Abstract
Aims
This study tests risk factors for four dimensions of alcohol use in the sequence from (a) early onset prior to age 13 to (b) adolescent alcohol use and (c) alcohol problems to (d) young adult alcohol abuse. It also examines whether family-focused preventive interventions buffer predictive relationships.
Design
Data were from a randomized prevention trial extending from ages 11 to 21.
Setting
Families of sixth graders enrolled in 33 rural schools in the Midwestern United States were invited to participate.
Participants
Families (N = 667) were pretested and randomly assigned to a control group (n = 208) or to family interventions (n = 459). The average age of participating youth was 11.3 years when the study began (52% female). Measurements: Questionnaire data were collected on alcohol dimensions during adolescence (early onset, alcohol use, alcohol problems) and young adulthood (alcohol abuse), and on risk factors in early adolescence (male gender, impulsive behaviors, aggression-hostility, peer deviance, and parent problem drinking).
Findings
Impulsive behaviors predicted early onset, peer deviance predicted alcohol use, and parent problem drinking predicted alcohol problems (p < .05). Aggression-hostility and alcohol problems predicted alcohol abuse in the control group (p < .05), but not in the family interventions group (p > .05).
Conclusions
Different dimensions of alcohol use and problems from before age 13 to young adulthood are predicted by different risk factors. Family-focused preventive interventions can reduce the influence of some of these risk factors, including early adolescent aggression-hostility and late adolescent alcohol problems.
Keywords: alcohol use, alcohol abuse, prevention, family, risk factors, youth
Introduction
Alcohol is the most commonly used substance among youth in many developed countries (1), including the United States (2). Of concern, alcohol can disrupt normative brain development among teenagers (2), and is associated with a range of cognitive, behavioral, emotional, and physical difficulties (3). Consequently, the global public health burden and economic costs of alcohol involvement are high (4).
Alcohol involvement is multidimensional (5;6), manifest in different behaviors that unfold in a developmental progression over time. Early onset occurs before age 13 (7). Alcohol use and alcohol problems increase steadily throughout adolescence (2), and the past year prevalence of alcohol abuse peaks in young adulthood (8). Although early alcohol onset has been shown to increase risk for alcohol disorders (9), there is a lack of research examining simultaneously multiple dimensions of alcohol involvement in the sequence from early onset to alcohol abuse. Thus, important questions remain unanswered.
It is unclear whether prominent risk factors are common or specific predictors of different alcohol dimensions. Among risk factors, male gender (10), impulsivity (11), aggression and related externalizing problems (12), peer deviance (13), and parent problem drinking (14) are potent predictors of various adolescent and young adult alcohol-related outcomes (15;16). Research examining differential predictors typically has considered simultaneously only two dimensions of alcohol involvement, usually alcohol use and alcohol problems (17–20). For example, Stice, Barrera, & Chassin (21) tested the hypothesis that socialization factors (e.g., peer influences) predict alcohol use, whereas psychopathology factors (e.g., externalizing symptoms) predict alcohol problems. Results partially supported the hypothesis by showing that externalizing symptoms and other psychopathology factors were directly related to alcohol problems in multivariate analyses; however, peer influences also were directly related to problem drinking (22). Research is needed that examines more than two alcohol dimensions at a time to more fully capture the multidimensional and developmental nature of alcohol involvement. Such research could contribute further to an understanding of the unique etiology of specific alcohol behaviors and inform prevention.
Family-focused substance misuse preventive interventions can delay alcohol onset (23;24), decrease adolescent alcohol use (25;26), and prevent young adult alcohol misuse and abuse (27;28). The extent to which effective family-focused preventive interventions moderate or alter the strength of relationships among the multiple dimensions of alcohol involvement remains unexamined. Such interventions might buffer links in the progression from early onset to alcohol abuse, making it less likely that youth will advance to problematic drinking. Moreover, family-focused preventive interventions, with their inclusion of components such as communication and coping skills and parent training, might attenuate the influences of risk factors on specific alcohol behaviors.
