Abstract
Rationale
Delay discounting (DD) describes the rate at which reinforcers lose value as the temporal delay to their receipt increases. Steeper discounting has been positively associated with vulnerability to substance use disorders, including cocaine use disorders.
Objectives
In the present study, we examined whether DD of hypothetical monetary reinforcers is associated with the duration of cocaine abstinence achieved among cocaine-dependent outpatients.
Methods
Participants were 36 adults who were participating in a randomized controlled trial examining the efficacy of voucher-based contingency management (CM) using low-magnitude (N = 18) or high-magnitude (N = 18) voucher monetary values.
Results
DD was associated with the number of continuous weeks of cocaine abstinence achieved, even after adjusting for treatment condition during the initial 12-week (t(33) = 2.48, p = .045) and entire recommended 24-week of treatment (t(33) = 2.40, p = .022). Participants who exhibited steeper discounting functions achieved shorter periods of abstinence in the Low-magnitude voucher condition (12-week: t(16) = 2.48, p = .025; 24-week: t(16) = 2.68, p = .017), but not in the High-magnitude voucher condition (12-week: t(16) = 0.51, p = .618; 24-week: t(16) = 1.08, p = .298), although the interaction between DD and treatment condition was not significant (12-week: t(32) = −1.12, p = .271; 24-week: t(32) = −0.37, p = .712).
Conclusions
These results provide further evidence on associations between DD and treatment response and extend those observations to a new clinical population (i.e., cocaine-dependent outpatients), while also suggesting that a more intensive intervention like the High-magnitude CM condition may diminish this negative relationship between DD and treatment response.
Key Terms: Temporal discounting, delay discounting, cocaine dependence, contingency management, vouchers, treatment response
Introduction
Delay discounting (DD) describes a relationship wherein the value of a reinforcer decreases as a hyperbolic function of the length of temporal delay to its availability (Rachlin & Green, 1972). This relationship between the delay to reinforcement and discounted value is orderly and described as follows (Mazur, 1987): The value (V) of a reinforcer of some amount (A) is discounted as a function of delay (D) to receiving that reinforcer. The free parameter k indicates the rate at which the delayed reinforcer is discounted. Higher k values indicate steeper discounting, and their hyperbolic discounting functions show steeper declines relative to lower k values. In an adjusting-amounts task as was used in the present study, participants are typically asked to choose between a smaller, immediate amount and a delayed, larger amount (Rachlin, Raineri, & Cross, 1991). Indifference points are determined by adjusting the value of the immediate amount until it is deemed by the participant to be equivalent to the value of the delayed amount. That is, the indifference point is the point at which both the immediate and delayed amounts subjectively have the same value (Madden & Johnson, 2010).
DD has been investigated across various types of substance use disorders (SUDs), including cocaine (Heil et al., 2006), opioid (Madden et al., 1999), alcohol (MacKillop et al., 2007; Vuchinich & Simpson, 1998), and nicotine dependence (Bickel et al., 1999). A common finding across these studies is that discounting of hypothetical monetary reinforcers reliably discriminates between individuals with SUDs and control subjects without SUDs (Bickel & Marsch, 2001; Bickel et al., 2007) and in some instances between individuals with different severities of SUDs (Ohmura et al., 2005, Yi, Mitchell, & Bickel, 2010).
In several recent studies examining DD in clinical populations, especially nicotine-dependent cigarette smokers and opioid-dependent adults, steeper discounting has predicted poorer treatment outcome (Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Passetti et al., 2008; Yoon et al., 2007). Krishnan-Sarin et al. (2007) focused on adolescent smokers who participated in a high school based smoking-cessation program combining contingency management (CM) and cognitive behavioral therapy. Those with steeper discounting of real monetary reinforcers sustained a shorter period of abstinence from smoking during a 4-week treatment. MacKillop and Kahler (2009) treated nicotine-dependent adults who were also heavy drinkers with eight weeks of nicotine replacement therapy combined with three weeks of individual counseling. Those with steeper discounting of hypothetical monetary reinforcers had fewer days to the first smoking lapse. Passetti et al. (2008) reported a non-significant trend towards steeper discounting of real monetary reinforcers among opioid-dependent patients with frequent lapses back to illicit drug use compared to abstainers. Finally, Yoon et al. (2007) demonstrated that among pregnant women who quit smoking during pregnancy, those with steeper discounting of hypothetical monetary rewards relapsed back to smoking sooner during postpartum.
