Abstract
There are many definitions and classifications of chronic neck pain and of neck pain following whiplash injury, many of them developed for a single study. This study compares three different outcome measures (neck disability index, Gargan and Bannister grade, general health questionnaire) in 277 patients who were examined for medicolegal reporting following isolated whiplash injury. There is significant correlation between the physical outcome scales and also between the physical and psychological outcome scales examined (both p <0.01). Definitions of chronic neck pain (with or without whiplash injury) and measures to assess and classify patients with chronic symptoms are reviewed. We recommend the use of a simple self-administered questionnaire that does not require physical measurement as the most useful tool in the evaluation of these patients and the most accurate method of classifying outcome.
Keywords: Whiplash, Cervical spine, Outcome measure, Prognosis
Introduction
With the advent of clinical guidelines, evidence-based practice and systematic review, the methods by which illness, injury and treatment interventions are evaluated have come under increased scrutiny. Conditions require a validated assessment measure that is reliable, relevant, responsive, acceptable to patients, and as easily applicable to routine practice settings as to research trials. The measure needs to be standardised, and its use needs to be widespread to allow the comparison of data from different studies.
There is a remarkable heterogeneity of definitions and classifications of all clinical aspects related to neck pain and whiplash injury, many of them developed for a single study and not fully validated. The poor understanding of pathogenesis, lack of objective signs and variable course followed by many patients suffering whiplash injury may have contributed to this. There is a paucity of trials on patients with neck pain when compared with low back pain, where there are a number of measures that are used in routine practice (eg Oswestry low back pain and disability questionnaire [7], Rowland disability scale [27], Waddell disability index [34], Million index [24, 25]).
There are problems in evaluating the severity of neck pain and related symptoms, both in the general population [3, 4, 20, 22], and in those suffering from whiplash [21, 32]. Clinical findings do not correlate well with subjective symptoms [18, 34], and radiographic [31] and MRI examination [28] can be inconclusive. As pain is the predominant symptom, assessment (and therefore the design of an outcome measure) is difficult due to the varied input of physical, psychological, social and emotional factors. The interplay between these factors is well established in low back pain [19], with a similar complex relationship in neck pain following whiplash injury.
The aim of this study was to review the suitability of measures available for assessing neck pain, and to compare three different outcome measures in a large group of patients presenting for medicolegal reporting following isolated whiplash injury.
Materials and methods
Reports of 277 patients with isolated whiplash injuries examined for medicolegal reporting (by the senior author) between 9 months and 5 years after injury (average 21 months) were analysed. The outcome following whiplash injury was assessed using three scoring systems.
The neck disability index (NDI) [32] is a validated scoring system for functional outcome, derived from the Oswestry low back pain disability questionnaire [7]. It combines pain and disability in a self-administered 10-item questionnaire with a maximum score of 50. Results are doubled to create a percentage (0% normal, 100% maximum disability in every category). All reports contained a record of the NDI.
The scaled version of the general health questionnaire (GHQ) [12] is a self-administered screening questionnaire designed for use in consulting situations to detect psychiatric disorder. It has 28 questions in four subscales that cover somatic symptoms, anxiety and insomnia, social dysfunction and severe depression. The clinician scores the questionnaire (using the 0–0-1–1 scoring method described by Goldberg and Hillier) to give a result between 0 (normal) and 28. A threshold score of 5/6 is 80% sensitive and 89% specific for a diagnosable psychiatric disorder. The questionnaire is printed on coloured paper, which is more acceptable to patients. All reports contained a record of the GHQ.
The Gargan and Bannister grade (GBG) [10] is a simple, reproducible, validated classification based on the severity of symptoms. The GBG was not recorded in the original report, but was derived from the symptoms recorded. Blind repeat testing was performed to validate the method of grade allocation. For ease of analysis, the GBG was recorded as 1–4 rather than the original A–D.
Statistics
Statistical analysis was performed using SPSS. The associations between the outcome measures were assessed using Spearman’s rank correlation coefficient (Spearman’s rho) for non-parametric data, as one of the scoring systems records ordinal data (GBG), and the others are not normally distributed. The significance of any association was determined using a two-tailed t -test.