Using data from a longitudinal prevention trial that has followed a sample of rural youth over ages 11 to 21 years (28), this study has two aims. The first aim is to examine the sequence of alcohol involvement from early alcohol onset to adolescent alcohol use and alcohol problems to young adult alcohol abuse, and test differential predictors (gender, impulsive behaviors, aggression-hostility, peer deviance, and parent problem drinking) of these alcohol dimensions. Positive links in the alcohol sequence are hypothesized. Psychopathology factors (e.g., aggression-hostility) are expected to predict alcohol problems and alcohol abuse, whereas socialization factors (e.g., peer and parent influences) are expected to predict early onset and alcohol use, although peer factors might also predict problem drinking (21;22). Because problem drinking is more common among males than females (8), male gender is expected to predict alcohol problems and alcohol abuse. The second aim is to examine the extent to which effective family-focused substance misuse preventive interventions moderate both the developmental progression of alcohol dimensions and the influences of prominent risk factors. It is hypothesized that associations in the alcohol sequence will be buffered by family-focused preventive interventions, and that such interventions will attenuate risk factor influences.
Method
Participants
Participants were families of 6th graders enrolled in 33 rural schools in 19 counties of a Midwestern state in the United States. Schools in communities with a population of less than 8,500 and in districts with at least 15% of families eligible for free or reduced cost lunches were selected. After blocking on school size and proportion of students residing in low income households, 11 schools each were randomly assigned to one of three conditions: a minimal-contact control condition, a Preparing for the Drug Free Years (PDFY; 29) condition, and an Iowa Strengthening Families Program (ISFP; 30) condition. A CONSORT flow diagram for the randomized trial that generated the data used in the current study is provided elsewhere (28).
Of the 1,309 eligible families, 667 (51%) were enrolled and completed pretesting in fall 1993, including 208 control, 221 PDFY, and 238 ISFP families. Reflecting the region, most participants were Caucasian (98.6%). Families had an average of three children, and 85% were dual-parent. The average age of target children was 11.3 years when the study began; 52% of these children were girls (n = 345). Nineteen percent of mothers and 22% of fathers had graduated from college. The median annual household income in 1993 was $33,400.
Of the 667 pretested families, 551 (83%) completed posttesting in the 6th grade at approximately age 12. Follow-up assessments were conducted with 472, 438, 447, and 457 families when youth were in the 7th (age 13), 8th (age 14), 10th (age 16), and 12th (age 18) grades, respectively, and with 483 target youth at age 21. Prior research (26;31;32) has 1) documented the representativeness of enrolled families; 2) established baseline equivalence of the conditions; 3) ruled out differential attrition across conditions; and 4) found little evidence for selective attrition from the study.
Procedures
Parents provided informed consent for their participation and for that of their adolescent children; youth provided assent during adolescence and consent in early adulthood. Families were mailed a packet that included information about the study and initial questionnaires. Subsequently, home visits, which lasted about 2.5 hours, were conducted with families to obtain additional assessments. Participants were assured of the confidentiality of their responses. Each family member received $10/hour for their participation. Similar procedures were used at the post-test and follow-up assessments during adolescence. Phone interviews were conducted with target participants at age 21. Procedures were approved by the Human Subjects Review committees at Iowa State University and the University of Washington.
Interventions
PDFY and ISFP have been described in detail elsewhere (28). Briefly, PDFY helps parents develop and communicate clear expectations and consequences regarding substance use, and increases involvement, reduces conflict, and promotes bonding in the family. One of the five sessions focuses on peer resistance skills and is attended by parents and adolescents. Sessions are about 2 hours long. In each of the seven ISFP sessions, adolescents and parents participate separately in the first hour and then join together during the second hour. ISFP helps parents improve communication and parenting skills, and reduces family conflict. Adolescents learn problem solving, coping, and peer resistance skills. Control families received four leaflets describing different aspects of adolescent development. Effects of both interventions on alcohol outcomes are summarized above and in prior project reports (24;26–28;31;32).
Measures
Family interventions
Family interventions status was coded 1 for randomization into either the PDFY or ISFP groups and 0 for randomization into the control group, since the purpose was to examine the moderating influence of family interventions, in general, and because prior project analyses have already examined specific program effects. PDFY and ISFP have similar program components, and direct comparisons have revealed very few statistically significant differences in intervention effects across PDFY and ISFP conditions (26).
