Abstract
We compared clinical outcomes following conservative treatment of subaxial fracture dislocations of the cervical spine and posterior fusion using bone grafts and interspinous Roger’s wiring (Bohlman modification). We reviewed 106 patients: 51 were treated primarily surgically, and 55 treated conservatively served as historical controls. Those patients who neurologically recovered at least one Frankel grade had on average less displacement on discharge (1.3 mm vs 3.1 mm, p=0.04). Although anatomical outcomes were better in the operatively treated group (1.6 mm vs 2.9 mm displacement at end of follow-up, p=0.001), there was no difference in neurological recovery. Late neck pain correlated with residual displacement (p=0.04) and was more common in the conservatively treated patients (p=0.01). Time in hospital was shorter in the group with posterior fusions, and complication rates were similar to those found after conservative treatment. A significant number of the conservatively treated patients developed kyphotic deformity, and 29% needed later surgery because of chronic instability or unacceptable anatomical results.
Keywords: Cervical spine trauma, Spine fractures, Fracture dislocation, Spinal surgery
Introduction
The treatment of fracture dislocations of the cervical spine still varies. Several reports on various treatment protocols have been published, but surprisingly few [3, 16] have compared their benefits and drawbacks. There is controversy as to whether conservative treatment would be sufficient or surgery always necessary [2, 8, 16]. In recent years, early operative treatment has gained increasing acceptance [1]. In our clinic, the approach changed in the late 1980s. Before 1988, most patients were primarily treated conservatively, using skull traction and halo vest. Surgical fusion was undertaken when conservative treatment failed to result in sufficient stabilization. Since 1988, most fractures have been treated by means of posterior fusion, using bone grafts and interspinous Roger’s wiring (Bohlman modification [4, 15]). Closed reduction by means of skull traction is accomplished prior to surgery. If necessary, open reduction is performed. The purpose of this study was to assess the benefits, problems and in vivo results of these two treatment protocols.
Materials and methods
Files of 106 patients who had been treated between 1977 and 1998 in Helsinki University Central Hospital were reviewed retrospectively. Each patient had sustained an unstable flexion-type subaxial fracture dislocation of the cervical spine, based on the instability criteria of White [22]: all anterior or posterior elements insufficient, more than 3.5 mm displacement, or more than 11° rotation difference to that of adjacent vertebra. Only posterior column fractures were included in the study, i.e., burst, compression or flexion-teardrop fractures were excluded. Only patients treated conservatively or by posterior fusion using bone grafts and interspinous Roger’s wiring (Bohlman triple wire modification [4, 15]) were included, i.e., patients who had primary anterior surgery or posterior stabilization by any other instrumentation were excluded. Patients were divided into two groups on the basis of treatment method used.
The surgically treated group consisted of 51 patients. After an initial reposition of dislocations by means of skull traction (mean duration, 4.2 days, anatomic realignment achieved in 27 out of 46 patients) or open posterior reduction of facet joints, stabilization was undertaken by means of bone grafting and interspinous wiring (Fig. 1). Forty-two (82%) patients had received surgery within 2 weeks and 34 (67%) of these received it in the first week. In 11 patients, the diagnosis was delayed more than 2 days (average 13 days). A Philadelphia collar (Camp Philadelphia, Cervical Collar, Westville, New Jersey, USA) had been worn for 90 days on average, after operation.
Fig. 1A–D.