Results
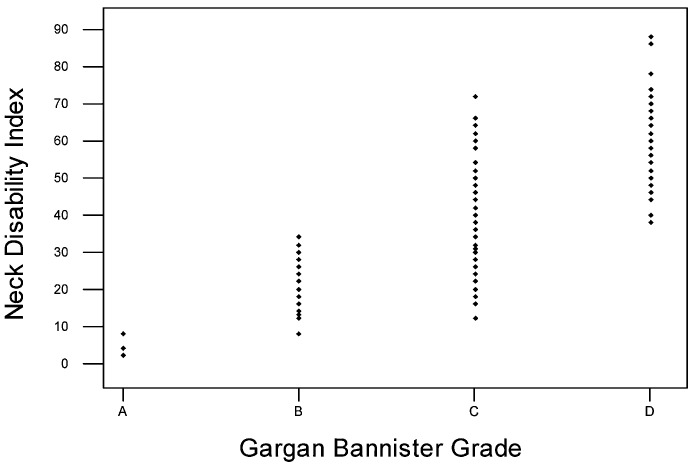
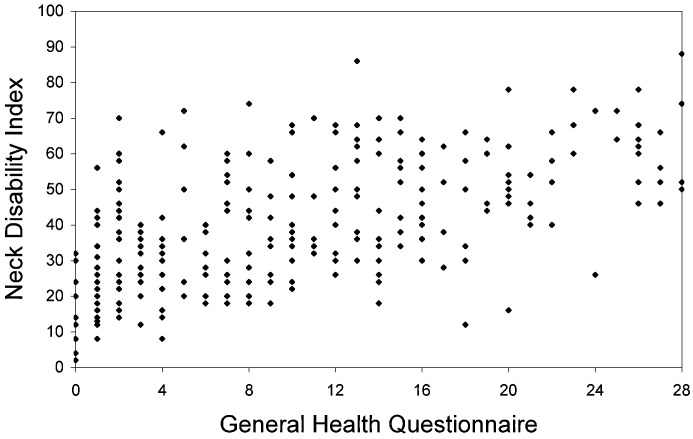
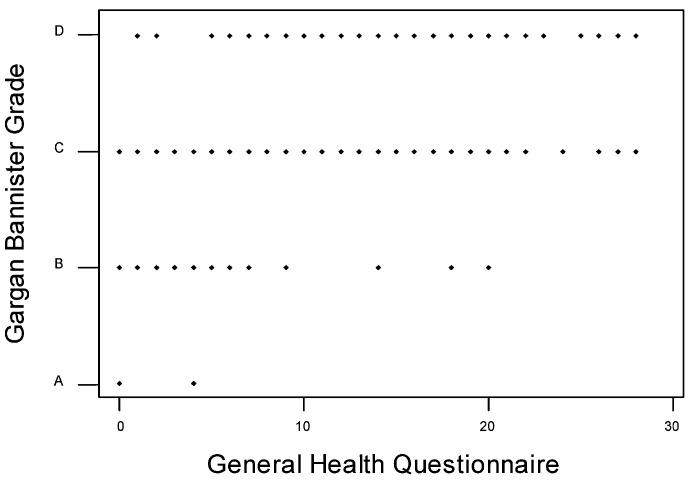
The mean and standard deviation of the three measures is shown in Table 1. There is a highly significant association between the physical outcome scales (Table 2, Fig. 1) and also between the physical and psychological outcome scales (Table 2, Figs. 2, 3).
Table 1.
Descriptive statistics
| Outcome measure | Mean | SD |
|---|---|---|
| NDI (%) | 39.9 | 17.8 |
| GBG (1–4) | 3.1 | 0.7 |
| GHQ (0–28) | 10.0 | 8.0 |
Table 2.
Correlation of outcome measures
| Outcome measures compared | Spearman’s rho | P value |
|---|---|---|
| NDI and GBG (Fig. 1) | 0.72 | <0.01 |
| NDI and GHQ (Fig. 2) | 0.58 | <0.01 |
| GBG and GHQ (Fig. 3) | 0.50 | <0.01 |
Fig. 1.
Correlation of NDI and GBG
Fig. 2.
Correlation of NDI and GHQ
Fig. 3.
