Abstract
Three separate stages have previously been defined in the progressive degenerative process. The first stage, characterized as temporary dysfunction with early degenerative findings, transforms into a second period of segmental instability evidenced by a resulting deformity. With the deformity the process has reached a late stage of definitive stabilization induced by osteoligamentary repair mechanisms. To test the validity of this three-stage hypothesis, we assessed the intervertebral mobility for the two most-distal lumbar disc levels in 18 adult patients with low back pain, disc degenerative findings and no prior spinal surgery. Each spinal segment was categorized according to grade of disc degeneration: (IA) normal disc height without dehydration; (IB) normal disc height with dehydration; (II) disc height decreased by less than 50%; (III) disc height decreased by at least 50%; and (IV) disc height obliterated. The intervertebral mobility was measured by radiostereometric analysis (RSA) and compared between the categories. With the patient changing position from supine to sitting, the mean vertical translation across the 11 discs categorized as IA was 2.0 mm. A small increase in mean vertical mobility with progressive loss of disc height through the degenerative stages IB (2.2 mm, seven discs) and II (2.6 mm, ten discs) was not significant. Further degeneration to grade III meant a significant mean reduction in vertical mobility to 0.8 mm for the eight discs in that category. No discs were classified as obliterated, category IV. The corresponding values for sagittal translations were 3.0 mm, 3.1 mm, 3.6 mm and 1.7 mm for the four disc categories found. These alterations were not statistically significant. We conclude that intervertebral mobility changes throughout the degenerative process, and a stage of stabilization begins when disc height is reduced by 50%. The segmental mobility status cannot be deduced from the radiographic, degenerative disc stage, since the inter-individual differences in mobility are pronounced for the same disc status. A fully stable situation cannot be taken for granted, even when the disc is reduced by more than 50%, considering the fact that some persisting mobility was seen for most patients in category III. A preceding stage of instability, in the clinical situation proven by a resulting deformity, was not verified in this study.
Keywords: Degenerative disc disease, Radiostereometric analysis, Intervertebral translations, Segmental instability
Introduction
The pathomechanics of the degenerative lumbar spine was described by Kirkaldy-Willis and Farfan [9], who postulated three stages with differing conditions of stability and motion. The early degenerative stage, named temporary dysfunction, is thereby assumed to transform into a stage of segmental instability evidenced by the resulting deformity. With the deformity, the process has reached the third and last stage of definitive stabilization. Such a three-stage course would have certain clinical implications but has been hard to confirm, in part due to a high error of measurement with conventional radiographic techniques.
Radiostereometric analysis (RSA) [16] brings the possibility of measuring intervertebral mobility with high accuracy [6]. Introducing percutaneous technique—for the application of the skeletal markers required for RSA—now offers an opportunity to study pathological spinal conditions before surgical intervention [1]. We applied RSA to assess the intervertebral mobility in patients considered for lumbar fusion due to low back pain and degenerative disc disease. The discs were assessed and categorized into five grades of degeneration, and the intervertebral kinematics were studied for each category. The aim was to test the hypothesis by Kirkaldy-Willis and Farfan [9] that the degenerative process includes an unstable phase, and we sought to determine whether and when it ends up in a stabilized condition with a fixed deformity.
Materials and methods
Patients
Eighteen patients, 12 women and six men, were considered for a lumbar fusion due to long-standing low back pain and had an external fixation test, according to Magerl [12], as part of the preoperative prognostication [13]. Mean age was 44 years (33–59). The mean duration of low back pain was 5 years (1–15). No patient had sciatic pain and none had been previously treated with spinal surgery. Non-operative treatment had been carried out in all cases but without success. The diagnosis was degenerative disc disease on the level L4–L5 and/or L5–S1. A secondary degenerative slip was seen in two patients, both on the L4–L5 level. The slip measured 5 mm in case 1 (Table 1) and 10 mm in case 16. Patients with spondylolysis were not included.
Table 1.