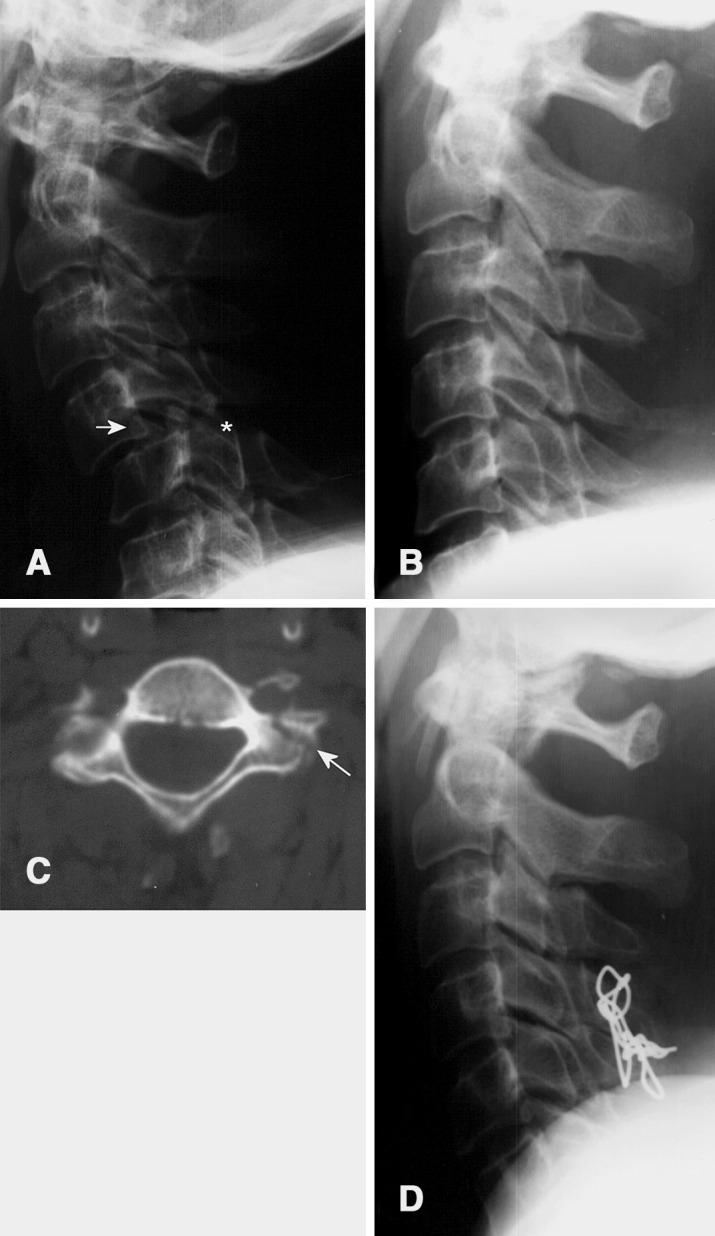
A 56-year-old man sustained an unstable C4/5 fracture dislocation in an automobile accident. A Lateral radiograph taken on admission reveals 11 mm C4/5 displacement, fracture of the tip of C5 spinous process, unilateral facet joint fracture luxation and contralateral subluxation. The upper part of the C5 superior articular process (arrow) is separated from the remainder of the articlar process (asterisk) indicating a fracture of the facet joint; B the fracture dislocation was successfully repositioned by skull traction; C left superior articular process fracture verified by CT (arrow); D since this flexion-type injury mainly compromises posterior column stability and there were no indications for disc removal, a posterior stabilization and fusion were performed by interspinous wiring and bone grafts tightened on both sides of the spinous processes
The historical control group of conservatively treated consisted of 55 patients. Thirty-nine of these patients were treated by means of skull traction (mean duration, 34 days, anatomic realignment achieved in 35 patients) followed by application of a Philadelphia collar (mean duration, 58 days). Nine conservatively treated patients had been treated by means of a halo vest (mean duration, 41 days) followed by application of a Philadelphia collar (for 46 days on average). In seven cases, Philadelphia-collar treatment (for an average of 84 days) had been considered sufficient. More than 2 days had elapsed from injury to diagnosis in seven cases (average 5 days).
No case was included in the study unless follow-up had lasted for 3 months or more and 6 months or more in the case of patients who had sustained spinal cord injury. The median follow-up was 11.9 months (3.1–41.2 months) in the operative treatment group and 12.4 months (3.2–111.8 months) in the conservatively treated (average 13.8 months and 24.0 months, respectively). Radiographs obtained on admission, on discharge and at the end of follow-up were reviewed. Displacement and kyphotic deformities were measured. To exclude the effects of radiographic magnification and size differences among patients, displacements were standardized for percentages of vertebral body sagittal diameters (% VBS). Neurological status was assessed by using Frankel’s classification [9]. Information relating to symptoms of radiculopathy were obtained from medical records. Demographic data, accompanying injuries and neurological status on admission are summarized in Table 1. The chi-square test was used in connection with statistical analysis of ratios, and the Mann–Whitney rank sum test in connection with statistical analysis of continuous nonparametric variables.
Table 1.
