Abstract
We studied the brace effect on the spinal profile in idiopathic scoliosis, using a MR procedure visualising the complete scoliotic spine in any vertical plane, while rotating it 180° on the longitudinal axis of the patient. Thirty-eight female patients (mean age, 14.5 years) were included in the study. Inclusion criteria were an idiopathic scoliosis, a Cobb angle greater than 20°, age of 10–17 years and bracing with a Chêneau brace. The brace effect was studied in 38 thoracic curves. The MR examinations were carried out in direct sequences, with and without brace. A reconstruction algorithm allows visualising the whole spine in vertical projections, with rotational steps of 2°, from −90° to 90°, referred to as MR animation. In various vertical MR projections, the changes of the curves were evaluated by measuring the Cobb angle. Additionally, a translation angle of the apical vertebra was determined, representing the lateral deviation of the apical vertebra from a defined midline. Testing the reproducibility of the Cobb angles, the standard deviation of the intra-individual differences was 1.7° and of the inter-individual differences, 2.1°. For the translation angles, the standard deviation of the intra-individual differences was 0.8° and of the inter-individual differences, 0.9°. With brace the mean Cobb angle of the thoracic curves was significantly reduced in the various vertical MR projections. The mean translation angle was also reduced. MR analysis showed that the brace effect is a translation process, straightening the profile of the scoliotic spine in all vertical planes. MR animation allows visualising the brace effect on the spine in scoliosis based on a 3D data set, without additional radiation exposure. It showed the straightening effect of the brace leading to a flattening of the sagittal spinal profile.
Keywords: Idiopathic scoliosis, Brace treatment, Magnetic resonance tomography
Introduction
Idiopathic scoliosis is a complex, three-dimensional (3D) deformity of the spine. The deformation is characterized by a primary lordosis, a secondary lateral curvature and a rotational component. Brace treatment is one option in the treatment of progressive curves. Although the use of spinal orthosis is documented in many studies, it is questionable, if the brace can restore the normal sagittal profile of the spine [1]. To study the brace effect on the sagittal, spinal profile in individual patients, an imaging technique visualising the brace effects based on 3D data without additional radiation exposure was needed.
In idiopathic scoliosis, magnetic resonance imaging (MRI) is used for the preoperative evaluation to exclude the presence of a syrinx or other intraspinal pathologies [2, 4]. The department of radiology at the University of Bonn developed the MR total spine imaging to reduce the radiation exposure in the follow-up of scoliosis patients [5, 10]. A further reconstruction algorithm allows visualising the whole spine in vertical projections with rotational steps of 2°, from −90° to 90°, referred to as MR animation. Using the MR animation we studied the brace effect on the spinal profile in idiopathic scoliosis.
Material and methods
Thirty-eight female patients (mean age 14.5 years±1.7 years) were included in the study. Inclusion criteria were an idiopathic scoliosis, a Cobb angle of more than 20°, age of 10–17 years and bracing with a Chêneau brace. Patients were excluded if they had a secondary scoliosis or if their braces were produced externally. There were 17 patients with a thoracic scoliosis and 21 with an s-shaped scoliosis. Therefore, 38 thoracic curves were investigated.
The Chêneau brace contains only few metallic parts, all of which were tested for ferromagnetism prior to the examination. Informed written consent was obtained from all patients/guardians.
MR examination
The MR examination was carried out in a standard supine position. The cervical and upper thoracic vertebrae and the lower thoracic and lumbar vertebrae were measured in two scans using a body coil. Measurements were carried out using a 1.5-T Gyroscan ACS-NT PowerTrak 6000 system (Philips Medical Systems, The Netherlands). Sixty-four slices with a reconstructed coronal and sagittal slice thickness of 2 mm were selected. Coronal and sagittal images were reconstructed from the cranial and caudal scans [5]. Using these acquisitions, further image processing was performed. Based on the axial data set, vertical projections of the spine were reconstructed in rotational steps of 2°, referred to as MR animation. Using this MR method the spine could be viewed in any vertical plane while rotating 180° along the longitudinal axis of the patient. Fig 1 shows various vertical projections of the same scoliosis. Average total acquisition time per measurement was 14 min and post-processing on a Pentium PC took approximately another 15 min.
