Abstract
OBJECTIVE
To characterize the costs and cost-effectiveness of a telephonic behavioral intervention to promote glycemic control in the Improving Diabetes Outcomes study.
RESEARCH DESIGN AND METHODS
Using the provider perspective and a time horizon to the end of the 1-year intervention, we calculate the costs of a telephonic intervention by health educators compared with an active control (print) intervention to improve glycemic control in adults with type 2 diabetes. We calculate the cost-effectiveness ratios for a reduction of one percentage point in hemoglobin A1c (A1C), as well as for one participant to achieve an A1C <7%. Base-case and sensitivity analysis results are presented.
RESULTS
The intervention cost $176.61 per person randomized to the telephone group to achieve a mean 0.36 percentage point of A1C improvement. The incremental cost-effectiveness ratio was $490.58 per incremental percentage point of A1C improvement and $2,617.35 per person over a 1-year intervention in achieving the A1C goal. In probabilistic sensitivity analysis, the median (interquartile range) of per capita cost, cost per percentage point reduction in A1C, and cost per person achieving the A1C goal of <7% are $175.82 (147.32–203.56), $487.75 (356.50–718.32), and $2,312.88 (1,785.58–3,220.78), respectively.
CONCLUSIONS
The costs of a telephonic intervention for diabetes self-management support are moderate and commensurate to the modest associated improvement in glycemic control.
The goal for glycemic control for most individuals with type 2 diabetes is a hemoglobin A1c (A1C) of <7% (1); however, more than 40% of individuals with diabetes in the U.S. do not reach this goal (2). Implementation of a diabetes management plan should include clinical care, diabetes self-management education, and ongoing support (1). Most individuals with diabetes report lack of or access challenges for receiving diabetes self-management education or support (3,4). Several studies have reported self-management education and support delivered in the community by community peer educators (5,6), by Web-based applications (7), or by telephone (8,9). A telephonic intervention delivered by health educators was successful for a poor, urban, bilingual diabetes population for a single behavior, such as going for a dilated eye examination for retinopathy screening (10), and at a moderate cost (11). This telephonic behavioral counseling intervention was broadened in the Improving Diabetes Outcomes (I DO) study to promote change in multiple behaviors, including medication adherence, healthy eating, and increased physical activity (12,13). Information about the costs of such an intervention is necessary for knowledgeable translation of the intervention to the broad community.
RESEARCH DESIGN AND METHODS
The I DO study was a randomized controlled trial of a behavioral telephonic intervention delivered by health educators with improvement in glycemic control as the primary outcome in adults with type 2 diabetes. All randomized participants received selected diabetes self-management print materials in English or Spanish, as requested (12). The telephonic intervention successfully led to a significantly greater decrease in A1C compared with the active control (print) group (13). I DO study baseline data and methods (12) and main results (13) have been published previously. In summary, these 526 lower-income, urban adults with type 2 diabetes and a baseline A1C ≥7.5%, were members/spouses in a health care workers’ union; as such, they received full health care coverage, including medications. They were 62% non-Hispanic black and 23% Hispanic, and 77% were foreign-born. Those randomized to the telephone group (n = 262) were assigned to a health educator for up to 10 self-management support phone calls to discuss self-management as found in the print materials mailed to them. Those randomized to the print group (n = 264) received only the print materials. At the end of the 1-year intervention, the primary outcome, change in A1C, showed a mean (95% CI) decrease of 0.36% (0.02–0.69) more in the telephone group than in the print group (P = 0.04). Adjusted for baseline A1C, the mean reduction in A1C for the telephone group compared with the print group was 0.42% (0.11–0.73; P = 0.008).