Alcohol involvement
Early onset of alcohol use prior to age 13 is measured with responses to a questionnaire item at posttest that asked youth to indicate if they had ever drunk beer, wine, or liquor without a parent’s permission (coded 1 for yes and 0 for no). Alcohol use at age 16 is a latent variable with two indicators (α . 64). First, adolescents reported how many times they consumed beer, wine, wine coolers, or other liquor within the past month and also indicated how much they usually drink on a drinking occasion using a scale ranging from 0 “I don’t drink alcohol” to 5 “More than 6 drinks.” Responses to these items were standardized and summed to compute a quantity-frequency index. Second, adolescents reported how many times they had consumed three or more drinks in a row within the past month as a measure of heavy episodic drinking. An alcohol problems latent variable at age 18 is measured with four items (α = .67) that assessed memory problems, getting sick, and getting into fights due to alcohol (on a scale ranging from 0 “Never” to 4 “Four or more times”) and use of alcohol-related services (coded 1 for presence and 0 for absence of service use). Past year alcohol abuse at age 21 is measured using a short form of the Diagnostic Interview Schedule (33), indicating the presence (coded 1) or absence (coded 0) of a disorder according to DSM-IV criteria (34).
Risk factors
Male gender is coded 1 for males and 0 for females. Peer deviance at age 11 is a latent variable represented by two questionnaire items (α = .73) that assessed serious deviance and asked adolescents to report how much they agree that their close friends sometimes get into trouble with the police and sometimes break the law, with response options ranging from 1 “Strongly disagree” to 5 “Strongly agree.” An impulsive behaviors latent variable at age 11 is measured with four indicators (α = .73; e.g., “If someone annoys me, I tell them what I think of them”) on a scale ranging from 1 “Not at all [like me]” to 5 “Exactly [like me].” Separate adolescent-, mother-, and father-report scales calculated as the mean of five items each drawn from the questionnaire portion of the Iowa Youth and Family Ratings Scales (35; e.g., “Hit, push, grab, or shove” and “Criticize”) serve as indicators of an aggression-hostility latent variable at age 11 (α .63); response options for the items ranged from 1 “Never” to 7 “Always.” Seven items from the Iowa Youth and Families Project (36) asked mothers and fathers about their problem drinking in the past 12 months on a scale ranging from 1 “Never” to 4 “Often” (e.g., “How often have you had family problems because of drinking?”). Items were averaged within gender to create both maternal and paternal problem drinking scales, which serve as indicators of a parent problem drinking latent variable at age 11 (α .51).
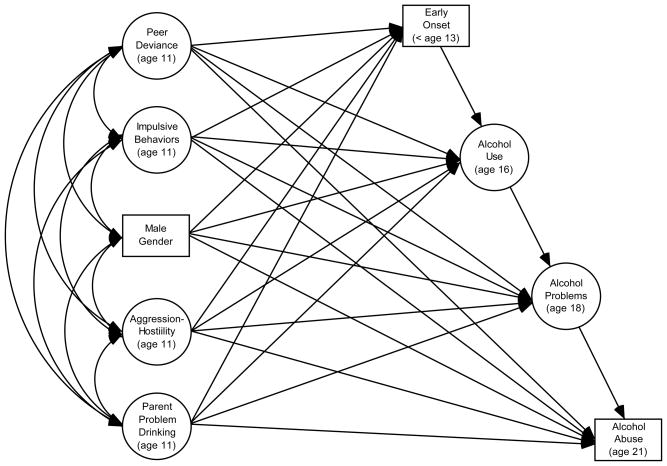
Analyses
The conceptual model depicted in Figure 1 was estimated with multiple group structural equation modeling (SEM) in Mplus 6.1 (37) using the Weighted Least Squares Means- and Variance-Adjusted (WLSMV) estimator, which is appropriate for models with binary and ordered categorical dependent variables (i.e., early onset, alcohol abuse, and alcohol service use) and is generally robust to deviations from normality in the latent response distribution assumed to underlie the observed data (38). Family Interventions was the grouping variable, and school was specified as a clustering variable. In Mplus, the WLSMV estimator incorporates a pair-wise deletion strategy for handling missing data, which resulted in the loss of one case from the sample. Model fit was evaluated using the chi-square statistic, the comparative fit index (CFI), and the root mean square error of approximation (RMSEA).
Figure 1.
Conceptual model of the alcohol sequence and risk factor influences
To begin, the measurement model was evaluated with confirmatory factor analysis (CFA) in the full sample and also in a multiple group context to test for group differences in the factor loadings. Next, tests of structural differences between the family interventions and control groups were conducted with multiple group SEM in three steps. In Step 1, a “structurally unconstrained” model was estimated that allowed all path coefficients to be different across groups.