The purpose of the present study was to examine whether DD of hypothetical monetary reinforcement was associated with treatment response among cocaine-dependent outpatients who participated in a randomized controlled trial examining the influence of voucher monetary values on outcomes in a contingency-management (CM) intervention (Higgins et al., 2007). Our group previously reported that a period of sustained abstinence did not alter DD in these subjects (Heil et al., 2006). The present study investigated whether DD was associated with the amount of cocaine abstinence achieved during treatment and whether any such associations might vary by whether patients received low or high-magnitude voucher-based CM.
Method
Participants
Study participants were the 36 cocaine-dependent adult outpatients from the Heil et al. study who participated in a randomized clinical trial investigating different magnitudes of voucher-based CM therapy (Higgins et al., 2007). All participants completed a computerized DD measure (described below) at some point during the course of treatment. The average number of days in treatment prior to implementing the DD measure was 77.06 ± 10.7 days for all participants, 83.28 ± 15.02 days for those in the Low-magnitude voucher condition, and 70.83 ± 15.54 days for those in the High-magnitude voucher condition.
To be included in the trial, individuals had to be at least 18 years of age, meet criteria for current cocaine dependence [Diagnostic and Statistical Manual version IV (DSM-IV); American Psychiatric Association], have used cocaine in the past 30 days, and reside within the county in which the clinic is located. Exclusion criteria were current physical dependence on opioids or sedatives, psychosis, dementia, pregnancy, plans to leave the immediate geographical area within 12 months (including pending incarceration), and having a significant other already enrolled in the trial. Additional information about methods and the manual-guided Community Reinforcement Approach (CRA) plus vouchers therapy used in this trial is provided in Higgins et al. (2007). The 36 participants included in the present study were the only ones in the trial who completed the DD task. They were recruited as a convenience sample for the Heil et al. study examining whether DD differed between cocaine-dependent individuals and a control sample without SUDs and whether a period of sustained abstinence altered DD rates within the cocaine-dependent sample. An additional seven cocaine-dependent participants in the Heil et al. study were excluded from the present study because they received miscellaneous treatments that precluded meaningful investigation of how associations between DD and treatment response might vary by treatment condition.
Assessment of DD
The DD task was conducted in a quiet room, in which participants used a notebook computer running Microsoft Visual Basic 6.0 with a staff member present. The DD program we used has been described previously (Johnson & Bickel, 2002). Briefly, participants were seated in front of a computer screen, which displayed the following message:
Imagine that you have a choice between waiting (length of time) and then receiving $1,000 and receiving a smaller amount of money right away. Please choose between the two options.
In the instructions, the length of time given was either 1 day, 1 week, 1 month, 6 months, 1 year, 5 years, or 25 years. When participants were ready to begin the task, they clicked on the start button located on the screen, and the DD program was initiated. Participants chose between two different options, always a fixed amount ($1,000) at a fixed delay, or a smaller amount available immediately. The DD program adjusted the value of the smaller reinforcer in each trial according to an algorithm wherein adjusted values of the smaller reinforcer were presented across trials until an indifference point was determined, in which the value of the smaller, immediate amount was subjectively equivalent to the delayed $1,000 reinforcer (Johnson & Bickel, 2002). Once an indifference point for a given delay was determined, the next delay was introduced until indifference points were established for each of the seven delays noted above. The order of the delays was presented in a fixed ascending or descending order for a given participant but determined randomly across participants. Prior to assessment of each new delay, participants were presented again with the instructions described above.
Urinalysis Monitoring
Urine specimens were collected from all study participants according to a thrice-weekly schedule (Monday, Wednesday, Friday) during weeks 1–12 and a twice-weekly schedule (Monday, Thursday) during weeks 13–24 of treatment. Specimens were screened immediately using an on-site enzyme-multiplied immunoassay technique (Syva, San Jose, CA, USA). Specimens were obtained under observation of a same-sex staff member and screened for benzoylecgonine, a cocaine metabolite. Benzoylecgonine levels of 300 ng/ml and above were considered positive for cocaine use; one randomly selected specimen each week was also screened for the presence of other abused drugs. Failure to submit specimens on five consecutive occasions resulted in termination from treatment. Participants were informed of urinalysis results within several minutes of specimen collection.