Intervertebral translations (mm) across 36 discs ordered according to grade of degeneration
| Disc degeneration | Level | Patient number | Transverse translation | Vertical translation | Sagittal translation |
| x* | y* | z* | |||
| IA | L5–S1 | 2 | 0.3 | 3.5 | 5.9 |
| IA | L5–S1 | 3 | 0.2 | 3.0 | 4.8 |
| IA | L5–S1 | 7 | 0.4 | 4.2 | 5.3 |
| IA | L5–S1 | 11 | 0.4 | 0.1 | 1.5 |
| IA | L5–S1 | 15 | 0.3 | 0.9 | 1.5 |
| IA | L5–S1 | 17 | 0.3 | 0.5 | 1.4 |
| IA | L4–L5 | 3 | 0.4 | 1.8 | 2.3 |
| IA | L4–L5 | 13 | 0.4 | 2.9 | 3.8 |
| IA | L4–L5 | 14 | 1.4 | 3.9 | 4.5 |
| IA | L4–L5 | 15 | 0.2 | 0.8 | 1.3 |
| IA | L4–L5 | 18 | 0.1 | 0.9 | 0.8 |
| IB | L5–S1 | 8 | 0.6 | 1.1 | 6.4 |
| IB | L5–S1 | 16 | 0.4 | 1.9 | 2.6 |
| IB | L5–S1 | 18 | 0.1 | 1.8 | 2.0 |
| IB | L4–L5 | 5 | 0.3 | 0.6 | 0.9 |
| IB | L4–L5 | 6 | 0.1 | 0.6 | 0.8 |
| IB | L4–L5 | 9 | 0.4 | 7.1 | 6.0 |
| IB | L4–L5 | 12 | 0.6 | 2.3 | 2.9 |
| II | L5–S1 | 4 | 0.1 | 3.9 | 5.6 |
| II | L5–S1 | 5 | 0.2 | 0.4 | 0.8 |
| II | L5–S1 | 9 | 0.3 | 1.7 | 3.8 |
| II | L5–S1 | 12 | 0.4 | 1.6 | 2.9 |
| II | L4–L5 | 2 | 0.8 | 5.9 | 3.6 |
| II | L4–L5 | 4 | 0.1 | 3.7 | 4.4 |
| II | L4–L5 | 7 | 0.3 | 5.6 | 4.7 |
| II | L4–L5 | 8 | 0.8 | 0.8 | 6.4 |
| II | L4–L5 | 10 | 0.2 | 1.2 | 1.3 |
| II | L4–L5 | 17 | 0.1 | 1.5 | 2.2 |
| III | L5–S1 | 1 | 0.1 | 0.6 | 0.6 |
| III | L5–S1 | 6 | 0.4 | 0.5 | 3.1 |
| III | L5–S1 | 10 | 0.1 | 0.9 | 1.4 |
| III | L5–S1 | 13 | 0.1 | 1.0 | 1.9 |
| III | L5–S1 | 14 | 0.4 | 1.2 | 2.8 |
| III | L4–L5 | 1 | 0.1 | 1.6 | 2.6 |
| III | L4–L5 | 11 | 0.1 | 0.1 | 0.2 |
| III | L4–L5 | 16 | 0.7 | 0.2 | 0.6 |
*Minimum significant measurement is 0.5 mm (x), 0.5 mm (y) and 0.7 mm (z)
Radiography
All patients were examined by conventional radiography, antero-posterior (AP) and lateral views, as well as T1- and T2-weighted MRI. On this basis, the preoperative status of the L4–L5 and L5–S1 discs were assessed semi-quantitatively, according to a classification modified from Saraste et al. [15]. Five categories were then defined with the following disc characteristics:
- IA
Normal disc height without dehydration
- IB
Normal disc height with dehydration
- II
Disc height decreased by less than 50%
- III
Disc height decreased by at least 50%
- IV
Disc height obliterated
External pedicular fixation
The pedicular Schanz screws for the external fixator and the tantalum indicators for the RSA were inserted during general anesthesia. Percutaneous technique was applied using an image intensifier for localization in both the AP and lateral planes. The 0.8 mm tantalum indicators were placed in L4 and L5 in a standardized pattern, with the bases of the transverse processes and the tip of the spinous process as landmarks (Fig. 1). In the sacrum, the lateral masses and central crest were used.
Fig. 1.
The formation of tantalum indicators placed in each vertebra, analyzed for intervertebral mobility along the x, y, and z axis
The time for test fixation was 1 week for all patients (2). The test procedure was then completed by removal of the frame, including extraction of the pedicular screws. Two months later, the radiostereometric analysis was performed. By that time, the influence of the external fixation test on the lumbar mobility was considered minimal, since the soft tissues were fully healed and the patients had regained their usual low back pain.