Here we present a cost accounting and cost-effectiveness analysis of that intervention. Our perspective is that of a provider of health services, and our time horizon is the duration of the intervention of up to 1 year. Because all costs and effects occurred within 1 year, no discounting was applied in these analyses. The telephonic intervention group received up to 10 telephone calls from a health educator, one call every 4–6 weeks, in addition to the same print diabetes self-management education materials that were sent to the print (active control) group. Therefore, the incremental costs for the telephone group are those associated with the telephonic intervention itself. These costs are characterized as labor costs for the health educators making the telephone calls, labor costs for the supervision and training of the health educators by a nurse diabetes educator, and direct telephone use charges.
The labor of the health educators consisted of several components: time spent on attempted and completed telephone calls, record review and preparation in advance of each call, and documentation after completed calls. Average completed call time per person was abstracted from electronic study work logs that noted the start and end time of each call. The number of incomplete call attempts was estimated from a random sample and stratified on the number of completed calls, based on paper work logs recording this activity. All completed calls and incomplete call attempts were assumed to require an additional 5 min of record review and preparation before each call. Record updating after completed calls was assumed to require yet another 5 min. These times were estimated by consensus of the health educators and their nurse supervisor as being representative across participants.
The health educators, by study design, were not certified or licensed health professionals. They were college-educated community members who were trained for ∼2 weeks by the supervisory nurse, who was a certified diabetes educator in diabetes self-management support and counseling skills as well as in the skills needed to monitor a research protocol and collect accurate data. They were supervised daily and had continuing education by weekly case management in counseling skills and study protocol. The main emphases for subjects’ behavior change during the telephone calls were diabetes medication adherence, healthy eating, and increasing physical activity to improve diabetes control (12,13).
