Abstract
Objective
To examine if children use supplements to fill gaps in nutritionally inadequate diets or whether supplements contribute to already adequate or excessive micronutrient intakes from foods.
Study design
Data were analyzed for children (2–18 y) from the NHANES 2003–2006, a nationally representative, cross-sectional survey (n=7,250). Diet was assessed using two 24-hour recalls, and dietary supplement use was assessed with a 30-day questionnaire.
Results
Prevalence of supplements use was 21% (< 2 y) and 42% (2–8 y). Supplement users had higher micronutrient intakes than nonusers. Calcium and vitamin D intakes were low for all children. Inadequate intakes of phosphorus, copper, selenium, folate, and vitamins B-6 and B-12 were minimal from foods alone among 2–8 y olds. However, among 9–18 y olds, a higher prevalence of inadequate intakes of magnesium, phosphorus, and vitamins A, C, and E were observed. Supplement use increased the likelihood of intakes above the Upper Tolerable Intake Level for iron, zinc, copper, selenium, folic acid, and vitamins A and C.
Conclusions
Even with the use of supplements, more than a one-third of children failed to meet calcium and vitamin D recommendations. Children 2–8 y had nutritionally adequate diets regardless of supplement use. However, in children older than 8 y dietary supplements added micronutrients to diets that would have otherwise been inadequate for magnesium, phosphorus, vitamins A,C, and E. Supplement use contributed to the potential for excess intakes of some nutrients. These findings may have implications for reformulating dietary supplements for children.
Keywords: children, NHANES, dietary supplement, users and non-users of supplements
More than half of adults in the U.S. report using dietary supplements, most commonly multivitamin/mineral supplements (MVMM) (1–3). Among adults, dietary supplement users are more likely to be female (4, 5), leaner (4, 5), more physically active (5, 6) and to have higher levels of educational attainment and socioeconomic status than non-users (4, 7). Adult supplement users have higher total intakes of most micronutrients than non-users (5, 8, 9). However, very little is known about the differences in micronutrient intakes in children who do or do not use dietary supplements. Data from the National Health and Nutrition Examination Survey (NHANES) II (1976–1980) indicate that children who used supplements (< 19 y) had higher intakes of vitamin C and fruit and vegetables than non-users (10).
Parents who use dietary supplements are more likely to have children who do so (11). More than a third of infants, children, and adolescents (henceforth children) in the U.S. are reported to use a dietary supplements (1, 12). Picciano et al reported that MVMMs were the most commonly used type of dietary supplement and other frequently used supplements were vitamins A, C, D, and calcium and iron. It remains unclear whether dietary supplements provide micronutrient intakes to help children meet the micronutrient targets specified in the Dietary Reference Intakes (DRI) or whether supplements simply provide an excess of nutrients to children who already have adequate intakes from foods.
Methods
The National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention collects the NHANES data. Written informed consent was obtained for all participants and the survey protocol was approved by the Research Ethics Review Board at the NCHS. The NHANES data are publicly available and NCHS recommends that analysts combine four or more years of data to improve the reliability and stability of statistical estimates (13). This analysis was completed using NHANES 2003–2004 and NHANES 2005–2006 datasets. The combined sample included 18,063 participants who had provided 24-hour dietary intake data. Of these, those who were 19 y or older, pregnant or lactating were excluded, leaving an analytical sample of 7,250 for children ages 2 to 18 y. We also examined prevalence of dietary supplement use in those < 2 y of age (n = 1,703); however, complete dietary recall data is not available on this age group so that analysis is limited to basic descriptive data.
Dietary intake
Dietary Intake Using 24-hour Recalls
NHANES participants were asked to complete two dietary recall interviews. The first dietary recall interviews were collected in-person by trained dietary interviewers. Proxy respondents provided dietary information for young children and proxy-assisted interviews were used for 6 to 11 y olds. The second dietary recall interview was completed by telephone 3 to 10 days after the health examination. Both recalls were collected using the U.S. Department of Agriculture (USDA) Automated Multiple-Pass Method dietary interview methodology (14, 15).
Dietary Supplement Use
The dietary supplement questionnaire was collected as part of the household interview (16). This questionnaire assesses participants’ use of vitamins, minerals, herbs, and other dietary supplements over the past 30 days. Survey personnel also collected detailed information about the type, consumption frequency, duration, and amount of each reported dietary supplement that respondents took. The average daily intake of vitamins from dietary supplements was calculated for individuals using the number of days that supplement use was reported, the reported amount taken per day, and the serving size unit from the product label; the details on these procedures are available elsewhere (17, 18). We defined non-users of supplements as those who did not report taking a dietary supplement within the last 30 days. Users of dietary supplements are defined as those who reported taking a dietary supplement that contained a given vitamin or mineral within the last 30 days.
Comparisons to the DRI Values
The prevalence of inadequate dietary intakes of a group was determined using the Estimated Average Requirement (EAR) cut-point method for all vitamins and minerals except iron (18). The probability method was used to determine iron intakes below the EAR. Both the probability and the cut-point method require more than one 24-hour dietary recall in order to adjust the dietary intakes for individual variation in order to produce usual dietary intakes. The EAR cut-point method assumes that there is no correlation between intakes and requirements; the variance in intakes is greater than the variance of requirements; and the distribution of requirements is symmetrical around the EAR. If these assumptions are met, as was the case for all nutrients examined in this study except iron, the number of individuals with usual intakes below the EAR is proportionate to the prevalence of the group with inadequate intakes. Because the distribution of requirements for iron was skewed (i.e., not symmetrical), the cut-point method was not appropriate and the probability method was applied (19).