Statistical Methods
The hyperbolic model V = A/(1+kD) was fit to each participant’s indifference points using nonlinear regression (SAS, PROC NLIN). Each participant’s derived discounting parameter (k) was used to compute corresponding ED50 values (1/k) for subsequent analyses (Yoon & Higgins, 2008). These ED50 values represent the estimated delay at which the immediate value of the reinforcer was discounted by 50% and provides an intuitive interpretation of the rate of discounting. For example, a k value of 0.001 equals to 1000 days as the ED50 value, indicating that the delayed outcome lost 50% of its original objective value by 1000 days.
Because the distribution of ED50 values is typically skewed, the natural log transformation of ED50 values was employed, which normalized the distribution of ED50 values for subsequent statistical analyses. It is important to note that log transformed ED50 values and log transformed k values differ only by sign [i.e., log(k) = −(log(ED50)].
Linear regression analysis was used to examine whether the estimated ED50 values of participants were associated with treatment outcome, expressed as weeks of continuous cocaine abstinence. Treatment condition was included as an additional explanatory variable in the model. These regression analyses were performed both with and without an interaction term. Regression models were also run within each treatment condition. Stepwise regression was used to examine the role of demographics, drug use characteristics, and days in treatment prior to the discounting task as potential confounds. Finally, demographic and drug use characteristics were compared between treatment conditions using t-tests for continuous measures and chi-square tests for categorical variables. All analyses were performed using SAS Version 9 statistical software (SAS Institute, Cary NC). Statistical significance was determined based on α = .05.
Results
Participants Characteristics
Table 1 shows participant characteristics in each voucher condition. No significant differences were observed between treatment conditions in any participant characteristics. Table 2 displays estimated discounting parameters (i.e. k values) and corresponding ED50 values for all participants by treatment condition. No significant difference in these measures was observed between treatment conditions (t(34) = 0.33, p = .745).
Table 1.
Participant Characteristics
| High Voucher (n=18) | Low Voucher (n=18) | p-value | |
|---|---|---|---|
| Demographics | |||
| Gender (% male) | 67 | 56 | 0.49 |
| Age, years | 33.05 ± 6.90 | 34.81 ± 6.16 | 0.43 |
| Education, yearsa | 12.44± 2.03 | 12.62± 2.20 | 0.79 |
| Employment (% full time) | 61 | 61 | 1.00 |
| Income/weekb, c | 360 (200, 625) | 298 (200, 450) | 0.69 |
| Marital status (% never married) | 61 | 39 | 0.18 |
| Cocaine Use | |||
| No. of days cocaine used in past 30 days | 11.44 ± 8.12 | 9.56 ± 6.88 | 0.46 |
| Years of regular cocaine use | 7.67 ± 5.49 | 8.47 ± 6.42 | 0.69 |
| Years of occasional cocaine use | 3.38 ± 3.13 | 3.82 ± 5.33 | 0.76 |
| Age first used cocaine | 20.22 ± 4.75 | 21.61± 5.89 | 0.44 |
| Preferred route of cocaine use (%) | |||
| intranasal (i.n.) | 44 | 28 | 0.22 |
| smoke | 39 | 67 | |
| intravenous (i.v.) | 17 | 6 | |
| $/week spent on cocainec | 200 (106, 420) | 165 (75, 358) | 0.59 |
| Prior cocaine treatment (%) | 44 | 61 | 0.32 |
| Other Drug Dependence | |||
| Alcohol dependent (%) | 44 | 50 | 0.74 |
| Cannabis dependent (%) | 28 | 22 | 0.70 |
| Nicotine dependent (%) | 78 | 56 | 0.16 |
| Michigan Alcohol Screening Test Score | 18.41± 14.74 | 18.50 ± 13.37 | 0.99 |
| Beck Depression Inventory (BDI) Score | 20.78 ± 11.68 | 20.13 ± 8.28 | 0.86 |
Notes:
means ± SD unless noted otherwise.
data includes employed and unemployed participants.
median (interquartile range).