Demographic data, associated injuries and neurological status on admission
| Surgical treatment | Conservative treatment | |
|---|---|---|
| Patients (F:M) | 51 (11:40) | 55 (10:45) |
| Mean age, years (range) | 42.8 (16.3–80.7) | 43.2 (16.8–87.1) |
| Trauma, patients (%) | ||
| Motor vehicle accident | 28 (55%) | 23 (42%) |
| Fall | 7 (14%) | 10 (18%) |
| Fall from a height | 6 (12%) | 10 (18%) |
| Diving | 3 (6%) | 3 (5%) |
| Other | 7 (14%) | 9 (16%) |
| Sites of associated injury, patients | ||
| Head | 7 | 6 |
| Chest | 3 | 3 |
| Abdomen | - | - |
| Pelvis | 2 | - |
| Spine | 1 | 1 |
| Extremity | 6 | 10 |
| Multiple injuries | - | 1 |
| Injury level | ||
| C3/4 | 1 | 10 |
| C4/5 | 11 | 14 |
| C5/6 | 15 | 15 |
| C6/7 | 22 | 16 |
| C7/Th1 | 2 | - |
| Neurological status on admission, Frankel grade | ||
| A Complete motor and sensory loss | 4 | 7 |
| B Preserved sensation only | 3 | 3 |
| C Non-functional motor activity | 3 | 3 |
| D Functional motor activity | 3 | 6 |
| E Normal neurology below injury level | 38 | 36 |
| Radicular symptoms or findings | 24 | 21 |
Results
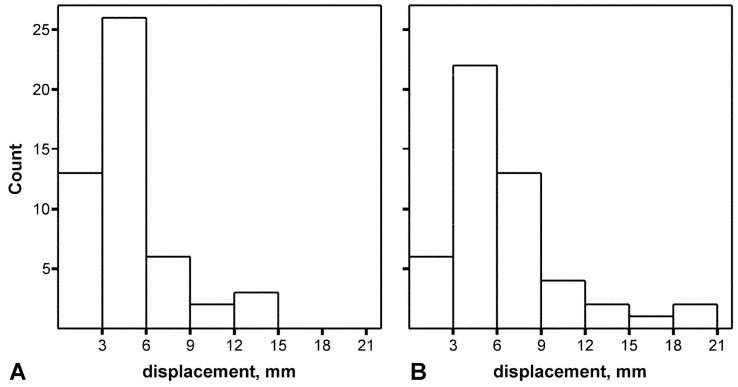
In 93 patients (90%), the dislocation was located between C4/5, C5/6 or C6/7 (Table 1). Facet dislocation had been bilateral in 21 of the surgically treated patients, unilateral in 30. Nineteen of the conservatively treated patients had suffered bilateral facet dislocation, 36 unilateral. Multiple fractures were common. Seventeen of the surgically treated patients and 18 of the conservatively treated patients had two or more fractured vertebrae. Thirty-eight of the surgically treated patients and 32 of the conservatively treated patients had fractures of the spinous process or laminae. There were articular-process fractures in 22 of the surgically treated patients and in 35 of the conservatively treated patients. On admission, the surgically treated patients exhibited 7.0 mm (SD 4.1 mm) displacement (30% VBS) on average (Fig. 2). In the conservatively treated patients, the average displacement was 5.6 mm (SD 3.8 mm) (24% VBS). Twenty-one of the surgically treated patients and 23 of the conservatively treated patients exhibited more than 5°of kyphotic deformity (averages, 17° and 10°, respectively). Lordotic deformity of more than 5° occurred in seven surgically treated patients (average, 11°) and 12 conservatively treated patients (average, 12°).
Fig. 2A, B.
Amount of displacement on admission. A In the group of conservatively treated patients; B in the surgical group
Six of the surgically treated patients required a second operation because of residual instability (0 days, 3 days, 6 days, 41 days, 88 days and 245 days, respectively, after the first operation). One of them had disc extrusion, which could have caused medullary impingement, necessitating anterior discectomy. Sixteen (29%) of the conservatively treated patients were subjected to late surgical stabilization because of instability, progression of neurological symptoms or an unacceptable anatomical result (average 54 days (SD 40 days) after the trauma and one case 6.5 years following trauma). One of these patients had medullary impingement caused by disc material. The average length of primary stay in hospital was 27 days (SD 25 days) in the surgical treatment group (Frankel grade-E patients, 18 days, Frankel grades A–D patients, 56 days), 53 days (SD 50 days) in the conservatively treated patients (Frankel grade-E patients, 38 days, Frankel grades A–D patients, 84 days).
