Abstract
To clarify the injury pattern, initial spinal instability, degree of discoligamentous injuries in cervical lateral mass and facet joint fractures, we retrospectively analyzed radiological parameters and introduced a new classification for these injuries. Surgical treatment was performed with cervical pedicle screw fixation (CPS), and overall neurological and radiological outcome was evaluated with a minimum follow-up period of 2 years. Lateral mass fractures were divided into the following four subtypes: separation, comminution, split, and traumatic spondylolysis. The sagittal and frontal alignments were evaluated at both mainly injured and adjacent spinal segments on radiographs. The initial discoligamentous injuries were investigated on magnetic resonance imaging in terms of their frequencies, subtype of injuries, and involved spinal levels. Anterior translation of fractured vertebra was demonstrated in 77% of lateral mass fractures, while 24% of anterior translation was observed, even in cephalad-adjacent vertebrae. On magnetic resonance imaging, signal changes in anterior longitudinal ligament (ALL) and intervertebral disc were demonstrated in 76% of caudal segments and 24% of cephalad segments adjacent to fractured vertebra of lateral mass fractures. The subtype analyses of lateral mass fractures demonstrated high rates of anterior translation in separation, split, and traumatic spondylolisthesis, as well as significant coronal malalignment in comminution and split types (p<0.05). Thirty-one patients underwent surgical treatments using a cervical pedicle screw fixation. The CPS provided the superior capability of deformity correction without pseudoarthrosis, as well as excellent neurological recovery. The average numbers of stabilized segments were minimized without serious complications. In separation, facet joint fracture, and fractures with mild lateral mass comminution, the single level posterior fixation can be considered. The significant unstable injuries of split and comminution type with coronal malalignment can be treated with exclusive two-level posterior stabilization with CPS. The initial evaluation of fracture subtypes helps to successfully minimize the stabilized spinal segment.
Keywords: Cervical lateral mass fracture, Facet joint fracture, Discoligamentous injury, Magnetic resonance imaging, Cervical pedicle screw
Introduction
With the recent progress in medical imaging technologies, an increasing number of lateral mass and facet joint fractures are clinically detected in the cervical spine. These often require conservative treatment. However, surgical treatment is indicated when there is a neurologic disturbance or definite segmental spinal instability at the injured segment [8, 9, 11, 14, 18]. Due to a limited number of clinical reports, these fractures remain unclear in terms of fracture patterns, injury mechanism, frequency of initial sagittal and coronal deformity, and the degree of associated soft-tissue injuries [11, 18]. These data are required for the accurate diagnosis and the determination of initial treatment strategies.
In addition, there were several surgical procedures for lateral mass and facet joint fractures. Jeanneret et al. reported the osteosynthesis of the fractured lateral mass for the fracture separation of lateral mass without sacrificing the motion segment [14]. Other procedures include posterior spinous process wiring [6], lateral mass screw-plate fixation [5, 8, 9, 13, 18, 20], and combined anterior and posterior stabilization [19]. We have utilized a cervical pedicle screw fixation (CPS) over 300 cases of cervical spine disorders since 1990, demonstrating excellent clinical outcome [1, 2, 3].
To clarify the injury pattern and initial spinal instability, as well as the degree of discoligamentous injuries in cervical lateral mass and facet joint fractures, we introduced a new classification for these injuries and retrospectively analyzed fracture patterns and discoligamentous abnormalities on radiograph and MR imaging. The surgical treatment was performed with cervical pedicle screw fixation (CPS), and overall neurological and radiological outcome was evaluated with a minimum follow-up period of 2 years.
