kyphosis of the segments to be treated.
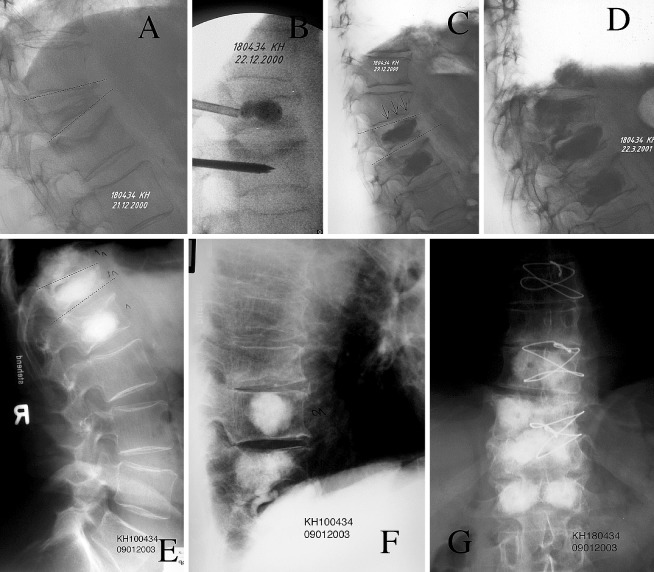
Two patients needed further spine interventions during the one-year follow-up. In one (no. 5, SH), kyphoplasty at T12 failed to relieve the pain and a dorsal stabilisation at L4–S1 was performed due to significant degenerative changes. In that case the VAS data at the latest follow-up was disregarded. In one case (no. 20, KH), an additional fracture developed cranial to the initially treated level T12 and a two-level vertebroplasty was performed at T10 and T11 (Fig. 1).
Fig. 1A–G.
Representative case (no. 20, KH). A Pre-operative situation with severely painful fractures of T12 and L1. Kyphotic deformity of T12=28°. B Treatment of T12 with kyphoplasty and conventional vertebroplasty of L1. Important correction of T12 with 18° immediately postoperative, and absolute disappearance of the pain. C Acute recurrence of pain after 1 week; a fracture of the adjacent vertebra (T11) was observed ( arrows) on the X-ray. D The patient was treated successfully with a conventional vertebroplasty on T11 and T10 that was injected in a prophylactic sense. E–G The course was uneventful with mild pain. The follow-up X-rays after 2 years show a stable situation with no sintering of the reinforced bones and no loss of the initial reduction
All but one patient experienced pain relief following kyphoplasty (Table 2), which was neither related to the level treated nor to the amount of reduction achieved. In two cases early in this series, significant improvement was noted at the 2 month follow-up, whereas 21 patients reported an immediate change. After one year, a constant score on VAS was noted by 17 patients, with a further improvement noted by 4 patients. However, one of them (no. 20, KH) had received further vertebroplasties due to adjacent segment pathology during follow-up.
Table 2.
Pain score as given on VAS (1–10), pre-operatively and at follow-ups. For average values, one patient counts as a single procedure
| No | Pat | Pre-op | Post-op | 2Mo | 1Y |
|---|---|---|---|---|---|
| 1 | WY | 9 | 8 | 3 | 3 |
| 2 | WY | 9 | 8 | 3 | 3 |
| 3 | HE | 5 | 4 | 1 | 1 |
| 4 | HE | 5 | 4 | 1 | 1 |
| 5 | SH | 7 | 7 | – | – |
| 6 | StH | 8 | 1 | 1 | 0 |
| 7 | StH | 8 | 1 | 1 | 0 |
| 8 | BS | 10 | 5 | 1 | 1 |
| 9 | MH | 9 | 2 | 0 | 0 |
| 10 | KH | 10 | 0 | – | 0 |
| 11 | HG | 8 | 2 | 1 | 2 |
| 12 | NK | 3 | 0 | 0 | 0 |
| 13 | HM | 9 | 1 | 0 | 0 |
| 14 | HE | 9 | 2 | 1 | 1 |
| 15 | FF | 10 | 5 | 5 | 8 |
| 16 | CE | 10 | 6 | 4 | 4 |
| 17 | MC | 8 | 4 | 1 | 1 |
| 18 | FH | 9 | 3 | 2 | 1 |
| 19 | WU | 6 | 3 | 2 | 0 |
| 20 | KH | 8 | 4 | 4 | 1 |
| 21 | KR | 9 | 2 | 2 | 2 |
| 22 | FE | 10 | 0 | 0 | 0 |
| 23 | SE | 10 | 6 | 2 | 2 |
| 24 | ZC | 9 | 5 | 2 | 2 |
| 25 | SW | 9 | 5 | 3 | 3 |
| 26 | BA | 7 | 2 | 0 | 0 |
| 27 | PN | 10 | 4 | 3 | 3 |
| Av | 8.4 | 3.8 | 1.7 | 1.5 |
Two patients reported deterioration; one of them (no. 11, HG) with a minimal change of score from “1” at 2 months follow-up to “2” after one year. The other patient (no. 15, FF) had exacerbated pain one year following kyphoplasty at T5. Further interventions were suggested to address the thoracic kyphosis caudal to the treated level, but the patient refused. An acute fracture could not be observed at this stage.