Correlation of GBG and GHQ
Discussion
This study involves a large cohort of patients who are pursuing compensation following isolated whiplash injury. This is clearly a selected group, biased towards those with poor outcome, but this does not prevent the comparison of different methods of outcome assessment.
The results demonstrate a significant association between these three outcome measures, each very different in design. It is not possible using Spearman’s rho to determine the proportion of the variability that is attributable to the relationship. The closest association occurs between the two measures that concentrate on the physical features of the disorder (NDI and GBG). The highly significant associations between these physical measures and the GHQ are harder to explain.
Studies of the various back pain disability scales have demonstrated similar correlations between measures of pain and physical function and measures of emotional and cognitive function, with coefficients between 0.3 and 0.7 [19]. While it is recognised that there is poor understanding of the physical basis for the symptoms associated with whiplash injury, it is apparent that in many cases there is a non-organic element. There is conflicting evidence in the literature as to whether the pain and disability adversely affect the psychological state of the patient, or whether pre-existing psychological stress increases restriction in activity or biases the reporting of disability.
Gargan et al. [11] showed that a secondary psychological disorder followed whiplash injury that did not remit within two years and Squires et al. [30] showed that this persisted after 15 years, but a history of psychological or anxiety disorder prior to injury is also strongly associated with poor outcome [13]. Van der Donk et al. [31] showed that neuroticism is a more powerful determinant of neck pain than radiological signs of disc degeneration or osteoarthritis in the general population. It is likely that this association following whiplash injury is the result of a combination of primary and secondary effects.
When assessing outcome after whiplash injury, it is important to consider the presence (and definition) of chronic neck pain in the general population. This is a frequent symptom, particularly in women [3, 4, 20, 22] and is an important cause of sickness absenteeism [6]. The definition of chronic neck pain is inevitably arbitrary and often vague.
Lawrence [20] found that neck and shoulder pain was present in 9% of males and 12% of females in the UK. Three times this number reported symptoms at some time in the past. Bovim et al. [3] defined chronic neck pain as “troublesome neck pain for more than 6 months of the previous year”. In 7,500 Norwegian adults selected randomly from the general population, 13.8% of respondents (10% of males, 17% of females) fell into this group. The gender difference was significant, and there was a significant increase with age in both sexes, so that more than 25% of females over 50 years old reported chronic neck pain. This broad definition fails to distinguish accurately between trivial and disabling conditions.
Makela et al. [22] defined “chronic neck syndrome” if there was a convincing history of severe longstanding neck pain that had manifested symptoms in the last month, a documented history of previously diagnosed neck syndrome with objective signs on examination, or mild or moderate neck pain with objective signs at examination. Out of 7,217 Finnish adults from the general population, 9.5% of men and 13.5% of women fell into this definition. A history of injury to the back, neck or shoulder was strongly associated with the syndrome. Industrial or agricultural employment, obesity and smoking had significant association. Mental stress at work was more closely associated than physical stress. Current neck pain of short duration was not considered a “neck syndrome”. Intra-observer reliability was good, but there was considerable variation between examiners due to a substantial difference in the diagnostic threshold.
Cote et al. [4] used the chronic pain questionnaire [33] to stratify pain subjects into subgroups with varying levels of pain severity, duration and dysfunctional behaviour. They found a lifetime prevalence of neck pain in Saskatchewan adults of 67%, and a 6 month prevalence ranging from 39% for low intensity, low disability neck pain to 5% for severely limiting, intense disabling pain.
Considering the frequent occurrence of chronic neck pain in the general population and the difficulty in defining its severity, it is no surprise that the classification of outcome following whiplash injury is both difficult and controversial.
A variety of assessment tools have been developed for use in patients that have suffered whiplash injury, subsequent to the measures used in this study [2, 18, 21, 26, 29, 35]. Many of these involve self-assessment questionnaires, which are a convenient and reproducible measure of subjective symptoms. Self-report is the only reliable method of pain measurement [17]. The measures vary widely, from those that cover all the complex aspects of the complaint but may be impractical for common use, to those that are simple and easy to use (by patients and clinicians) but may underestimate the breadth of symptoms and functional impairment, compromising validity and reliability.
