Abstract
OBJECTIVE
To examine whether baseline pulse pressure (PP), a marker of arterial stiffness, is associated with subsequent development of atrial fibrillation (AF) in type 2 diabetes.
RESEARCH DESIGN AND METHODS
A total of 350 type 2 diabetic patients, who were free from AF at baseline, were followed for 10 years. A standard electrocardiogram was performed annually and a diagnosis of incident AF was confirmed in affected participants by a single cardiologist.
RESULTS
During the follow-up, 32 patients (9.1% of total) developed incident AF. After adjustments for age, sex, BMI, diabetes duration, presence of left ventricular hypertrophy, hypertension treatment, kidney dysfunction, and pre-existing history of coronary heart disease, heart failure, and mild valvular disease, baseline PP was associated with an increased incidence of AF (adjusted odds ratio 1.76 for each SD increment [95% CI 1.1–2.8]; P < 0.01).
CONCLUSIONS
Our findings suggest that increased PP independently predicts incident AF in patients with type 2 diabetes.
Atrial fibrillation (AF) is the most common sustained arrhythmia and contributes to substantial increases in morbidity and mortality (1–3). Increased pulse pressure (PP), a marker of arterial stiffness, has been reported to be an important predictor of new-onset AF in U.S. adults, independently of several clinical AF risk factors (4). In this prospective, observational study, we tested the hypothesis that baseline PP predicts subsequent development of incident AF in patients with type 2 diabetes.
RESEARCH DESIGN AND METHODS
A total of 350 type 2 diabetic outpatients, who were free from AF at baseline, were followed for 10 years. They were randomly selected among those who regularly attended our diabetes clinic during 2000–2001 (n= 1,918) after exclusion of those who had a history of AF, atrial flutter, hyperthyroidism, or moderate-to-severe valvular heart disease and those who were taking antiarrhythmic drugs. Participants were seen every 6–12 months for medical examinations of glycemic control, chronic diabetes complications, and routine electrocardiograms (ECGs). The ascertainment at the end of follow-up (January 2011) for the sample was 100%. The local ethics committee approved the study protocol. All participants gave their informed consent.
Pre-existing history of coronary heart disease, congestive heart failure (CHF), and mild valvular heart disease was confirmed by reviewing hospital medical records, including diagnostic symptoms patterns, echocardiograms, and other laboratory results. Presence of left ventricular hypertrophy (LVH) was diagnosed on the basis of a standard 12-lead ECG according to Sokolow-Lyon voltage criteria and/or Cornell voltage criteria (5).
During the follow-up, participants were diagnosed with AF if AF or atrial flutter was present on an ECG that was obtained from hospital or physician chart or from a routine clinic examination in our clinic (i.e., a 12-lead ECG was performed yearly in all participants. A single, experienced cardiologist, who was blinded to subjects’ details, confirmed the diagnosis of incident AF in affected participants.
