Abstract
OBJECTIVE
The discrepancy of diabetes incidence and care between socioeconomic statuses has seldom been studied concurrently in nations with universal health coverage. We aimed to delineate whether income disparity is associated with diabetes incidence and inequality of care under a national health insurance (NHI) program in Asia.
RESEARCH DESIGN AND METHODS
From the Taiwan NHI database in 2000, a representative cohort aged ≥20 years and free of diabetes (n = 600,662) were followed up until 2005. We regarded individuals exempt from paying the NHI premium as being poor. Adjusted hazard ratios (HRs) were used to discover any excess risk of diabetes in the poor population. The indicators used to evaluate quality of diabetes care included the proportion of diabetic patients identified through hospitalization, visits to diabetes clinics, and completion of recommended diabetes tests.
RESULTS
The incidence of type 2 diabetes in the poor population was 20.4 per 1,000 person-years (HR, 1.5; 95% CI, 1.3–1.7). Compared with their middle-income counterparts, the adjusted odds ratio (OR) for the poor population incidentally identified as having diabetes through hospitalization was 2.2 (P < 0.001). Poor persons with diabetes were less likely to visit any diabetes clinic (OR, 0.4; P < 0.001). The ORs for the poor population with diabetes to receive tests for glycated hemoglobin, low-density lipoprotein cholesterol, triglycerides, and retinopathy were 0.6 (0.4–0.9), 0.4 (0.2–0.7), 0.5 (0.4–0.8), and 0.4 (0.2–0.9), respectively.
CONCLUSIONS
Poverty is associated not only with higher diabetes incidence but also with inequality of diabetes care in a northeast Asian population, despite universal health coverage.
In Western economies, low-income populations have been found to be more likely to develop diabetes (1,2). A hazardous home environment, unhealthy behaviors, obesity, and stress are all risks contributing to a higher incidence of diabetes among poor populations (1,3,4). The discrepancy of diabetes incidence between different socioeconomic status (SES) groups has seldom been studied in developing or recently developed economies, however, especially in Asia.
In addition to their disproportionate diabetes occurrence, individuals with low SES tend to have poorer glycemic control, more diabetes complications, and higher mortality (5–7). Apart from personal vulnerability and other predisposing factors (8), lack of access to health care has been considered an important risk factor for the consequences of diabetes among the socioeconomically deprived (9). Some studies have been conducted to assess whether improved health-care access through universal or voluntary health insurance coverage can ensure quality of diabetes care across socioeconomic gradients; however, results have been inconclusive. Brown et al. (10) reported that low-income patients in managed-care health plans were less likely to receive dilated eye examinations because of the unaffordable copayment. Booth and Hux (11) found that limited access in rural areas and high out-of-pocket cost for medications and monitoring supplies might contribute to otherwise avoidable hospitalizations for low-SES patients with diabetes in the Canadian health system. Israeli studies (12,13) have reported, however, that even though low-SES people with diabetes in their government-funded health maintenance organizations may have higher rates of glycated hemoglobin (HbA1c) and LDL cholesterol testing, their outcomes remain persistently worse. Although universal health care has often been advocated as a silver bullet to eliminate health disparity (14–16), few large-scale studies have demonstrated empirical effectiveness of universal health coverage in resolving health inequalities for poor people with chronic diseases such as diabetes.
In 1995, Taiwan launched a single-payer comprehensive national health insurance (NHI) program with full coverage of ambulatory care, hospitalization, laboratory tests, and prescribed medications (17). To ensure accessibility for the entire population, the government waives premiums and copayments for entitled low-income individuals, those living below the local lowest living index. This health policy for the poor population provides an opportunity to investigate the true influence of poverty on the development of diabetes and the equality of diabetes care. The empirical evidence from Taiwan’s health system is also important for the recent global movement toward a goal of universal health coverage (15,18,19). We aimed to examine whether the risk of diabetes development in the poor is higher than that of general population in a northeast Asian country with recent economic advancement and the introduction of universal health insurance. In the same setting, we examined the impact of income status on diabetes care where there ought to be no barriers to its access.