We identified average U.S. wages for these health educators and for their nurse supervisor from the on-line database of the U.S. Department of Labor’s Bureau of Labor Statistics’ National Compensation Survey for 2009 (the latest year available) (14). For our base-case analysis, the labor of the health educators (level 7) was evaluated at $18.26/h plus 28% fringe benefits. Supervisor time for training and supervision was estimated as 1 h for each 20 h of health educator time. Supervisor wages were estimated as $41.41/h (level 10 nurse health educator) plus 28% fringe benefits. Telephone charges were estimated at $0.05 for each call initiated (whether completed or not) plus $0.10/min for completed calls. Total costs were computed as the sum of labor and telephone costs.
Two measures of health effect were used for the cost analyses: 1) the mean decrease in A1C measurement between the beginning and end of the intervention period and 2) the proportion of participants achieving a target A1C value of <7% (A1C goal). Incremental cost-effectiveness ratios (ICERs) for each of these effects were calculated using the standard formula: ICER = [telephone group total costs – print group total costs]/[telephone group outcome – print group outcome] (15).
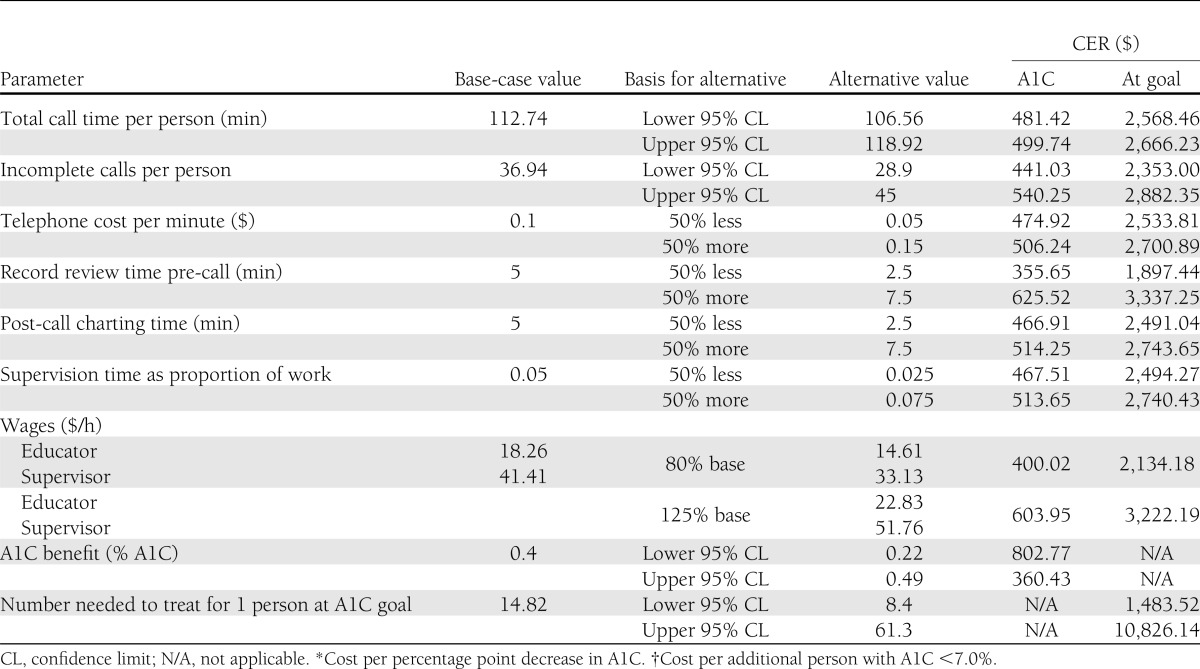
To assess the effect of uncertainty in our assumptions, we performed one-way and probabilistic sensitivity analyses, enabling us to estimate the effects of all of the uncertain assumptions on our findings. For the one-way sensitivity analyses, parameters that were estimated from data gathered in the study were ranged over their 95% CIs. Parameters that were assumptions were allowed to vary ±50% from their baseline values. Wage parameters, which were extracted from a national database, were varied between 80 and 125% of their baseline values.
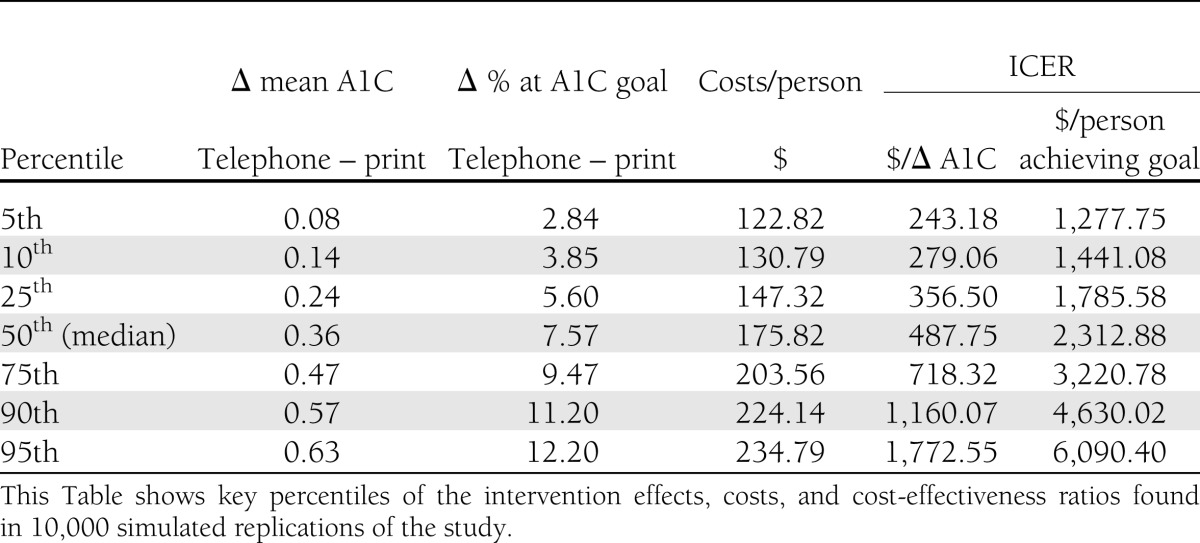
In the probabilistic sensitivity analysis, uncertainty about the number telephone calls, call attempts made, and health effects was captured through bootstrap resampling of the study database (16). Uncertainty in wage rates for health educators and nurse supervisors was modeled by a bivariate normal distribution with means equal to base-case values, SDs of $2 and $4 per hour, respectively, and a correlation coefficient of 0.14. With these SD, the upper and lower limits used in the one-way sensitivity analyses of wages were close to the 5th and 95th percentiles of the distributions in the probabilistic sensitivity analysis. The correlation coefficient of 0.14 was calculated from data on U.S. wages for a variety of jobs over time (17). Other than these wages, all parameters were sampled independently. We simulated 10,000 replications of the I DO study, each with its own cost components and effects drawn from these distributions, calculated the corresponding total costs and cost-effectiveness ratios, and tracked the resulting distributions of costs, effects, and cost-effectiveness ratios.