Two of the surgically treated patients died in hospital, one from myocardial infarction 8 days after trauma (a 69-year-old man, Frankel grade E, on the third day after operation), one from cerebral infarction 19 days after trauma (a 20-year-old man, Frankel grade A, on the 19th day after operation). Three of the conservatively treated patients died, one from respiratory insufficiency 1 day after trauma (an 84-year-old man, Frankel grade A, injured at C3/4), one from pneumonia 8 days after trauma (an 87-year-old man, Frankel grade C) and one from pulmonary embolism 18 days after trauma (a 71-year-old man, Frankel grade A). Complications are summarized in Table 2.
Table 2.
Complications during hospitalization and follow-up
| Surgical treatment | Conservative treatment | |||
|---|---|---|---|---|
| Frankel grade A to D | Frankel grade E | Frankel grade A to D | Frankel grade E | |
| During hospital treatmenta | ||||
| Patients (patient years, py) | 13 (1.89 py) | 38 (1.87 py) | 19 (3.78 py) | 36 (3.77 py) |
| Respiratory complications | 4 (2.1/py) | 3 (1.6/py) | 6 (1.6/py) | 2 (0.5/py) |
| Cardiac complications | 1 (0.5/py) | 2 (1.1/py) | 2 (0.5/py) | - |
| Cerebral infarction | 1 (0.5/py) | - | - | - |
| Deep vein thrombosis | - | 1 (0.5/py) | 3 (0.8/py) | 2 (0.5/py) |
| Pulmonary embolism | - | - | 1 (0.3/py) | 1 (0.3/py) |
| Urinary tract infection | 4 (2.1/py) | - | 4 (1.1/py) | - |
| Gastrointestinal complications | 1 (0.5/py) | - | 2 (0.5/py) | 1 (0.3/py) |
| Decubitus ulcer | - | - | 1 (0.3/py) | - |
| Recurrent nerve injury | - | - | 1 (0.3/py) | - |
| Pulmonary air embolism | - | 1 (0.5/py) | - | - |
| Surgical infection | - | 2 (1.1/py) | - | 2 (0.5/py) |
| Loosening of pins | - | - | - | 2 (0.5/py) |
| Disturbance of swallowing | - | 2 (1.1/py) | - | - |
| During follow-upb | ||||
| Patients (patient years, py) | 12 (12.7 py) | 37 (38.9 py) | 16 (40.2 py) | 36 (55.1 py) |
| Urinary tract infection | 3 (0.24/py) | 2 (0.05/py) | 2 (0.05/py) | - |
| Cerebral infarction | - | 1 (0.03/py) | - | - |
| Decubitus ulcer | 2 (0.16/py) | - | 1 (0.02/py) | - |
| Surgical infection | - | 1 (0.03/py) | - | 1 (0.02/py) |
aCalculated from admission to discharge
bCalculated from discharge to end of follow-up
Neurological outcomes in the patients with spinal cord injury are shown in Table 3. In the surgically treatment group nine of the 12 spinal cord injured patients recovered by at least one Frankel grade. Ten of the 16 conservatively treated patients of this kind improved by at least one grade (p=0.8, chi-square test) but one patient deteriorated. Methylprednisolone had been given to two patients with spinal cord injury who were treated surgically. One improved from Frankel grade A to Frankel grade B, the other from Frankel grade B to Frankel grade D. On admission, 24 of the surgically treated Frankel E patients and 21 of the conservatively treated Frankel E patients exhibited radicular symptoms at the injury level. At the end of follow-up, radicular symptoms persisted in ten and four of these patients (p=0.2, chi-square test), respectively. These numbers include those patients, who had persisting radicular symptoms after late surgery, but not those patients who had radicular symptoms cured by late surgery during follow-up. Five patients without radicular symptoms or findings on admission exhibited radicular symptoms at the end of follow-up. Two had been in the surgical treatment group, three in the conservative treatment group. At the end of follow-up, four surgically treated patients (mean duration of follow-up, 13.4 months, SD 1.8 months) and 14 conservatively treated patients (mean duration of follow-up, 26.2 months, SD 29.8 months) were suffering from persistent neck pain (p=0.01, chi-square test). A correlation between late neck pain and displacement on discharge was found (2.8 mm in symptomatic patients vs 1.9 mm in non-symptomatic patients, p=0.04, Mann–Whitney test). The correlation between late neck pain and displacement at the end of follow-up was statistically not significant (2.6 mm versus 2.2 mm, p=0.2, Mann–Whitney test). There was no significant correlation between kyphotic deformity and late neck pain.