RESEARCH DESIGN AND METHODS
Data sources and study subjects
The NHI program has been the basis of the health-care system in Taiwan since 1995. As of 2007, 98.4% of Taiwan’s population of 23 million was enrolled in the NHI program. The NHI Research Database (NHIRD) is derived from this program for research purposes. From the registration and reimbursement files in the NHIRD, the Longitudinal Health Insurance Database 2000 (LHID2000) was constructed by randomly sampling from the year 2000 Registry for Beneficiaries of the NHIRD (20). There were no significant differences in the sex or age distributions or in the average insurable income between the samples in the LHID2000 and the subjects in the original NHIRD of 2000. We have studied the LHID2000 with antecedent data from 1 January 1997. To calculate incidence of type 2 diabetes, we formed an eligible cohort of 600,662 participants who were aged 20 years or older, diabetes free for at least 3 years before 2000, and registered as NHI beneficiaries on 1 January 2000. We then divided this eligible cohort into four groups according to economic status. Because the poor group was significantly outnumbered by the other groups, we used the simple random sampling (without replacement) method to select 7,596 subjects (three times the number in the poor group) from each of the three wealthier groups as the study subjects to minimize the possibility of overestimating a true difference between groups because of a large differences in the sample sizes. There were no statistical differences in the distribution of sex, age, income, and baseline comorbidity between each selected group and its original study population. Diabetic subjects identified in the four groups were further investigated with regard for quality of diabetes care.
Definition of economic status
The study subjects’ economic statuses were estimated according to their insurable monthly incomes recorded in the NHI registry archives in 2000, by which the Bureau of NHI calculated the beneficiaries’ premiums. Four economic categories were thereby determined: poor (n = 2,532), low income (monthly income less than Taiwan’s minimum wage level in 2000 of 15,840 new Taiwan dollars [NTD], n = 89,868), middle income (monthly income 15,840–57,779 NTD, n = 478,086), and high income (monthly income at or above the highest rank of insurable income in 2000 [57,800 NTD], n = 30,176). The exchange rate from US currency to the NTD is about 1:30.
Individuals categorized as poor were recognized by the local municipal authorities as living below the local lowest living index and were entitled to receive social welfare subsidies and special NHI benefits, namely exemption from NHI premiums and copayments.
Diabetic subjects
Cases of type 2 diabetes in the period 2000–2005 were ascertained by one of the following criteria: 1) hospitalization for diabetes-related illness (ICD-9-CM: 250.xx) or prescribed antidiabetic drugs during the admission course, 2) at least one prescription of oral antidiabetic agents and one ambulatory visit for diabetes-related illness (ICD-9-CM: 250.xx or A181 [an abridged diabetes code used by physicians in Taiwan before 2000 for ambulatory visits]) within 1 year, or 3)at least four ambulatory visits for diabetes-related illness within 1 year. Excluded were individuals who had diabetes diagnoses (ICD-9-CM: 250.xx or A181) or who had been prescribed antidiabetic agents in 1997–1999. Those who had a diagnosis of type 1 diabetes (ICD-9-CM: 250.x1 or 250.x3) made during the follow-up or those who were younger than 30 years of age and did not have any oral antidiabetes drugs recorded but who received insulin therapy for the first entire year after diabetes diagnosis were regarded as having type 1 diabetes, so they were also excluded (n = 175) from further analysis.
Quality of diabetes care
To evaluate promptness of diabetes identification across different income strata, we calculated the proportion of new diabetic patients who were incidentally identified as having diabetes through hospitalization. Diabetic patients who don’t get prompt diagnosis until hospitalization may be less likely to receive screening for early detection or may not be sufficiently aware of diabetes-related symptoms to seek appropriate health care. The indicators used to evaluate quality of diabetes care were the percentage of diabetic patients who visited diabetes clinics and the percentage of diabetic patients with diabetes clinic visits who received annual tests for fasting glucose, HbA1c, LDL cholesterol, triglycerides, creatinine, urine dipstick, urine microalbumin, and retinopathy within 1 year of the diabetes diagnosis.
Statistical analysis
The incidence rate of type 2 diabetes in the follow-up period was estimated by the number of new type 2 diabetes cases per 1000 person-years. The person-years were calculated as the time elapsed from the date of cohort entry (1 January 2000) until the date of diabetes development, withdrawal from the NHI program, or the end of follow-up (31 December 2005), whichever came first. The calculation of a 95% CI for the incidence rate was based on the assumption that the incident cases followed a Poisson distribution. We used Cox proportional hazards models to estimate adjusted hazard ratios of diabetes development in different income groups relative to the middle-income group. The proportional hazard assumption was examined by plotting the Kaplan-Meier survival curves and by testing the interaction between income levels and follow-up time. Multivariable logistic regressions were used to evaluate the association between income disparity and quality of diabetes care. The middle-income group was treated as the reference group to represent the general population. The covariates included sex, age, comorbidity, NHI registration location (city, township, and rural area), and the year of diabetes diagnosis. Comorbidities were measured by the Charlson comorbidity index (CCI) (21), and three chronic conditions, including hyperlipidemia (ICD-9-CM: 272, A182, or A189), hypertension (ICD-9-CM: 401 or A269), and gout (ICD-9-CM: 274). We defined subjects as having comorbidity if at least three NHI diagnoses were identified in 1999. Analyses were performed with SAS software, version 9.1 (SAS Institute, Cary, NC).