Materials and methods
Patient demographics
From January 1991 to December 1999, 31 patients, including 23 lateral mass fractures and eight facet joint fractures, received surgical treatment in our institution. Twenty-six patients were male and five were female. The average age at surgery was 46 years old (18–63 years). The injuries were caused by a traffic accident in 20, falls in six, a heavy object in two, and other causes in two. The days from injury to surgery were 22 days on average (0–257 days). Most patients were treated in other hospitals initially and subsequently transferred to our institution, due to residual deformity or neurological disturbance. The spinal fracture levels were C6 in 14, C5 in eight, C7 in six, C4 in two, and C3 in one. One patient suffered from a superior articular process fracture of C4 in combination with inferior articular process fracture of C3. The injury types were classified by evaluating injury X-rays according to Allen’s classification [4]. There were 27 compressive-extension injuries, three lateral flexion injuries, and one distractive-flexion injury. The neurological disturbance at surgery was a persistent radiculopathy in 21 patients, while five patients had myelopathy with various degrees of Frankel grade, from B to D [10]. The associated injury was recorded in one patient with a cerebral contusion treated conservatively.
Radiographic analyses of fracture patterns and associated soft-tissue injury
From X-rays and MRI analyses, the fractures were classified into subtypes. The translation of fractured and adjacent vertebrae in the sagittal and coronal planes, uncovertebral joint subluxation, and the degree of vertebral body destruction were evaluated preoperatively and at follow-up. The signal changes and the rupture of the intervertebral disc and spinal ligaments—anterior longitudinal ligament (ALL); posterior longitudinal ligament (PLL); supraspinous and interspinous ligaments (SSL and ISL)—were examined at both a mainly injured spinal segment and adjacent segments on initial MRI films. These changes were subsequently classified into partial or complete change. The associated bony bruise was also evaluated on MRI films. The occurrence of these parameters was compared between the lateral-mass-fracture group and the articular-process-fracture group, as well as between each fracture subtype, to examine whether the severity of injury corresponded to these changes.
Surgical procedures
Thirty patients underwent posterior reduction and stabilization with the cervical pedicle screw system. Simultaneous posterior neural decompression was conducted in eight patients: foraminotomy in six and multiple-level laminectomies for developmental narrow canal in two. Four patients received additional anterior decompression and fusion for the release of rigid deformity or requirement of additional anterior column support. Osteosynthesis for the separation fracture of the lateral mass was performed in one patient with a titanium cannulated screw. In an early series of transpedicular screw fixation, a scaled-down VSP screw (Depuy AcroMed, Raynham, MA, USA) was used in eight patients. In subsequent cases, the cervical transpedicular-screw system was used with screw diameters of 3.5 mm, 4.0 mm, and 4.5 mm. The bone graft was conducted with locally harvested bone from spinous processes and was properly placed bilaterally under the cervical pedicle screw plate.
Assessment of surgical outcome and functional recovery
At a final follow-up, the fusion status and spinal alignment were evaluated using functional X-rays and CT scans by three orthopedic spine surgeons. The radiographic criteria for spinal fusion included no pedicle screw loosening and existence of facet fusion, as well as no segmental motion detected on functional X-rays. The number of stabilized segments was compared among fracture subtypes to assess whether short fusion was achieved in specific fracture subtypes. The neurologic recovery was evaluated using a Frankel grade for myelopathy, and the pain, motor, and sensory changes were descriptively recorded for radiculopathy cases. Early and late complications were recorded in terms of infections, pseudoarthrosis, implant failures, and neurologic deterioration.
Results
All cases were followed until a final follow-up (average 5.2 years, 2 years to 10 years and 1 month).
Radiographic analyses of fracture patterns and associated soft-tissue injury
The lateral mass fractures were divided into the following four subtypes: separation fracture in 11, comminution type in four, split type in five, and traumatic spondylolysis in two (Fig. 1, 2). Separation fracture was defined as two fracture lines of unilateral lamina and pedicle, thereby isolating and separating the entire unilateral articular mass [14, 16, 18]. The comminution type showed multiple fracture lines in the lateral mass, with significant fragmentation, frequently accompanied by lateral wedging deformity in a coronal plane. The split-type fracture had a vertical fracture line on a coronal plane in the unilateral lateral mass, creating an anterior-posterior separation with the invagination of the superior articular process of the caudal adjacent vertebra. The traumatic spondylolysis showed bilateral horizontal fracture lines at the pars interarticularis, leading to a separation between anterior and posterior spinal elements. Superior and inferior articular-process fractures were seen in one patient each, respectively, and a combination of both fractures at consecutive vertebrae was seen in six patients.
Fig. 1.