Radiostereometry
Spinal RSA was performed with two roentgen tubes, which were 40° angulated, and a combined reference plate and calibration device with 0.8 mm tantalum indicators placed at known positions in front of the film plane. The intervertebral translations across the two most-distal lumbar disc levels were measured with the patient changing position from supine to sitting, a method providing enhanced but standardized mobility provocation of the lower lumbar spine [7]. Using the Kinema program for computed data processing according to Selvik [16], the intervertebral translations along the transverse (x), vertical (y) and sagittal (z) axes were calculated (Fig. 1), representing a measure for the provided three-dimensional vertebral movement. The measurement accuracy with this RSA setup has been calculated by double examinations of healed non-instrumented fusions and the minimum significant measurement—i.e., the accuracy level for each axis—is 0.5 mm (x) , 0.5 mm (y) and 0.7 mm (z) [8]. Values below these were considered insignificant.
Statistics
For statistical analysis, the Student t-test was used to find the difference between means.
Results
Grade of disc degeneration
For 11 discs there were no signs of degeneration (IA) (Table 1). Dehydration without disc-height reduction, categorized as IB, was seen in seven discs. Category II (disc height decreased less than 50%) and III (disc height decreased at least 50%) included ten and eight discs, respectively. No disc among the 36 was obliterated, i.e., no category-IV discs were seen.
Transverse translation (x)
The transverse translations were mostly negligible (Table 1) and did not differ between the four categories of disc degeneration identified.
Vertical translation (y)
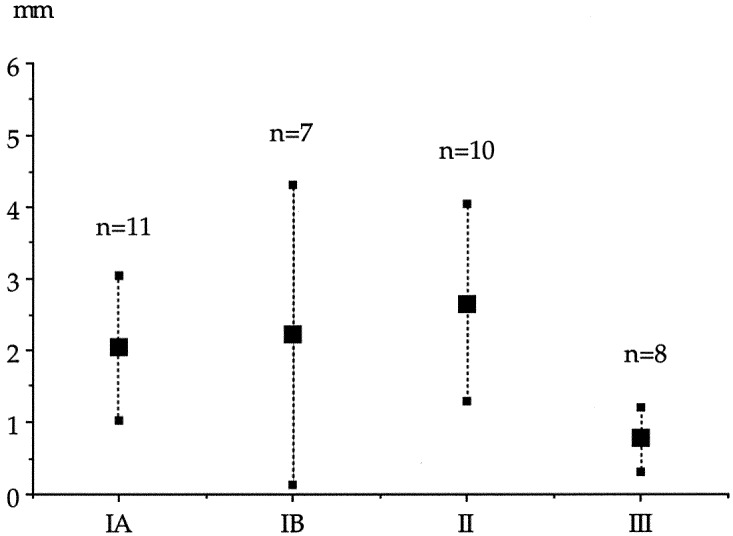
The mean vertical, intervertebral mobility is given in Fig. 2, with the 36 discs categorized into the four groups of degeneration found. Across the 11 discs without degeneration (IA), the mean vertical mobility was 2.0 mm. A small increase in mean vertical mobility with progressive loss of disc height through the degenerative stages IB and II was not significant, according to the confidence intervals given in Fig. 2. The mean values were 2.2 mm and 2.6 mm, respectively. With further degeneration to grade III, a decrease was demonstrated that was significant (p=0.01), with a mean vertical mobility of 0.8 mm for the eight discs in that category.
Fig. 2.
Mean, vertical intervertebral mobility with confidence intervals given for 36 discs categorized according to grade of degeneration
No significant vertical mobility was provided across four discs, one in category IA, one in category II and two in category III (Table 1). The most mobile segment in the vertical direction was seen in patient No. 9, with a translation of 7.1 mm at the L4–L5 level categorized as IB.