This study was granted ethical approval by the Institutional Review Board of the National Health Research Institutes of Taiwan.
RESULTS
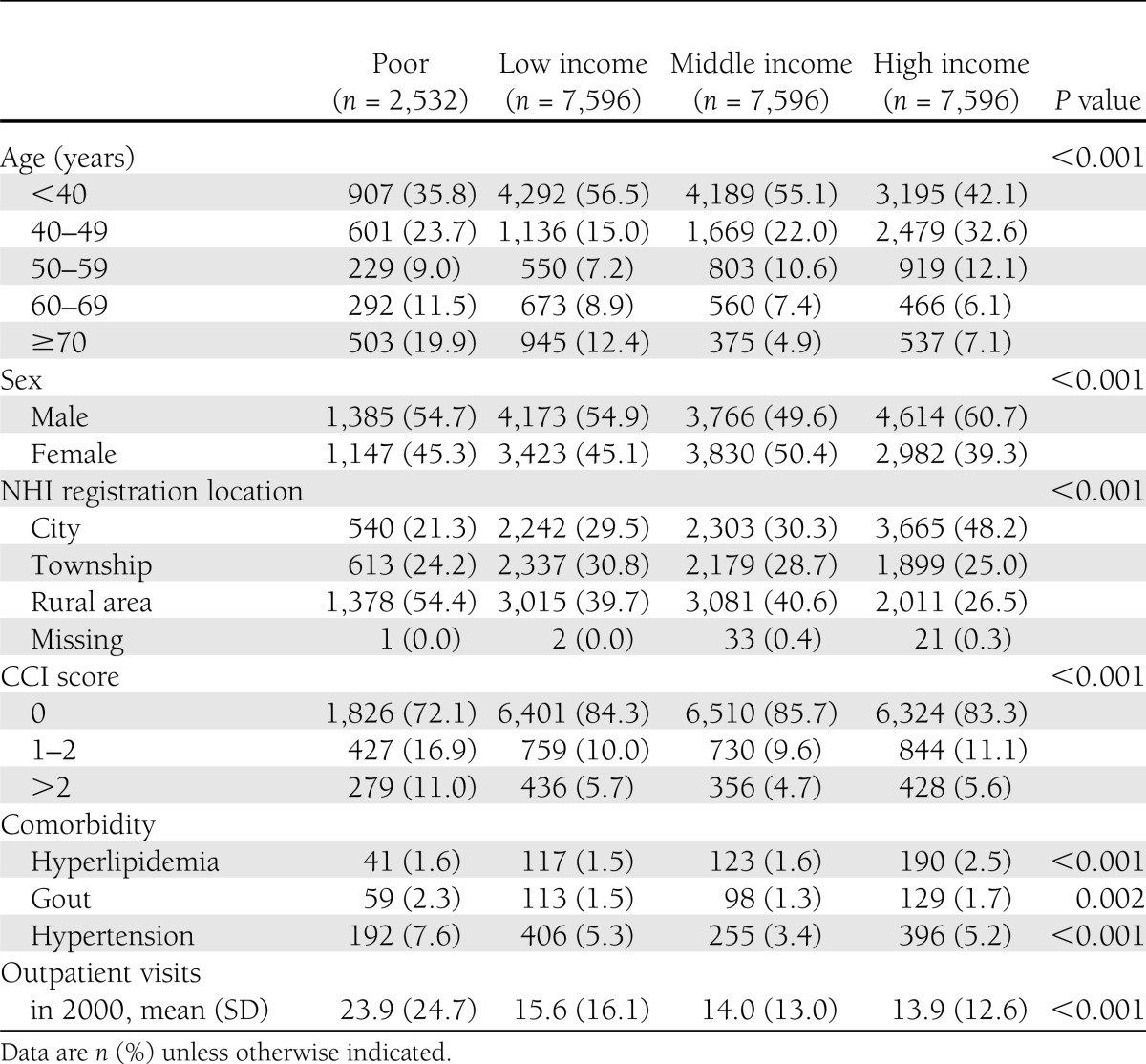
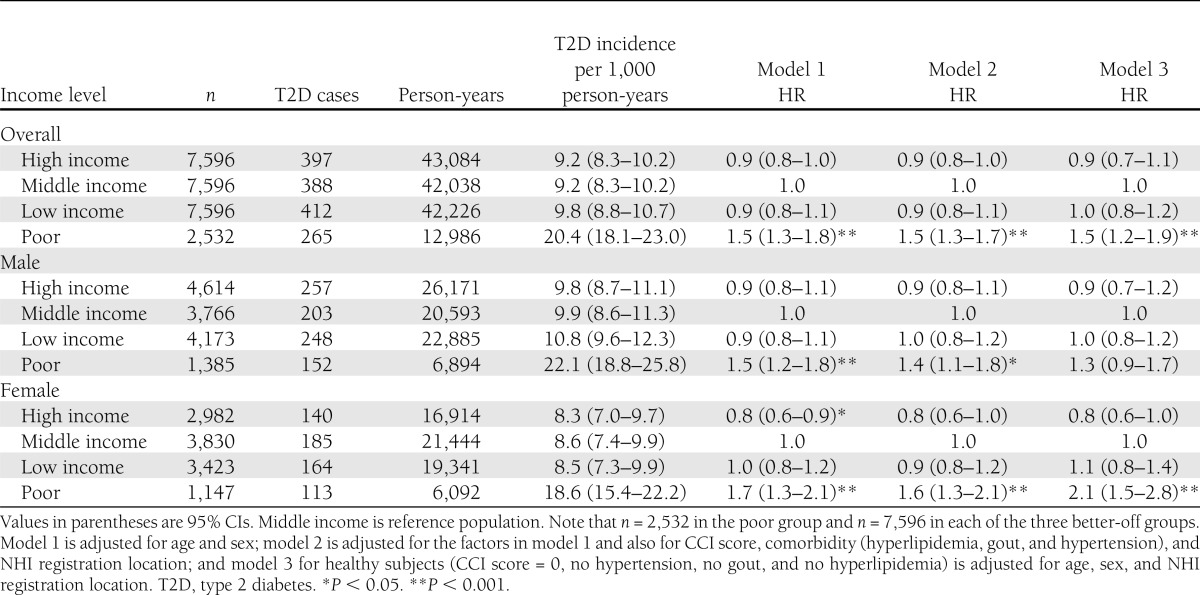
Table 1 reveals demographic differences between poor and other income groups. Poor people tended to be older, live in rural areas, and suffer from more chronic diseases. They also visited outpatient clinics more frequently. As shown in Table 2, the income disparity was significantly associated with the discrepancy in type 2 diabetes incidence in both males and females. Poor people were more likely to develop type 2 diabetes during the 6-year follow-up period. Compared with the middle-income group, in the poor group the diabetes risk was 40% higher for males and 60% higher for females. To eliminate confounding effects of higher prevalence of comorbidities in the poor group, we selected healthy subjects (CCI score of 0 and no hypertension, gout, or hyperlipidemia in 1999) for subgroup analysis (model 3 in Table 2). This analysis found that among women, the poor population remained the most vulnerable group for diabetes development (HR, 2.1; 95% CI, 1.5–2.8).
Table 1.
Demographics and outpatient visits of study subjects in different income status
Table 2.
Relative incident risk of type 2 diabetes in four groups according to income level
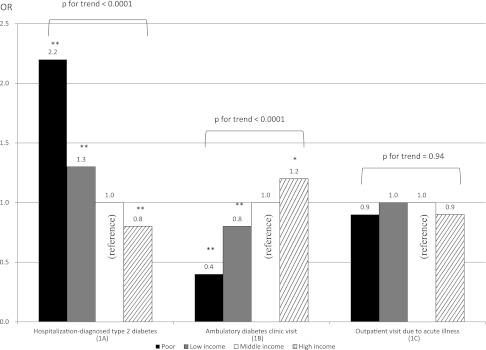