In Step 2, a series of models was estimated in which each of the three paths in the alcohol sequence was independently constrained to take on the same value across groups. The fit of each constrained model was then compared to that of the structurally unconstrained model using a chi-square difference test (i.e., the difftest option in Mplus). A statistically significant chi-square value indicates a group difference. To guard against an inflated family-wise error rate in this series of tests, a Bonferroni-corrected alpha level was applied (.05 alpha/3 tests = .017). Step 2 culminated in an “alcohol constrained” model with a combination of freely estimated and constrained paths in the sequence from early onset to alcohol abuse.
In Step 3, a series of models was estimated in which each of the 20 paths between the risk factors and the alcohol outcomes was independently forced to take on the same value across groups, comparing the fit of each constrained model to that of the final Step 2 model. A Bonferroni-corrected alpha level was applied to this series of tests (.05 alpha/20 = .0025). Step 3 culminated in an “alcohol-risk constrained” model with a combination of freely estimated and constrained paths in both the alcohol sequence and the risk factor influences.
Results
Correlations, means, and standard deviations for the measured variables are reported in Tables 1 (control group) and 2 (interventions group). Tests of the measurement model showed that the fit of the full sample CFA was acceptable, χ2 (137, N = 666) = 185.37, p < .05, CFI = .943, RMSEA = .020, and factor loadings were satisfactory (Table 3). In multiple groups CFAs, a chi-square difference test comparing the fit of an unconstrained model, χ2 (284, N = 666) = 314.45, p > .05, CFI = .961, RMSEA = .018, to that of a model that forced each respective factor loading to take on the same value across groups, χ2 (295, N = 666) = 336.31, p < .05, CFI = .948, RMSEA = .021, was statistically significant, χ2 (11, N = 666) = 33.33, p < .05, indicating group differences. To isolate group differences, each factor loading was examined separately (available on request). Releasing the constraints on two factor loadings, including an alcohol problems indicator and a parent problem drinking indicator (both of which had higher loadings in the interventions group), resulted in a measurement model with acceptable fit, χ2 (293, N = 666) = 322.90, p > .05, CFI = .962, RMSEA = .018, and satisfactory factor loadings (Table 3). This partially invariant measurement model (39) served as the basis for all subsequent SEMs.
Table 1.
Correlations, Means, and Standard Deviations: Control Group
| Factor - Measured Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Male gender | ||||||||||||||||||||
| 2. PD - Friends break law | .31* | |||||||||||||||||||
| 3. PD - Friends trouble | .17* | .45* | ||||||||||||||||||
| 4. IMP - Let them have it | .27* | .17* | .00 | |||||||||||||||||
| 5. IMP - Say nasty things | .13 | .18* | .04 | .30* | ||||||||||||||||
| 6. IMP - Yell back | .16* | .10 | −.07 | .38* | .48* | |||||||||||||||
| 7. IMP - Tell what I think | .15* | .13 | .11 | .36* | .37* | .48* | ||||||||||||||
| 8. AH - Aggression-Hostility | .05 | .15* | .16* | .19* | .34* | .36* | .22* | |||||||||||||
| 9. AH - Aggression-Hostility (F) | .00 | .08 | .08 | .04 | .15 | .14 | .07 | .31* | ||||||||||||
| 10. AH - Aggression-Hostility (M) | .10 | .07 | .16* | .06 | .17* | .23* | .16* | .37* | .40* | |||||||||||