Vitamin Bioequivalence
Folic acid does not occur naturally in the food supply but, instead, is the form of the vitamin that manufacturers use to fortify foods and in dietary supplements. The bioavailability of food folate is lower than that of folic acid in fortified foods and dietary supplements. For this reason, the Food and Nutrition Board of the National Academies developed the dietary folate equivalent (DFE) to reflect this differential bioavailability (20). The EAR for folate is expressed in DFE whereas the Tolerable Upper Intake Level (UL) is for synthetic folic acid only. The Food and Nutrition Board established the EAR for vitamin A in μg of retinol activity equivalents to account for the different biological activities of retinol and the provitamin-A carotenoids (21). The UL for vitamin A applies only to μg of retinol and does not include the provitamin-A carotenoids. The DRI for vitamin E is established in mg of alpha-tocopherol (22). The UL for vitamin E is only for supplemental sources and does not include vitamin E that occurs naturally in foods. The UL is set for magnesium only from supplemental sources (23).
Statistical Analysis
We adjusted the 24-hour dietary recall data for within-person variability and other covariates using the National Cancer Institute (NCI) method (24); the amount-only part of the NCI method (i.e., not the frequency of intake that applies to usual intake of foods) is applicable to estimates of usual nutrient intakes. This method removes the effect of the sequence of the 24-hour dietary recall from the estimated nutrient intake distribution (Day 1 or Day 2). We also adjusted for the day of the week that the survey personnel collected the 24-hour recall data, which we dichotomized as weekend (Friday–Sunday) or weekday (Monday–Thursday). The final covariate was the use of dietary supplements. Additional details on the NCI method are available elsewhere (24), and the SAS macros necessary to fit this model and to estimate usual intake distributions are available on the NCI website (25).
All statistical analyses were performed using SAS (version 9.2, SAS Institute Inc., Cary, NC) software. Sample weights were used to account for differential non-response and non-coverage and to adjust for planned oversampling of some groups. Mean usual dietary and total vitamin and mineral intakes were estimated, and these means were compared between dietary supplement users and non-users and the proportion meeting the EAR and exceeding the UL by computing a Z-statistic. Significance was set at a Bonferroni-corrected p-value of <0.003.
Results
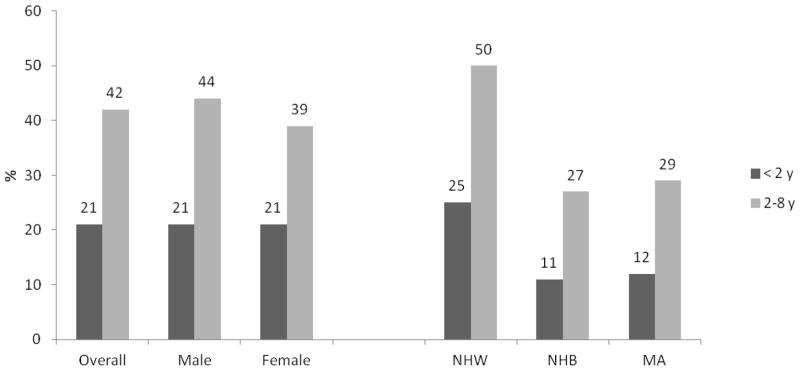
Prevalence of dietary supplement use varied by age. Among children less than the age of 2, 21% reported use of dietary supplements (Figure 1; available at www.jpeds.com). Non-Hispanic White infants (25%) were more likely than Non-Hispanic Black (11%) or Mexican American (12%) infants to use supplements. Among 2 – 8 y old children, 42% used dietary supplements (44% in males and 39% in females); non-Hispanic White children were reported to have higher use of supplements (50%) than non-Hispanic Black (27%) or Mexican American (29%) children. The prevalence of use of any dietary supplement by those 9 – 13 y (29% for both males and females) and 14 – 18 y (26%, 23% in males and 30% in females) has been reported elsewhere (1).
Figure 1.
Prevalence (%) of dietary supplement use by gender and race in infants (< 2y of age) and those aged 2–8 y in the U.S., 2003–2006
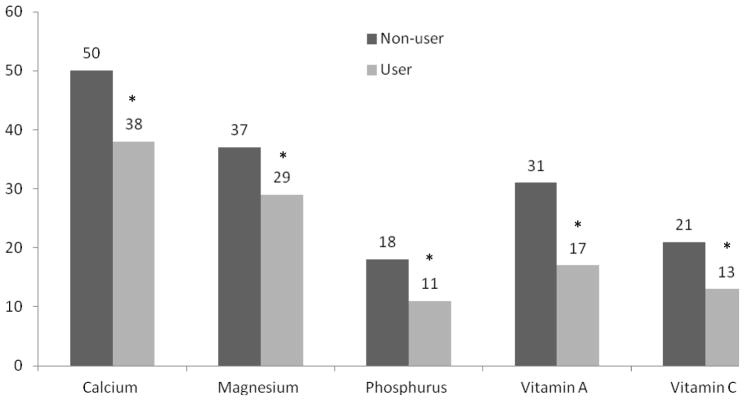
Comparison of Micronutrients from Food Sources Only
No significant differences existed between users and nonusers of dietary supplements in mean micronutrient intakes from food sources only (Tables I and II; available at www.jpeds.com). However, children who were nonusers had a significantly higher prevalence of inadequate intakes (i.e. % < EAR) from food sources only than supplement users for calcium, magnesium, phosphorus, vitamin A and vitamin C (Figure 2; available at www.jpeds.com); but, the prevalence did not differ for the other vitamins and mineral examined.