Fig. 1.
Vertical MR projections of the whole spine by scoliosis. Rotational views of −90°, −70°, −40°, −20°, 0°, 20°, 40°, 70° and 90°
Evaluation of brace effect
The MR examinations were carried out in direct sequences, with and without brace. At first, the changes of the curves were evaluated by measuring the Cobb angle on the digitised MR images in the different vertical planes. In the 0° projection, the end vertebrae of the curve were determined. Between these end vertebrae, the Cobb angle was measured in the following vertical projections: −90°, −70°, −40°, −20°, 0°, 20°, 40°, 70° and 90°. The values of the Cobb angles were displayed in a line chart.
Additionally, we determined a translation angle of the apical vertebra. The translation angle represents the lateral deviation of the apical vertebra from a defined midline. The midline was the connecting line between the midpoints of C7 and L5. The angle was measured between the midline and the connecting line of the apical vertebra and L5. The measurements were done with a self-developed PC programme (SkolioOrg, copyright: König et al.). The midpoints of the vertebrae were selected with a precision cursor. The translation angle was measured in the vertical projections −90°, −70°, −40°, −20°, 0°, 20°, 40°, 70° and 90°. The values of the translation angles were displayed in a line chart.
Statistics
For statistical analysis the differences between the measurements with and without brace were tested by a non-parametric test (Wilcoxon rank sum test, statistic program SPSS for Windows). The level of significance (P) was set at 0.05.
Testing the reproducibility of the Cobb angles, 20 thoracic curves were measured in the vertical projection, at −90°, −70°, −20°, 0° and 70°, by two independent observers. The translation angles of the thoracic apical vertebra were also measured in 20 patients in the vertical projections −90° and 0° by two independent observers. Observer 1 repeated the measurements 4 weeks later. For the intra-observer and interobserver correlation, the mean differences with the standard deviation and the 95% confidence interval (CI) were calculated.
Results
The intra-observer correlation of the mean intra-individual Cobb angle differences was −0.05°±1.66° with a 95% CI of [−0.28; 0.18]. For the interobserver correlation, the mean of the differences was 0.16°±2.07° [−0.12; 0.45].
For the measurements of the translation angle, the mean of the intra-individual differences was 0.10°±0.75 with a 95% CI of [−0.06; 0.27]. The mean of the inter-individual differences was 0.13°±0.92 [−0.07; 0.33].
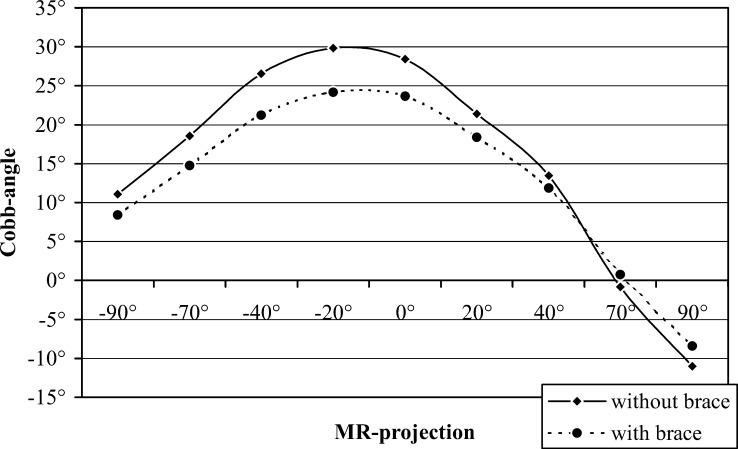
The line charts of the thoracic Cobb angles showed a reduction of the Cobb angles with a brace in all MR projections (Fig. 2). Most reduction was seen in the MR projections between −40° and 0°. Therefore, the brace primarily corrected the lateral curvature of the deformity. The coronal 0° projection simulates the anterior-posterior X-ray projection. In 37 of the 38 thoracic curves, the Cobb angle was reduced, and it showed no change in one patient. On average the thoracic curve was reduced by 17% in the 0° projection.