Our cost model is simple accounting of costs over a short-term period, so no models of asset depreciation or the like were required. Our health outcomes are taken from one randomized controlled trial, so no synthesis of diverse epidemiologic and clinical studies needed to be modeled. Owing to the simplicity and transparency of this model, we did not investigate the sensitivity of the ICERs to model structure.
RESULTS
Base case
On average, each telephone group participant received 7.9 (SEM, 0.1) completed telephone calls, encompassing 112.7 (7.9) minutes of contact time. In addition, an average of 36.9 (4.0) incomplete call attempts (for up to 10 intervention calls by protocol) per person were made; these included additional contact numbers and cellular telephones. Applying the factors above, telephone charges averaged $13.51 per person, educator labor costs averaged $146.49 per person, and supervisory labor costs averaged $16.61 per person. Incremental costs per person for the telephonic intervention were $176.61. The print intervention, also given to the telephone group, cost $4.00 per person for the educational materials, postage, and handling. Thus, the total cost of the intervention for the telephone group was $180.61 per person.
As reported by Walker et al. (13), the mean difference in A1C change between the telephone and print groups was 0.36 percentage points of A1C. Therefore, assuming the mean cost per fractional A1C percentage point can be linearly extrapolated, the ICER is $490.58 per percentage point in A1C improvement.
The study eligibility criterion was A1C ≥7.5%, and mean preintervention A1C was 9.2%. In the telephone group, 11.8% of the 228 participants attained A1C ≤7% at the end of the study, whereas only 5.1% of 216 print group participants did so. Thus, the intervention resulted in 1 additional person with A1C <7% for every 15 people receiving it. With a per capita intervention cost over the print group of $176.61, the ICER is $2,617.35 per additional person achieving the A1C goal.
Sensitivity analyses
The results of one-way sensitivity analyses are reported in Table 1. Most of the parameter changes do not materially modify the ICERs. Of the resources used for the intervention, the ICERs are most sensitive to the amount of time spent reviewing records before calling patients. This reflects that this effort must be made even before an incomplete call attempt and is often repeated, probably contributing little or nothing to the health outcome. By contrast, time required to make record notes after calls is incurred only after a completed call, so the time needed for each such activity has much less impact on study costs. The parameters that most affect cost-effectiveness ratios, however, are not program resources but the actual health effects achieved. The great sensitivity of the cost-effectiveness ratio to outcome reflects the range of uncertainty in study outcomes themselves, particularly for the number needed to treat to achieve the A1C goal. It should be born in mind that the average effect of any intervention targeting A1C is likely to be of the order of magnitude of ≤1%, so that attaining the A1C goal is unlikely for people starting out with A1C of ≥9%. With ∼40% of our participants having a baseline A1C ≥9%, the proportion who achieved the goal in either group was, as already noted, fairly small, so that the group difference (and, hence, its reciprocal, the number needed to treat) is estimated with limited precision in a study this size.
Table 1.