Schematic drawings showing fracture subtypes of lateral mass fracture. A Separation fracture: defined as two fracture lines of unilateral lamina and pedicle, thereby isolating and separating the entire unilateral articular mass. B Comminution type. There are multiple fracture lines in the lateral mass with significant fragmentations, frequently accompanied by lateral wedging deformity in a coronal plane. C Split type. There is a vertical fracture line on a coronal plane in the unilateral lateral mass, creating an anterior-posterior separation with invagination of the superior articular process of caudal adjacent vertebra. D Traumatic spondylolysis. There are bilateral horizontal fracture lines at pars interarticularis, leading to a separation between the anterior and posterior spinal elements
Fig. 2.
Typical radiographs and CTs showing fracture subtypes of lateral mass fracture. A separation fracture; B comminution type; C split type; D traumatic spondylolysis
In terms of spinal alignment on initial radiographs, anterior translation of fractured vertebrae was demonstrated in 77% of whole lateral-mass fractures, while anterior translation was observed even in 24% of cephalad adjacent vertebrae and 10% of caudal adjacent vertebrae (Table 1). Alignment change in the coronal plane was detected in 33% of lateral mass fractures. Thirty-three percent of articular-process fractured vertebrae showed anterior translation, while 50% of the upper adjacent vertebrae did, and 0% of the caudal adjacent vertebrae did. Alignment change in the coronal plane was not detected in any articular process fractures.
Table 1.
Translation of fractured and adjacent vertebrae on sagittal and frontal plane. (Frequency shown as percentage in each fracture type) (Upp. adj. upper adjacent vertebrae, Fractured fractured vertebra, Low. adj. lower adjacent vertebra)
| - | Anterior translation | Frontal translation | ||
|---|---|---|---|---|
| Fracture type | Upp. adj. | Fractured | Low. adj. | Fractured |
| Lateral mass | 24% | 77% | 10% | 33% |
| Articular process | 50% | 33% | 0% | 0% |
The subtype analysis in lateral mass fractures demonstrated that the separation, split type and traumatic spondylolysis fractures showed high rates of anterior translation in 91%, 80%, and 100%, respectively. The anterior translation of the adjacent vertebrae was 20% in separation fractures, 50% in comminution type fractures, 0% in split type fractures and 50% in traumatic spondylolysis fractures. However, there was no statistical difference between groups due to a small number of patients in each group. The comminution and split type fractures demonstrated higher rates of coronal malalignment—in 25% and 40%, respectively—when compared with that of separation fractures (3%) (p<0.05).
In terms of vertebral body destruction, both groups of lateral mass fractures and articular process fractures showed 33% of vertebral body destruction rate. However, in the subgroups of lateral mass fractures, the separation fractures demonstrated a significantly lower rate (1%) than that of other subtypes (50–60%) (p<0.05).
On MRI, the main injured segment was the caudal segment adjacent to the fractured vertebra in the lateral mass fractures. Signal changes of ALL and disc in lateral mass fractures were demonstrated in 76% for the caudal segments and 24–29% for the cephalad segments adjacent to the fractured vertebra (Table 2). The changes in the PLL and supraspinous and interspinous ligaments (SISL) at the main injured segment were 35% and 12%, respectively, in the lateral mass fractures. The adjacent PLL or SISL change was minimal (0–6%) in lateral mass fractures. Meanwhile, signal changes for articular process fractures were demonstrated in 40% in ALL and 80% in the disc, at the cephalad segment adjacent to the fractured vertebra. The signal changes of PLL and SISL were not detected in either cephalad and caudal segments. Additionally, the caudal adjacent segment did not show any signal change of ALL and disc in articular process fractures. The subtype analyses in lateral mass fractures demonstrated that each subtype showed the same trend as that in the whole lateral-mass-fracture group. There were no significant differences among fracture subtypes in terms of frequency of signal changes.
Table 2.
