Abstract
OBJECTIVE
Because of the increasing incidence and prevalence of diabetes as a leading cause of end-stage renal disease (ESRD) in the aging population, we estimated the expected life-years (LYs) saved from successful prevention of ESRD in elderly patients with diabetes.
RESEARCH DESIGN AND METHODS
We conducted a population-based cohort study using the National Health Insurance Research Database. We identified all incidences of ESRD in the individuals >65 years of age who were receiving maintenance hemodialysis (N = 24,243) from the registry files of catastrophic illnesses in Taiwan from 1 July 1997 to 31 December 2005. We then retrospectively searched the database to determine whether there had been a diagnosis of diabetes in these cases. After the exclusion of individuals with malignancy (n = 3,423), we extrapolated the survival rates through the end of 2006 using the Monte Carlo method. Using the data of preventable ESRD cases due to diabetes and expected years of life lost (EYLL) in each age stratum, we further estimated the expected LYs saved from successful prevention of ESRD in elderly patients with diabetes.
RESULTS
The estimated average EYLL was 10.6–5.8 and 12.3–7.3 years for diabetic males and females, respectively, aged 65–79 years. In total, 5,430.1 LYs and 10,177 LYs could be saved by the successful prevention of ESRD in male and female elderly patients with diabetes, respectively, in a single year.
CONCLUSIONS
The LYs saved by successful prevention of ESRD in elderly patients with diabetes in a single year are substantial and deserve special attention, especially in elderly females.
The incidence and prevalence of diabetes keeps rising worldwide (1). The combined effects of an aging population, increased obesity and inactivity, and improved survival among diabetic individuals all contribute to this emerging pandemic. Diabetes is a disease highly prevalent in older individuals (2,3), and approximately one-third of adults >65 years have diabetes (4), which presents a great burden to individuals, society, and healthcare services.
Chronic kidney disease (CKD) is one of the most common long-term complications related to diabetes, and diabetic nephropathy is the leading cause of end-stage renal disease (ESRD) in many countries (5). In developed countries, approximately half of the new ESRD cases are related to diabetes, and the prevalence of diabetes generally increases as the population ages (5,6). The U.S., Japan, Mexico, and Taiwan have the highest incidence and prevalence of ESRD in the world (5). In Taiwan, ∼6.33% of all healthcare expenditures covered by the National Health Insurance were allocated to individuals with ESRD for dialysis in 2009, although these individuals accounted for only 0.24% of the total population (5). ESRD not only produces a financial burden but also impairs quality of life for the elderly and their families (7,8).
The standardized mortality ratios of elderly patients with ESRD are significantly higher in patients with diabetes than in nondiabetic subjects (9). Although life expectancy (LE) has been reported for elderly patients undergoing maintenance dialysis (9–12), research on the effects of diabetes among different age groups within the elderly population seems lacking (9,10). Moreover, the expected years of life lost (EYLL) for elderly patients with ESRD undergoing maintenance dialysis has not yet been investigated. We hypothesize that optimal control of blood glucose and blood pressure in elderly patients with diabetes is a worthwhile prevention strategy to reduce the incidence of ESRD, even in the oldest populations. Using the National Health Insurance Research Database (NHIRD), we conducted a population-based cohort study to determine the impact of diabetes, sex, and age on LE in elderly patients undergoing maintenance hemodialysis. We also examined the EYLL and estimated life-years (LYs) gained by the successful prevention of ESRD in elderly patients with diabetes from different age strata to evaluate the potential gain of health benefits from the effective prevention of ESRD.
RESEARCH DESIGN AND METHODS
Study population and data collection
The current study was conducted following the approval of the Institutional Review Board of the National Cheng Kung University Hospital. Taiwan launched a single-payer National Health Insurance Program on 1 March 1995. In 2011, >99% of the people in Taiwan were enrolled in this program (13). The database of this program contains registration files and original claim data for reimbursement. The National Health Research Institutes transformed these datasets into a research database, entitled NHIRD. Because the identification number of each insured individual was transformed and encrypted, privacy was fully protected. These files provided detailed information on each individual’s health care services, including all payments for outpatient visits, hospitalizations, and prescriptions.