Table 1.
Usual daily mean (SE) mineral intakes from food sources only by dietary supplement use, gender, and age group in U.S. children and adolescents, 2003–20061,2
| 2–8 y old | 9–13 y old | 14–18 y old | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Non-users
|
Users-Foods
|
Non-users
|
Users-Foods
|
Non-users
|
Users-Foods
|
|
| Males | n=1264 | n=1009 | n=1351 | |||
| Calcium (mg) | 1104 (22) | 1118 (43) | 1081 (31) | 1128 (71) | 1151 (32) | 1335 (83) |
| Iron (mg) | 14.7 (0.3) | 14.4 (0.7) | 17.3 (0.4) | 17.4 (1.2) | 19.1 (0.5) | 24.5 (2.7) |
| Magnesium (mg) | 237 (4) | 228 (7) | 250 (6) | 254 (11) | 285 (9) | 316 (16) |
| Zinc (mg) | 11.3 (0.2) | 10.9 (0.4) | 12.7 (0.3) | 13.8 (0.5) | 14.9 (0.4) | 15.6 (0.7) |
| Phosphorus (mg) | 1277 (19) | 1271 (46) | 1418 (25) | 1361 (67) | 1562 (40) | 1799 (124) |
| Copper (mg) | 1.1 (0.02) | 1.0 (0.03) | 1.2 (0.03) | 1.2 (0.1) | 1.3 (0.03) | 1.6 (0.1) |
| Selenium (μg) | 88 (1) | 78 (7) | 108 (3) | 106 (12) | 127 (3) | 143 (110 |
| Females | n=1337 | n=1039 | n=1250 | |||
| Calcium (mg) | 942 (21) | 1041 (37) | 911 (29) | 1068 (75) | 794 (19) | 972 (58) |
| Iron (mg) | 13.3 (0.3) | 12.8 (0.7) | 13.9 (0.3) | 15.1 (1.5) | 13.5 (0.3) | 13.8 (0.7) |
| Magnesium (mg) | 207 (4) | 219 (6) | 214 (5) | 250 (15) | 203 (5) | 240 (5)* |
| Zinc (mg) | 9.6 (0.2) | 9.8 (0.3) | 10.5 (0.2) | 11.0 (1.0) | 9.9 (0.2) | 10.0 (0.5) |
| Phosphorus (mg) | 1127 (22) | 1198 (54) | 1166 (29) | 1344 (74) | 1101 (25) | 1122 (59) |
| Copper (mg) | 0.9 (0.02) | 1.0 (0.03) | 1.0 (0.02) | 1.2 (0.04) | 1.0 (0.02) | 1.0 (0.2) |
| Selenium (μg) | 81 (1) | 95 (6) | 90 (2) | 101 (25) | 88 (2) | 91 (5) |
Mineral intakes for non-users and users of dietary supplements are from food sources only. Minerals contributed from dietary supplements are not included in the estimates.
Values presented as mean (SE). Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
Table 2.
Usual daily mean (SE) vitamin intakes from food sources only by dietary supplement use, gender, and age group in U.S. children and adolescents, 2003–20061,2
| 2–8 y old | 9–13 y old | 14–18 y old | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Non-users
|
Users-Foods
|
Non-users
|
Users-Foods
|
Non-users
|
Users-Foods
|
|
| Male | n=1264 | n=1009 | n=1351 | |||
| Folate (DFE) | 535 (12) | 548 (20) | 592 (19) | 657 (43) | 641 (20) | 757 (35) |
| Vitamin B6 (mg) | 1.8 (0.1) | 1.7 (0.1) | 1.9 (0.05) | 2.0 (0.1) | 2.2 (0.1) | 2.3 (0.2) |
| Vitamin B12 (μg) | 6.0 (0.2) | 5.5 (0.3) | 6.1 (0.2) | 6.2 (0.3) | 7.1 (0.3) | 7.2 (0.6) |
| Vitamin A (RAE) | 664 (17) | 642 (30) | 678 (26) | 714 (38) | 628 (23) | 704 (53) |
| Vitamin C (mg) | 103 (5) | 100 (5) | 80 (4) | 87 (7) | 88 (6) | 95 (9) |
| Vitamin D (μg) | 7.8 (0.2) | 7.6 (0.5) | 6.3 (0.2) | 6.8 (0.6) | 6.0 (0.2) | 6.5 (0.6) |
| Vitamin E (ATE) | 5.6 (0.1) | 5.1 (0.2) | 6.6 (0.2) | 6.5 (0.4) | 7.3 (0.3) | 7.2 (0.4) |
| Vitamin K (μg) | 48.6 (1.6) | 49.2 (5.4) | 57.9 (2.1) | 51.3 (6.4) | 64.5 (2.8) | 75 (8) |
| Female | n=1337 | n=1039 | n=1250 | |||
| Folate (DFE) | 506 (14) | 476 (13) | 510 (15) | 582 (43) | 478 (13) | 512 (38) |
| Vitamin B6 (mg) | 1.6 (0.1) | 1.5 (0.1) | 1.6 (0.1) | 1.7 (0.1) | 1.5 (0.04) | 1.5 (0.1) |
| Vitamin B12 (μg) | 5.2 (0.1) | 4.8 (0.2) | 4.9 (0.2) | 4.9 (0.6) | 4.2 (0.1) | 4.5 (0.3) |
| Vitamin A (RAE) | 574 (16) | 584 (23) | 531 (23) | 669 (58) | 460 (15) | 559 (59) |
| Vitamin C (mg) | 90 (3) | 81 (4) | 74 (4) | 85 (9) | 68 (3) | 69 (7) |
| Vitamin D (μg) | 6.5 (0.3) | 6.7 (0.4) | 5.2 (0.3) | 6.0 (0.9) | 3.7 (0.2) | 5.0 (0.5) |
| Vitamin E (ATE) | 5.1 (0.1) | 5.0 (0.2) | 5.6 (0.2) | 6.8 (0.5) | 5.6 (0.2) | 5.6 (0.3) |
| Vitamin K (μg) | 49.8 (2) | 56 (6) | 58.3 (1.8) | 69 (24) | 59.4 (2.1) | 55 (5) |
DFE = Dietary Folate Equivalent; RAE = Retinol Activity Equivalent; ATE = Alpha Tocopherol Equivalent
Vitamin intakes for non-users and users of dietary supplements are from food sources only. Vitamins contributed from dietary supplements are not included in the estimates.