Table 3.
Neurological status on admission and at end of follow-up
| On admission, Frankel grade | At end of follow-up, Frankel grade | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Surgical treatment | Conservative treatment | |||||||||
| A | B | C | D | E | A | B | C | D | E | |
| A | 1 | 1 | 1 | - | - | 4 | - | - | 1 | - |
| B | - | 1 | 1 | 1 | - | 1 | - | 2 | - | - |
| C | - | - | - | 1 | 2 | - | - | - | - | 2 |
| D | - | - | - | 1 | 2 | - | - | - | 1 | 5 |
| E | - | - | - | - | 37 | - | - | - | - | 36 |
At discharge from the hospital, patients in the surgical and conservative treatment groups exhibited on average 1.5 mm (SD 1.6 mm) (7.1% VBS) and 2.6 mm (SD 2.1 mm) (11.3% VBS) displacement, respectively (p=0.004, Mann–Whitney test). At the end of follow-up, the displacement in surgically treated patients was 1.6 mm (SD 1.6 mm) (7.9% VBS) on average. In conservatively treated patients, the average displacement was 3.0 mm (SD 2.2 mm) (13.0% VBS) (p=0.001), including 16 patients who underwent late surgical stabilization. If these 16 patients and the surgically treated patients who underwent a second operation are excluded, the average displacement at the end of follow-up is 1.6 mm (SD 1.7 mm) (7.7% VBS) in the surgically treated patients, and 2.9 mm (SD 2.2 mm) (13.1% VBS) in the conservatively treated patients (p=0.006). The 16 conservatively treated patients who underwent late surgical stabilization had on average a 5.1 mm (SD 2.1 mm) re-dislocation and 13° (SD 6°) kyphotic deformity.
Patients with spinal cord injury who recovered by at least one Frankel grade had on average less displacement on admission (6.9 mm (SD 4.7 mm), 28.4% VBS, both treatment groups included) than those who did not improve (11.8 mm (SD 6.6 mm), 49.3% VBS, both groups included, p=0.08). Patients with spinal cord injury who showed improvement in Frankel grading by the end of follow-up had on average exhibited less displacement on discharge (1.3 mm, SD 1.5 mm; 6.5% VBS) than patients with spinal cord injury whose Frankel grading had not improved by the end of follow-up (3.1 mm, SD 2.5 mm; 13.1% VBS, p=0.04). The correlation between neurological recovery and displacement at end of the follow-up is statistically not significant (1.6 mm, SD 1.8 mm, vs 2.7 mm, SD 2.1 mm, p=0.3). For surgically treated patients, the statistics are 0.6 mm vs 2.1 mm displacement (p=0.1) on discharge, and 1.1 mm vs 0 mm displacement (p=0.5) at the end of follow-up. For the conservatively treated patients, the statistics are 2.0 mm vs 3.5 mm displacement (p=0.3) on discharge, and 2.2 mm vs 3.2 mm displacement (p=0.4) at the end of follow-up.
At the end of follow-up, 5° or more of kyphotic deformity was observed in 14 patients in the surgical group (range 5–26°, average 14°; SD 5.9°), and in 25 conservatively treated patients (range 5–47°, average 13°; SD 9.3°). Lordotic deformity of 5° or more was observed in 13 surgically treated patients (range 5–23°, average 11°; SD 4.8°) and eight conservatively treated patients (range 5–18°, average 10°; SD 4.2°), including the 16 patients who had been subjected to late surgical stabilization. Of the 36 conservatively treated patients who did not have late surgical fusion, 20 developed kyphotic and five developed lordotic deformity.