One-way sensitivity analyses
The probabilistic sensitivity analysis gives a more comprehensive picture of the uncertainty of the ICERs because it takes into account the uncertainty of all of the assumptions about the parameters while still properly representing the low probability that several parameters will simultaneously take on extreme values. Table 2 provides key percentiles of the simulated distributions of I DO effects, costs, and cost-to-effectiveness ratios. The median ICER of $487.75 for change in A1C and $2,312.88 for those who achieved the A1C goal are close to the base-case ICERs, as expected. In 90% of replications, the ICER for change in A1C falls between the 5th and 95th percentiles, to wit $243.18 and $1,772.55, and the ICER for persons achieving the A1C goal, between $1,277.75 and $6,090.40. In addition, we note that in 1.8% of the simulated study replications, the print group achieved lower mean A1C levels than the telephone group, and in 0.4% the print group achieved a higher rate of achieving the A1C goal.
Table 2.
Probabilistic sensitivity analysis
Decision makers may have threshold values for the ICER, below which they consider an intervention acceptable. In the current situation, if a decision maker’s threshold were, say, $1,000 per percentage point improvement in A1C, we see from Table 2 that the probability that our intervention meets that cost-effectiveness limit is close to 90%. (The actual probability is 87%.)
CONCLUSIONS
We have found that the incremental per capita costs of the telephonic intervention, $176.61, were modest. Each additional percentage point reduction in A1C and each additional person attaining the A1C goal of <7% cost, respectively, $490.58, and $2,617.35. The cost-effectiveness ratios are robust to most of our assumptions in sensitivity analysis. The largest single source of uncertainty was the CI around the actual A1C effect observed in the trial. Even in probabilistic sensitivity analysis, where all uncertain assumptions vary simultaneously, the 95th percentile ICER exceeds the base-case estimate only by approximately a factor of two. Our findings supplement the earlier report of the clinical effectiveness of the I DO telephonic (13) intervention with estimates of its cost and cost-effectiveness.
Studies of behavioral interventions to improve glycemic control have had varying results. For example, Frosch et al. (18) tested an intervention consisting of an educational DVD and booklet combined with up to 2.5 h of telephonic coaching and motivational enhancement by a nurse educator over 6 months. A control group received a diabetes self-management brochure developed by the National Diabetes Education Program. Of recent reported studies, their intervention is most similar to ours. At the end of 6 months, both groups showed substantial improvement in A1C, but the improvements in A1C in the two groups were similar (∼0.5% A1C) and the difference was not statistically significant (18). Our findings may differ because of differences in A1C inclusion criteria (≥8% A1C vs. ≥7.5% in the I DO study), length of the intervention (6 vs. 12 months in the I DO study), counseling techniques, or details of intervention implementation. There was no cost analysis associated with their study.
For simplicity, we framed one of our effectiveness outcomes as cost per percentage point reduction in A1C. The observed difference in mean A1C change between groups in our study, however, was 0.36 percentage points. One might, therefore, denominate the cost-effectiveness ratio in this unit of change: $176.61 per 0.36 percentage point A1C improvement, as a full percentage point improvement in A1C was not, on average, achieved with this intervention. We do not know whether or how this modality of intervention might be amplified to achieve that average level of improvement in glycemic control or whether the costs per fractional percentage point in A1C improvement can be linearly extrapolated.
Cost-effectiveness ratios are readily used to compare different interventions that produce the same outcome. The ICER then becomes, in effect, a unit price, a measure of value for money. There is no broadly accepted threshold of cost-effectiveness per unit of change in A1C or per person achieving A1C ≤7%, but we can compare our findings with other studies that have calculated cost-effectiveness ratios in these units.