Fig. 1A reveals that the possibility of initial diabetes identification during hospitalization was inversely related to income level. About 50% of poor people (data not shown) did not receive professional diabetes care until they developed symptoms or complications that were severe enough to require hospitalization. Compared with the middle-income group, the adjusted risks of hospitalization-diagnosed diabetes for the poor, low-income, and high-income groups were 2.2, 1.3, and 0.8, respectively (P < 0.0001 for trend).
Figure 1.
Adjusted ORs of hospitalization-diagnosed type 2 diabetes (1A), ambulatory diabetes clinic visits within 1 year after diabetes diagnosis (1B), and outpatient visits for acute illnesses for diabetes patients in different income groups (1C). *P < 0.05; **P < 0.001. The logistic regression models have been adjusted for age, sex, CCI score, comorbidity (hyperlipidemia, gout, and hypertension), and NHI registration location.
With regard to diabetes care, Fig. 1B illustrates that the income gradient is significantly related to the likelihood of clinical follow-up (P < 0.0001 for trend). Poor people with diabetes were less likely to have medical follow-up for their newly diagnosed diabetes. Overall, about 45% of the poor people with diabetes had not visited any diabetes clinic within 1 year of their diagnosis (data not shown). Compared with the middle-income group, the adjusted odds ratios (ORs) for ambulatory diabetes clinic visits for the poor, low-income, and high-income groups were 0.4 (P < 0.001), 0.8 (P < 0.001), and 1.2 (P < 0.05), respectively. On the other hand, the likelihood of outpatient visits for acute illnesses did not seem to decrease for economically disadvantaged groups. The multivariable adjusted model (Fig. 1C) shows no income discrepancy for access to acute illness care (P = 0.94 for trend).