Discussion
Fracture dislocations of the cervical spine cause a heterogeneous group of injuries ranging from ligamentous insufficiency to unstable fracture, involving both posterior and anterior structures in the spinal column. Both spinal cord and root injuries are common. Spinal cord and root injuries associated with fracture dislocation have been treated successfully using a number of different methods. The question is to what extent the observed neurological recovery is a natural outcome of this disorder. Our findings indicate that perfect reduction of fracture dislocation correlates to some extent with neurological recovery. According to the patient data in our study, results following posterior fusion using interspinous wiring were anatomically better than results following conservative treatment. However, our findings suggest that this method used for stabilization does not per se warrant neurological recovery in patients with fracture dislocation. Neurological outcomes were very similar in both surgically and conservatively treated patients. Why is this? Evidence from animal models suggests that the severity of a spinal cord injury depends both on the force of the initial impact and persisting spinal cord compression [8, 11]. Therefore, it could hypothetically be that, in patients with fracture dislocation, it is the force of the initial impact that mainly determines the outcome. In the data we studied, the degree of displacement on admission did not correlate statistically significantly with outcome, although a weak association was found. To our knowledge, no study has been conducted to determine whether post-injury radiographic deformity correlates with occlusion of the spinal canal during impact in fracture dislocations of the cervical spine. In an experimental study Chang et al. [6] demonstrated that, in burst fractures, post-injury radiographs underestimated and correlated poorly with the severity of spinal canal occlusion during impact.
As a significant part of the instability in fracture dislocations is caused by posterior column disruptions, the most logical solution in these injuries is restoration of the posterior column integrity. Interspinous wiring is, however, ineffective in multiple, contiguous spinous-process or laminar fractures. In Bohlman triple-wire technique, with bone grafts and an interspinous tension band construct, bone quality and wires cutting through the spinous processes are thought to be less of a problem than in conventional Roger’s wiring. Interspinous cervical fusion is generally safer than posterior sublaminar techniques, as the spinal canal is not unnecessarily entered. It is also technically less demanding than anterior approaches or posterior lateral mass plating. The posterior approach allows, when necessary, a relatively safe open reduction of facet joints—which can be difficult, or occasionally impossible, by using anterior techniques. In biomechanical testing, posterior triple-wire fixation has provided posterior column stability comparable with lateral mass plating [15]. The type of surgery, anterior or posterior, not only depends on the direction of instability and type of fracture, but is also influenced by spinal canal compromise with bone fragments, epidural hematoma or herniated disc material. Traumatically herniated disc material causing medullary compression [7, 14], either before or after reduction, is a probable confounding factor in a retrospective study setting of this kind. Most of the cases in this series were treated before the era of MRI. The incidence of posteriorly herniated disc material is high [21] in facet dislocations.
Neurological deterioration, due to posteriorly herniated disc material causing medullary impingement at the moment of vertebral reduction, is a rare [10, 20], but feared, complication. With the evolution of MRI, herniated disc material can be identified and complications of this kind avoided by choosing anterior surgery. On the other hand, imaging takes time and, especially in cord compression, time could be a critical factor. Should these patients undergo MRI scanning prior to reduction? This is a controversial topic [1, 13, 17]. We agree with Hart and Vaccaro [13], who state that patients with complete or nearly complete cord injuries attributable to bony narrowing of the spinal canal have little to lose and the most to gain, and should undergo immediate closed repositioning prior to MRI. In our opinion, patients with less severe neurological symptoms should also be imaged by MRI, either before or after skull traction has been applied. The decision as to whether skull traction is applied prior to MRI should be based on the severity and progression of the neurological symptoms and on the degree that these symptoms can be attributed to bony encroachment of the spinal canal. In other words, what will harm the patient more—the delay caused by imaging or the risk of additional cord compression by disc material? The current literature does not provide enough information to solve this dilemma. Emergent decompression using skull traction is supported by results from animal studies, where neurological recovery has correlated with early decompression, ranging from minutes to a few hours after the impact.[8] Until recently, fracture dislocations in neurologically intact, awake patients have been repositioned in our clinic by skull traction under close neurological monitoring. If any signs of neurological deterioration occurred, urgent MRI was performed followed by discectomy and anterior fusion, when necessary. Today, a more cautious approach, with MRI prior to repositioning, is used increasingly often in our clinic. In dislocations irreducible by skull traction, MRI should be done prior to anesthesia and open reduction. In our opinion, the indications and timing for radiological investigations, more specifically MRI, require further study. According to Hadley [12], cervical spine facet luxation without apparent fracture does not respond well to conservative treatment. We think that such injuries should be studied separately from fracture dislocations.