All the measurement tools include a measure of pain—the predominant symptom for most patients. Physical impairment and resulting disability (which are related to pain, but not strongly correlated [34]) are an important consideration, and are usually included. Psychological, social and emotional well-being and quality of life can also be measured by questionnaire.
Many of the published scoring systems are remarkably similar. Parmar and Raymakers [26] produced a simple scoring system based on symptoms (scored 0–3) that is almost identical to the Gargan and Bannister grade [10] (scored A–D). Leak et al. [21] adapted the Oswestry disability questionnaire [7] in a similar fashion to the NDI [32], to produce the Northwick Park neck pain questionnaire (NPQ). It also contains 10 five-part questions, and is scored as a percentage. It has no features that make its use preferable to the NDI, which was developed first.
The Quebec task force [29] attempted to “propose definitions and classifications that would facilitate evaluation of research and be helpful to the clinician”. The group produced a complex definition of whiplash injury and whiplash associated disorders (WAD), and classified patients into 5 groups at clinical presentation based on a mixture of symptoms and signs (Table 3).
Table 3.
Quebec task force classification of whiplash-associated disorders
| Score | Symptoms and signs |
|---|---|
| 0 | No symptoms or signs |
| 1 | Pain, stiffness or tenderness, with no objective physical signs |
| 2 | Neck complaint and musculo-skeletal signs (point tenderness, decreased range of movement) |
| 3 | Neck complaint and neurological signs (decreased or absent reflexes, weakness, sensory deficits) |
| 4 | Neck complaint and fracture or dislocation |
The task force limited itself to patients in groups 1–3. The group definitions are simple to apply, but the combining of symptoms and signs raises questions of validity [9]. The subjects studied were from a selected subpopulation, no formal assessment of recovery was made and unsubstantiated conclusions were reached [8]. However, one study has shown that the classification has prognostic value and recommends its routine use [15], and the task force definitions are found throughout the whiplash literature [14].
Wheeler et al. [35] published the neck pain and disability scale (NPDS), designed from the Million visual analogue scale [24, 25]. It has 20 items on a self-assessment questionnaire that has been validated, and has been shown to correlate well with other physical (ODQ, pain disability index) and psychological (Beck depression inventory) scales, confirming the association between psychological symptoms and the patient’s perception and report of pain and disability. The NPDS is valid, simple to use, does not require physical measurements, and is sensitive to pain intensity.
Jordan et al. [18] produced a more complex but highly consistent Copenhagen neck functional disability scale, which includes a self-assessment questionnaire, a doctor’s global assessment of function and neck status, and separate scores for neck pain and arm pain. It does not include questions on psychological status.
Bolton and Humphreys [2] developed the Bournemouth questionnaire from a back pain index [1] used in chiropractic outpatient clinics for use in patients with non-specific neck pain. This self-assessment questionnaire is the only one to include separate pre- and post-treatment sections. It has numerical rating scales that cover pain, its effect on functional and social activity, depression, anxiety and coping ability. The instrument has been shown to be reliable, valid and responsive.
The results from this study and Wheeler et al. [35] show that there is overlap between assessment tools, even those that concentrate purely on physical (GBG) or psychological (GHQ) symptoms. Symptoms are the most prominent feature in mechanical neck pain caused by whiplash injury, and correlate well with outcome, unlike measurements of movement and other physical signs which are weakly correlated with pain and disability and do not predict outcome accurately [10, 16, 18, 23]. We believe that a simple self-administered questionnaire (not requiring physical measurement) that concentrates on physical symptoms and their effect on work and leisure activities and psychological well-being is the most useful tool in the evaluation of these patients and allows the most accurate classification of outcome.
Deyo et al. have proposed a similar standardisation for low back pain outcome measurement [5]. Having considered many available instruments, they produced a core set of six questions for use in routine care settings, again concentrating on symptoms and their effect, with an expanded outcome set for more precise measurement in research settings.
Given the multitude of measurement tools already available, it is unlikely that development of further scales will provide any advance in the assessment of whiplash injury.