We identified all incidences of ESRD in the individuals undergoing maintenance dialysis from the registry files of catastrophic illnesses in the NHIRD. Because each individual registered in the database of catastrophic illnesses is exempt from any copayment for dialysis therapy, the registry is comprehensive. Furthermore, the validity of the registry is assured by the careful monitoring of the National Health Insurance to prevent any abuse. A nephrologist typically makes the diagnosis of ESRD. The registry ESRD criteria are as follows: a diagnosis of CKD with an irreversible creatinine level of >8 mg/dL or a level of >6 mg/dL with diabetes as a comorbid condition. We allowed 6 months of duration (between 1 January and 30 June 1997) to exclude all prevalent cases. We also excluded cases undergoing maintenance peritoneal dialysis because of the small number of these cases (n = 769). We defined dialysis of >90 days as maintenance (long-term) dialysis. From 1 July 1997 to 31 December 2005, there were 52,756 incident cases of ESRD under maintenance hemodialysis for >90 days. Among them, 24,243 cases were >65 years. To estimate the incidence rates of ESRD in elderly patients with and without diabetes, we retrospectively searched the database to determine if such a diagnosis had been reported in the discharge summary or outpatient claim for diabetes (ICD-9-CM code 250) before the diagnosis of ESRD. The diagnosis of diabetes was confirmed if it had been included as one of the diagnoses at discharge or if there had been more than three outpatient claims for diabetes. The proportions of patients with diabetes stratified by age and sex were estimated based on interpolation of data from the following three national surveys conducted in Taiwan: the 1999–2000 Elderly Nutrition and Health Survey (14) and the Taiwanese Surveys on Blood Sugar, Blood Lipids and Blood Pressure conducted during 2002 and 2007 (15–17). The 5-year age-specific incidence rates of ESRD in elderly patients with diabetes and nondiabetic subjects undergoing maintenance hemodialysis were then calculated with the national population of Taiwan as the denominator. Cumulative incidence rates between 65 and 84 years of age (CIR65–84) were also calculated to estimate the occurrence of ESRD in elderly patients with diabetes and nondiabetic subjects undergoing maintenance hemodialysis using the following formula:
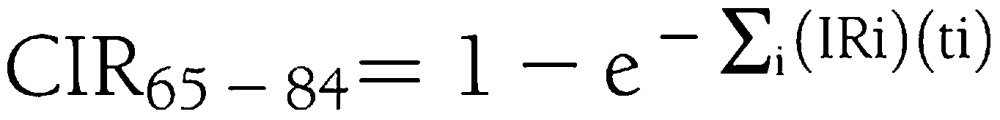 |
(18,19). To prevent confounding, we further excluded 3,423 cases with malignancy. Therefore, a total of 20,820 cases were included in the final analysis. Subsequently, the LE and EYLL in the elderly were estimated after stratification by age, sex, and the presence of diabetes, and LYs gained by successful prevention of ESRD in elderly patients with diabetes were calculated.
Survival in the ESRD population under maintenance hemodialysis
All incident cases were followed through the end of 2006 or death. The NHIRD indicates whether an individual is living, and therefore, most deceased cases of ESRD can be identified. For cases with missing information on this item, we defined the date of death as 1 month after the date of the last medical visit. Because individuals undergoing dialysis typically die within 1 month if no renal replacement therapy is provided, the above assumption seems acceptable. We used the Kaplan-Meier method to estimate the survival function based on follow-up data from 1 July 1997 to 31 December 2006. All incident cases were further divided into patients with diabetes and nondiabetic subjects, and LE and EYLL were analyzed in the 5-year age stratification.
Extrapolation of long-term survival for the ESRD population under maintenance hemodialysis
Because many cohorts with chronic diseases may not have been followed for a sufficient amount of time, we used a semiparametric method for extrapolation (20) to estimate survival analysis up to 50 years. The extrapolation was mathematically proven to be valid if constant excess hazard can be assumed (21). It was composed of three processes (20). For every individual of the ESRD cohort, we first created an age- and sex-matched referent from the life tables of the general population using the Monte Carlo method. The life tables for the general population were obtained directly from the national vital statistics published by the Department of Statistics, Ministry of the Interior, Executive Yuan, Taiwan. The survival curve of the cohort of age- and sex-matched referents was obtained by applying the Kaplan-Meier method. Second, we fitted a simple linear regression line to the logit of the ratio of survival functions between the ESRD and referent cohorts to the end of follow-up. Finally, the regression line and survival curve of the cohort of referents were used to predict a long-term survival curve beyond the follow-up for the ESRD population. To facilitate the computation, we used an iSQoL (integration of Survival and Quality of Life) software program in the R statistical package. This software can be freely downloaded from http://www.stat.sinica.edu.tw/jshwang.
Estimation of EYLL
The average EYLL of an ESRD cohort was estimated as the difference in the area between the mean survival curves of the ESRD cohort and reference population. This calculation provides a measure of the burden of ESRD on an individual. It additionally demonstrates the amount of an individual’s life that is likely to be saved by a preventive program targeted at those with elevated risk for developing ESRD.