Intervertebral disc and ligamentous injuries on initial magnetic resonance imaging (frequency shown as percentage in each fracture type) (Adj. segment segment adjacent to main injured segment, ALL anterior longitudinal ligament, Disc intervertebral disc, PLL posterior longitudinal ligament, SISL supraspinous and interspinous ligaments)
| - | Main injured segment | Adj. segment | ||||
|---|---|---|---|---|---|---|
| Fracture type | ALL | Disc | PLL | SISL | ALL | Disc |
| Lateral mass | 76% | 76% | 35% | 12% | 24% | 29% |
| Articular proc. | 40% | 80% | 0% | 0% | 0% | 0% |
All signal changes of lateral mass fracture at adjacent segment were observed in cephalad-adjacent segments to fractured vertebrae
Surgical outcome and functional recovery
Arthrodesis was successfully achieved in all cases. Although the average number of injured segments was 1.7, 1.5 spinal segments were surgically stabilized on average, demonstrating the tendency for short-segment fusion in a whole group. The average number of stabilized segments in either the lateral-mass-fracture or articular-process-fracture group was 1.6 and 1.1 segments, respectively. In separation fractures, we successfully saved fixed segments in about one-half of cases, by exclusively fusing the segment just below the fractured vertebra (average fixed segments: 1.4). The average number of fixed segments in comminution, split, and traumatic spondylolysis types were 1.6, 2, and 2 segments, respectively. The more comminuted type of injury often requires two-level fixation.
The postoperative radiographic analysis demonstrated that there were six cases of slight anterior translation deformity at follow-up. Among them, three cases showed anterior translation of fractured vertebra due to incomplete reduction during operation. However, no correction loss was seen in any cases after postoperative periods. Another three cases of cephalad vertebra translation occurred due to short-segment fusion. A case of C6 separation fracture was treated with osteosynthesis of the unilateral fracture site using a cannulated screw. The reduction of the fractured lateral mass was successfully achieved. However, the translation of vertebra remained. Other two cases of C5 separation and C6 comminution type fractures showed anterior translation of fractured and cephalad vertebrae. However, because of a lack of soft-tissue injury at the adjacent segment on MRI, the main injured segment was stabilized exclusively. Although slight deformity was seen in the six cases described above, no problems relating to neurologic symptoms or pain were demonstrated at follow-up.
In terms of neurologic symptoms, there were five cases of cervical myelopathy, and 21 cases of radiculopathy, preoperatively. Based on the Frankel grading system, preoperative grades were B in one, C in three, and D in two cases. However, postoperative grades were C in one case, D in two, and E in three cases. Neurologic improvement more than one grade was seen in all myelopathy cases. All radiculopathy cases recovered in terms of radicular pain, numbness, and weakness in the upper extremities, except three cases who were between good and fair level but had persisting motor weakness.
Complications
There was one deep infection in a C5–C7 lateral flexion injury case, which was treated with C5–C7 pedicle screw fixation. Continuous irrigation without implant removal successfully resulted in the settlement of infection. No neurologic injury was observed in any cases. The patient who complained of pain due to skin irritation from the screw head required a hardware removal after completion of arthrodesis.
Case presentations
Case1
A 43-year-old male suffered from a separation fracture of the left C5 lateral mass due to a traffic accident. The initial neurologic presentation was incomplete Brown-Sequard syndrome with motor and sensory deficits. The imaging studies showed a typical horizontalization and fracture separation of the left C5 lateral mass, as well as ruptured ALL and disc injury at C5–C6 on sagittal MRI imaging. Posterior fixation and fusion was conducted using a cervical pedicle screw system. After 4 years postoperatively, arthrodesis was complete and no adjacent segment change was demonstrated (Fig. 3).
Fig. 3.