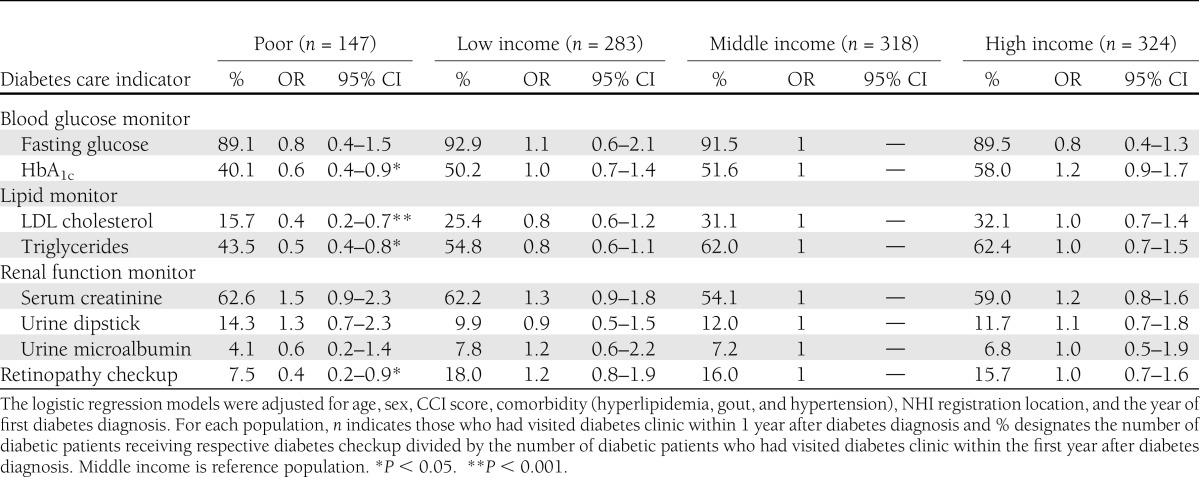
As shown in Table 3, individuals with diabetes in Taiwan generally received fewer of the recommended diabetes tests through regular diabetes clinic visits. Fasting glucose was ordered by physicians most frequently (89–93%). Compared with the middle-income group, poor people with diabetes were less likely to obtain most of the recommended annual tests in the first year after diagnosis, especially for HbA1c (OR, 0.6; P < 0.05), LDL cholesterol (OR, 0.4; P < 0.001), and triglycerides (OR, 0.5; P < 0.05), nor were they as likely to receive an ophthalmological examination for retinopathy (OR, 0.4; P < 0.05).
Table 3.
Percentage and adjusted ORs of type 2 diabetic patients receiving various diabetes checkups within 1 year after diagnoses, according to their income level
CONCLUSIONS
Poverty, as shown in this longitudinal study, is significantly associated with an increase in type 2 diabetes incidence, delayed diagnosis of diabetes, and inadequate diabetes care and management. Compared with those with a middle income, individuals who were poor had about a 50% higher risk of development of type 2 diabetes. The poor group outnumbered other income groups in their hospitalization-diagnosed diabetes, indicating probable delays in recognition and identification of a worsening prognosis. Moreover, poor people with diabetes were about 50% less likely to receive the recommended diabetes checkups. Overall, this population-based study demonstrates that economically disadvantaged people are more vulnerable to development of diabetes and more likely to experience inequality of care once diabetes has developed, despite universal health insurance coverage.
Similar to our findings, a growing body of studies has shown an association between low SES and increased diabetes incidence, especially in females. Limited resources in food choice (22), tendency toward obesity and physical inactivity (2,23), and detrimental psychosocial pressures, such as occupational stress and lack of social support (3,24), are often found to be unfavorable intermediate factors inherent in disadvantaged economic situations and serve as a link to the high incidence of diabetes. In Taiwan, the higher incidence of diabetes in the poor population could also derive from multiple risk factors, including physical vulnerability, disadvantaged environments, and risky behaviors, along with their mutual interaction (25–27).