Statistical analysis
One-way ANOVA, the Kruskal-Wallis test, and the χ2 test were used to compare the baseline characteristics of participants stratified by tertiles of baseline PP. Multivariate logistic regression analysis was used to separately examine the independent associations between the various components of blood pressure (systolic blood pressure, PP, or mean blood pressure, which were included in separate regression models as continuous variables, i.e., per 1-SD increment in each variable) and incident AF.
RESULTS
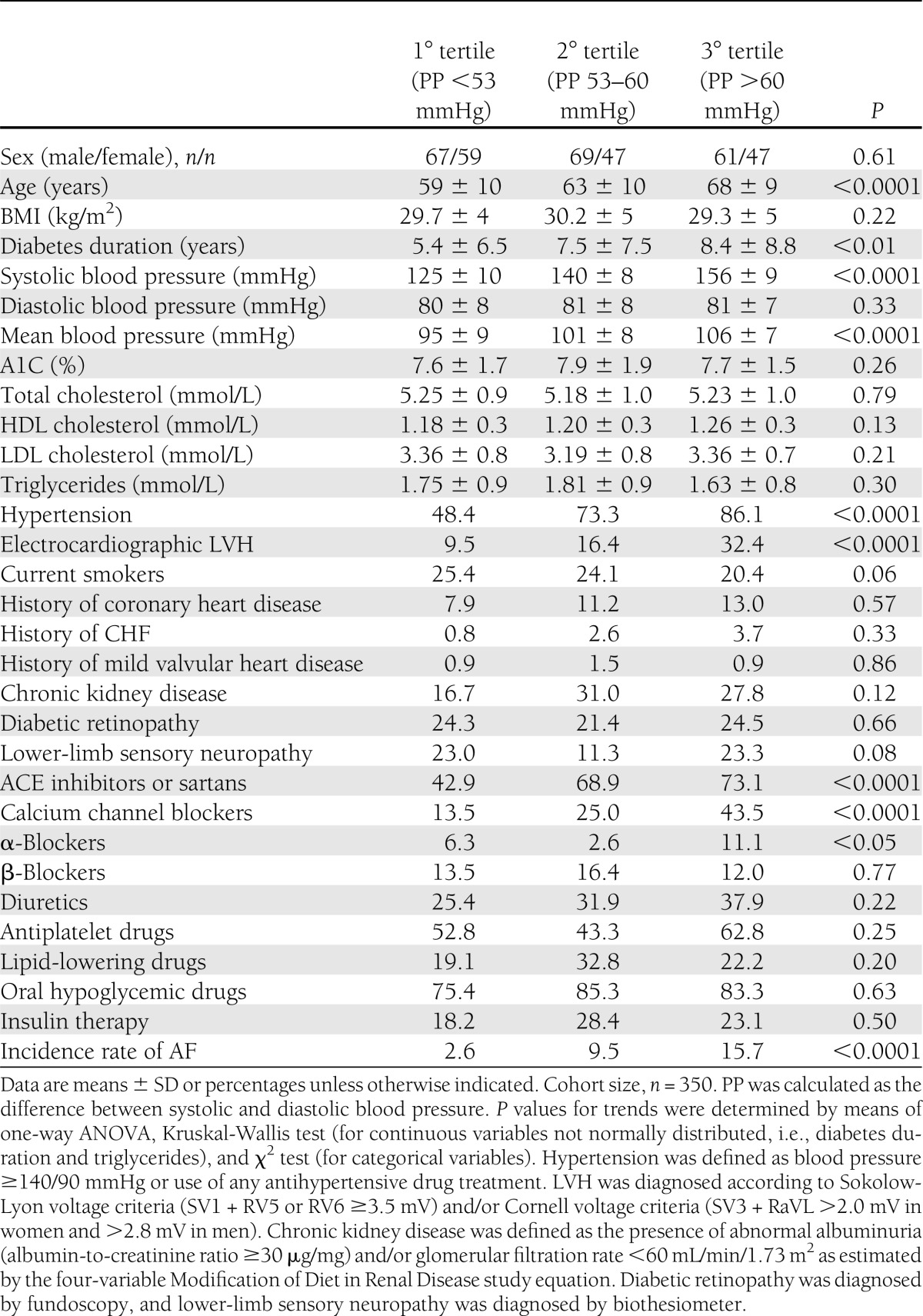
In the whole sample, age, diabetes duration, and A1C averaged 63 years, 6 years, and 7.7 %, respectively. Mean (SD) values of systolic blood pressure, PP, and mean blood pressure were 140 ± 15.2, 59.1 ± 12.8, and 100.7 ± 8.8 mmHg, respectively. Baseline characteristics of participants stratified by PP tertiles are displayed in Table 1.
Table 1.
Baseline clinical and biochemical characteristics of the sample stratified by tertiles of PP
During the follow-up of 10 years, 32 (9.1%) participants developed incident AF. The cumulative incidence of AF increased incrementally across PP tertiles (Table 1). In univariate analyses, each SD increment in PP (odds ratio [OR] 2.10 [95% CI 1.4–3.0]), systolic blood pressure (1.79 [1.2–2.6]) or mean blood pressure (1.43 [1.0–2.2]) was significantly associated with an increase in the risk of developing AF. After adjustment for age, sex, diabetes duration, electrocardiographic LVH, and hypertension treatment, only PP maintained a significant association with incident AF (adjusted OR 1.71 [1.1–2.7], P < 0.01). In contrast, the associations of systolic blood pressure (1.46 [0.9–1.9]) and mean blood pressure (1.21 [0.7–1.5]) with incident AF were no longer significant after adjusting for the above-mentioned covariates. Results remained unchanged even after exclusion of those who improved their PP values during the follow-up (∼40% of patients changed baseline PP tertiles during follow-up). In a less parsimonious regression model, the significant association between PP and incident AF persisted after additional adjustment for BMI, chronic kidney disease, and history of previous coronary heart disease, CHF, and mild valvular disease (1.76 [1.1–2.8], P < 0.01). However, given the number of clinical outcomes (n= 32), the results of this regression model should be interpreted with some caution. Notably, other independent predictors of incident AF were older age, LVH, and history of CHF (P < 0.001).
CONCLUSIONS
This is the first study to specifically examine the role of PP in predicting development of incident AF in type 2 diabetic individuals, who were free from AF at baseline. The major finding of this study was that increased PP predicted incident AF during 10 years of follow-up, independently of LVH and other clinical AF risk factors. In contrast, systolic blood pressure and mean blood pressure were not independently associated with incident AF.