In this series, kyphoplasty achieved a 47.7% average improvement of local bony kyphosis. A loss of reduction after one year was not seen in any case. In 4 of 27 vertebral bodies no or minimal reduction was measured (<20% change). These fractures were located at T5 (one case) or were older than 40 days. In fractures aged 40 days and younger, reduction was possible by 54.6%. In fractures older than 40 days, a change of 35.8% was measured.
Stepwise multiple regression resulted in the following regression formula: FC= −12.571 + 0.553 PK + 0.625 L − 0.037 FA + 0.070 A, r2 =0.651, p <0.0001. FC is the fracture correction in degrees, PK is the pre-operative kyphosis in degrees, L is the treated level, numbered sequentially from 1° at T1 to 17° at L5, FA is the fracture age in days and A is the patient age in years. Significant factors were pre-operative kyphosis ( p <0.0001), treated level ( p =0.035) and fracture age ( p =0.046). Patient age was not a significant predictor ( p =0.279), but inclusion improved the overall predictive power of the regression analysis.
Discussion
Osteoporotic VBCFs are a major cause of back pain in the elderly. Even though only about one third of all fractures come to clinical attention, the sequelae of VBCFs represent a major impact on patients’ physical function, quality of life, and survival. As our population ages, the rate of osteoporotic fractures is expected to triple over the next 30 years [21].
An ideal treatment for VBCFs should relieve fracture-related pain and durably correct the kyphotic deformity of the spinal segment. Vertebroplasty involving the percutaneous injection of polymethylmethacrylate (PMMA) into the vertebral body results in substantial pain relief in the majority of patients, which has led to this technique becoming very popular in the treatment of VBCFs [5]. Kyphoplasty seems to achieve at least comparable results, with pain improvement reported in 95% of cases [7, 12]. The reduction of pain directly contributes to improvements in quality of life and the ability to move independently [12].
We can confirm these results, as all but one patient in our series benefited from the procedure, and the effect was maintained at the one-year follow-up. The amount of reduction in deformity however, was not related to the degree of pain relief. The one failure case early in our experience was probably due to incomplete pre-operative workup, as the treated deformity was old and there were considerable further sources of pain in the lower back. Most of our patients now undergo additional pre-operative imaging, as MRI can document bone marrow edema as a sign of recent fracture and thereby select candidates for the procedure [23].
Recent biomechanical investigations have increased concerns about an increased fracture risk of adjacent non-augmented levels following vertebroplasty [2]. In a clinical series, Grados et al. [8] found that 13 out of 25 patients treated with vertebroplasty (52%) developed a total of 34 new vertebral fractures after a mean follow-up of 48 months. Another study with a two-year follow-up reported a 12.4% rate of new fractures, two-thirds of which were directly adjacent to the previously treated level [22]. In our kyphoplasty series, we observed only one adjacent vertebral fracture in 24 patients, but the follow-up was shorter. From our data, it is too early to conclude whether the risk of adjacent fractures is different following kyphoplasty as compared to vertebroplasty.
Safety issues of vertebroplasty have increasingly become a matter of discussion. Forcible injection of low-viscosity cement is necessary to inject the cement along small diameter tubes and cannulas, leading to cement leakage from the vertebral body in up to 65% of osteoporotic fractures [4]. Serious complications such as pulmonary embolism and paraplegia are rare, but have been reported [10, 13, 15]. Kyphoplasty seems to lower the risk of extravertebral cement leak, as it allows a vertebral cavity to be filled with more viscous cement [14].
In a study of 30 patients treated with kyphoplasty at 70 levels, Lieberman et al. [14] reported minor cement leakage at six levels (8.6%). Ledlie and Renfro [12] recorded 12 PMMA leaks during the repair of 133 fractures (9%). Particularly early in our experience we intended to augment the entire vertebral body rather than only fill the cavity left by the balloon. Vertebroplasty was initially done under higher cement injection pressures, leading to a relatively large rate of (minor) cement leaks (33%). However, no clinically relevant cement extrusions were observed.