One of our important findings is that equal access to medical care for acute illnesses in the poor group in a health system with universal insurance coverage was not mirrored by timely medical attention for diabetes diagnosis and care. Disparity of diabetes care among low-income patients is a global problem (28,29); however, the poor people in this study were entitled to waived premiums and no copayments for medical services, so their underuse of necessary diabetes care could not be solely attributed to the financial barriers identified in other studies (10,11). With regard to geographic inaccessibility to medical care facilities, this study showed no major access barrier for acute symptomatic illness in the poor population with diabetes. The high NHI participation rate of health providers (92.5% of all hospitals or clinics in Taiwan provide NHI services, including 100% of public institutions) (30) also helps to ensure accessibility for acute illness treatment. Good access to care for acute symptomatic illness, however, does not necessarily correspond with good access to care for chronic disease. Most primary care physicians in Taiwan only provide ambulatory acute care. Medical centers or regional hospitals equipped with high-tech facilities and multidisciplinary teams are thus usually the choice of patients to visit for management of chronic diseases. Unfortunately, most medical centers and regional hospitals are located in metropolitan areas, which could create a barrier of accessibility to diabetes care for those who live in rural areas. For the poor population, inaccessibility to a dedicated diabetes care is a structural obstacle to overcome, although the poor population does have good access to acute symptomatic illness management.
Furthermore, to prevent cardiovascular diseases, Taiwan’s government provides a free health examination (the measurement of blood pressure, body weight, and some basic biochemical tests, such as fasting glucose, creatinine, urine dipstick test, and lipid profiles) every 3 years for those aged 40–64 years and every year for those aged ≥65 years. This government-sponsored health checkup is usually conducted by primary care physicians; according to the current study, however, it does not seem to be effective in targeting the vulnerable disadvantaged group. The failure of early detection of diabetes in the national screening program may indicate that the function of primary care physicians should be further strengthened to reduce the possibility of delayed diagnosis, especially among the poor population. Encouraging partnerships between hospitals and primary care physicians is a practical way to minimize accessibility barriers related to geographic variation. This has been shown to be effective by mobilizing hospital-based dietitians to achieve better glycemic and diet control for diabetic patients in a Taiwanese primary care setting (31).
The discrepancy in the quality of diabetes care could result from physicians’ intentionally or subconsciously biased clinical management decisions owing to patients’ different SES (32). Low SES could also impair mutual understanding, damage effective communication, and weaken interactive partnership between doctors and patients (33). All these influences could therefore contribute inferior quality to the diabetes process measures for the poor group.
On the other hand, patients themselves may also need to be held accountable for the delayed diagnosis of diabetes, which would usually incur clinical symptoms; however, these symptoms may be unrecognized by patients (34,35). Lack of awareness of the relevance of diabetic symptoms to the disease is common in undiagnosed diabetic patients (36) and results in delayed diagnosis and poor prognosis. Our data revealed that the disparity of diabetes care was persistent after controlling for geographic locality, indicating the association between income level and quality of diabetes care is independent of the urban or rural setting. To optimize quality of diabetes care, apart from ameliorating access to health care, diabetes-related health literacy also needs to be improved for the general populace, particularly for the economically disadvantaged. It cannot be overemphasized that individualized patient education is important to reduce disparities in self-management and health care–seeking behavior among diabetic patients according to SES. As indicated in this study, the quality of diabetes care in Taiwan falls far short of standard recommendations. Although the completeness of fasting glucose testing is high (about 90%), the annual testing rates for HbA1c, LDL cholesterol, triglycerides, creatinine, urine dipstick, urine microalbumin, and retinopathy are generally low, although some improvement has been observed over time (data not shown). Suboptimal diabetes care in Taiwan was also reported by Tseng et al. (37). Because all aforementioned tests are covered by the Taiwanese NHI program and should be ordered by physicians, the lack of regular monitoring is apparently related to a paucity of professional accountability. Health providers’ responsiveness to diabetes care must be promoted before we can develop effective strategies to reduce SES disparity in diabetes care.
This study has several limitations. First, because there is no laboratory information recorded in the NHI data sets, the diabetes diagnosis was not based on clinical criteria, and we did not include some important clinical confounders (e.g., BMI) in the models to assess diabetes incidence. Instead, we used a conservative method to define diabetes, but one by which the accuracy of case finding can reach 96.1% (38). Second, individual insurable income, the only socioeconomic indicator available for analysis, as used to define the SES gradient, may underestimate a subject’s real income; it might also have been more appropriate to use family disposable income, occupation status, or education level to measure socioeconomic status had they been available to us. We were able to define clearly the disadvantaged, however, by identifying those in the “low-income households” entitled to be exempted from NHI premiums and copayments. We consider that the poor people in this study correctly represent those living below the local lowest living index in Taiwan. Again, lack of laboratory data in the NHI data sets prevents us from direct measurement of clinical outcomes; however, the recorded metabolic tests and referrals for retinal examination used for quality evaluation in this study constituted process measures for agreed best practice in diabetes care. The completion of these process indicators is indicative of the conduct of the required level of professional accountability.