Table 2.
Discounting Performance (N = 36)
| Low voucher condition (n = 18) | High voucher condition (n = 18) | ||||
|---|---|---|---|---|---|
|
| |||||
| Subject# | k values | ED50 values (days) | Subject# | k values | ED50 values (days) |
| 1 | 0.000006 | 176310.16 | 1 | 0.000011 | 94845.07 |
| 2 | 0.000023 | 43477.55 | 2 | 0.000079 | 12581.72 |
| 3 | 0.000246 | 4064.31 | 3 | 0.000239 | 4188.09 |
| 4 | 0.000521 | 1919.85 | 4 | 0.000431 | 2321.57 |
| 5 | 0.000617 | 1619.71 | 5 | 0.000435 | 2298.47 |
| 6 | 0.001855 | 539.15 | 6 | 0.000754 | 1326.10 |
| 7 | 0.002358 | 424.11 | 7 | 0.000793 | 1261.43 |
| 8 | 0.002504 | 399.41 | 8 | 0.001008 | 992.27 |
| 9 | 0.002880 | 347.23 | 9 | 0.004992 | 200.34 |
| 10 | 0.005407 | 184.93 | 10 | 0.005407 | 184.93 |
| 11 | 0.007828 | 127.74 | 11 | 0.006874 | 145.47 |
| 12 | 0.020242 | 49.40 | 12 | 0.007597 | 131.63 |
| 13 | 0.021068 | 47.47 | 13 | 0.008148 | 122.73 |
| 14 | 0.022371 | 44.70 | 14 | 0.008566 | 116.75 |
| 15 | 0.025223 | 39.65 | 15 | 0.017953 | 55.70 |
| 16 | 0.045502 | 21.98 | 16 | 0.038388 | 26.05 |
| 17 | 0.065219 | 15.33 | 17 | 0.078866 | 12.68 |
| 18 | 1.336427 | 0.75 | 18 | 0.444858 | 2.25 |
|
| |||||
| Median (interquartile range) | 0.0041 (0.00062, 0.0223) | 266 (45, 1619) | Median (interquartile range) | 0.0052 (0.00043, 0.00856) | 192 (116, 2298) |
Association of DD with Treatment Outcome
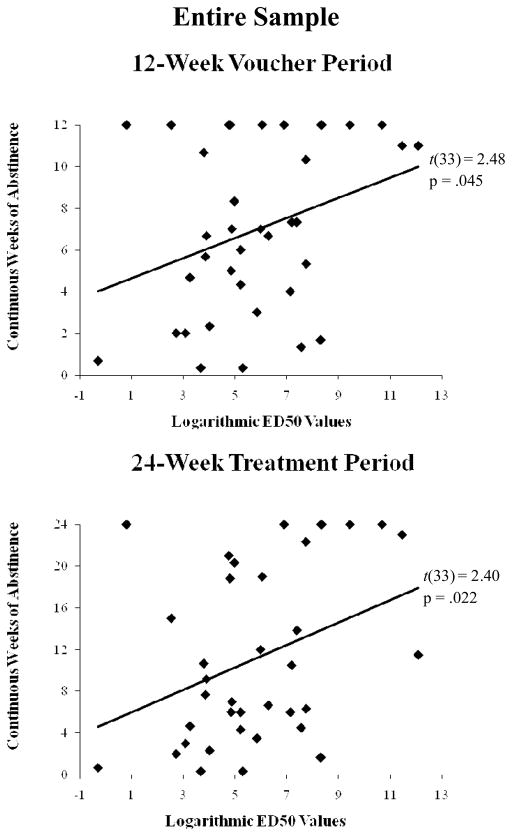
The discounting equation provided a good fit to the data with median R2 values of 0.91, 0.96, and 0.86 for all participants, those in the Low-magnitude voucher condition, and those in the High-magnitude voucher condition, respectively. Regression analyses indicated that DD was significantly associated with the duration of continuous cocaine abstinence achieved during the initial 12 weeks of treatment when the voucher program was operating (t(33) = 2.48, p = .045) even after adjusting for treatment condition, which was also a significant explanatory variable (t(33) = 2.17, p = .037) (Figure 1 top panel). Similar results were observed for the overall 24-week treatment period, with significant effects associated with DD (t(33) = 2.40, p = .022) and treatment condition (t(33) = 2.60, p = .014) (Figure 1 bottom panel). Participants receiving the higher magnitude vouchers achieved an estimated 6.3 weeks greater abstinence than those receiving the lower magnitude vouchers (t(33) = 2.5, p = .014).