Expected LYs gained by diabetes care in the elderly due to successful prevention of ESRD
We first calculated the prevalence of patients with diabetes in 2010 by multiplying the proportion of patients with diabetes from the 2007 Taiwanese Survey on Blood Sugar, Blood Lipids and Blood Pressure with the 2010 national population of Taiwan. Then, the number of preventable new ESRD cases was estimated from the proportion of patients with diabetes in 2010 by multiplying this number with the excess incidence rate, (= incidence rate of ESRD [patients with diabetes] − incidence rate of ESRD [nondiabetic subjects]), which was then multiplied with the EYLL per case of ESRD due to diabetes. Finally, we summed up the expected LYs gained in each age stratum and obtained the total LYs that could be saved by successful prevention of ESRD in elderly patients with diabetes between 65 and 84 years of age in a single year.
RESULTS
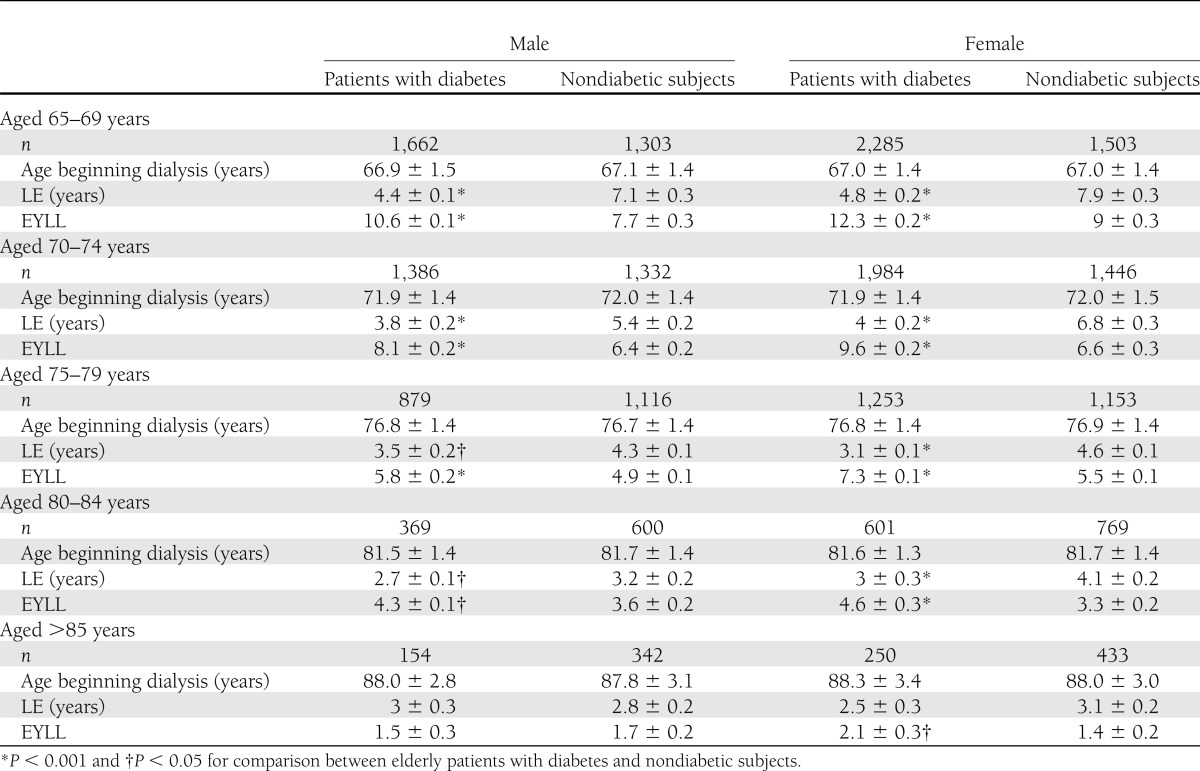
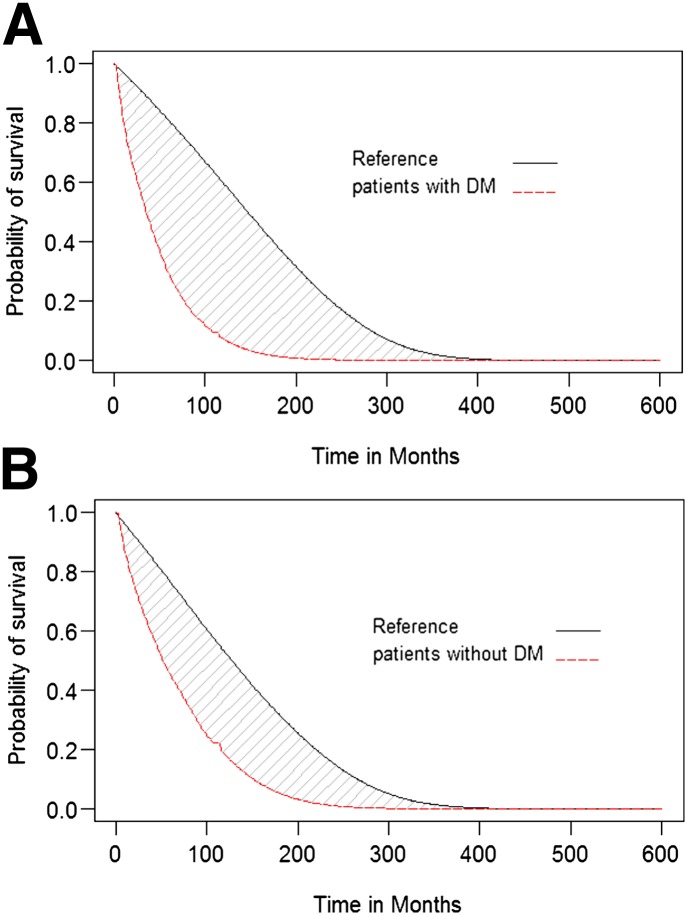
The LE and EYLL of elderly patients undergoing maintenance hemodialysis are summarized in Table 1. The estimated average EYLL of an ESRD cohort is the difference between the areas of estimated survival curves for the reference population and the ESRD cohort, as shown in Fig. 1A and B, respectively. Elderly patients with ESRD exhibited the longest LE for those aged 65–69 years among both patients with diabetes (4.4 ± 0.1 years in males and 4.8 ± 0.2 years in females) and nondiabetic subjects (7.1 ± 0.3 years in males and 7.9 ± 0.3 years in females). Elderly patients with diabetes generally showed a significantly shorter LE than elderly nondiabetic subjects in both sexes. For example, in males aged 65–69 years, the average ESRD diagnosis age was 66.9 ± 1.5 years among patients with diabetes compared with 67.1 ± 1.4 years among nondiabetic subjects. Furthermore, the LEs were 4.4 ± 0.1 and 7.1 ± 0.3 years (P < 0.001) for patients with diabetes and nondiabetic subjects, respectively.