A A 43-year-old male with C5 separation fracture of lateral mass with incomplete Brown-Séquard syndrome. AP radiograph showed a typical horizontalization of left C5 lateral mass. B MRI showed the ALL and disc injury at C5/C6 level. C CT scan demonstrated a typical floating lateral mass on the left side. D, E: Single segment posterior fixation and fusion was conducted with cervical pedicle screw system. After 4 years postoperatively, arthrodesis was complete and no adjacent segment change was demonstrated
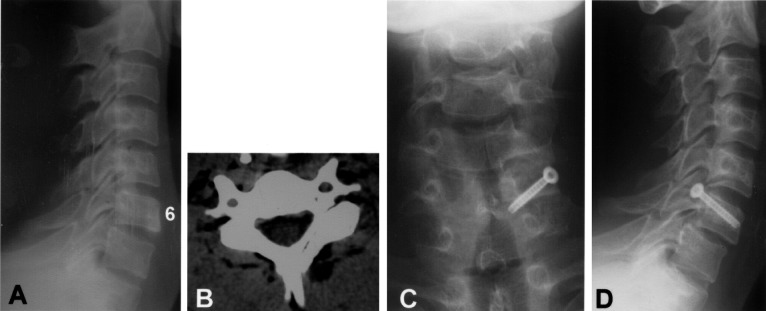
Case 2
A 33-year-old male sustained a C6 separation fracture of the left lateral mass with C6 radiculopathy. The CT scan demonstrated a typical floating lateral mass of C6. Osteosynthesis of the fractured pedicle was carried out using a cannulated titanium screw. At 5 years postoperatively, successful bony fusion was obtained at the fracture site. However, a slight anterior slippage of C6 vertebra remained without any symptoms (Fig. 4).
Fig. 4.
A, B A 33-year-old male sustained a C6 separation fracture of left lateral mass with C6 radiculopathy. C, D Osteosynthesis of the fractured pedicle was carried out using a cannulated titanium screw. At 5 years postoperatively, successful bony fusion was obtained at the fracture site. However, a slight anterior slippage of C6 vertebra remained without any symptoms
Case 3
A 60-year-old male sustained a comminution type fracture of the C5 lateral mass with spinal cord injury of Frankel C grade. The supposed injury mechanism was a C5–C6 compressive-extension injury according to Allen’s classification. The comminuted right lateral mass displaced posteriorly, demonstrating two-level instability. Two-level posterior fixation and fusion was carried out with a cervical pedicle screw system, followed by C4–C7 laminectomy. Successful arthrodesis was achieved at 1 year postoperatively (Fig. 5).
Fig. 5.
A, B A 60-year-old male sustained a comminution type C5 lateral mass fracture with spinal cord injury of Frankel C grade. The supposed injury mechanism was C5–C6 compressive-extension injury, according to Allen’s classification. C, D The comminuted right lateral mass displaced posteriorly, demonstrating two-level instability. E–G Two-level posterior fixation and fusion was carried out with cervical pedicle screw system, followed by C4–C7 laminoplasty. Successful arthrodesis was shown at 1 year postoperatively. The oblique X-ray demonstrated correct screw purchase
Discussion
Several authors have pointed out a low accuracy in the initial diagnosis of lateral mass and articular process fractures [7, 12, 18, 22, 24]. These fractures are often involved in the lower cervical spine, and initial plain radiographs do not demonstrate the abnormality in many cases. Oblique X-rays are recommended for better visualization of fracture sites; however, in patients who have suffered multiple trauma or neurological injury, it is sometimes difficult to take those views initially. Halliday et al. reported that only six of 24 cervical plain radiographs (25%) detected an initial abnormality in the emergency department [11]. Levine et al. reported that standard roentgenograms were effective in making the definitive diagnosis in only nine of 24 cases (38%) [18]. The use of CT or multidirectional tomography is recommended for better visualization of fracture and neural involvement [24, 25].
Fractures of the lateral mass and articular process were generally accepted as being produced by hyperextension or hyperextension combined with a rotational injury mechanism [12, 23, 24]. In our series, most injury types were classified into compressive-extension injuries followed by lateral flexion injuries, according to Allen’s classification [4]. In lateral flexion injuries, lateral mass fractures were more comminuted and associated with asymmetrical vertebral body fracture.
In this series of lateral mass fractures, we took the new step of dividing the fractures into the following four subtypes: separation, comminution, split, and traumatic spondylolysis. In these subtypes, comminution- and split-type fractures were new entities. The comminution-type fracture consisted of multiple fracture lines in the lateral mass with significant fragmentations, frequently accompanied by lateral wedging deformity in a coronal plane. Fractures similar to split fracture were previously reported by Sim and Yetkin et al. [21, 25]. However, this injury type was not recognized as a subtype of lateral mass fractures. Sim reported five cases of these injuries and asserted that the segmental stability was likely to be adequate and surgical indication was limited [21]. We experienced five cases of this injury type, all presenting an anterior translation, axial rotational deformity, and local lateral wedging deformity in a coronal plane. Although invagination of the superior articular process into the fractured cephalad-lateral mass possibly prevents gross initial instability, significant three-dimensional deformity should be corrected and stabilized to prevent subsequent persistent, severe neck pain.