Figure 1.
Best fit line representing the relationship between continuous weeks of abstinence and logarithmic ED50, which was evaluated at the mean of the indicator variable representing treatment for the entire sample during the 12-week voucher period (top panel) and 24-week treatment period (bottom panel). The ED50 value indicates the number of days that takes to lose 50% of the original objective value of a reinforcer, and is expressed as an inverted k (1/k). The greater the ED50 value, the greater the number of days needed for the reinforcer to lose 50% of its original objective value (i.e., low impulsivity).
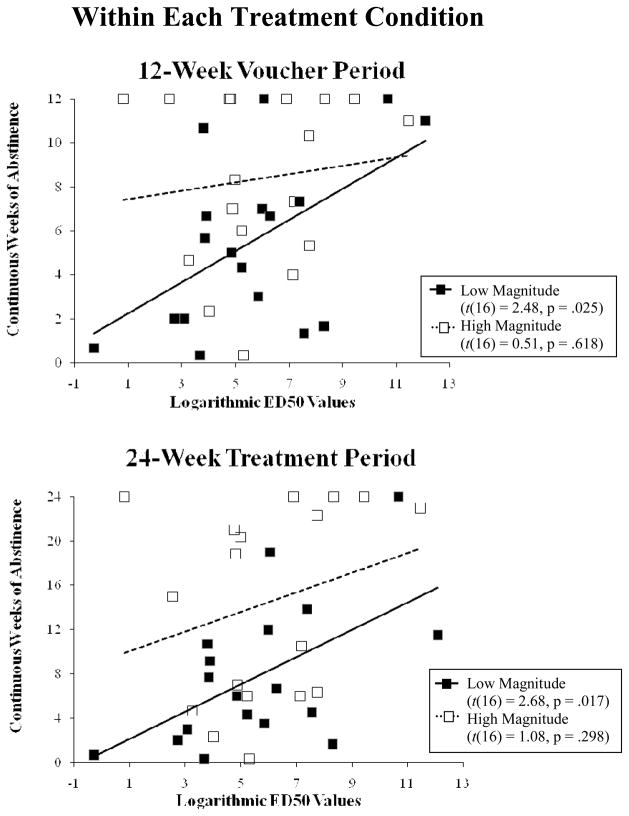
While no evidence of an interaction between DD and treatment condition was observed (t(32) = −1.12, p = .271), the relationship between DD and continuous abstinence during the initial 12-week period was significant within the Low-magnitude voucher condition (t(16) = 2.48, p = .025), but not within the High-magnitude voucher condition (t(16) = 0.51, p = .618) (Figure 2 top panel). Similar relationships were observed during the 24-week period, with DD being a significant explanatory variable in the Low- but not the High-magnitude conditions (Low-magnitude: t(16) = 2.68, p = .017, High-magnitude: t(16) = 1.08, p = .298)(Figure 2 bottom panel) and a non-significant interaction between treatment condition and DD (t(32) = −0.37, p = .712).
Figure 2.
Regression line between logarithmic ED50 and continuous weeks of abstinence in each treatment condition during the 12-week voucher period (top panel) and 24-week treatment period (bottom panel).
To investigate whether the relationship between DD and abstinence was confounded by other variables, stepwise regression was conducted using participant characteristics and days in treatment as candidate explanatory variables. After adjusting for treatment condition, DD was the only significant explanatory variable that met the entry criterion (p < .05) for the models corresponding to the 12- and 24-week time periods.
Discussion
To our knowledge, this is the first study to report significant associations between DD and treatment response among those being treated for cocaine dependence. DD was a significant explanatory variable of treatment response even after adjusting for treatment condition, the number of days in treatment, and demographic characteristics. The results were also suggestive of an interaction between DD and treatment condition, with steeper discounting associated with significantly shorter periods of abstinence within the Low-magnitude voucher condition but not within the High-magnitude voucher condition; however, a significant interaction was not observed. The difference between treatment conditions was especially pronounced when analyses were restricted to abstinence achieved during the initial 12-week period when the voucher program was operating.