| 11. PDK - Problem drinking (F) | .23* | .17 | .33* | .03 | .07 | .09 | .08 | .05 | .11 | .09 | ||||||||||
| 12. PDK - Problem drinking (M) | −.02 | .11 | −.02 | .05 | .13 | .07 | −.02 | .13 | .07 | .04 | .43* | |||||||||
| 13. Early alcohol onset | .07 | .00 | .13 | .05 | .07 | .08 | .04 | .10 | −.12 | .09 | .03 | .04 | ||||||||
| 14. ALC - Quantity-Frequency | −.01 | .05 | .14 | .04 | −.05 | −.12 | −.10 | −.08 | −.01 | .08 | .11 | .20 | .04 | |||||||
| 15. ALC - Heavy drinking | −.03 | −.03 | −.06 | −.03 | .01 | −.08 | −.07 | −.18* | −.07 | −.01 | −.07 | .01 | −.03 | .42* | ||||||
| 16. PRB - Trouble remembering | −.11 | .07 | .15 | .01 | −.04 | −.12 | −.10 | −.05 | .03 | −.14 | .10 | .16 | .10 | .23* | .22* | |||||
| 17. PRB - Sick or pass out | −.03 | .00 | −.07 | −.05 | −.04 | −.09 | −.09 | −.06 | −.06 | −.09 | .07 | −.08 | .12 | .21 | .23* | .55* | ||||
| 18. PRB - Get into fight | −.04 | −.05 | .00 | −.05 | .04 | .05 | .10 | −.14 | .16 | .00 | .15 | .05 | −.05 | .27* | .19* | .13 | .06 | |||
| 19. PRB - Alcohol Service use | .11 | .03 | .21* | .11 | .07 | −.07 | .10 | −.04 | −.02 | .12 | .18 | .10 | .21* | .12 | .06 | .43* | .26* | .02 | ||
| 20. Alcohol abuse | .11 | −.05 | −.04 | .18* | .11 | .07 | .13 | .09 | .12 | .12 | −.04 | −.01 | .10 | .14 | .17* | .02 | .04 | −.01 | .09 | |
| Mean (M) | .48 | 1.38 | 1.16 | 2.50 | 1.95 | 2.43 | 2.41 | 2.13 | 2.33 | 2.48 | 1.34 | 1.21 | .03 | .10 | .65 | .36 | .45 | .15 | .06 | .21 |
| Standard deviation (SD) | .50 | .78 | .51 | 1.28 | .97 | 1.22 | 1.21 | .81 | .73 | .81 | .49 | .34 | .18 | 1.65 | 1.73 | .74 | .84 | .51 | .25 | .41 |
Note. PD = Peer Deviance, IMP = Impulsive Behaviors, AH = Aggression-Hostility, PDK = Parent Problem Drinking, ALC = Alcohol Use, and PRB = Alcohol Problems. (F) denotes father-report and (M) denotes mother-report.
p < .05.
Table 3.
Factor Loadings from the Confirmatory Factor Analyses (CFAs)
| Factor/Indicator | Full Sample CFA | Multiple Group CFA | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Full Sample | Control | Interventions | ||||
| b | β | b | β | b | β | |
| Peer Deviance (age 11) | ||||||
| Friends break law | 1.0r | .91 | 1.0r | .69 | 1.0r | .93 |
| Friends trouble | .56* | .66 | .62* | .65 | .62* | .70 |
| Impulsive Behaviors (age 11) | ||||||
| Let them have it | 1.0r | .56 | 1.0r | .49 | 1.0r | .56 |
| Say nasty things | 1.06* | .74 | 1.10* | .71 | 1.10* | .74 |
| Yell back | 1.19* | .71 | 1.23* | .63 | 1.23* | .75 |
| Tell what I think | 1.14* | .65 | 1.19* | .61 | 1.19* | .67 |
| Aggression-Hostility (age 11) | ||||||
| Adolescent-report | 1.0r | .68 | 1.0r | .67 | 1.0r | .69 |
| Father-report | .67* | .48 | .65* | .49 | .65* | .48 |
| Mother-report | .94* | .62 | .92* | .62 | .92* | .61 |
| Parent Problem Drinking (age 11) | ||||||
| Problem drinking (Father) | 1.0r | .62 | 1.0r | .94 | 1.0r | .50 |
| Problem drinking (Mother) | .63* | .62 | [.35*] | .48 | [.87*] | .71 |
| Alcohol Use (age 16) | ||||||
| Quantity-Frequency | 1.0r | .64 | 1.0r | .64 | 1.0r | .65 |
| Heavy drinking | .93* | .61 | .90* | .55 | .90* | .62 |
| Alcohol Problems (age 18) | ||||||
| Trouble remembering | 1.0r | .74 | 1.0r | .79 | 1.0r | .68 |
| Sick or pass out | .89* | .69 | .92* | .64 | .92* | .70 |
| Get into fights | .50* | .48 | [.20*] | .23 | [.67*] | .59 |
| Alcohol service use | .78* | .52 | .93* | .55 | .93* | .57 |
1.0r = reference indicator fixed at unity for scaling and identification purposes. Factor loadings that were freely estimated across groups are in brackets.