Values presented as mean (SE). No significant difference existed between users and non-users of dietary supplements.
Figure 2.
Prevalence of U.S. children (ages 2–18 y) with inadequate micronutrient intakes from food sources only by dietary supplement use in the U.S., 2003–2006
1Values presented as percentage. Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
Contribution of Supplements to Micronutrient Intakes
Among 2 – 8 y olds, dietary supplement users had significantly higher mean total intakes (foods and supplements combined) of all minerals examined with the exception of calcium and selenium in males and phosphorus in both males and females (Table III). Among males 9 – 13 y, users had significantly higher intakes of calcium, iron, zinc and copper. Females age 9 – 13 y who used supplements had significantly higher intakes of all minerals than non-users with the exception of selenium. Both male and female supplement users ages 14 – 18 y, had higher mean mineral intakes for all minerals examined. Similarly, across all age and sex groups supplement users had significantly higher mean vitamin intakes than non-users for all vitamins examined except for vitamin K. (Table IV).
Table 3.
Usual daily mean (SE) mineral intakes by dietary supplement use, gender, and age group in U.S. children and adolescents, 2003–20061,2
| 2–8 y old
|
9–13 y old
|
14–18 y old
|
||||
|---|---|---|---|---|---|---|
| Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
|
| Males | n=1264 | n=1009 | n=1351 | |||
| Calcium (mg) | 1104 (22) | 1213 (36) | 1081 (31) | 1243 (36)* | 1151 (32) | 1490 (97)* |
| Iron (mg) | 14.7 (0.3) | 27.6 (1.6)* | 17.3 (0.4) | 30.8 (2.4)* | 19.1 (0.5) | 31.5 (1.3)* |
| Magnesium (mg) | 237 (4) | 246 (9)* | 260 (6) | 283 (14) | 281 (7) | 377 (21)* |
| Zinc (mg) | 11.3 (0.2) | 19.1 (1.1)* | 12.7 (0.3) | 21.9 (1.3)* | 14.9 (0.4) | 26.1 (1.3)* |
| Phosphorus (mg) | 1277 (19) | 1334 (42) | 1418 (25) | 1427 (67) | 1562 (40) | 1875 (144)* |
| Copper (mg) | 1.1 (0.02) | 2.5 (0.2)* | 1.2 (0.03) | 2.6 (0.2)* | 1.3 (0.03) | 2.9 (0.2)* |
| Selenium (μg) | 88 (1) | 107 (7) | 108 (3) | 118 (10) | 127 (3) | 180 (11)* |
| Females | n=1337 | n=1039 | n=1250 | |||
| Calcium (mg) | 942 (21) | 1119 (36)* | 911 (29) | 1161 (77)* | 794 (19) | 1188 (68)* |
| Iron (mg) | 13.3 (0.3) | 25.7 (1.9)* | 13.9 (0.3) | 25.7 (1.7)* | 13.5 (0.3) | 28.5 (2.3)* |
| Magnesium (mg) | 207 (4) | 233 (7)* | 217 (4) | 274 (17)* | 204 (4) | 286 (13)* |
| Zinc (mg) | 9.6 (0.2) | 17.3 (1.0)* | 10.5 (0.2) | 18.7 (1.7)* | 9.9 (0.2) | 19.2 (0.8)* |
| Phosphorus (mg) | 1127 (22) | 1250 (57) | 1166 (29) | 1413 (69)* | 1101 (25) | 1170 (57) |
| Copper (mg) | 0.9 (0.02) | 2.4 (0.2)* | 1.0 (0.02) | 2.3 (0.1)* | 1.0 (0.02) | 2.3 (0.1)* |
| Selenium (μg) | 81 (1) | 107 (8)* | 90 (2) | 114 (27) | 88 (2) | 115 (6)* |
Mineral intakes for non-users of dietary supplements are from food sources only. Mineral intakes for users of supplements represent the total intake from food sources and from dietary supplements.
Values presented as mean (SE). Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
Table 4.