Fig. 2.
Line chart of the Cobb angles of the thoracic curves (n=38) with and without brace. It shows a reduction of the Cobb angles with brace in the various MR projections
We also observed a significant reduction of the Cobb angles with the brace in the −70° and −90° MR projections (Table 1). With the −90° projection simulating a lateral X-ray projection, this reduction corresponds to a flattening of the sagittal spinal profile. In 33 thoracic curves the Cobb angle was reduced, in three curves the Cobb angle was constant and in two curves it increased. On average, the thoracic Cobb angle was reduced by 24% in this sagittal projection (Table 2).
Table 1.
Mean Cobb angles of the thoracic curves with and without brace
| MR projection | Cobb angles of the thoracic curves, n= 38 | |||||
|---|---|---|---|---|---|---|
| (1) Without brace | (2) With brace | Difference (1)− (2) | ||||
| Mean | Standard deviation | Mean | Standard deviation | Mean | Standard deviation | |
| −90° | 11.1 | 5.9 | 8.4 | 6.4 | 2.7a | 2.1 |
| −70° | 18.5 | 5.6 | 14.8 | 5.9 | 3.8a | 2.9 |
| −40° | 26.5 | 7.3 | 21.2 | 8.0 | 5.3a | 3.2 |
| −20° | 29.9 | 8.3 | 24.1 | 8.5 | 5.7a | 3.0 |
| 0° | 28.4 | 8.3 | 23.6 | 8.5 | 4.8a | 3.0 |
| 20° | 21.4 | 8.5 | 18.4 | 8.4 | 3.0a | 2.3 |
| 40° | 13.5 | 7.9 | 11.9 | 8.0 | 1.6a | 2.4 |
| 70° | −0.8 | 1.2 | 0.8 | 1.1 | −1.6a | 0.4 |
| 90° | −11.0 | 5.9 | −8.4 | 6.3 | −2.6a | 2.1 |
aSignificant difference, p< 0.05
Table 2.
Mean translation angles of the thoracic apical vertebra with and without brace
| MR projection | Translation angles of the thoracic apical vertebra, n= 38 | |||||
|---|---|---|---|---|---|---|
| (1) Without brace | (2) With brace | Difference (1)−(2) | ||||
| Mean | Standard deviation | Mean | Standard deviation | Mean | Standard deviation | |
| −90° | 4.0 | 2.7 | 3.2 | 2.6 | 0.9a | 1.2 |
| −70° | 5.6 | 2.4 | 4.6 | 2.4 | 0.9a | 1.6 |
| −40° | 6.5 | 2.2 | 5.4 | 2.1 | 1.1a | 1.1 |
| −20° | 5.9 | 2.3 | 4.8 | 2.3 | 1.0a | 1.3 |
| 0° | 4.5 | 2.6 | 3.8 | 2.5 | 0.8a | 1.2 |
| 20° | 3.0 | 3.1 | 2.5 | 2.8 | 0.5a | 1.2 |
| 40° | 0.9 | 3.2 | 0.8 | 3.0 | 0.2 | 1.4 |
| 70° | −2.0 | 3.0 | −1.6 | 2.9 | −0.4 | 1.3 |
| 90° | −4.0 | 2.7 | −3.3 | 2.6 | −0.8a | 1.3 |
aSignificant difference, p<0.05
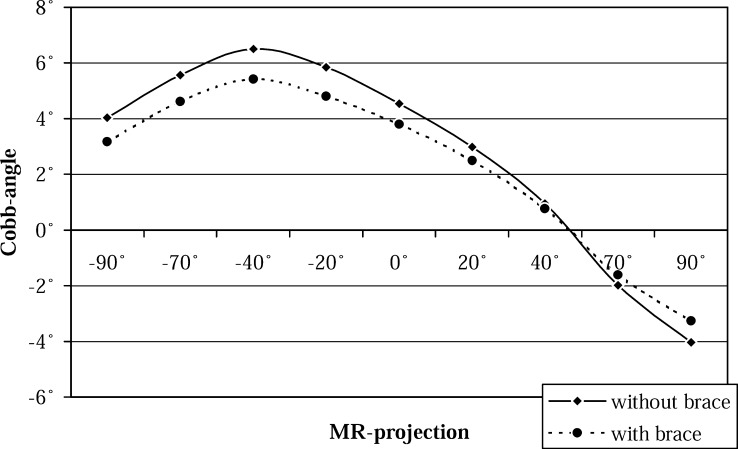
The line chart of the translation angles of the thoracic apical vertebra showed a reduction with the brace in all projections (Fig. 3). Therefore, the brace leads to a straightening of the thoracic spine in all vertical planes (Fig. 4). The translation angle was primarily reduced in the projections from −20° to 40°. In the 0° projection the mean reduction was 18%, and in the −90° projection, 23%.