Table 1.
Comparison of LE and EYLL between elderly patients with diabetes and nondiabetic subjects undergoing maintenance hemodialysis
Figure 1.
Mean survival difference between elderly patients with ESRD under maintenance hemodialysis and age- and sex-matched reference population after 50 years of extrapolation. A: Elderly patients with diabetes. B: Elderly nondiabetic subjects. (A high-quality color representation of this figure is available in the online issue.)
The estimated average EYLL was greater in elderly patients with diabetes than in elderly nondiabetic subjects after stratification by sex. For example, Table 1 showed that the estimated average EYLL for males aged 65–69 years was 10.6 ± 0.1 and 7.7 ± 0.3 years (P < 0.001) for patients with diabetes and nondiabetic subjects, respectively. For females aged 65–69 years, the estimated average EYLL was 12.3 ± 0.2 and 9 ± 0.3 years (P < 0.001) for patients with diabetes and nondiabetic subjects, respectively.
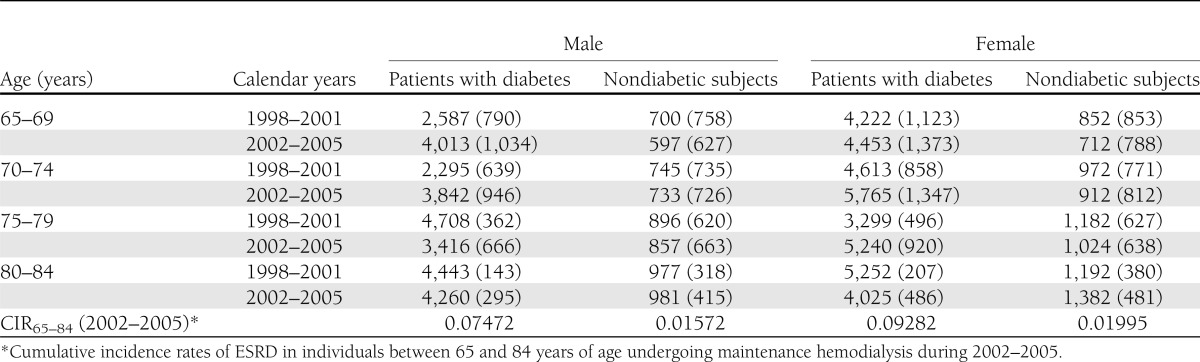
We further analyzed the incidence of ESRD (1/106 person-year) in elderly patients with diabetes and nondiabetic subjects, as summarized in Table 2. Table 2 shows that the incidence rates of ESRD undergoing maintenance hemodialysis were approximately three to five times higher in elderly patients with diabetes than in elderly nondiabetic subjects. CIR65–84 in elderly patients undergoing maintenance hemodialysis during 2002–2005 was 0.07472 and 0.09282 for diabetic males and females, respectively, but CIR65–84 was 0.01572 for and 0.01995 for nondiabetic males and females, respectively. In other words, 1 in 14 diabetic males and 1 in 11 diabetic females aged 65 years would develop ESRD and be treated with hemodialysis in the next 20 years if he/she did not die of other illnesses.