In conclusion, we have shown that poverty is related to an increase in diabetes development in an Asian population, especially among women. Furthermore, income disparity appears to predispose people with diabetes toward receiving unequal diabetes care, which includes delayed case identification and inadequate follow-up, even in a nation with a comprehensive universal health insurance program. This study indicates that the improvement of access through comprehensive and universal health coverage is merely a start toward eliminating inequality in diabetes care, not a silver bullet. Of the multiple strategies designed to mitigate the discrepancies in diabetes care caused by the SES gradient, promoting health literacy in diabetes, minimizing geographic variation of access to diabetes care, optimizing the primary care physician’s function, and reinforcing health providers’ accountability are likely to be the missing steps required to ensure high-quality diabetes care in Taiwan and probably elsewhere.
Acknowledgments
This study was supported by the Taiwanese National Science Council (Project Grant NSC 99-2314-B-400-002-MY2).
No potential conflicts of interest relevant to this article were reported.
C.-C.H. designed the study and conceived the idea. C.-C.H., C.-T.H., and J.-S.C. analyzed and interpreted the data. C.-C.H. and M.L.W. drafted the article. L.C., H.-L.H., S.-J.S., C.-H.L., H.-Y.C., S.-F.S., W.-C.T., and T.C. critically revised the article for important intellectual content. C.-C.H. and J.-S.C. had final approval of the article. H.-Y.C. and S.-F.S. provided statistical expertise. C.-T.H. provided administrative and logistical support. All authors reviewed the manuscript and had final responsibility for the decision to submit for publication. C.-C.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and diagnosed diabetes incidence. Diabetes Res Clin Pract 2005;68:230–236 [DOI] [PubMed] [Google Scholar]
- 2.Krishnan S, Cozier YC, Rosenberg L, Palmer JR. Socioeconomic status and incidence of type 2 diabetes: results from the Black Women’s Health Study. Am J Epidemiol 2010;171:564–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res 2002;53:891–895 [DOI] [PubMed] [Google Scholar]
- 4.Rathmann W, Strassburger K, Heier M, et al. Incidence of Type 2 diabetes in the elderly German population and the effect of clinical and lifestyle risk factors: KORA S4/F4 cohort study. Diabet Med 2009;26:1212–1219 [DOI] [PubMed] [Google Scholar]
- 5.Chaturvedi N, Jarrett J, Shipley MJ, Fuller JH. Socioeconomic gradient in morbidity and mortality in people with diabetes: cohort study findings from the Whitehall Study and the WHO Multinational Study of Vascular Disease in Diabetes. BMJ 1998;316:100–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weng C, Coppini DV, Sönksen PH. Geographic and social factors are related to increased morbidity and mortality rates in diabetic patients. Diabet Med 2000;17:612–617 [DOI] [PubMed] [Google Scholar]
- 7.Walker JJ, Livingstone SJ, Colhoun HM, et al. Scottish Diabetes Research Network Epidemiology Group Effect of socioeconomic status on mortality among people with type 2 diabetes: a study from the Scottish Diabetes Research Network Epidemiology Group. Diabetes Care 2011;34:1127–1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown AF, Ettner SL, Piette J, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev 2004;26:63–77 [DOI] [PubMed] [Google Scholar]
- 9.Maitra S. Can patient self-management explain the health gradient? Goldman and Smith’s “Can patient self-management help explain the SES health gradient?” (2002) revisited. Soc Sci Med 2010;70:802–812; discussion 813–815 [DOI] [PubMed] [Google Scholar]
- 10.Brown AF, Gregg EW, Stevens MR, et al. Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care 2005;28:2864–2870 [DOI] [PubMed] [Google Scholar]
- 11.Booth GL, Hux JE. Relationship between avoidable hospitalizations for diabetes mellitus and income level. Arch Intern Med 2003;163:101–106 [DOI] [PubMed] [Google Scholar]
- 12.Jotkowitz AB, Rabinowitz G, Raskin Segal A, Weitzman R, Epstein L, Porath A. Do patients with diabetes and low socioeconomic status receive less care and have worse outcomes? A national study. Am J Med 2006;119:665–669 [DOI] [PubMed] [Google Scholar]
- 13.Wilf-Miron R, Peled R, Yaari E, et al. Disparities in diabetes care: role of the patient’s socio-demographic characteristics. BMC Public Health 2010;10:729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luft HS. Universal health care coverage: a potential hybrid solution. JAMA 2007;297:1115–1118 [DOI] [PubMed] [Google Scholar]