Fig. 3.
Line chart of the translation angles of the thoracic apical vertebra (n=38) with and without brace. Showing brace reduction of the translation angles in the various MR projections
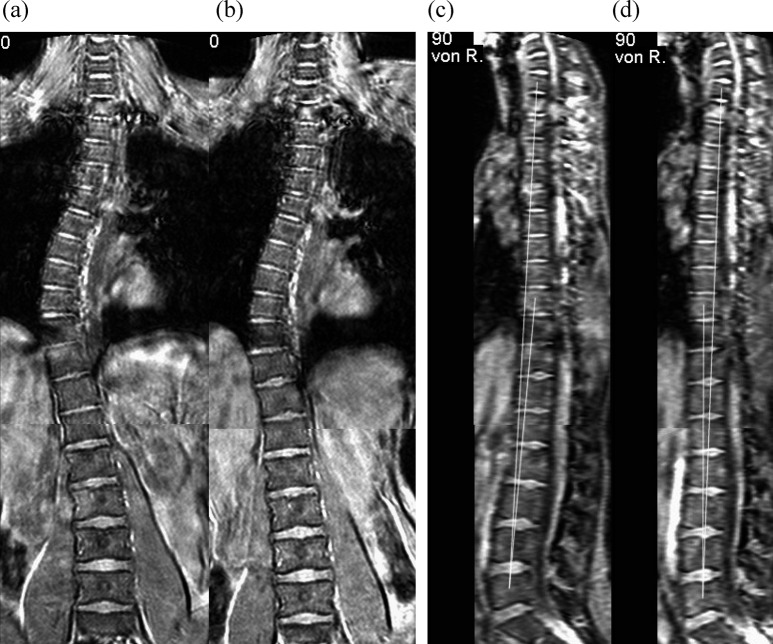
Fig. 4.
MR animation of thoracic scoliosis. 0° projection without a and with b brace and 90° projection without c and with d brace. The translation angle in the 90° projection changes from +3° without brace to −3° with brace, showing the lordotic effect on the sagittal profile
The changes of the Cobb angles and the translation angles with a brace were independent of the type of scoliosis. Between the thoracic scoliosis and the s-shaped scoliosis there was a high correspondence of the mean differences of the Cobb angles and the translation angles, with and without brace, with correlation coefficients of 0.98 and 0.84, respectively (p<0.01).
Discussion
The outcome of brace treatment is generally documented on the conventional X-ray in the frontal plane of the patient. But this anteroposterior view actually shows an oblique view of the scoliotic deformity. Stagnara defined with du Peloux the plane of choice as the frontal plane of the apical curve [3]. But there is not one single plane that the deformity can be depicted in as each vertebra is increasingly tilted and twisted. Each vertebra has its corresponding frontal and lateral plane of view. These planes, however, can be accurately depicted utilizing MR animation.