< .05.
Chi-square statistics and difference tests for the SEMs (Steps 1–3) are reported in Table 4. Step 1 results showed that the fit between the data and the structurally unconstrained model was acceptable, χ2 (299, N = 666) = 329.99, p > .05, CFI = .963, RMSEA = .018. Note that higher order alcohol paths were tested, but not indicated. Step 2 results showed that two of the three cross-group constraints on the alcohol paths were tenable, whereas one revealed a statistically significant group difference. Specifically, an alcohol constrained model was selected that fixed to equality across groups both the path from early onset to alcohol use and the path from alcohol use to alcohol problems, while freely estimating the path from alcohol problems to alcohol abuse. The fit between the data and the alcohol constrained model was acceptable, χ2 (301, N = 666) = 331.35, p > .05, CFI = .964, RMSEA = .017.
Table 4.
Chi-Square Statistics and Difference Tests
| Model/Constraint | χ2 (df) | Test | χ2 Diff (df) |
|---|---|---|---|
| Step 1 | |||
| 1. Structurally unconstrained model | 329.99 (299) | ----- | ----- |
| Step 2 | |||
| a2. early onset → alcohol use | 330.50 (300) | a2 vs. 1 | 0.43 (1) |
| b2. alcohol use → alcohol problems | 330.85 (300) | b2 vs. 1 | 1.01 (1) |
| c2. alcohol problems → alcohol abuse | 334.20 (300) | c2 vs. 1 | 8.50 (1) † |
| 2. Alcohol constrained model | 331.35 (301) | ----- | ----- |
| Step 3 | |||
| a3. peer deviance → early onset | 332.07 (302) | a3 vs. 2 | .23 (1) |
| b3. impulsive behaviors → early onset | 332.13 (302) | b3 vs. 2 | .25 (1) |
| c3. aggression-hostility → early onset | 332.28 (302) | c3 vs. 2 | 2.06 (1) |
| d3. parent problem drinking → early onset | 331.77 (302) | d3 vs. 2 | 1.18 (1) |
| e3. male gender → early onset | 332.12 (302) | e3 vs. 2 | .32 (1) |
| f3. peer deviance → alcohol use | 332.58 (302) | f3 vs. 2 | 2.71 (1) |
| g3. impulsive behaviors → alcohol use | 332.26 (302) | g3 vs. 2 | 1.96 (1) |
| h3. aggression-hostility → alcohol use | 331.92 (302) | h3 vs. 2 | .10 (1) |
| i3. parent problem drinking → alcohol use | 332.19 (302) | i3 vs. 2 | 1.04 (1) |
| j3. male gender → alcohol use | 332.20 (302) | j3 vs. 2 | .59 (1) |
| k3. peer deviance → alcohol problems | 335.20 (302) | k3 vs. 2 | 25.35 (1)‡ |
| l3. impulsive behaviors → alcohol problems | 333.70 (302) | i3 vs. 2 | 7.87 (1) |
| m3. aggression-hostility → alcohol problems | 334.52 (302) | m3 vs. 2 | 8.87 (1) |
| n3. parent problem drinking → alcohol problems | 331.77 (302) | m3 vs. 2 | 1.12 (1) |
| o3. male gender → alcohol problems | 335.56 (302) | o3 vs. 2 | 13.97 (1) ‡ |
| p3. peer deviance → alcohol abuse | 334.52 (302) | p3 vs. 2 | 14.31 (1) ‡ |
| q3. impulsive behaviors → alcohol abuse | 332.32 (302) | q3 vs. 2 | 1.20 (1) |
| r3. aggression-hostility → alcohol abuse | 333.87 (302) | r3 vs. 2 | 10.08 (1) ‡ |
| s3. parent problem drinking → alcohol abuse | 332.21 (302) | s3 vs. 2 | .31 (1) |
| t3. male gender → alcohol abuse | 332.60 (302) | t3 vs. 2 | 2.26 (1) |
| 3. Final alcohol-risk constrained model | 354.17 (317) | ----- | ----- |
p < .05;
Bonferroni-corrected p < .02 (.05 alpha/3 tests);
Bonferroni-corrected p < .003 (.05 alpha/20 tests).