The analysis of spinal-alignment abnormality at initial injury demonstrated the higher incidence of anterior translation or frontal plane deformity in lateral mass fractures than that in articular process fractures. In lateral mass fractures, anterior translation of vertebra was detected in 77% of fractured vertebra, while in 24% of upper adjacent vertebra as well as the frontal plane deformity in 33%. Levine et al. reported an incidence of anterior vertebral translation in 24 cases of lateral-mass-fracture separation [18]. Anterior translation of fractured vertebra was observed in 79% of fractured vertebra, as well as in 21% of cephalad-adjacent vertebra. These data were almost equivalent to that in the present study. In turn, fracture-subtype analysis demonstrated that split and comminution types showed significantly higher rates of coronal malalignment and vertebral body destruction when compared with separation fractures. This indicated that higher injury energy seemed to be associated with those two types of injuries.
This serves as the first study to precisely evaluate the initial intervertebral disc or ligamentous injuries at both fractured and adjacent spinal segments in cervical-lateral-mass and facet-joint fractures. Overall, 76% of ALL and disc, 35% of PLL, and 12% of SSL and ISL were injured on MRI at the main injured segment of lateral mass fractures. Halliday et al. reported 50% of ALL, 29% of PLL, and 75% of ISL injuries in 24 cases of lateral mass and facet fractures [11]. Considering the main injury mechanism of compressive-extension in Allen’s classification, it is reasonable to observe the higher frequency of ALL and disc injuries than those of SSL or ISL injuries. The associated lamina fractures often demonstrate T2 high signal-intensity changes around ISL, resembling SSL and ISL injuries. However, this signal change has to be carefully examined with T1-weighted images in terms of the continuity of SSL black line. Another possible explanation for this contrast is that our series may include more severely injured cases, compared with their series, which required surgery in only 50% of all cases. Moreover, 24–29% of ALL and disc signal changes at the cephalad-adjacent segment were demonstrated in this study, which serves as important data for diagnosis of injury type and subsequent treatment strategy.
In terms of surgical management, we utilized a cervical pedicle screw fixation, with a high fusion rate and patient satisfaction. In separation-fracture cases, osteosynthesis using a single screw is another choice for surgical treatment (Fig. 3) [14]. However, our case demonstrated a residual anterior translation of repaired vertebra due to the injured intervertebral disc below. As moderate or severe disc injuries are mostly associated with separation fractures, osteosynthesis is only indicated for separation fractures with minimal disc damage shown on MRI. In turn, according to the present data, one-level reduction and stabilization will be recommended in separation fractures or fractures with mild comminution based on the adjacent disc and ligament evaluation. To avoid the adjacent disc degeneration after multiple-level fusion, it is reasonable to save the stabilized segment. Although controversy remains over the choice of anterior or posterior approach, in this type of lateral-mass-fracture injury, the main injured structures were located mostly in posterior elements. Therefore, from the biomechanical point of view, the posterior procedure will be indicated. The anterior decompression procedure additionally destroys the remaining anterior structures. Even when using the exclusive posterior approach, CPS safely reduced the segment, without the excessive compression force, and stabilized the segment with slight distraction force. We have not experienced neurologic deterioration due to secondary disc herniation during reduction and stabilization, except a foraminal stenosis [1, 3].