These findings suggest that CM, at least high-magnitude CM, may be especially helpful in promoting abstinence among those with steeper DD, that is, individuals who would be expected to be less sensitive to potential naturalistic reinforcers such as improved health or family relations by remaining abstinent from cocaine use. The benefits of cocaine abstinence can be quite substantive but also associated with considerable temporal delays before being realized, including such examples as improved health (Higgins et al., 2003), healthy social network and recreational activities (Rogers et al., 2008), improved family relationships (Higgins et al., 1994), and stable employment (Higgins et al., 2003).
We want to acknowledge three potential limitations of the present study. First, the relatively small number of participants studied meant that the study was underpowered for adequately examining the interaction between DD and treatment condition. We believe that the present results are sufficiently promising to warrant future investigation of this relationship, which should help to elucidate the conditions under which DD is associated with treatment response, may provide insights into how CM and other interventions improve outcomes (i.e., mechanisms of action), and perhaps help to identify the type of interventions that will allow patients with steeper DD to succeed in treatment. Second, we used hypothetical instead of real money in estimating DD. Direct comparisons of real versus hypothetical reinforcers have produced generally comparable results (Johnson & Bickel, 2002). Nevertheless, there were outliers in the discounting result that may be an artifact of using hypothetical consequences. In particular, three participants showed extremely low k values and high ED50 values in the present study, taking more than 119 years to lose 50% of the original objective value of the reinforcer (i.e., low impulsivity). Future investigation may include examining discounting of real monetary reinforcers, which may influence on such extremely low discounting behavior. Third, where in the course of treatment DD was assessed varied across participants in the present study, which may have unnecessarily increased between-subject variability. That said, the number of days in treatment prior to completing the DD assessment was not a significant confounding variable in the regression model, and DD has been shown in other studies to be highly stable over many months (Audrain-McGovern et al., 2009; Takahashi et al., 2007; Yoon et al., 2007) suggesting that it is unlikely that this potential limitation had a substantive influence on the results obtained. This also suggests that the DD measure is likely to have utility in predicting treatment response if implemented upon entry into treatment.
In conclusion, the present findings extend to cocaine-dependent patients prior observations with cigarette smokers and opioid-dependent patients showing that steeper discounting predicts less during-treatment and post-treatment abstinence (Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Passetti et al., 2008; Yoon et al., 2007). In addition, the relationship between steeper discounting and shorter periods of abstinence may be conditional on the type or intensity of treatment provided, which, to our knowledge, has not been reported previously.
Acknowledgments
This research was supported byresearch grant R01DA009378 and training grant T32 DA07242 from the National Institute on Drug Abuse.
References
- Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, Wileyto EP. Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug and Alcohol Dependence. 2009;103:99–106. doi: 10.1016/j.drugalcdep.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: Delay discounting processes. Addiction. 2001;96:73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Miller ML, Yi R, Kowal BP, Lindquist DM, Pitcock JA. Behavioral and neuroeconomics of drug addiction: Competing neural systems and temporal discounting processes. Drug and Alcohol Dependence. 2007;90:85–91. doi: 10.1016/j.drugalcdep.2006.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Odum AL, Madden GJ. Impulsivity and cigarette smoking: Delay discounting in current, never, and ex-smokers. Psychopharmacology. 1999;146:447–454. doi: 10.1007/pl00005490. [DOI] [PubMed] [Google Scholar]