Sagittal translation (z)
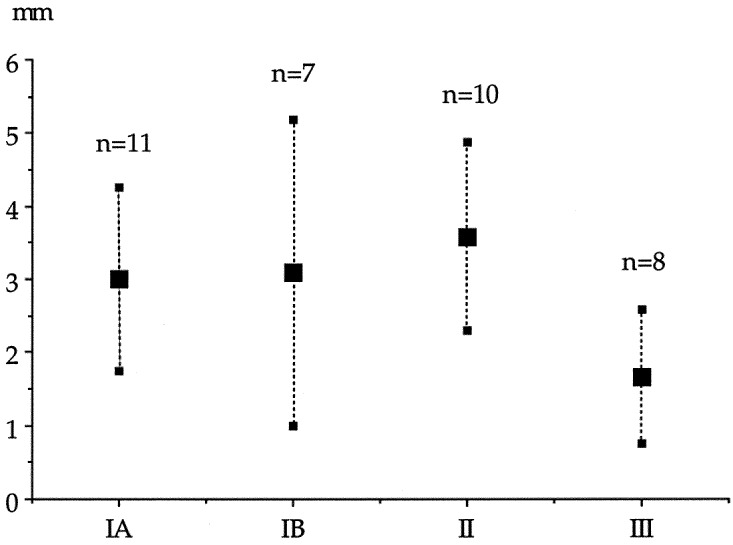
The mean sagittal, intervertebral mobility across the 11 discs categorized without degeneration (IA) was 3.0 mm. The corresponding values were 3.1 mm for degeneration-grade IB (seven discs), 3.6 mm for grade II (ten discs) and 1.7 mm for grade III (eight discs). The values are seen in Fig. 3 with no significant difference for the mean translations in this plane, according to the confidence intervals given. Lack of significant sagittal translation was seen across three discs, all having degenerative findings grade III (Table 1). The highest value for sagittal translation, 6.4 mm, was seen for two discs categorized as grade IB and grade II (both from patient No. 8).
Fig. 3.
Mean, sagittal intervertebral mobility, with confidence intervals given for 36 discs categorized according to grade of degeneration
Discussion
Three separate stages have been defined in the progressive degenerative process [9]. The first stage is characterized by early degenerative signs of the disc and fibrillation of the articular cartilage of the facet joints. Stage 2 includes a condition of segmental spinal instability, creating the basis for the deformity that is seen as the process transforms into the third stage—stabilization. In this last stage, the deformity is assumed to be stabilized by osteoligamentary repair mechanisms. Applied to the clinical situation, this staging supports treating the stenotic, olisthetic segment in the fixed-deformity stage with only decompression, whereas, according to Kirkaldy-Willis and Farfan [9], a patient in stage 2 instead needs a supplementary fusion.
Several methods have been presented as options for identifying hypermobility in the individual patient. Conventional radiography only reveals secondary findings, such as deformities and traction spurs [11]. Studying kinematics, trying to demonstrate the instability, makes the issue more controversial, calling methods and accuracy into question. Knutsson [10] used lateral radiographs in maximum flexion/extension and claimed that the instability seen, without anatomic degenerative signs, was the consequence of an early disc impairment not detectable by ordinary roentgen examination. An attempt to improve the method by introducing active traction/compression [5] was later questioned and probably of no value [14]. Cineradiography brings the possibility of studying continuous, dynamic lumbar motion in certain pathologic conditions [17]. The drawback of these methods is the measurement accuracy for translatory sagittal movements. All methods use radiographs for the purpose. For a true progressive slip, the difference between two examinations must be about 20% of the sagittal-vertebral diameter [3, 4], which is an obvious limitation in clinical practice.
According to Kirkaldy-Willis and Farfan, the degenerative radiographic findings can be connected to a specific mobility status. This would theoretically make it possible to deduce the stability and, thereby, to select the optimal surgical treatment for the individual patient, even without an adequate measuring method for spinal intervertebral mobility. Radiostereometry [16] applied to spinal mobility [6] cannot be used for the purpose in routine clinical practice. The technique has, however, the measurement accuracy to make it possible to test the hypothesis that the degenerative process includes an unstable phase, and to determine whether (and if so, when) it ends up in a stabilized condition with a diminished risk of a further deformity/slip.