Vertebroplasty focuses on prevention of further vertebral collapse. With the exception of very fresh fractures and mobile pseudarthroses, which might respond to a hyperlordotic positioning of the patient on the operating table, a reduction of the deformity does not seem possible. Kyphoplasty has shown the potential to achieve at least partial restoration of vertebral height. In our series, an average improvement of 47.7% of local bony kyphosis was measured. This is within the range of other publications. Lieberman et al. reported a mean vertebral body height restoration of 46.8% [14]. Garfin et al. stated that kyphoplasty improves kyphosis by over 50%, if performed within 3 months of the onset of the fracture [7].
In single cases of very fresh fractures, a height reduction may also be possible by a hyperlordotic positioning of the patient alone, but this potential seems very limited and was not generally seen in this case series. Our data also supports the conclusion that the potential for reduction is time-related. Pre-operative MRI investigation in cases of unclear fracture age may therefore be helpful to determine the potential benefit of kyphoplasty procedures.
The ability to restore vertebral height also improves with the amount of pre-operative kyphosis and more caudally located levels. Whether the latter is due to a more favourable relationship between cortical and cancellous bone remains to be discussed.
Conclusion
The treatment of osteoporotic VBCFs with kyphoplasty reliably reduced pain soon after surgery and at the one-year follow up. A 50% average improvement of local kyphosis was possible, with even more potential for reduction in fractures younger than 6 weeks. After one year, no loss of reduction was seen. However, the specific effect of height restoration and spinal realignment on the long-term clinical outcome and general parameters such as life quality and mortality of the patients remains to be investigated.
Acknowledgements
The authors would like to thank Stephen Ferguson (M.E. Mueller Institute for Biomechanics, Bern, Switzerland) for his statistical analysis of the data
References
- 1.Barr Spine. 2000;25:923. doi: 10.1097/00007632-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 2.Berlemann J Bone Joint Surg Br. 2002;84:748. doi: 10.1302/0301-620x.84b5.11841. [DOI] [PubMed] [Google Scholar]
- 3.Cook Arthritis Rheum. 1993;36:750. doi: 10.1002/art.1780360603. [DOI] [PubMed] [Google Scholar]
- 4.Cortet J Rheumatol. 1999;26:2222. [PubMed] [Google Scholar]
- 5.EinhornSpine 200025105110788846 [Google Scholar]
- 6.Evans Radiology. 2003;226:366. doi: 10.1148/radiol.2262010906. [DOI] [PubMed] [Google Scholar]
- 7.GarfinSpine 200126151111462078 [Google Scholar]
- 8.Grados Rheumatology. 2000;39:1410. doi: 10.1093/rheumatology/39.12.1410. [DOI] [PubMed] [Google Scholar]
- 9.HeiniEur Spine J 2000944511057541 [Google Scholar]
- 10.Jang Spine. 2002;27:E416. doi: 10.1097/00007632-200210010-00021. [DOI] [PubMed] [Google Scholar]
- 11.Kado Arch Intern Med. 1999;159:1215. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 12.Ledlie JT, Renfro M (2003) Balloon kyphoplasty: one-year outcomes in vertebral body height restoration, chronic pain, and activity levels. J Neurosurg (Spine 1) 98:36–42 [DOI] [PubMed]
- 13.Lee Spine. 2002;27:E419. doi: 10.1097/00007632-200210010-00022. [DOI] [PubMed] [Google Scholar]
- 14.LiebermanSpine 200126163111464159 [Google Scholar]
- 15.Padovani AJNR Am J Neuroradiol. 1999;20:375. [PMC free article] [PubMed] [Google Scholar]
- 16.Perez-Higueras Neuroradiology. 2002;44:950. doi: 10.1007/s00234-002-0856-1. [DOI] [PubMed] [Google Scholar]
- 17.PhillipsSpine 200227217312394934 [Google Scholar]
- 18.Ross Am J Med. 1997;103:30S. doi: 10.1016/s0002-9343(97)90025-5. [DOI] [PubMed] [Google Scholar]
- 19.Schlaich Osteoporos Int. 1998;8:261. doi: 10.1007/s001980050063. [DOI] [PubMed] [Google Scholar]
- 20.Silverman Bone. 1992;13:S27. doi: 10.1016/8756-3282(92)90193-z. [DOI] [PubMed] [Google Scholar]
- 21.Truumees Spine. 2001;26:930. doi: 10.1097/00007632-200104150-00016. [DOI] [PubMed] [Google Scholar]
- 22.Uppin Radiology. 2003;226:119. doi: 10.1148/radiol.2261011911. [DOI] [PubMed] [Google Scholar]
- 23.Watts Osteoporos Int. 2001;12:429. doi: 10.1007/s001980170086. [DOI] [PubMed] [Google Scholar]
- 24.Wittenberg Spine. 1991;16:647. doi: 10.1097/00007632-199106000-00009. [DOI] [PubMed] [Google Scholar]