- Heil SH, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addictive Behaviors. 2006;31:1290–1294. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Badger GJ. Participation of significant others in outpatient behavioral treatment predicts greater cocaine abstinence. The American Journal of Drug and Alcohol Abuse. 1994;20:47–56. doi: 10.3109/00952999409084056. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Sigmon SC, Wong CJ, Heil SH, Badger GJ, Donham R, Dantona RL, Anthony S. Community reinforcement therapy for cocaine-dependent outpatients. Archives of General Psychiatry. 2003;60:1043–1052. doi: 10.1001/archpsyc.60.9.1043. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Dantona R, Donham R, Matthews M, Badger GJ. Effects of varying the monetary value of voucher-based incentives on abstinence achieved during and following treatment among cocaine-dependent outpatients. Addition. 2007;102:271–281. doi: 10.1111/j.1360-0443.2006.01664.x. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. Within-subject comparison of real and hypothetical money rewards in delay discounting. Journal of the Experimental Analysis of Behavior. 2002;77:129–146. doi: 10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, Potenza MN. Behavioral impulsivity predicts treatment outcome in a smoking cessation program. Drug and Alcohol Dependence. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Mattson RE, Anderson-MacKillop EJ, Castelda BA, Donovick PJ. Multidimensional assessment of impulsivity in undergraduate hazardous drinkers and controls. Journal of Studies on Alcohol and Drugs. 2007;68:785–788. doi: 10.15288/jsad.2007.68.785. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Bickel WK, Jacobs EA. Discounting of delayed rewards in opioid-dependent outpatients: Exponential or hyperbolic discounting functions? Experimental and Clinical Psychopharmacology. 1999;7:284–293. doi: 10.1037//1064-1297.7.3.284. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Johnson PS. A delay-discounting primer. In: Madden GJ, Bickel WK, editors. Impulsivity: The behavioral and neurological science of discounting. Washington, DC: American Psychological Association; 2010. pp. 11–37. [Google Scholar]
- Mazur JE. An adjusting procedure for studying delayed reinforcement. In: Commons ML, Mazur JE, Nevin JA, Rachlin H, editors. Quantitative analyses of behavior: Vol. 5. The effects of delay and of intervening events on reinforcement value. Hillsdale, NJ: Erlbaum; 1987. pp. 55–73. [Google Scholar]
- Passetti F, Clark L, Mehta MA, Joyce E, King M. Neuropsychological predictors of clinical outcome in opiate addiction. Drug and Alcohol Dependence. 2008;94:82–91. doi: 10.1016/j.drugalcdep.2007.10.008. [DOI] [PubMed] [Google Scholar]
- Rachlin H, Green L. Commitment, choice, and self-control. Journal of the Experimental Analysis of Behavior. 1972;17:15–22. doi: 10.1901/jeab.1972.17-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachlin H, Raineri A, Cross D. Subjective probability and delay. Journal of the Experimental Analysis of Behavior. 1991;55:233–244. doi: 10.1901/jeab.1991.55-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RE, Higgins ST, Silverman K, Thomas CS, Badger GJ, Bigelow G, Stitzer M. Abstinence-contingent reinforcement and engagement in non-drug-related activities among illicit drug abusers. Psychology of Addictive Behaviors. 2008;22:544–550. doi: 10.1037/0893-164X.22.4.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohmura Y, Takahashi T, Kitamura N. Discounting delayed and probabilistic monetary gains and losses by smokers of cigarettes. Psychopharmacology. 2005;82:508–515. doi: 10.1007/s00213-005-0110-8. [DOI] [PubMed] [Google Scholar]
- Takahashi T, Furukawa A, Miyakawa T, Maesato H, Higuchi S. Two-month stability of hyperbolic discount rates for delayed monetary gains in abstinent inpatient alcoholics. Neuro Endocrinology Letters. 2007;28:131–136. [PubMed] [Google Scholar]
- Vuchinich RE, Simpson CA. Hyperbolic temporal discounting in social drinkers and problem drinkers. Experimental and Clinical Psychopharmacology. 1998;6:292–305. doi: 10.1037//1064-1297.6.3.292. [DOI] [PubMed] [Google Scholar]
- Yi R, Mitchell SH, Bickel WK. Delay-discounting and substance abuse-dependence. In: Madden GJ, Bickel WK, editors. Impulsivity: The behavioral and neurological science of discounting. Washington, DC: American Psychological Association; 2010. pp. 191–211. [Google Scholar]
- Yoon JH, Higgins ST. Turning k on its head: Comments on use of an ED50 in delay discounting research. Drug and Alcohol Dependence. 2008;95:169–172. doi: 10.1016/j.drugalcdep.2007.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, Badger GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Experimental Clinical Psychopharmacology. 2007;15:176–186. doi: 10.1037/1064-1297.15.2.186. [DOI] [PubMed] [Google Scholar]