Table 2.
Incidence rates of ESRD (1/106 person-year) and incident case numbers (in parentheses) in elderly patients with diabetes and nondiabetic subjects undergoing maintenance hemodialysis
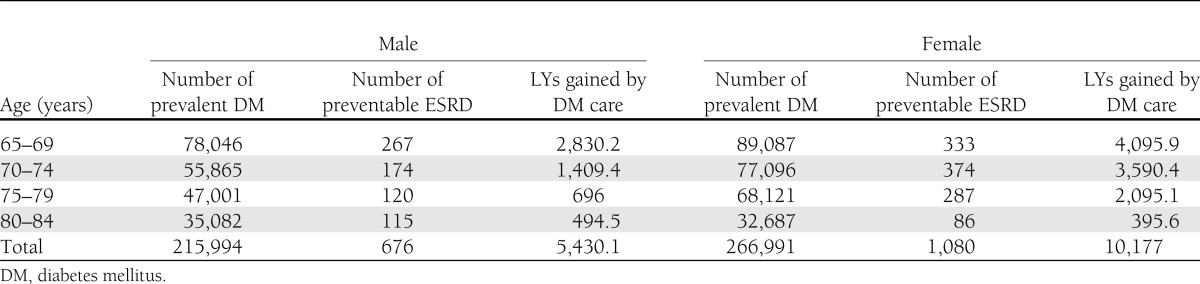
Table 3 displays the number of preventable ESRD cases due to diabetes and LYs gained by the successful prevention of ESRD in elderly patients with diabetes. The estimated prevalence of patients with diabetes in the year 2010 was 215,994 males and 266,991 females between 65 and 84 years of age. There were 676 and 1,080 preventable ESRD cases in males and females, respectively, due to diabetes in a year; thus, there would be 5,430.1 LYs and 10,177 LYs saved by the successful prevention of ESRD in elderly diabetic males and females, respectively, in a year.
Table 3.
The number of preventable incident ESRD cases due to diabetes and LYs gained by successful prevention of ESRD in elderly patients with diabetes between 65 and 84 years of age in a single year
CONCLUSIONS
Although previous studies have investigated the impact of diabetes on elderly patients undergoing dialysis (9), the current study is the first to estimate the LE and EYLL (22) in elderly patients with ESRD stratified by age, sex, and the presence of diabetes. We found that the average EYLL for the young-old (between 65 and 75 years of age) patients with diabetes is quite substantial (Table 1). Therefore, attention should be paid to preventive care of ESRD in the patients with diabetes. For example, in elderly patients with diabetes who are 70–74 years old, the average EYLL was 8.1 ± 0.2 and 9.6 ± 0.2 for males and females, respectively, indicating that for this age-group, successfully preventing development of ESRD in elderly patients with diabetes would save 8.1 and 9.6 LYs for society. Thus, the total number of LYs gained by successful prevention of ESRD in elderly patients with diabetes within a single year would be 5,430.1 and 10,177 LYs for males and females, respectively (Table 3). Because we did not count the potential LYs saved by sound diabetes care in elderly patients with ESRD undergoing maintenance dialysis, the above conclusion may be an underestimation. Moreover, the above calculation did not include the loss of utility from reduced quality of life or the additional financial burden related to the development of ESRD. These facts further stress the value of diabetes care in the elderly and prevention of diabetes-related complications, including ESRD.