Overall, our costs per person are moderate, as are the costs per percentage point reduction in A1C and per person achieving A1C goal. For comparison, Patel et al. (19) studied motivational enhancement and cognitive behavioral therapy delivered by nurses trained in these techniques to improve outcomes in patients with diabetes in the U.K. The combination of those two interventions reduced A1C by 0.45 percentage points, a somewhat larger effect than we obtained. But the cost-effectiveness ratio was £1,765 ($2,824 at current exchange rates) per percentage point of A1C reduction (19), making our intervention far more cost-effective than theirs. Another recently published study reported the cost evaluation of a diabetes self-management intervention for Latinas (20) that was considerably more intensive (including in-person visits and counseling from licensed health care professionals) than the I DO study. It was also a little more costly per capita, $184 per person in the in-person treatment group. The health effect they targeted was increased consumption of fruits and vegetables, not change in A1C. Accordingly, their cost-effectiveness ratios are not directly comparable with ours. The authors, however, included recommendations to consider using the telephone as a means to maintain effectiveness, reduce costs, and increase the reach of a self-management support program to many more who might benefit from it (20).
We believe that the use of health educators, not trained as clinicians, in our intervention restrained the cost of our program, while the continuing education and rigorous supervision by a nurse diabetes educator bolstered the quality and effectiveness of the intervention.
Our study has several limitations. First, we do not know how long the effects of the I DO telephonic intervention persist; continuing phone contact or intermittent “boosters” might be required to sustain the improvements achieved. Access to follow-up A1C data for all study participants or to intervene after the 1-year intervention was outside the scope of our study. Accordingly, we restricted the time horizon of our analysis to the intervention period itself and cannot estimate cost-utility ratios based on quality-adjusted life-years. Research on the durability of the intervention effect and long-term health outcomes would facilitate cost-utility analysis.
Second, the optimal implementation of interventions like ours is not known. A briefer intervention with fewer calls might have achieved much of the benefit we realized, or a longer intervention might have promoted behavior change for some of the participants who did not benefit during the 1-year intervention. Our study and analysis shed no light on these possible improvements or their economic implications; further data are necessary to resolve those questions.
A third limitation is the generalizability of our study sample. Although participants were lower-income with racial and ethnic diversity, they did all have the benefit of health care coverage by virtue of their employment and union benefits.
Our perspective is that of a health care organization providing services to these patients: during the study we did not collect information about intervention-related time, effort, expenses incurred by the participants and their families and caregivers, or health services utilization.
Our cost estimates exclude supplies, office space for intervention personnel, and storage space for records because we believe this type of intervention would normally be implemented using existing staff and facilities. For the same reason, we did not include start-up costs, such as staff recruitment, in our analysis. Protocol development time in a nonresearch context is difficult to estimate, but we believe it would be small; and as a one-time, up-front cost, when allocated over all patients, we think it would be trivial. Implementation of the intervention does not require development or special maintenance of any data systems that would not already be operational in a health care setting, so we allocated no costs for this.
Following standard practice of reporting ICERs, we did not include the cost of the print materials and postage that were common to both study arms in our cost-effectiveness ratio calculations. At $4 per person, this would be an additional cost to a provider implementing this intervention in settings with nothing similar to the print intervention already in place. In that situation, the simultaneous implementation of two interventions might lead to improvement in glycemic control different from what was observed in our study. The I DO study did not include a no-intervention (control) group, for ethical reasons, because diabetes self-management education is a standard of care (1,3), and because most providers of diabetes care already furnish print materials or access to on-line resources similar to our print materials. Accordingly, although we have reported the total cost along with the incremental cost, we can estimate neither an effect nor a cost-effectiveness ratio for the simultaneous implementation of print and telephonic interventions in a context currently offering neither.
In summary, the I DO study results suggest that a modest improvement in A1C can be achieved at a moderate cost using a telephonic intervention conducted by health educators trained and supervised by a nurse certified diabetes educator.
Acknowledgments
This study was supported by National Institutes of Health grants R18 DK-62038 and DK-020541.
No potential conflicts of interest relevant to this article were reported.