- 15.Sehgal AR. Universal health care as a health disparity intervention. Ann Intern Med 2009;150:561–562 [DOI] [PubMed] [Google Scholar]
- 16.Doherty RB. Universal health care coverage in the United States: Is it “slip slidin’ away”? Ann Intern Med 2011;154:118–120 [DOI] [PubMed] [Google Scholar]
- 17.Cheng TM. Taiwan’s new national health insurance program: genesis and experience so far. Health Aff (Millwood) 2003;22:61–76 [DOI] [PubMed] [Google Scholar]
- 18.Connors EE, Gostin LO. Health care reform—a historic moment in US social policy. JAMA 2010;303:2521–2522 [DOI] [PubMed] [Google Scholar]
- 19.Latko B, Temporão JG, Frenk J, et al. The growing movement for universal health coverage. Lancet 2011;377:2161–2163 [DOI] [PubMed] [Google Scholar]
- 20.National Health Research Institutes. National Health Insurance Research Database (NHIRD). [Internet]. Available from http://w3.nhri.org.tw/nhird/date_01.html Accessed 30 May 2011
- 21.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613–619 [DOI] [PubMed] [Google Scholar]
- 22.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr 2004;79:6–16 [DOI] [PubMed] [Google Scholar]
- 23.Auchincloss AH, Diez Roux AV, Mujahid MS, Shen M, Bertoni AG, Carnethon MR. Neighborhood resources for physical activity and healthy foods and incidence of type 2 diabetes mellitus: the Multi-Ethnic study of Atherosclerosis. Arch Intern Med 2009;169:1698–1704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Norberg M, Stenlund H, Lindahl B, Andersson C, Eriksson JW, Weinehall L. Work stress and low emotional support is associated with increased risk of future type 2 diabetes in women. Diabetes Res Clin Pract 2007;76:368–377 [DOI] [PubMed] [Google Scholar]
- 25.Wen TH, Chen DR, Tsai MJ. Identifying geographical variations in poverty-obesity relationships: empirical evidence from Taiwan. Geospat Health 2010;4:257–265 [DOI] [PubMed] [Google Scholar]
- 26.Wai JP, Wen CP, Chan HT, et al. Assessing physical activity in an Asian country: low energy expenditure and exercise frequency among adults in Taiwan. Asia Pac J Clin Nutr 2008;17:297–308 [PubMed] [Google Scholar]
- 27.Cheng TY, Wen CP, Tsai MC, Tsai SP. The current status of smoking behavior in Taiwan: data analysis from National Health Interview Survey in 2001. Taiwan J Public Health 2003;22:453–464 [Google Scholar]
- 28.Bell RA, Camacho F, Goonan K, et al. Quality of diabetes care among low-income patients in North Carolina. Am J Prev Med 2001;21:124–131 [DOI] [PubMed] [Google Scholar]
- 29.Asch SM, Sloss EM, Hogan C, Brook RH, Kravitz RL. Measuring underuse of necessary care among elderly Medicare beneficiaries using inpatient and outpatient claims. JAMA 2000;284:2325–2333 [DOI] [PubMed] [Google Scholar]
- 30.Bureau of National Health Insurance. National Health Insurance in Taiwan 2010. [Internet]. Available from http://www.nhi.gov.tw/Resource/webdata/Attach_13767_1_National%20Health%20Insurance%20in%20Taiwan%202010.pdf.Accessed9June2011
- 31.Huang MC, Hsu CC, Wang HS, Shin SJ. Prospective randomized controlled trial to evaluate effectiveness of registered dietitian-led diabetes management on glycemic and diet control in a primary care setting in Taiwan. Diabetes Care 2010;33:233–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernheim SM, Ross JS, Krumholz HM, Bradley EH. Influence of patients’ socioeconomic status on clinical management decisions: a qualitative study. Ann Fam Med 2008;6:53–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Willems S, De Maesschalck S, Deveugele M, Derese A, De Maeseneer J. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns 2005;56:139–146 [DOI] [PubMed] [Google Scholar]
- 34.Singh BM, Jackson DM, Wills R, Davies J, Wise PH. Delayed diagnosis in non-insulin dependent diabetes mellitus. BMJ 1992;304:1154–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.UK Prospective Diabetes Study. IV. Characteristics of newly presenting type 2 diabetic patients: male preponderance and obesity at different ages. Multi-center study. Diabet Med 1988;5:154–159 [PubMed] [Google Scholar]
- 36.Koopman RJ, Mainous AG, 3rd, Jeffcoat AS. Moving from undiagnosed to diagnosed diabetes: the patient’s perspective. Fam Med 2004;36:727–732 [PubMed] [Google Scholar]
- 37.Tseng FY, Lai MS, Syu CY, Lin CC. Professional accountability for diabetes care in Taiwan. Diabetes Res Clin Pract 2006;71:192–201 [DOI] [PubMed] [Google Scholar]
- 38.Lin CC, Lai MS, Syu CY, Chang SC, Tseng FY. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J Formos Med Assoc 2005;104:157–163 [PubMed] [Google Scholar]