Abstract
The primary aim of the study was to compare the prevalence of neck pain and disability in a group exposed to motor vehicle accidents (MVAs) with those in the general population. The secondary aim was to assess the prevalence of a past history of exposure to an MVA with sequelae of neck pain in the general population. The exposed group consisted of 121 patients with neck complaints following an MVA in 1983. The control group, consisting of 1,491 subjects, was randomly selected, with attention to the distribution of age and gender in the exposed group. A neck-pain questionnaire was mailed to the subjects. In the control group, it included enquiry about a history of exposure to an MVA with sequelae of neck pain. The Neck Disability Index (NDI) was used to assess neck-related disability. In the exposed group 108 subjects (89%) responded, and in the control group 931 (62%) did. Seventeen years after the MVA, 59 subjects (55%) reported neck pain in the exposed group, with no gender differences. In the control group 270 (29%) reported neck pain with a higher frequency among women (34%) than men (19%) (p<0.01). There was a significant difference between the exposed group and the control group regarding the occurrence of neck pain (p<0.001). In the control group 34% recalled a history of an MVA, among whom one-third reported neck pain in connection with the accident and 28% had persistent neck pain referable to the accident. The exposed group scored significantly higher on the NDI (p<0.001) and reported significantly higher neck pain intensity than did the control group (p<0.001). In conclusion, a past history of exposure to an MVA with sequelae of neck pain appears to have a substantial impact on future persistent neck pain and associated disability.
Keywords: Neck pain, Prevalence, Whiplash, Cohort study
Introduction
Neck pain constitutes a major health problem, accounting for a large proportion of disability and occupational illness in the general population [4, 6, 12, 15, 22], and may be explained by many different factors. One frequently reported and confounding factor is exposure to a motor vehicle accident (MVA), which might have a substantial impact on persistent neck pain and associated disability [3]. Despite extensive research the concept and prevalence of residual neck complaints inflicted by an accident-related physical injury is one of the most debated conditions in medicine.
In the acute stage the neck pain is attributed to soft-tissue injuries to the cervical region [18, 24]. Neck pain and headache are the most frequently reported features of the condition [16], termed whiplash associated disorder (WAD) [20]. In addition, WAD comprises various disabling complaints including radiating pain in the shoulder/arm/hand, fatigue, concentration difficulties, dizziness, visual and auditory symptoms, emotional disturbances such as anxiety, depression, and general irritability, as well as poor coping strategies, low self-efficacy beliefs, and high disability levels [13, 18, 19, 20]. However, long-lasting neck pain and disability following MVAs, sometimes referred to as “the late whiplash syndrome” is a poorly understood and controversial issue [10, 21].
Despite the considerable number of studies concerning the prevalence of persistent neck pain after whiplash-type injuries, it is difficult to give a confident long-term prognosis for the patients. This is due to the generally short follow-up and the often-small study populations, based on selected groups of patients and not presenting a clear picture of the long-term consequences of WAD.
For a better understanding of the development of persistent pain and disability attributed to traffic collisions, it is important to include a comparison group representing the general population when evaluating the symptoms. Only a few studies have used such a design addressing this issue, presenting contradictory results [2, 17]. If the accidental trauma to the neck is the major factor for the prolonged pain and disability, the prevalence of neck complaints in an exposed group should be higher than in the general population [2].
The objectives of the study were twofold. The primary aim was to compare the prevalence of neck pain and disability in a group exposed to MVAs with those in the general population. The secondary aim was to assess the prevalence of a past history of exposure to an MVA with sequelae of neck pain in the general population.