The beneficial effects of methylprednisolone treatment in spinal cord injuries have been demonstrated by Bracken [5], although the safety of such treatment is questionable [19]. Two of the patients whose data we studied received methylprednisolone treatment. We restricted our data to the mid-1990s, as an increasing proportion of corticosteroid-treated patients probably would have introduced unwanted bias. Pettersson [18] showed that methylprednisolone treatment helped prevent whiplash-associated disorder (WAD).
Incidences of complications in surgically and conservatively treated patients were similar. Conservative treatment had clear disadvantages, however. The average stay in hospital was longer. Late deformities and instability were very common in the conservatively treated patients, and almost one-third (29%) had to undergo late surgical stabilization. Beyer [3] concluded that non-anatomical reduction and residual cervical translation are associated with late neck pain and stiffness. We also found a correlation between incidence of late neck pain and extent of residual displacement. Conservative treatment also correlated strongly with occurrence of chronic neck pain.
We conclude that, in our clinic, the transition from conservative treatment to surgical stabilization using bone grafting and interspinous Roger’s wiring resulted in better anatomic end results, with complication rates as low as with conservative treatment methods. Appropriate reduction of fracture dislocations correlated with neurological recovery in spinal-cord-injured patients, although surgical stabilization by this method per se does not seem to affect the neurological outcome. Late neck pain is correlated with residual displacement, and it was more common in conservatively treated patients. The briefer periods of hospitalization required by surgically treated patients allow rehabilitation to be started earlier than in conservatively treated patients.
References
- 1.Allred Spine. 2001;26:1927. doi: 10.1097/00007632-200109010-00021. [DOI] [PubMed] [Google Scholar]
- 2.Beyer Orthopedics. 1992;15:311. doi: 10.3928/0147-7447-19920301-08. [DOI] [PubMed] [Google Scholar]
- 3.Beyer J Bone Joint Surg Br. 1991;73B:977. doi: 10.1302/0301-620X.73B6.1955448. [DOI] [PubMed] [Google Scholar]
- 4.Bohlman J Bone Joint Surg Am. 1979;61A:1119. [PubMed] [Google Scholar]
- 5.BrackenJ Neurosurg 199276231727165 [Google Scholar]
- 6.Chang Spine. 1994;19:973. doi: 10.1097/00007632-199404150-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eismont J Bone Joint Surg Am. 1991;73A:1555. [PubMed] [Google Scholar]
- 8.Fehlings Spine. 2001;26:S101. doi: 10.1097/00007632-200112151-00017. [DOI] [PubMed] [Google Scholar]
- 9.FrankelParaplegia 196971795360915 [Google Scholar]
- 10.Grant GA, Mirza SK, Chapman JR, Winn HR, Newell DW, Jones DT, Grady MS (1999) Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg 90 [Suppl 1]:13–18 [DOI] [PubMed]
- 11.Guha Paraplegia. 1987;25:324. doi: 10.1038/sc.1987.61. [DOI] [PubMed] [Google Scholar]
- 12.Hadley Neurosurgery. 1992;30:661. [PubMed] [Google Scholar]
- 13.Hart Spine. 2002;27:116. doi: 10.1097/00007632-200201010-00030. [DOI] [PubMed] [Google Scholar]
- 14.Harrington Neurosurgery. 1991;29:374. doi: 10.1097/00006123-199109000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Hisanori Spine. 2001;26:1662. doi: 10.1097/00007632-200108010-00007. [DOI] [PubMed] [Google Scholar]
- 16.Lee J Bone Joint Surg Br. 1994;76B:352. [PubMed] [Google Scholar]
- 17.Nockels Spine. 2001;26:S31. doi: 10.1097/00007632-200112151-00007. [DOI] [PubMed] [Google Scholar]
- 18.Pettersson Spine. 1998;23:984. doi: 10.1097/00007632-199805010-00004. [DOI] [PubMed] [Google Scholar]
- 19.Short Spinal Cord. 2000;38:273. doi: 10.1038/sj.sc.3100986. [DOI] [PubMed] [Google Scholar]
- 20.Vaccaro Spine. 1999;24:1210. doi: 10.1097/00007632-199906150-00007. [DOI] [PubMed] [Google Scholar]
- 21.Vaccaro Spine. 2001;26:1866. doi: 10.1097/00007632-200109010-00009. [DOI] [PubMed] [Google Scholar]
- 22.White Clin. 1975;Orthop:85. doi: 10.1097/00003086-197506000-00011. [DOI] [PubMed] [Google Scholar]