Usual daily mean (SE) vitamin intakes by dietary supplement use, gender, and age group in U.S. children and adolescents, 2003–20061,2
| 2–8 y old
|
9–13 y old
|
14–18 y old
|
||||
|---|---|---|---|---|---|---|
| Non-users
|
Users-Total
|
Non-users
|
Users-Total
|
Non-users
|
Users-Total
|
|
| Male | n=1264 | n=1009 | n=1351 | |||
| Folate (DFE) | 535 (12) | 1049 (52)* | 592 (19) | 1428 (273)* | 641 (20) | 1250 (64)* |
| Vitamin B6 (mg) | 1.8 (0.1) | 3.1 (0.2)* | 1.9 (0.05) | 4.5 (0.9)* | 2.2 (0.1) | 8.8 (2.6)* |
| Vitamin B12 (μg) | 6.0 (0.2) | 11.6 (1.3)* | 6.1 (0.2) | 14.2 (2.4)* | 7.1 (0.3) | 18.3 (3.1)* |
| Vitamin A (RAE) | 664 (17) | 1525 (102)* | 678 (26) | 2201 (603)* | 628 (23) | 1558 (127)* |
| Vitamin C (mg) | 103 (5) | 186 (12)* | 80 (4) | 201 (24)* | 88 (6) | 257 (24)* |
| Vitamin D (μg) | 7.8 (0.2) | 15.6 (0.9)* | 6.3 (0.2) | 17.8 (3.7)* | 6.0 (0.2) | 13.1 (2.2)* |
| Vitamin E (ATE) | 5.6 (0.1) | 20.1 (2.0)* | 6.6 (0.2) | 28.3 (8.5)* | 7.3 (0.3) | 35.8 (6.3)* |
| Vitamin K (μg) | 48.6 (1.6) | 63.5 (7.2) | 57.9 (2.1) | 66.1 (6.0) | 64.5 (2.8) | 92.7 (7.9)* |
| Female | n=1337 | n=1039 | n=1250 | |||
| Folate (DFE) | 506 (14) | 1038 (115)* | 510 (15) | 1068 (92)* | 478 (13) | 953 (39)* |
| Vitamin B6 (mg) | 1.6 (0.1) | 2.9 (0.3)* | 1.6 (0.1) | 3.2 (0.3)* | 1.5 (0.04) | 4.8 (0.8)* |
| Vitamin B12 (μg) | 5.2 (0.1) | 12.0 (2.2)* | 4.9 (0.2) | 10.0 (1.3)* | 4.2 (0.1) | 13.4 (2.0)* |
| Vitamin A (RAE) | 574 (16) | 1536 (171)* | 531 (23) | 1548 (148)* | 460 (15) | 1427 (135)* |
| Vitamin C (mg) | 90 (3) | 169 (16)* | 74 (4) | 199 (24)* | 68 (3) | 245 (22)* |
| Vitamin D (μg) | 6.5 (0.3) | 15.8 (2.2)* | 5.2 (0.3) | 13.8 (1.7)* | 3.7 (0.2) | 11.4 (0.6)* |
| Vitamin E (ATE) | 5.1 (0.1) | 19.1 (2.4)* | 5.6 (0.2) | 21.4 (2.6)* | 5.6 (0.2) | 47.6 (17.8)* |
| Vitamin K (μg) | 49.8 (1.9) | 66.8 (7.7) | 58.3 (1.8) | 85.6 (25.1) | 59.4 (2.1) | 75.6 (7.6) |
DFE = Dietary Folate Equivalent; RAE = Retinol Activity Equivalent; ATE = Alpha Tocopherol Equivalent
Vitamin intakes for non-users of dietary supplements are from food sources only. Vitamin intakes for users of supplements represent the total intake from food sources and from dietary supplements.
Values presented as mean (SE). Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
Micronutrient supplement use lowered the prevalence of inadequate intakes for many vitamins and minerals among children and adolescents in the U.S. (Figure 3). Compared with users, non-users had a significantly higher prevalence of inadequacy in their usual intakes of calcium, and vitamins A, C, D, and E across all age groups (Table V; available at www.jpeds.com). The prevalence of inadequate dietary intakes of phosphorus, copper, selenium, zinc, folate, or vitamin B-6 and B-12 among 2 – 8 y olds in the U.S. was negligible, regardless of supplement use. Among 9 – 13 y olds, the prevalence of inadequate phosphorus, copper, selenium or vitamin B-12 intake did not differ between users and nonusers, but it did for the other micronutrients examined. Among those aged 14 – 18 y, supplement users had a significantly lower prevalence of inadequate intake of all of the micronutrients examined, with the sole exceptions of iron and phosphorous.
Figure 3.
Prevalence (%) of U.S. children (ages 2–18 y) with inadequate micronutrient intakes in the U.S. by dietary supplement use in the U.S., 2003–20061
1Values presented as percentages. Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
Table 5.
The prevalence of inadequate mineral and vitamin intakes by dietary supplement use and age group in U.S. children and adolescents, 2003–20061,2
| 2–8 y old n=2,601 |
9–13 y old n=2,048 |
14–18 y old n=2,601 |
||||
|---|---|---|---|---|---|---|
| Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
|
| Calcium (mg) | 23 (1) | 13 (2)* | 66 (2) | 46 (5)* | 67 (2) | 36 (5)* |
| Iron (mg) | 0.6 (0.1) | 0 | 0.4 (0.1) | 0* | 5.6 (0.5) | < 1 |
| Magnesium (mg) | 2 (0.3) | < 1 | 33 (2) | 18 (3)* | 84 (2) | 52 (5)* |
| Zinc (mg) | 0.2 (0.1) | 0 | 7.3 (1.0) | < 1* | 12.7 (1.4) | 1.7 (0.6)* |
| Phosphorus (mg) | < 1 | 0 | 29 (2) | 16 (4) | 29 (2) | 19 (4) |
| Copper (mg) | 0 | 0 | 1.6 (0.3) | <1 | 8.5 (0.8) | 2.1 (1.0)* |
| Selenium (μg) | 0 | 0 | < 1 | 0 | 1.1 (0.3) | 1.0 (0.7) |
| Folate (DFE) | < 1 | 0 | 2.4 (0.6) | <1* | 10.9 (1.3) | 1.1 (0.5)* |
| Vitamin B6 (mg) | < 1 | 0 | 2.6 (0.6) | <1* | 10 (1) | < 1* |
| Vitamin B12 (μg) | 0 | 0 | < 1 | 0 | 3.1 (0.6) | <1* |
| Vitamin A (RAE) | 5 (0.7) | < 1* | 30 (2) | 1.5 (0.7)* | 59 (2) | 5.9 (1.2)* |
| Vitamin C (mg) | 2 (0.4) | < 1* | 20 (1.7) | 1.7 (0.8)* | 42 (3) | 7.3 (1.2)* |
| Vitamin D (μg) | 81 (2) | 27 (3)* | 89 (1) | 32 (6)* | 93 (1) | 36 (4)* |
| Vitamin E (ATE) | 64 (2) | 3.7 (0.6)* | 89 (1) | 12 (4)* | 97 (1) | 21 (2)* |
Nutrient intakes for non-users of dietary supplements are from food sources only. Nutrient intakes for users of supplements represent the total intake from food sources and from dietary supplements.