Materials and methods
Study population
Exposed group
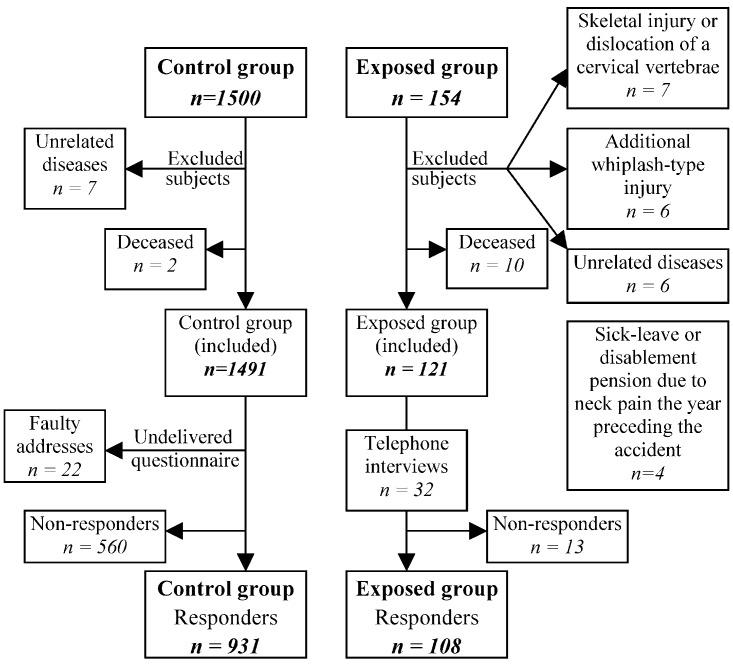
This population has previously been described in detail [5]. The group including 154 patients (89 women and 65 men) was diagnosed as having whiplash injuries at the two main hospital emergency rooms in Göteborg in 1983. The diagnosis of a whiplash injury was based on anamnestic and radiological information and the presence of neck pain and stiffness following an MVA. It was defined as soft-tissue injury with no skeletal injury or significant dislocation of a cervical vertebra. Routine treatment consisted of advice to rest for a few days, analgesics, and a soft cervical collar. Subjects with unrelated diseases or additional injuries such as skeletal injuries or a significant dislocation (>3 mm) of a cervical vertebra—with or without a spinal cord or cervical root injury—that precluded completion of the questionnaire or would make evaluation difficult were excluded. Furthermore, subjects suffering from severe neck pain causing more than 1 month of sick leave or disablement pension the year preceding the accident were excluded, as were subjects involved in a second whiplash-type injury. Of the 154 patients, 23 failed to meet the inclusion criteria (Fig. 1). After exclusions, including ten patients who had died since the accident, the exposed group consisted of 121 patients.
Fig. 1.
Flow chart for the study population
Thirteen patients in the exposed group (11%) did not take part in the study. Among these, two refused to participate. Five patients were not found in the national registration. Four of those five were temporarily in Sweden at the time of the accident and could not be traced. Another six patients could not be reached because of secret or unknown phone numbers.
Control group
A control group representing the population of Göteborg was randomly selected from a computerized population-based register (SPAR) with consideration taken for the distribution of age and gender in the exposed group. Included were 1,500 subjects (915 women and 585 men). The data comprised information drawn from the national register, including year of birth in 5-year intervals and current addresses. Seven subjects were excluded because of unrelated diseases and two had died, leaving a total study population of 1,491 subjects. Among the 560 control subjects who did not take part in the study, 22 were not found because of faulty addresses, and the questionnaires were returned undelivered.
Assessments
A standardized self-administered questionnaire consisting of two parts was mailed to all participants. In the first part, the subjects in the exposed group were asked a yes-or-no question about persistent neck pain linked to the MVA in 1983. The subjects in the control group were asked to report, yes or no, the occurrence of neck pain. Furthermore, the control group was asked about a previous history of exposure to an MVA, for a yes or no response. If yes, they were asked to specify the year of occurrence and asked whether or not they had any neck pain in connection with the accident, and whether or not they had sought medical care in connection with the accident due to the neck pain. If yes, the answer was to include details as to hospital emergency room, primary care or other health care specialist. Finally, they were to answer a yes-or-no question as to whether they had persistent neck pain referable to the MVA.
The second part consisted of the Neck Disability Index (NDI), a self-reporting instrument used to measure limitations in daily activities due to neck pain. The NDI was originally partly generated from the Oswestry low back pain questionnaire [9] and addressed particularly to sufferers of disabling neck pain that may arise from whiplash-type injuries [23]. The NDI has proved to be valid, reliable and sensitive to change, and it has high internal consistency [14, 23]. The NDI has been translated to a Swedish version.