Footnotes
No financial assistance was required to complete this study
References
- 1.Bolton J Manipulative Physiol Ther. 1999;22:503. doi: 10.1016/s0161-4754(99)70001-1. [DOI] [PubMed] [Google Scholar]
- 2.Bolton J Manipulative Physiol Ther. 2002;25:141. doi: 10.1067/mmt.2002.123333. [DOI] [PubMed] [Google Scholar]
- 3.Bovim Spine. 1994;19:1307. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Cote Spine. 1998;23:1689. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 5.Deyo Spine. 1998;23:2003. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 6.Dimberg Scand J Soc Med. 1989;17:77. doi: 10.1177/140349488901700112. [DOI] [PubMed] [Google Scholar]
- 7.Fairbank Physiotherapy. 1980;66:271. [PubMed] [Google Scholar]
- 8.Freeman MD, Croft AC (1998) The controversy over late whiplash: are chronic symptoms after whiplash real? In: Gunzburg R, Szpalski M (eds) Whiplash injuries: current concepts in prevention, diagnosis and treatment of the cervical whiplash syndrome, Lippincott, Williams and Wilkins, pp 161–165
- 9.Freeman Spine. 1998;23:1043. doi: 10.1097/00007632-199805010-00015. [DOI] [PubMed] [Google Scholar]
- 10.Gargan J Bone Joint Surg Br. 1990;72B:901. doi: 10.1302/0301-620X.72B5.2211780. [DOI] [PubMed] [Google Scholar]
- 11.Gargan J Bone Joint Surg Br. 1997;79B:523. doi: 10.1302/0301-620X.79B4.6940. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg Psychol Med. 1979;9:139. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 13.Gozzard J Bone Joint Surg Br. 2001;83B:506. doi: 10.1302/0301-620X.83B4.11228. [DOI] [PubMed] [Google Scholar]
- 14.Gunzburg Whiplash. 1998;injuries:current. [Google Scholar]
- 15.Hartling Spine. 2001;26:36. doi: 10.1097/00007632-200101010-00008. [DOI] [PubMed] [Google Scholar]
- 16.Hohl J Bone Joint Surg Br. 1974;56A:1675. [PubMed] [Google Scholar]
- 17.Jadad AR, McQuay HJ (1993) The measurement of pain. In: Pynsent P, Fairbank J, Carr A (eds) Outcome measures in orthopaedics and trauma, chapter 2, Butterworth Heinemann
- 18.Jordan J Manipulative Physiol Ther. 1998;21:520. [PubMed] [Google Scholar]
- 19.Kopec Spine. 1995;20:1943. doi: 10.1097/00007632-199509000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Lawrence Ann Rheum Dis. 1969;28:121. doi: 10.1136/ard.28.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leak Br J Rheumatol. 1994;33:469. doi: 10.1093/rheumatology/33.5.469. [DOI] [PubMed] [Google Scholar]
- 22.Makela Am J Epidemiol. 1991;134:1356. doi: 10.1093/oxfordjournals.aje.a116038. [DOI] [PubMed] [Google Scholar]
- 23.McKinneyBr Med J 198929910062511939 [Google Scholar]
- 24.Million Ann Rheum Dis. 1981;40:449. doi: 10.1136/ard.40.5.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MillionSpine 198272046214028 [Google Scholar]
- 26.ParmarInjury 199324758505130 [Google Scholar]
- 27.RowlandSpine 198381416222486 [Google Scholar]
- 28.Schellhas Spine. 1996;21:300. doi: 10.1097/00007632-199602010-00009. [DOI] [PubMed] [Google Scholar]
- 29.Spitzer Spine. 1995;20:S1. [Google Scholar]
- 30.Squires J Bone Joint Surg Br. 1996;78B:955. doi: 10.1302/0301-620X78B6.1267. [DOI] [PubMed] [Google Scholar]
- 31.Van J Rheumatol. 1991;18:1884. [PubMed] [Google Scholar]
- 32.Vernon J Manipulative Physiol Ther. 1991;14:409. [PubMed] [Google Scholar]
- 33.Von Pain. 1990;40:279. doi: 10.1016/0304-3959(90)91125-3. [DOI] [PubMed] [Google Scholar]
- 34.WaddellSpine 198492046233713 [Google Scholar]
- 35.Wheeler Spine. 1999;24:1290. doi: 10.1097/00007632-199907010-00004. [DOI] [PubMed] [Google Scholar]