According to a previous report (23), the cumulative lifetime risks for ESRD were 0.073–0.078 and 0.018–0.025 for 20-year-old black and white Americans, respectively. In the current study, we also calculated the CIR65–84 in elderly developing ESRD that requires maintenance hemodialysis. The results showed that the likelihood of developing ESRD for elderly patients with diabetes aged 65 years would be ∼1 in 14 for males and 1 in 11 for females in the next 20 years, which would be nearly five times the risk for elderly nondiabetic subjects. Thus, careful screening and follow-up of renal function accompanied with optimal control of blood glucose, serum lipids, and blood pressure must be considered when treating this population (24–29). Prevention of diabetes-related ESRD could possibly be accomplished through comprehensive diabetes care, and efforts to improve public awareness regarding prevention of CKD should also be strengthened (30,31).
Diabetes was reported to be associated with a higher risk of death in individuals with ESRD (9), which was corroborated in this study. We have further quantified magnitudes of differences in EYLL for different age strata (Table 1). However, differences between elderly patients with diabetes and nondiabetic subjects narrowed as the age advanced, and the effects of diabetes seemed to be greater in the young-old individuals. Our finding is consistent with a previous report (2), which showed that the young-old individuals have a higher risk of mortality, and the oldest old individuals (>85 years of age) have a lower rate of complications. Although Table 1 shows that the LE was better in females than in males, as was reported previously (6,32), the EYLL was greater in females than in males, which may result from a general longer life expectancy in females (33). Thus, both male and female elderly patients with diabetes should be paid attention for prevention of ESRD (24,34).
According to the Neal “thrifty gene” hypothesis (35), the diabetogenic genes persisted at a high level in times of nutritional deprivation because they contributed to a survival advantage, which might be good for survival of human species. However, as the food shortage is no longer a major threat nowadays, the sedentary lifestyles of modern times aggravate the occurrence of diabetes (36). Both factors contribute to the development of hyperlipidemia, metabolic syndrome, and diabetes, which further result in an increased premature mortality of cardio- and cerebrovascular diseases, especially among the ESRD cohort (9). Because Taiwan has the highest incidence and prevalence of treated ESRD (5), it is crucial that we identify preventable factors as early as possible in life and control them. As mentioned in the position statement (24), all practitioners must emphasize lifestyle modifications on dietary intake and exercise to optimize glucose, lipids, and blood pressure control plus regular screening of urine albumin excretion and serum creatinine for early detection and control of CKD. With the standard of medical care and the CKD prevention program in elderly patients with diabetes with CKD (24–29), we hoped that diabetes-related ESRD could be decreased gradually in the future. Moreover, such a control program would generally produce spillover effects on reducing cardio- and cerebrovascular morbidities and mortalities, especially among the elderly (37,38). Future studies are needed to quantify the magnitudes of effects on different causes of death.
Although we analyzed the most comprehensive national data currently available in Taiwan, there are potential limitations that must be addressed. First, our estimation of LE and EYLL was dependent upon the assumption of constant excess hazard and premature mortality of ESRD. We checked the assumption by fitting the logit transform of the survival ratio between cohorts with ESRD and the age- and sex-matched general population, which showed a straight line and fulfilled the assumption. Second, the lifetime extrapolation was based on current and prior experiences of survival, including the life tables of the current population. As the dialysis technology and control for comorbidities may improve in the coming years, our results might underestimate the LE and overestimate the EYLL of elderly patients with diabetes and nondiabetic subjects with ESRD. However, because the improved survival of ESRD cohorts generally accompanies an increased cost for treatment, the overall saving from prevention is still a worthwhile investment. Third, this study did not include elderly patients undergoing maintenance peritoneal dialysis and cannot make a general inference for this population. Although the Bureau of National Health Insurance has promoted peritoneal dialysis during the last 5 years, hemodialysis seems to be the predominant modality of dialysis therapy in the elderly in Taiwan because of a lower requirement for education and learning. Because no significant differences on survival for peritoneal dialysis and hemodialysis were found in the previous study (22), the current estimates of LE and EYLL might be a close approximation for peritoneal dialysis among elderly patients with diabetes and nondiabetic subjects. Fourth, we did not begin following these subjects when they had been first diagnosed with diabetes. Thus, we may underestimate the latency period and overestimate the incidence rate of ESRD for elderly patients with diabetes. However, the current study stratified the population at risk into 5-year age groups, which reduces the above effect to some extent. Finally, because the NHIRD does not contain any information related to quality of life, we were not able to calculate the quality-adjusted life expectancy. Future studies need to address these issues.
In conclusion, we found that successful prevention of ESRD in the elderly is worthwhile, especially among elderly patients with diabetes, and may save up to a decade of LYs for each diabetic individual. As the incidence of diabetes has increased continually, the LYs saved by comprehensive diabetes care in our society would be substantial, and diabetes care deserves special attention, especially in elderly females. Future studies should take into account quality of life and cost of active prevention and dialysis to evaluate cost-effectiveness of prevention programs for elderly patients with diabetes.