The NDI consists of ten items addressing pain intensity, personal care, lifting, reading, headache, concentration, work, driving, sleep, and recreation. For each item there are six possible answers describing the degree of disability scored 0 (no activity limitation) to 5 (major activity limitation). It was made clear to the participants that the items specifically referred to neck pain. All items are summed up and an overall percentage degree of disability is calculated by dividing the final score by the maximal score of 50. A higher score indicates greater disability. To deal with the questions left blank by the participants, a strategy similar to the method described for the Oswestry questionnaire was used, by transforming the score into a percentage [9]. If the alternative “not applicable” in the item concerning driving was chosen, that item was excluded.
The study was approved by the ethics committee of Göteborg University.
Statistical method
Analyses were done using the Statistical Package for Social Sciences (SPSS 11.0). The chi-square test was used to compare the occurrence of neck pain between the exposed group and the control group and to compare gender differences within the groups.
The chi-square test was also used to compare gender differences within the control group with respect to a recalled history of an MVA, neck pain and medical care in connection with the accident, and persistent neck pain referable to the MVA. Analyses were also done using the Mann–Whitney U-test to compare the scores on the NDI between the exposed group and the control group and to compare gender differences within the groups. For all statistical tests, a P value of less than 0.05 was considered significant.
Results
A total of 1,039 subjects (64%) completed the present study after two written reminder and telephone interviews. A flow chart for the study population is shown in Fig. 1. In the exposed group a total of 108 patients (89%) responded, mean age 54 years (range 36–83). Seventy-six patients (70%) responded by returning the completed questionnaire and 32 patients (30%) responded through interviews over the phone. In the control group 931 subjects (62%) responded to the questionnaire, mean age interval 53–57 years (range 31–85). Non-participants were similar to participants in both groups with regard to age and gender.
Prevalence of neck pain
In the exposed group 59 subjects (55%) considered themselves as having persistent neck pain linked to the MVA in 1983. This group included 55% of the women (n=36, mean age 53 years, range 37–76) and 55% of the men (n=23, mean age 55 years, range: 36–83). Forty-nine patients (45%) considered themselves fully recovered.
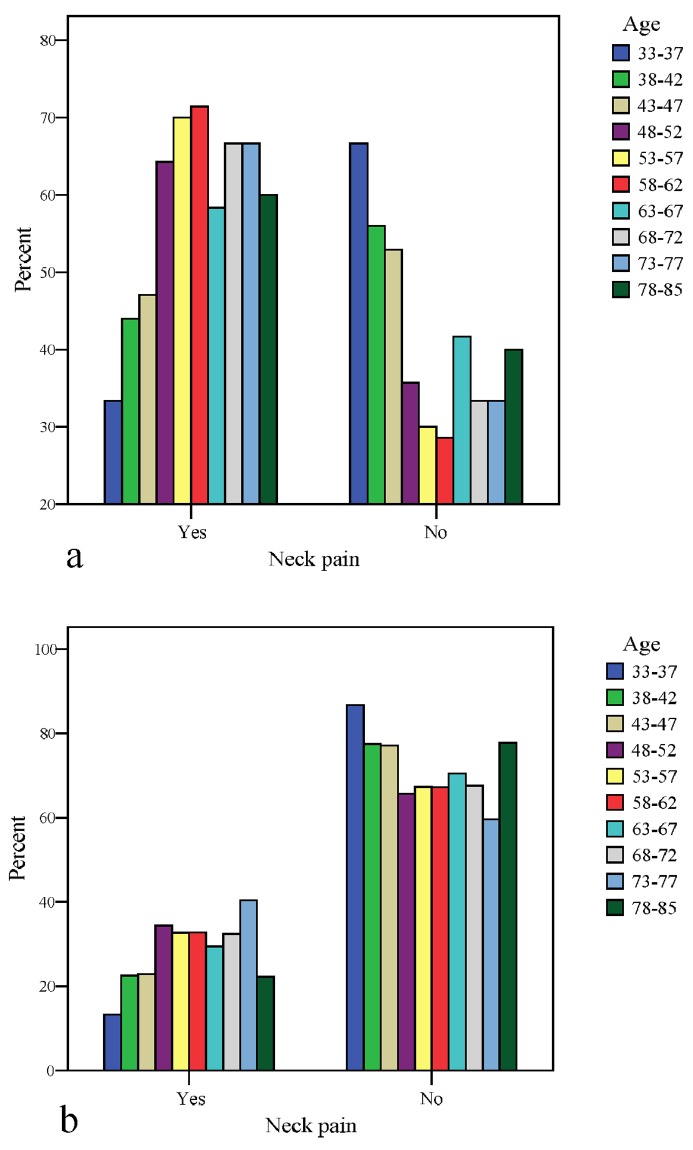
In the control group, 270 subjects (29%) reported neck pain, with a higher frequency among women (34%, n=208) than men (19%, n=62) (p<0.01), (mean age interval 48–52 and 53–57, respectively). There was a significant difference between the exposed group and the control group in the occurrence of neck pain (p<0.001). The prevalence of neck pain and gender distributions within the groups is presented in Fig. 2.