Values presented as percentage (SE). Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
Dietary supplement use was associated with an increased prevalence of usual intakes above the UL for several micronutrients: iron, zinc, folic acid, and vitamins A and C (and copper and selenium among 2 – 8 y olds) (Figure 4; Table VI; available at www.jpeds.com). For other micronutrients, users of dietary supplements had the same or only a negligibly higher prevalence of intakes above the UL when compared with non-users for calcium, magnesium, phosphorus, vitamins B-6, D, and E. There is no UL established for vitamin B-12 in children and so this nutrient could not be evaluated. Among those age 2 – 8 y old, more than 70% of supplement users exceeded the UL for zinc (84%), folate (71%), and vitamin A (72%). Among 9 – 13 y olds, the highest prevalence of intakes exceeding the UL was for folate (35%) and zinc (32%) the UL whereas among those aged 14–18 it was iron (~9%), zinc (8%) and folate (13%).
Figure 4.
Prevalence of U.S. children (ages 2–18y) with micronutrient intakes exceeding the Upper Tolerable Intake Level by dietary supplement use in the U.S., 2003–20061
1Values presented as percentage. Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
Table 6.
The prevalence of mineral and vitamin intakes exceeding the Tolerable Upper Intake Level by dietary supplement use, gender, and age group in U.S. children and adolescents, 2003–20061,2,3
| 2–8 y old n=2,601 |
9–13 y old n=2,048 |
14–18 y old n=2,601 |
||||
|---|---|---|---|---|---|---|
| Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
|
| Calcium (mg) | <1 | <1 | <1 | <1 | <1 | <1 |
| Iron (mg) | 0 | 4.5 (1.0)* | 0 | 5.4 (2.4)* | 0 | 8.5 (2.6)* |
| Magnesium (mg) | 0.2 (0.1) | <1 | 0 | <1 | 0 | 1.0 (0.7) |
| Zinc (mg) | 45 (2) | 84 (2)* | <1 | 32(5)* | <1 | 8 (2)* |
| Phosphorus (mg) | 0 | <1 | 0 | 0 | 0 | 0 |
| Copper (mg) | 7.7 (0.8) | 39 (4)* | 0 | <1 | 0 | 0 |
| Selenium (μg) | 7.5 (0.6) | 20 (6)* | <1 | 0 | 0 | <1 |
| Folic Acid (μg) | 8.7 (1.2) | 71 (3)* | <1 | 35 (6)* | <1 | 13 (2) |
| Vitamin B6 (mg) | 0 | <1 | 0 | <1 | 0 | 1.5 (1.0) |
| Vitamin A (μg Retinol) | 13(1) | 72 (3)* | <1 | 21(3)* | 0 | 1.5 (0.6) |
| Vitamin C (mg) | <1 | 2.5 (0.4)* | 0 | 1.0 (0.8) | 0 | <1 |
| Vitamin D (μg) | 0 | <1 | 0 | 1.8 (1.1) | 0 | 0 |
| Vitamin E (ATE) | 0 | <1 | 0 | 0 | 0 | <1 |
DFE = Dietary Folate Equivalent; RAE = Retinol Activity Equivalent; ATE = Alpha Tocopherol Equivalent
Nutrient intakes for non-users of dietary supplements are from food sources only. Nutrient intakes for users of supplements represent the total intake from food sources and from dietary supplements.
Values presented as percentage (SE). Significant differences are denoted by an asterisk at a Bonferroni-corrected P value ≤ 0.003.
The UL for magnesium is for added magnesium to foods or from dietary supplements. The UL for Folate is in μg of folic acid, not including folate that naturally occurs in food. The UL for vitamin A is from retinol only, not from carotenoids with provitamin A activity.
Discussion
Adequate nutrient intake through food choices should always be recommended by nutrition and health professionals. Dietary supplement use may be appropriate and is recommended during certain life stages; for example, vitamin D for breast-fed infants and folic acid for reproductive-aged females. However, the use of dietary supplements is widespread in both adults and children in the US. The question of interest in this analysis was whether supplements were being given to children to help meet nutrient recommendations, and it appears that they were, at least for some nutrients. Micronutrient supplement use lowered the prevalence of inadequate intakes of calcium, iron, magnesium, and vitamins A, C, D and E. However, supplement use had little effect on the prevalence of inadequate intakes of phosphorus, copper, selenium, folate, and vitamin B-6 and B-12 among younger children (2 – 8 y) because there were no inadequacies of these micronutrients to begin with in that age group. In 9 – 18 y olds, the use of dietary supplements lowered the prevalence of inadequate intakes more substantially than it did in the 2–8 yr old for almost all vitamins and minerals. However, the prevalence of use of supplements among 14–18 yr olds was quite low, and so their impact on adequacy of intakes as a whole was lessened. The use of dietary supplements did not substantially alter intakes of phosphorus, selenium and vitamin K because these tend to be in very low doses in children’s supplements.