Acknowledgments
Funding for this study was provided by grants from the National Health Research Institutes of Taiwan (Intramural Project EO-100-EO-PP04), the National Science Council (NSC 99-2628-B-006-036-MY3), and the National Cheng Kung University Hospital (Intramural Grant NCKUH-10001020).
No potential conflicts of interest relevant to this article were reported.
D.-C.Y., C.-M.C., and J.-D.W. contributed to the study design and interpretation of data and developed the first draft of the manuscript. L.J.-H.L., C.-C.H., M.-C.W., and W.-H.L. contributed to the review and editing of the manuscript. Y.-Y.C. contributed to the collection and analysis of data. All authors approved the final draft of the manuscript for submission. C.-M.C. and J.-D.W. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the National Health Research Institutes for providing the data for analysis.
Footnotes
The interpretation and conclusions of this article do not represent those of the National Health Research Institutes.
References
- 1.van Dieren S, Beulens JW, van der Schouw YT, Grobbee DE, Neal B. The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil 2010;17(Suppl. 1):S3–S8 [DOI] [PubMed] [Google Scholar]
- 2.Ferrer A, Padrós G, Formiga F, Rojas-Farreras S, Perez JM, Pujol R. Diabetes mellitus: prevalence and effect of morbidities in the oldest old. The Octabaix study. J Am Geriatr Soc 2012;60:462–467 [DOI] [PubMed] [Google Scholar]
- 3.Morley JE. Diabetes and aging: epidemiologic overview. Clin Geriatr Med 2008;24:395–405 [DOI] [PubMed] [Google Scholar]
- 4.Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHANES), 1999-2006. Diabetes Care 2010;33:1055–1060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United States Renal Data System 2011 Annual Data Report. Atlas of end-stage renal disease in the United States: international comparisons. Am J Kidney Dis 2012;59(Suppl. 1):e291–e302 [DOI] [PubMed] [Google Scholar]
- 6.Yang WC, Hwang SJ, Taiwan Society of Nephrology Incidence, prevalence and mortality trends of dialysis end-stage renal disease in Taiwan from 1990 to 2001: the impact of national health insurance. Nephrol Dial Transplant 2008;23:3977–3982 [DOI] [PubMed] [Google Scholar]
- 7.De Biase V, Tobaldini O, Boaretti C, et al. Prolonged conservative treatment for frail elderly patients with end-stage renal disease: the Verona experience. Nephrol Dial Transplant 2008;23:1313–1317 [DOI] [PubMed] [Google Scholar]
- 8.Yang SC, Kuo PW, Wang JD, Lin MI, Su S. Quality of life and its determinants of hemodialysis patients in Taiwan measured with WHOQOL-BREF(TW). Am J Kidney Dis 2005;46:635–641 [DOI] [PubMed] [Google Scholar]
- 9.Villar E, Remontet L, Labeeuw M, Ecochard R. Effect of age, gender, and diabetes on excess death in end-stage renal failure. J Am Soc Nephrol 2007;18:2125–2134 [DOI] [PubMed] [Google Scholar]
- 10.Chandna SM, Da Silva-Gane M, Marshall C, Warwicker P, Greenwood RN, Farrington K. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant 2011;26:1608–1614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 2007;146:177–183 [DOI] [PubMed] [Google Scholar]
- 12.Joly D, Anglicheau D, Alberti C, et al. Octogenarians reaching end-stage renal disease: cohort study of decision-making and clinical outcomes. J Am Soc Nephrol 2003;14:1012–1021 [DOI] [PubMed] [Google Scholar]
- 13.Governmental Information Office. Taiwan. Available from http://info.gio.gov.tw/ct.asp?xItem=19930&ctNode=2847 Accessed 1 March 2012
- 14.Pan WH, Hung YT, Shaw NS, et al. Elderly Nutrition and Health Survey in Taiwan (1999-2000): research design, methodology and content. Asia Pac J Clin Nutr 2005;14:203–210 [PubMed] [Google Scholar]
- 15.Shih YT, Hung YT, Chang HY, et al. The design, contents, operation and the characteristics of the respondents of the 2001 National Health Interview Survey in Taiwan. Taiwan J Public Health 2003;22:419–430 [Google Scholar]
- 16.Bureau of Health Promotion, Department of Health, Executive Yuan, Taiwan. Taiwanese Survey on Blood Sugar, Blood Lipids and Blood Pressure in 2002. Available from http://www.bhp.doh.gov.tw/health91/study-2.htm Accessed November 2003