Our results complement and expand recent findings from the Framingham Heart Study demonstrating that baseline PP is an independent risk factor for new-onset AF in the community (4). It is remarkable to note that both in the Framingham Heart Study and in our study, the analysis of the components of blood pressure indicates that the relationship between blood pressure and incident AF is potentially related specifically to the age-related pulsatile component of blood pressure as assessed by PP. The increase in PP adds significantly to the pulsatile load of blood pressure on the heart (6), thereby promoting LVH (7), impaired LV diastolic relaxation (8–10), and left atrial enlargement (11). Strong evidence supports the concept of increased arterial stiffness in people with type 2 diabetes (12–14).
Our study has some important limitations. First, because our sample comprised white type 2 diabetic individuals, who were followed at an outpatient diabetes clinic, our results may not necessarily be generalizable to other nonwhite diabetic populations. Second, we measured PP, which is a simple and readily accessible if somewhat indirect measure of arterial stiffness. Third, the diagnosis of LVH was based on widely accepted ECG criteria (that have a specificity of 98–100% but a sensitivity of 30–40% compared with echocardiographic findings); echocardiography for detecting LVH at baseline was available only for few patients. Finally, there were also a relatively small number of clinical events during the follow-up; therefore, the results should be interpreted with some caution
In conclusion, our results suggest that elevated PP is associated with an increased incidence of AF in type 2 diabetic patients, independently of several AF clinical risk factors. Further studies are needed to confirm this finding and to explore whether pharmacological interventions aimed at reducing PP or preventing the increase in PP with advancing age effectively reduce the incidence of AF in type 2 diabetic patients.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
F.V. researched data, contributed to discussion, and wrote the manuscript. S.B. and G.A. contributed to discussion and reviewed and edited the manuscript. L.B. and L.Z. researched data and reviewed and edited the manuscript. G.T. researched data, analyzed data, and wrote the manuscript. G.T. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Lip GY, Tse HF, Lane DA. Atrial fibrillation. Lancet 2012;379:648–661 [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 1998;98:946–952 [DOI] [PubMed] [Google Scholar]
- 3.Jabre P, Roger VL, Murad MH, et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation 2011;123:1587–1593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell GF, Vasan RS, Keyes MJ, et al. Pulse pressure and risk of new-onset atrial fibrillation. JAMA 2007;297:709–715 [DOI] [PubMed] [Google Scholar]
- 5.Vanezis AP, Bhopal R. Validity of electrocardiographic classification of left ventricular hypertrophy across adult ethnic groups with echocardiography as a standard. J Electrocardiol 2008;41:404–412 [DOI] [PubMed] [Google Scholar]
- 6.Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension 2004;43:1239–1245 [DOI] [PubMed] [Google Scholar]
- 7.Watabe D, Hashimoto J, Hatanaka R, et al. Electrocardiographic left ventricular hypertrophy and arterial stiffness: the Ohasama study. Am J Hypertens 2006;19:1199–1205 [DOI] [PubMed] [Google Scholar]
- 8.Abhayaratna WP, Barnes ME, O’Rourke MF, et al. Relation of arterial stiffness to left ventricular diastolic function and cardiovascular risk prediction in patients > or =65 years of age. Am J Cardiol 2006;98:1387–1392 [DOI] [PubMed] [Google Scholar]
- 9.Galderisi M. Diagnosis and management of left ventricular diastolic dysfunction in the hypertensive patient. Am J Hypertens 2011;24:507–517 [DOI] [PubMed] [Google Scholar]
- 10.Leite-Moreira AF, Correia-Pinto J, Gillebert TC. Afterload induced changes in myocardial relaxation: a mechanism for diastolic dysfunction. Cardiovasc Res 1999;43:344–353 [DOI] [PubMed] [Google Scholar]
- 11.Vaziri SM, Larson MG, Lauer MS, Benjamin EJ, Levy D. Influence of blood pressure on left atrial size. The Framingham Heart Study. Hypertension 1995;25:1155–1160 [DOI] [PubMed] [Google Scholar]
- 12.Cameron JD, Bulpitt CJ, Pinto ES, Rajkumar C. The aging of elastic and muscular arteries: a comparison of diabetic and nondiabetic subjects. Diabetes Care 2003;26:2133–2138 [DOI] [PubMed] [Google Scholar]
- 13.Stehouwer CDA, Henry RMA, Ferreira I. Arterial stiffness in diabetes and the metabolic syndrome: a pathway to cardiovascular disease. Diabetologia 2008;51:527–539 [DOI] [PubMed] [Google Scholar]
- 14.Christen AI, Armentano RL, Miranda A, et al. Arterial wall structure and dynamics in type 2 diabetes mellitus methodological aspects and pathophysiological findings. Curr Diabetes Rev 2010;6:367–377 [DOI] [PubMed] [Google Scholar]