C.B.S. contributed to every aspect of this article. H.W.C. and E.A.W. contributed to the study design, discussion, analysis, and writing of the manuscript. C.S. contributed to the study design and the editing of the manuscript. C.B.S. is the guarantor of this work, and as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the data contributions of Ralph Ullman and Fionnuala King of the 1199SEIU Benefit and Pension Funds; their talented health educators, including Giovanna DiFrancesca, Kathleen McCabe, Gisela Mojica, Jennifer Case, Tara DeWitt, Gabriel Ferreira, Marlene Taveras, Samara Lipsky, Dr. Hollie Jones, and Hector Cariello; data management support from Maria Kalten and Jennifer Lukin, all staff from the Albert Einstein College of Medicine; and especially, the participants in New York City who volunteered for the study.
References
- 1.American Diabetes Association Standards of medical care in diabetes—2011. Diabetes Care 2011;34(Suppl. 1):S11–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care 2008;31:81–86 [DOI] [PubMed] [Google Scholar]
- 3.Funnell MM, Brown TL, Childs BP, et al. National standards for diabetes self-management education. Diabetes Care 2010;33(Suppl. 1):S89–S96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peyrot M, Rubin RR. Access to diabetes self-management education. Diabetes Educ 2008;34:90–97 [DOI] [PubMed] [Google Scholar]
- 5.Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med 2010;153:507–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brownson CA, Heisler M. The role of peer support in diabetes care and self-management. Patient 2009;2:5–17 [DOI] [PubMed] [Google Scholar]
- 7.Glasgow RE, Kurz D, King D, et al. Twelve-month outcomes of an internet-based diabetes self-management support program. Patient Educ Couns 2011;87:81–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: a randomized, controlled trial. Med Care 2000;38:218–230 [DOI] [PubMed] [Google Scholar]
- 9.Wennberg DE, Marr A, Lang L, O’Malley S, Bennett G. A randomized trial of a telephone care-management strategy. N Engl J Med 2010;363:1245–1255 [DOI] [PubMed] [Google Scholar]
- 10.Walker EA, Schechter CB, Caban A, Basch CE. Telephone intervention to promote diabetic retinopathy screening among the urban poor. Am J Prev Med 2008;34:185–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schechter CB, Basch CE, Caban A, Walker EA. Cost effectiveness of a telephone intervention to promote dilated fundus examination in adults with diabetes mellitus. Clin Ophthalmol 2008;2:763–768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen HW, Shmukler C, Ullman R, Rivera CM, Walker EA. Measurements of medication adherence in diabetic patients with poorly controlled HbA(1c). Diabet Med 2010;27:210–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker EA, Shmukler C, Ullman R, Blanco E, Cohen HW. Results of a successful telephonic intervention to improve diabetes control in urban adults: a randomized trial. Diabetes Care 2011;34:2–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.United States Department of Labor. Bureau of Labor Statistics. National Compensation Survey [Internet]. Available from http://data.bls.gov/cgi-bin/dsrv?nw. Accessed 14 February 2011.
- 15.Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. 3rd ed. Oxford, Oxford University Press, 2006 [Google Scholar]
- 16.Efron B, Tibshirani RJ. An Introduction to the Bootstrap. Boca Raton, FL, CRC Press, 1994 [Google Scholar]
- 17.Freeman RB, Oostendorp RH. Occupational Wages of the World Database [Internet]. Available from http://www.nber.org/oww/. Accessed 3 March 2012.
- 18.Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med 2011;171:2011–2017 [DOI] [PubMed] [Google Scholar]
- 19.Patel A, Maissi E, Chang H-C, et al. Motivational enhancement therapy with and without cognitive behaviour therapy for type 1 diabetes: economic evaluation from a randomized controlled trial. Diabet Med 2011;28:470–479 [DOI] [PubMed] [Google Scholar]
- 20.Ritzwoller DP, Sukhanova AS, Glasgow RE, et al. Intervention costs and cost effectiveness for a multiple risk factor diabetes self-management trial for Latinas: economic analysis of ¡Viva Bien! Tranl Behav Med 2011;3:427–435 [DOI] [PMC free article] [PubMed] [Google Scholar]