The optimal measurement situation would, of course, include individuals without current low back pain, to eliminate the confounding effects on the spinal mobility induced by a varying pain level and grade of muscular spasm. Since radiostereometry requires the invasive implantation of skeletal markers, conducted under general anesthesia, and would not for ethical reasons be possible in asymptomatic subjects, we studied patients scheduled for an external fixation test [13] due to a long-standing low back problem. On the other hand, the effects of these confounding factors were minimized by avoiding active spinal-mobility provocation, as in flexion-extension, and instead using a method with a positional change from supine to sitting [7]. This setup makes it possible to standardize the examinations, which is a prerequisite when comparing spinal mobility between individuals.
Our result in this RSA-based study, although in a rather limited number of discs, does bring support for a late stage of stabilization within the progressive, degenerative course for intervertebral kinematics, as proposed by Kirkaldy-Willis and Farfan [9]. This third stage of stabilization is revealed when the disc height is reduced by at least 50%, according to the mean mobility results given in Fig. 2 and Fig. 3. A preceding period of instability is not revealed by our findings, since the increase in mobility throughout the two earliest stages of disc degeneration, IB and II, is insignificant.
For the clinical situation, trying to deduce the intervertebral stability for the individual patient from the disc status by conventional radiography, as proposed by Kirkaldy-Willis and Farfan [9], our result clearly shows that the inter-individual differences are considerable for discs with the same degenerative status (Table 1). Thus, with the disc height reduced by 50%, the mobility was still 2–3 mm in the sagittal plane for some patients. According to this, for the patient with a significant disc-reduction grade III, the risk of developing a deformity or a progressive slip in a postoperative situation seems reduced but not eliminated.
Conclusion
The intervertebral mobility changes throughout the degenerative process, and a stage of stabilization is apparent when disc height is reduced by 50%. The segmental mobility status cannot be deduced from the radiographic, degenerative disc stage, because inter-individual differences in mobility are pronounced for the same disc status. A fully stable situation cannot be taken for granted, even when disc height is reduced by more than 50%, considering the fact that minor but persisting mobility was seen for most patients in that category. For this limited patient cohort, we could not verify the preceding stage of instability claimed by Kirkaldy-Willis and Farfan [9] in their three-stage theory for degeneration and in certain clinical situations proven by a resulting deformity.
Acknowledgements
This study was supported by grants from the Medical Faculty of the University of Lund, Stiftelsen för bistånd åt vanföra i Skåne, Stiftelsen Tornspiran, The Swedish Society of Medicine (Tryggers Fund) and The Swedish Medical Research Council
References
- 1.Axelsson Spine. 2000;25:1701. doi: 10.1097/00007632-200007010-00014. [DOI] [PubMed] [Google Scholar]
- 2.AxelssonEur Spine J 2003124112592546 [Google Scholar]
- 3.Danielson Acta Radiol. 1988;29:345. [PubMed] [Google Scholar]
- 4.Danielson Acta Radiol. 1989;30:65. [PubMed] [Google Scholar]
- 5.FribergSpine 1987121192954216 [Google Scholar]
- 6.JohnssonSpine 1990153472363063 [Google Scholar]
- 7.Johnsson R, Axelsson P, Strömqvist B (1997) Mobility provocation of the lumbar spine evaluated by RSA. Acta Orthop Scand [Suppl 274] 68:103–104
- 8.Johnsson Spine. 2002;27:2654. doi: 10.1097/00007632-200212010-00004. [DOI] [PubMed] [Google Scholar]
- 9.Kirkaldy-Willis Clin Orthop. 1982;165:110. [PubMed] [Google Scholar]
- 10.Knutsson Acta Radiol. 1944;25:593. [Google Scholar]
- 11.Macnab J Bone Joint Surg. 1971;53A:663. [PubMed] [Google Scholar]
- 12.Magerl Clin Orthop. 1984;189:125. [PubMed] [Google Scholar]
- 13.OlerudClin Orthop 1986203672937596 [Google Scholar]
- 14.Pitkänen Spine. 1997;22:193. doi: 10.1097/00007632-199701150-00012. [DOI] [PubMed] [Google Scholar]
- 15.SarasteSpine 1985102363992342 [Google Scholar]
- 16.Selvik Acta Orthop Scand Suppl. 1989;232:60. [PubMed] [Google Scholar]
- 17.Takayanagi Spine. 2001;26:1858. doi: 10.1097/00007632-200109010-00008. [DOI] [PubMed] [Google Scholar]