Fig. 2 a.
Prevalence of neck pain in the exposed group; b prevalence of neck pain in the control group
History of an MVA
In the control group a total of 313 subjects (34%) recalled a history of exposure to an MVA (Table 1), among whom 97 (31%) reported neck pain in connection with the accident and 28% had persistent neck pain referable to the accident. The mean reported time since the MVA was 18 years (range 1–60 years).
Table 1.
A history of exposure to an MVA, neck pain and medical care in connection with the accident, and persistent neck pain referable to the MVA in the control group
| Total | Women | Men | P value | |
|---|---|---|---|---|
| (N=931) | (N=605) | (N=326) | ||
| n (%) | n (%) | n (%) | ||
| A history of exposure to an MVA | 313 (34) | 178 (29) | 135 (41) | <0.001 |
| Neck pain in connection with the MVA | 97 (31)* | 65 (37) | 32 (24) | <0.05 |
| Sought medical care in connection with the MVA | 102 (33)** | 71 (40) | 31 (23) | <0.01 |
| Emergency room | 68 (67) | 46 (65) | 22 (71) | - |
| Primary care | 15 (15) | 9 (13) | 6 (19) | - |
| Other health care specialist | 17 (17) | 14 (20) | 3 (10) | - |
| Persistent neck pain referable to the MVA | 89 (28)*** | 63 (35) | 26 (20) | <0.01 |
*Data missing for four subjects
**Data missing for seven subjects
***Data missing for four subjects
Among the 270 subjects who answered “yes” to the question regarding the occurrence of neck pain, 63 (23%) recalled a history of exposure to an MVA with neck pain, among whom 53 (84%) sought medical care in connection with the accident.
A history of exposure to an MVA was more common in men than in women (p<0.001). However, women reported neck pain and sought medical care in connection with the accident more frequently than men (p<0.05 and p<0.01 respectively). Persistent neck pain referable to the MVA was more common in women than in men (p<0.01).
Neck Disability Index
The scores on the NDI are presented in Table 2. The total score of the NDI was significantly higher in the exposed group compared with the control group (p<0.001). The item analysis revealed that the exposed group scored significantly higher on the item “pain intensity” than the control group did (p<0.001). There was no significant sex difference on the NDI in the exposed group, whereas the women in the control group scored significantly higher on the NDI than men did (p<0.001).
Table 2.
Neck Disability Index (NDI) scores
| NDI score | Exposed group | Control group | P value* |
|---|---|---|---|
| (N=99) | (N=931) | ||
| Median (min–max) | Median (min–max) | ||
| Mean (SD) | Mean (SD) | ||
| Items (0–5) | |||
| Pain intensity | 1 (0–5) | 0 (0–5) | <0.001 |
| 1.3 (1.3) | 0.5 (0.9) | - | |
| Personal care | 0 (0–5) | 0 (0–4) | - |
| 0.5 (0.9) | 0.1 (0.5) | - | |
| Lifting | 1 (0–5) | 0 (0–5) | <0.001 |
| 1.5 (1.6) | 0.6 (1.2) | - | |
| Reading | 0 (0–5) | 0 (0–5) | - |
| 1.1 (1.3) | 0.4 (0.9) | - | |
| Headache | 1 (0–5) | 0 (0–5) | <0.001 |
| 1.5 (1.6) | 1.0 (1.3) | - | |
| Concentration | 0 (0–5) | 0 (0–5) | - |
| 0.8 (1.2) | 0.4 (0.8) | - | |
| Work | 1 (0–5) | 0 (0–5) | <0.001 |
| 1.2 (1.5) | 0.7 (1.1) | - | |
| Driving | 0 (0–5) | 0 (0–5) | - |
| 0.9 (1.3) | 0.4 (0.9) | - | |
| Sleep | 1 (0–5) | 0 (0–5) | <0.001 |
| 1.2 (1.5) | 0.7 (1.1) | ||
| Recreation | 0 (0–5) | 0 (0–5) | |
| 1.0 (1.4) | 0.5 (1.1) | ||
| Median (for all 10 items) | 1 (0–5) | 0 (0–5) | <0.001 |
| 1.0 (1.2) | 0.4 (0.8) | ||
| Total score (0–100) | 18 (0–80) | 4 (0–98) | <0.001 |
| 22.1 (21.7) | 10.6 (15.2) | ||
Discussion
The main findings in the present study were that a group exposed to MVAs reported significantly higher occurrence and intensity of neck pain and neck-related disability compared with a control group representing the general population.