The majority of children aged 2 – 8 y who did not use supplements failed to meet recommendations for calcium, and vitamins D and E and more than ~30% failed to meet the EAR for magnesium and vitamin A. However, even among supplement users, more than a third of the children aged 2 – 18 y failed to meet calcium and vitamin D recommendations (Figure 3), suggesting that consideration should be given to reformulating supplements for these nutrients. In those ages 14 – 18 y several other nutrients of public health concern were also identified from this analysis: magnesium, phosphorus, and vitamins A, C, and E. Calcium and vitamin D are critical for healthy bone and teeth formation(26), and vitamin E is important for immune function and acts as an antioxidant (22). Vitamin A is important for vision, bone growth and cell division and differentiation (22). Magnesium is needed for over 300 biochemical reactions in the body and is involved in energy production, protein synthesis, and muscle contraction(23). About half of those who used magnesium-containing dietary supplements in their teenage years did not achieve the EAR.
Conversely, supplement use did increase the prevalence of intakes above the UL for iron, zinc, vitamin A and folic acid in all age groups and for vitamin C, copper, and selenium in those 2 – 8 y. Little is known about the long-terms effects of high doses of these micronutrients in children. The DRIs for children are generally set as extrapolations from studies conducted with adults. These data should be interpreted with this caveat in mind, particularly in the youngest of children for whom the least data is available to set recommendations. More than 7% of children (2 – 8 y) usually have nutrient intakes from foods alone that exceed the UL for copper, selenium, folic acid, vitamin A and zinc, with zinc being the most notable (45% of non-users and 84% of users reporting usual intakes > UL).
The strengths of this investigation are that it utilizes nationally-representative survey data and that we have employed statistical models to estimate long-term, habitual micronutrient intakes (19). We extend previous by examining users and non-users as 2 distinct groups. When supplement users and non-users are combined in to one group for analysis, the impact that supplements make are diluted. The prevalence of inadequate intakes (i.e. % < EAR) is under-estimated for non-users, whereas the prevalence of excessive intakes (i.e. % > UL) is under-estimated for users. However, it should be noted that the statistical models that we applied to make these estimates reflective of habitual, usual intakes rely upon the assumptions that reported nutrient intakes from food sources on the 24-hour recalls are unbiased and the self-reported dietary supplement intake reflects true long-term supplement intake. The estimates of nutrients contributed by dietary supplements depend on the label declarations rather than analytical values; work is underway by the NIH Office of Dietary Supplements and the USDA Nutrient Data Laboratory to examine the analytical content of children’s dietary supplement in comparison with labeled levels (27).
Few studies are available for comparison. Previous work indicates the users of dietary supplements are more likely than non-users to have higher intakes of energy, iron and vitamin C (10) and were also more likely to make healthy food choices (28) and physical activity practices (29). Taken together with this study, these data support the contention that the basic diets of children who use dietary supplements are different than children who do not use supplements for most of the micronutrients. Children who are users of supplements consistently had a significantly lower prevalence of nutrient inadequacy when compared with children who do not use supplements. However, usual intakes of calcium, vitamin A, vitamin D and magnesium remain low in children despite use of these supplements (i.e. > 20% have total intakes <EAR), suggesting that additional strategies, possibly including reformulation of the levels of some of these nutrients in supplements may be in order. Those age 14 – 18 y are of particular concern because they have the highest prevalence of nutrient inadequacy and low prevalence of dietary supplement use.
Dietary supplement use in children remains a controversial strategy to improve nutrient intakes because, even though their use is associated with lower prevalence of inadequate intakes, it is also associated with an increased risk of excessive intakes (i.e. above the UL). For this reason, Murphy et al have previously suggested that dietary supplement manufacturers better tailor the levels of micronutrients in supplements to help achieve a balance between nutrient adequacy and excess (30).
Acknowledgments
Supported in part by the US Department of Agriculture Research Service (agreement 58-1950-7-707) and the Office of Dietary Supplements at the National Institutes of Health. Data generation was funded by the Fortification Committee of the International Life Sciences Institute, North American Branch.