- 17.Bureau of Health Promotion, Department of Health, Executive Yuan, Taiwan. Taiwanese Survey on Blood Sugar, Blood Lipids and Blood Pressure in 2007. Available from http://www.bhp.doh.gov.tw/BHPNET/Portal/Them_Show.aspx?Subject=200712250011&Class=2&No=201102140001 Accessed 29 July 2011
- 18.Davis W. Cancer Registration and its Techniques. Lyon, France, International Agency for Research on Cancer, 1978, p.162–163 [Google Scholar]
- 19.Wang JD. Basic Principles and Practical Applications in Epidemiological Research. Singapore, World Scientific, 2002, p. 135–137 [Google Scholar]
- 20.Hwang JS, Wang JD. Monte Carlo estimation of extrapolation of quality-adjusted survival for follow-up studies. Stat Med 1999;18:1627–1640 [DOI] [PubMed] [Google Scholar]
- 21.Fang CT, Chang YY, Hsu HM, et al. Life expectancy of patients with newly-diagnosed HIV infection in the era of highly active antiretroviral therapy. QJM 2007;100:97–105 [DOI] [PubMed] [Google Scholar]
- 22.Kao TW, Huang JW, Hung KY, et al. Life expectancy, expected years of life lost and survival of hemodialysis and peritoneal dialysis patients. J Nephrol 2010;23:677–682 [PubMed] [Google Scholar]
- 23.Kiberd BA, Clase CM. Cumulative risk for developing end-stage renal disease in the US population. J Am Soc Nephrol 2002;13:1635–1644 [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association Standards of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl. 1):S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sibal L, Home PD. Management of type 2 diabetes: NICE guidelines. Clin Med 2009;9:353–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Kidney Foundation K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(Suppl. 1):S1–S266 [PubMed] [Google Scholar]
- 27.Hwang SJ, Tsai JC, Chen HC. Epidemiology, impact and preventive care of chronic kidney disease in Taiwan. Nephrology (Carlton) 2010;15(Suppl. 2):3–9 [DOI] [PubMed] [Google Scholar]
- 28.Wu IW, Wang SY, Hsu KH, et al. Multidisciplinary predialysis education decreases the incidence of dialysis and reduces mortality—a controlled cohort study based on the NKF/DOQI guidelines. Nephrol Dial Transplant 2009;24:3426–3433 [DOI] [PubMed] [Google Scholar]
- 29.Lai MN, Lai JN, Chen PC, Hsieh SC, Hu FC, Wang JD. Risks of kidney failure associated with consumption of herbal products containing Mu Tong or Fangchi: a population-based case-control study. Am J Kidney Dis 2010;55:507–518 [DOI] [PubMed] [Google Scholar]
- 30.Hsu CC, Hwang SJ, Wen CP, et al. High prevalence and low awareness of CKD in Taiwan: a study on the relationship between serum creatinine and awareness from a nationally representative survey. Am J Kidney Dis 2006;48:727–738 [DOI] [PubMed] [Google Scholar]
- 31.Wen CP, Cheng TY, Tsai MK, et al. All-cause mortality attributable to chronic kidney disease: a prospective cohort study based on 462 293 adults in Taiwan. Lancet 2008;371:2173–2182 [DOI] [PubMed] [Google Scholar]
- 32.Shinzato T, Nakai S, Akiba T, et al. Survival in long-term haemodialysis patients: results from the annual survey of the Japanese Society for Dialysis Therapy. Nephrol Dial Transplant 1997;12:884–888 [DOI] [PubMed] [Google Scholar]
- 33.Trovato F, Heyen NB. A varied pattern of change of the sex differential in survival in the G7 countries. J Biosoc Sci 2006;38:391–401 [DOI] [PubMed] [Google Scholar]
- 34.Brown AF, Mangione CM, Saliba D, Sarkisian CA, California Healthcare Foundation/American Geriatrics Society Panel on Improving Care for Elders with Diabetes Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc 2003;51(Suppl. Guidelines):S265–S280 [DOI] [PubMed] [Google Scholar]
- 35.Neel JV. Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet 1962;14:353–362 [PMC free article] [PubMed] [Google Scholar]
- 36.Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature 2001;414:782–787 [DOI] [PubMed] [Google Scholar]
- 37.Gu K, Cowie CC, Harris MI. Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971-1993. Diabetes Care 1998;21:1138–1145 [DOI] [PubMed] [Google Scholar]
- 38.Bertoni AG, Krop JS, Anderson GF, Brancati FL. Diabetes-related morbidity and mortality in a national sample of U.S. elders. Diabetes Care 2002;25:471–475 [DOI] [PubMed] [Google Scholar]