Included in the exposed group were all patients who had attended the two major hospital emergency rooms in Göteborg during 1983, suggesting that the group is a representative sample of patients with whiplash-type neck pain following MVAs. The control group was intended to give information about the prevalence of all types of neck pain and neck-related disability in the population of Göteborg as a whole.
In the exposed group over half of the subjects (55%) reported neck pain 17 years after the MVA, approximately half of the women and half of the men. The corresponding figures of prevalence in the control group were 29%, with a higher frequency among women (34%) than men (19%). This gender pattern has been reported in several studies [4, 8, 11]. However, among subjects suffering from whiplash-associated neck pain, gender appears to have no influence on residual pain in the long term [5].
The findings in the present study are in accordance with a previous Swedish cohort study, which concluded that in subjects with reported whiplash injury there is a higher risk of neck or shoulder pain 7 years after the collision, as compared with subjects without reported whiplash injury [1]. Our results are contrary to the findings of two previous studies in which the authors stated that the prevalence of neck pain in a group of exposed subjects with whiplash-type injuries was the same as in atraumatic subjects [4, 17].
It is difficult to compare the findings in the present study with other studies because of differences in study design. Since the control group was intended to give information about the prevalence of neck pain in the population as a whole, no initial distinction was made between subjects with or without a previous history of an MVA. Hence, the proportion of neck pain in the control group may be explained by various reasons. The reported prevalence of all types of neck pain in a population-based study from Sweden is 43% and chronic neck pain in the same population was identified in 19% of the women and 16% of the men [11]. In a similar population study Côté et al. [7] also reported a high prevalence of neck pain.
In the control group 34% of the subjects recalled a previous history of exposure to an MVA, among whom one-third reported neck pain in connection with the accident and 28% had persistent neck pain referable to the original accident, corresponding to 10% of the control group as a whole. These findings agree with a previous study estimating that, in population terms, 11% recall a neck injury [8]. A history of exposure was more common in males.
From another point of view, among the 270 subjects who reported neck pain, 63 (23%) recalled an MVA with sequelae of neck pain. These figures are in accordance with previous findings concluding that the proportion of neck pain is more frequent in individuals with a history of neck injuries [7, 8, 11, 15].
The findings in the present study suggest that, in the general population, women more frequently report neck pain in connection with an MVA, are more inclined to seek medical care, and more frequently suffer from persistent neck pain referable to the accident than are men. This supports the suggestions in a previous study [5].
None of the subjects in the control group had a validated diagnosis, and a history of an MVA cannot be assumed to be equivalent with a whiplash-type injury. Yet, there is no reason to believe that the population is not aware of this condition, since neck pain in connection with an MVA is a well-known disorder. Furthermore, since neck pain is highly prevalent in the general population, it is reasonable to assume that to some extent, pre-existing neck pain was certainly present prior to the recalled MVA in the control group.
For ethical reasons the study information enclosed with the questionnaire mailed to the control group had to refer to the exposed group under study. The subjects in the control group with a history of exposure to an MVA may, therefore, have felt more obliged to respond to the questionnaire. Furthermore, individuals with neck complaints resulting in disability of any measure tend to answer a questionnaire to a greater extent than those who have no complaints. This might have resulted in an overestimation of the proportion of subjects suffering from neck pain and disability in the control group.
In the literature, prevalence studies give no information regarding the degree of disability caused by the neck pain, which would contribute to the evaluation of the outcome after exposure to an MVA. In the present study there was a significant difference in NDI scores between the exposed group and the control group, which is in accordance with the findings of Berglund et al. [2], which concluded that rear-end collisions resulting in reported whiplash injuries seem to have a substantial impact on health complaints, even a long time after the collision.