Cervical pedicle screw fixation was reported to offer superior three-dimensional biomechanical stability and pullout strength [15, 17]. Kotani et al. demonstrated the clear advantage of cervical pedicle screw fixation over that of combined anterior and posterior fixation using Bohlman’s triple wiring or posterior lateral-mass screw fixation even in the severe discoligamentous injury model [17]. This stabilizing capacity clinically provides excellent correction of fractured vertebra, as well as a high fusion rate. Consequently, we successfully saved the stabilized segments in separation fractures or fractures with mild comminution, based on evaluation of the adjacent disc and ligament. However, severely comminuted lateral mass fractures with coronal plane malalignment required two-level posterior fixation. Regarding the clinical risk of CPS, previous studies showed no increased neurovascular complications using CPS over that of other posterior fixation techniques [3]. However, correct CPS insertion into the fractured body or cases with coronal deformity requires high technical skill, and therefore the surgical risk should not be ignored. Finally, exclusive posterior stabilization with a cervical pedicle screw system provides short fusion as well as a normal spinal alignment, even in lateral mass fractures with severe spinal instability.
Conclusion
We have introduced a new classification of cervical lateral mass fractures with subtype analysis of fracture pattern and associated soft-tissue involvement. In separation fracture, facet joint fracture, and fractures with mild lateral mass comminution, single-level posterior fixation can be considered. Significant unstable injuries of split and comminution type with coronal malalignment can be treated with exclusive two-level posterior stabilization, demonstrating excellent clinical outcome without pseudoarthrosis.
Acknowledgement
The authors acknowledge Masanori Fujiya, M.D., Michinori Saita, M.D., Yasuhiro Shono, M.D., and Takahiro Iida, M.D., for their cooperative work in correction of patient data
References
- 1.Abumi J Spinal Disord. 1994;7:19. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 2.AbumiJ Neurosurg 1999901910413121 [Google Scholar]
- 3.Abumi Spine. 2000;25:962. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 4.Allen Spine. 1982;7:1. doi: 10.1097/00007632-198200710-00001. [DOI] [PubMed] [Google Scholar]
- 5.AnClin Orthop 19973351019020210 [Google Scholar]
- 6.Bohlman J Bone Joint Surg Am. 1979;61:1119. [PubMed] [Google Scholar]
- 7.Bucholz J Neurosurg. 1989;70:884. doi: 10.3171/jns.1989.70.6.0884. [DOI] [PubMed] [Google Scholar]
- 8.CooperNeurosurgery 1989233003226509 [Google Scholar]
- 9.FehlingsJ Neurosurg 1994813418057140 [Google Scholar]
- 10.FrankelParaplegia 196971795360915 [Google Scholar]
- 11.Halliday Spine. 1997;22:2614. doi: 10.1097/00007632-199711150-00007. [DOI] [PubMed] [Google Scholar]
- 12.Harris JH, Mirvis SE (1996) Radiology of acute cervical spine trauma, 3rd edn. Williams & Wilkins, Baltimore, pp 320–339
- 13.Heller Spine. 1995;20:2442. doi: 10.1097/00007632-199511001-00013. [DOI] [PubMed] [Google Scholar]
- 14.Jeanneret J Spinal Disord. 1994;7:222. doi: 10.1097/00002517-199407030-00004. [DOI] [PubMed] [Google Scholar]
- 15.Jones Spine. 1997;22:977. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 16.Judet Rev Chir Orthop Reparatrice Appar Mot. 1970;56:155. [PubMed] [Google Scholar]
- 17.Kotani Spine. 1994;19:2529. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 18.Levine Spine. 1992;17:S447. doi: 10.1097/00007632-199210001-00018. [DOI] [PubMed] [Google Scholar]
- 19.SchultzJ Neurosurg 2000Spine21411012051 [Google Scholar]
- 20.ShapiroJ Neurosurg 1999Spine1910419364 [Google Scholar]
- 21.SimJ Neurosurg 1995822397815152 [Google Scholar]
- 22.Smith Clin Radiol. 1976;27:335. doi: 10.1016/s0009-9260(76)80085-2. [DOI] [PubMed] [Google Scholar]
- 23.Whitley Am J Roentgenol Radium Ther Nucl Med. 1960;83:633. [PubMed] [Google Scholar]
- 24.Woodring J Trauma. 1993;34:32. doi: 10.1097/00005373-199301000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Yetkin AJNR Am J Neuroradiol. 1985;6:633. [PMC free article] [PubMed] [Google Scholar]