Abbreviations
- AI
Adequate Intake
- ATE
alpha-tocopherol equivalent
- EAR
Estimated Average Requirement
- DFE
Dietary Folate Equivalent
- DRI
Dietary Reference Intake
- IU
International Unit
- NCI
National Cancer Institute
- NHANES
National Health and Nutrition Examination Survey
- NHW
Non-Hispanic White
- NHB
Non-Hispanic Black
- MA
Mexican American
- RAE
retinol activity equivalent
- UL
Tolerable Upper Intake Level
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
References
- 1.Bailey RL, Gahche JJ, Lentino CV, Dwyer JT, Engel JS, Thomas PR, et al. Dietary supplement use in the United States, 2003–2006. J Nutr. 2011;141:261–6. doi: 10.3945/jn.110.133025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol. 2004;160:339–49. doi: 10.1093/aje/kwh207. [DOI] [PubMed] [Google Scholar]
- 3.Gahche J, Bailey R, Burt V, Hughes J, Yetley E, Dwyer J, et al. Dietary Supplement Use Among U.S. Adults Has Increased Since NHANES III (1988–1994) NCHS Data Brief. 2011:61. [PubMed] [Google Scholar]
- 4.Rock CL. Multivitamin-multimineral supplements: who uses them? Am J Clin Nutr. 2007;85:277S–9S. doi: 10.1093/ajcn/85.1.277S. [DOI] [PubMed] [Google Scholar]
- 5.Foote JA, Murphy SP, Wilkens LR, Hankin JH, Henderson BE, Kolonel LN. Factors associated with dietary supplement use among healthy adults of five ethnicities: the Multiethnic Cohort Study. Am J Epidemiol. 2003;157:888–97. doi: 10.1093/aje/kwg072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrison RA, Holt D, Pattison DJ, Elton PJ. Are those in need taking dietary supplements? A survey of 21 923 adults. Br J Nutr. 2004;91:617–23. doi: 10.1079/BJN20031076. [DOI] [PubMed] [Google Scholar]
- 7.Block G, Jensen CD, Norkus EP, Dalvi TB, Wong LG, McManus JF, et al. Usage patterns, health, and nutritional status of long-term multiple dietary supplement users: a cross-sectional study. Nutr J. 2007;6:30. doi: 10.1186/1475-2891-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sebastian RS, Cleveland LE, Goldman JD, Moshfegh AJ. Older adults who use vitamin/mineral supplements differ from nonusers in nutrient intake adequacy and dietary attitudes. J Am Diet Assoc. 2007;107:1322–32. doi: 10.1016/j.jada.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 9.Bailey RL, Fulgoni VL, Keast DR, Dwyer JT. Dietary supplement use is associated with higher intakes of minerals from food sources. Am J Clin Nutr. 2011;94:1376–81. doi: 10.3945/ajcn.111.020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Looker AC, Sempos CT, Johnson CL, Yetley EA. Comparison of dietary intakes and iron status of vitamin-mineral supplement users and nonusers, aged 1–19 years. Am J Clin Nutr. 1987;46:665–72. doi: 10.1093/ajcn/46.4.665. [DOI] [PubMed] [Google Scholar]
- 11.Dwyer J, Nahin R, Rodgers G, Barnes P, Jacques P, Bailey R, et al. Prevalence and Predictors of Children’s Dietary Supplement Use: The 2007 National Health Interview Survey. doi: 10.3945/ajcn.112.052373. Under Peer-review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Picciano MF, Dwyer JT, Radimer KL, Wilson DH, Fisher KD, Thomas PR, et al. Dietary supplement use among infants, children, and adolescents in the United States, 1999–2002. Arch Pediatr Adolesc Med. 2007;161:978–85. doi: 10.1001/archpedi.161.10.978. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control NCfHS. http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf The National Health and Nutrition Examination Survey (NHANES) Analytic and Reporting Guidelines.
- 14.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136:2594–9. doi: 10.1093/jn/136.10.2594. [DOI] [PubMed] [Google Scholar]
- 15.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88:324–32. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics. SP Questionnaire Component: Dietary Supplements Questionnaire Data. 2003–2004. National Health and Nutrition Examination Survey. [Google Scholar]
- 17.Bailey RL, Dodd KW, Gahche JJ, Dwyer JT, McDowell MA, Yetley EA, et al. Total folate and folic acid intake from foods and dietary supplements in the United States: 2003–2006. Am J Clin Nutr. 91:231–7. doi: 10.3945/ajcn.2009.28427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bailey RL, Dodd KW, Goldman JA, Gahche JJ, Dwyer JT, Moshfegh AJ, et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr. 140:817–22. doi: 10.3945/jn.109.118539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Food and Nutrition Board. Dietary reference intakes applications in dietary assessment. Washington, DC: National Academy Press; 2000. [Google Scholar]
- 20.Food and Nutrition Board. Dietary reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. Washington, DC: National Academy Press; 1998. [PubMed] [Google Scholar]
- 21.Food and Nutrition Board. Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, molybdenum, nickel, silicon, vanadium and zinc. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 22.Food and Nutrition Board. Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 23.Food and Nutrition Board. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D and floride. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 24.Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, et al. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106:1575–87. doi: 10.1016/j.jada.2006.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Cancer Institute. Usual Dietary Intakes: The NCI Method. Bethesda, MD: 2009. [Google Scholar]
- 26.Food and Nutrition Board. Dietary reference intakes for calcium and vitamin D. Washington, DC: National Academy Press; 2010. [Google Scholar]
- 27.Dwyer JT, Holden J, Andrews K, Roseland J, Zhao C, Schweitzer A, et al. Measuring vitamins and minerals in dietary supplements for nutrition studies in the USA. Anal Bioanal Chem. 2007;389:37–46. doi: 10.1007/s00216-007-1456-z. [DOI] [PubMed] [Google Scholar]
- 28.Dwyer JT, Garcea AO, Evans M, Li D, Lytle L, Hoelscher D, et al. Do adolescent vitamin-mineral supplement users have better nutrient intakes than nonusers? Observations from the CATCH tracking study. J Am Diet Assoc. 2001;101:1340–6. doi: 10.1016/s0002-8223(01)00321-2. [DOI] [PubMed] [Google Scholar]
- 29.George GC, Springer AE, Forman MR, Hoelscher DM. Associations among dietary supplement use and dietary and activity behaviors by sex and race/ethnicity in a representative multiethnic sample of 11th-grade students in Texas. J Am Diet Assoc. 111:385–93. doi: 10.1016/j.jada.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 30.Murphy SP, White KK, Park SY, Sharma S. Multivitamin-multimineral supplements’ effect on total nutrient intake. Am J Clin Nutr. 2007;85:280S–4S. doi: 10.1093/ajcn/85.1.280S. [DOI] [PubMed] [Google Scholar]