The item analysis revealed that the exposed group scored significantly higher on the item “pain intensity” than the control group did. In the exposed group there was no significant gender difference on the NDI. In the control group women scored significantly higher than men did on the NDI, which is in accordance with the higher prevalence of neck pain among women than in men.
A history of an MVA with sequelae of neck pain seems to be a predictor of long-lasting neck pain, which might explain the similarities observed in neck-injury cohort studies and population studies. To present a clear picture of the long-term consequences of WAD, future studies should include a comparison group and assess the degree of disability caused by the pain. They should also make a clear distinction between subjects exposed to MVAs, with or without neck pain in connection with the accident, when evaluating the outcome of disabling neck pain following whiplash-type injuries.
Conclusion
A past history of exposure to an MVA with sequelae of neck pain appears to have a substantial impact on future persistent neck pain and associated disability.
References
- 1.Berglund J Clin Epidemiol. 2000;53:1089. doi: 10.1016/S0895-4356(00)00225-0. [DOI] [PubMed] [Google Scholar]
- 2.Berglund J Clin Epidemiol. 2001;54:851. doi: 10.1016/S0895-4356(00)00369-3. [DOI] [PubMed] [Google Scholar]
- 3.Bogduk Curr Opin Rheumatol. 1998;10:110. doi: 10.1097/00002281-199803000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bovim Spine. 1994;19:1307. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Bunketorp Eur Spine J. 2002;11:227. doi: 10.1007/s00586-002-0393-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.C Spine. 1998;23:1689. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 7.C Accid Anal Prev. 2000;32:151. doi: 10.1016/S0001-4575(99)00117-7. [DOI] [PubMed] [Google Scholar]
- 8.Croft Pain. 2001;93:317. doi: 10.1016/S0304-3959(01)00334-7. [DOI] [PubMed] [Google Scholar]
- 9.Fairbank Physiotherapy. 1980;66:271. [PubMed] [Google Scholar]
- 10.Ferrari J Neurol Neurosurg Psychiatry. 2001;70:722. doi: 10.1136/jnnp.70.6.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guez Acta Orthop Scand. 2002;73:455. doi: 10.1080/00016470216329. [DOI] [PubMed] [Google Scholar]
- 12.Hasvold Scand J Prim Health Care. 1993;11:219. doi: 10.3109/02813439308994834. [DOI] [PubMed] [Google Scholar]
- 13.Hildingsson Acta Orthop Scand. 1990;61:357. doi: 10.3109/17453679008993536. [DOI] [PubMed] [Google Scholar]
- 14.Hoving Pain. 2003;102:273. doi: 10.1016/S0304-3959(02)00406-2. [DOI] [PubMed] [Google Scholar]
- 15.Makela Am J Epidemiol. 1991;134:1356. doi: 10.1093/oxfordjournals.aje.a116038. [DOI] [PubMed] [Google Scholar]
- 16.Norris J Bone Joint Surg Br. 1983;65:608. doi: 10.1302/0301-620X.65B5.6643566. [DOI] [PubMed] [Google Scholar]
- 17.Obelieniene J Neurol Neurosurg Psychiatry. 1999;66:279. doi: 10.1136/jnnp.66.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radanov BP, Sturzenegger M, Di Stefano G (1995) Long-term outcome after whiplash injury. A 2-year follow-up considering features of injury mechanism and somatic, radiologic, and psychosocial findings. Medicine (Baltimore) 74:281–297 [DOI] [PubMed]
- 19.Soderlund Clin Rehabil. 2000;14:457. doi: 10.1191/0269215500cr348oa. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer Spine. 1995;20:1S. [PubMed] [Google Scholar]
- 21.Stovner Spine. 1996;21:2735. doi: 10.1097/00007632-199612010-00006. [DOI] [PubMed] [Google Scholar]
- 22.Van J Rheumatol. 1991;18:1884. [PubMed] [Google Scholar]
- 23.Vernon J Manipulative Physiol Ther. 1991;14:409. [PubMed] [Google Scholar]
- 24.Yoganandan Spine. 2001;26:2443. doi: 10.1097/00007632-200111150-00010. [DOI] [PubMed] [Google Scholar]