The MR investigation is carried out in the supine position. On the conventional X-ray, the brace effect is documented in the standing position. However, it is useful to examine the brace effect in the supine position, because the standing position increases the Cobb angle due to the static influences [11]. In standing position, the brace also has to correct the static component of the curve magnitude. Therefore, in the supine position we measure the direct correction of the deformity itself. A second reason for measuring in the supine position is that wearing the brace at night is an essential part of treatment.
Using the MR animation, the complex scoliotic deformity can be depicted on the basis of a 3D data set in 2D vertical projections. The scoliotic curves can be viewed in any vertical plane while rotating 180° along the longitudinal axis of the patient. The vertical projection allows a simple measurement of the curve magnitude using the Cobb angle method. In comparison with procedures generating three-dimensional spine models, the MR animation provides a direct imaging of the whole scoliotic spine [7, 8].
To analyse the brace effect we measured the Cobb angle and a translation angle in various vertical projections. The translation angle shows the lateral deviation of the apical vertebra from a spinal midline. The reproducibility of both angles was sufficient. The mean differences with and without brace had a high correlation for the intra-individual and inter-individual comparison. Pruijs et al. [9] reported the interobserver variability of the Cobb angle measurements on conventional X-rays with a standard deviation of 2.0°. On the MR projections the standard deviation of the inter-individual differences was 2.1° for the Cobb angles and 0.9° for the translation angles.
The MR analysis shows that the brace effect is a translation process. The brace applies a laterodorsal force to the spine, moving the spine forward and leading to a straightening of the scoliotic spine in the coronal and sagittal plane. Especially for the thoracic curves, the Cobb angles and the translation angles were reduced in the coronal and sagittal plane. Therefore, the brace corrects the lateral curvature but also results in a flattening of the sagittal spinal profile.
Our results are confirmed by other studies that have showed that brace treatment had a lordotic effect on the thoracic kyphosis [6, 7]. At this time, MR animation is a new procedure with a potential for use in monitoring the brace effect in scoliosis. We cannot give precise data about the cost until the method is routinely involved in the MRI unit. But it would certainly be more than a conventional X-ray. Further studies are necessary before clinical application can be recommended.
Conclusion
The introduced MR method allows studying the brace effect on the spinal profile in scoliosis, based on a 3D data set without any radiation exposure. The MR animation shows that the brace had a straightening effect on the thoracic spine, leading to a flattening of the sagittal profile.
References
- 1.Dickson J Bone Joint Surg Br. 1999;81:193. doi: 10.1302/0301-620X.81B2.9630. [DOI] [PubMed] [Google Scholar]
- 2.Do J Bone Joint Surg Am. 2001;83:577. doi: 10.2106/00004623-200104000-00014. [DOI] [PubMed] [Google Scholar]
- 3.du Rev Chir Orthop Reparatrice Appar Mot. 1965;51:517. [PubMed] [Google Scholar]
- 4.Hausmann Eur Spine J. 2003;12:501. doi: 10.1007/s00586-003-0568-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Konig Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr. 1999;170:258. [PubMed] [Google Scholar]
- 6.Korovessis Spine. 2000;25:2064. doi: 10.1097/00007632-200008150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Labelle Spine. 1996;21:59. doi: 10.1097/00007632-199601010-00013. [DOI] [PubMed] [Google Scholar]
- 8.Perie D, Sales De Gauzy J, Sevely A, Hobatho MC (2001) In vivo geometrical evaluation of Chêneau-Toulouse-Munster brace effect on scoliotic spine using MRI method. Clin Biomech (Bristol, Avon) 16:129–137 [DOI] [PubMed]
- 9.Pruijs Skeletal Radiol. 1994;23:517. doi: 10.1007/BF00223081. [DOI] [PubMed] [Google Scholar]
- 10.Schmitz Eur Spine J. 2001;10:114. doi: 10.1007/s005860100250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.TorellSpine 1985104254049109 [Google Scholar]