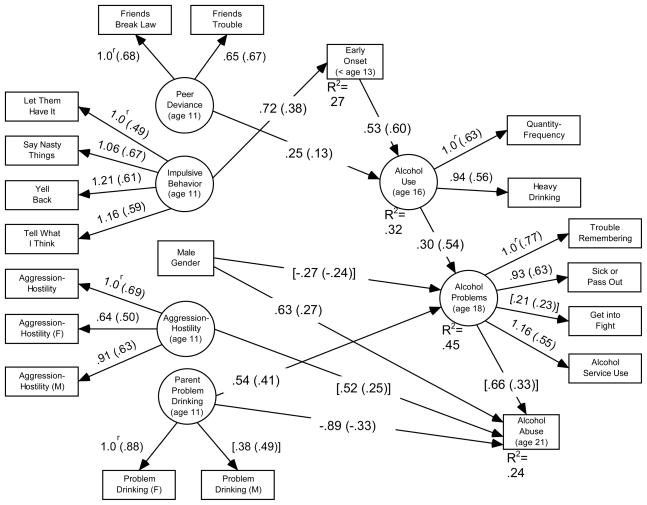
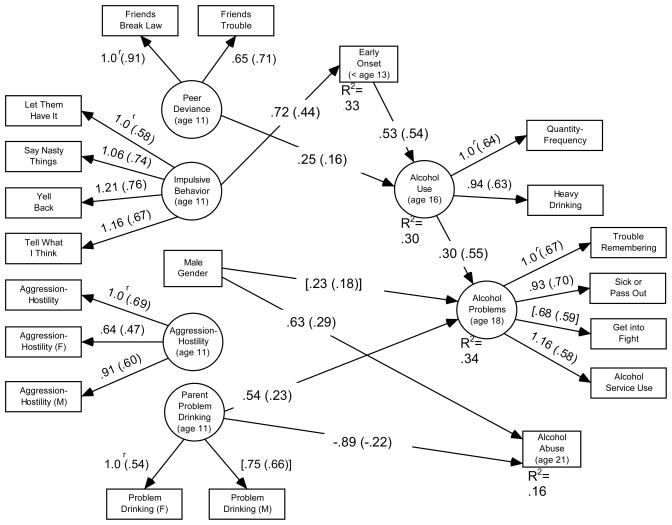
Step 3 results showed that 16 of the 20 cross-group constraints on the risk factor paths were tenable, whereas four revealed statistically significant group differences. Specifically, a final alcohol-risk constrained model was selected that freely estimated not only the path from alcohol problems to alcohol abuse but also the paths from both male gender and peer deviance to alcohol problems and the paths from both peer deviance and aggression-hostility to alcohol abuse; all remaining structural paths were fixed to equality across groups. The fit between the data and the final alcohol-risk constrained model was acceptable, χ2 (317, N = 666) = 354.17, p > .05, CFI = .956, RMSEA = .019. Factor loadings and statistically significant paths are presented in Figures 2 (control group) and 3 (interventions group). Coefficients in brackets were freely estimated across groups. Note that the paths depicted in Figures 2 and 3 were estimated simultaneously in the final alcohol-risk constrained model, therefore adjustments for multiple tests were not needed at this stage of the analysis.
Figure 2.
Multiple group structural equation model of paths in the alcohol sequence and risk factor influences: Control group. Statistically significant unstandardized estimates are presented with standardized estimates in parentheses. Factor loadings that were freely estimated across groups are in brackets. 1.0r = reference indicator fixed at unity for scaling and identification purposes.
Figure 3.
Multiple group structural equation model of paths in the alcohol sequence and risk factor influences: Family interventions group. Statistically significant unstandardized estimates are presented with standardized estimates in parentheses. Factor loadings that were freely estimated across groups are in brackets. 1.0r = reference indicator fixed at unity for scaling and identification purposes.
Results showed that paths in the sequence from early onset to alcohol use and from alcohol use to alcohol problems were positive and statistically significant for both groups. The path from alcohol problems to alcohol abuse, although positive and statistically significant in the control group, was statistically non-significant in the interventions group.
The overall pattern of prediction from risk factors to the alcohol outcomes was similar across groups. Impulsive behaviors, peer deviance, parent problem drinking, and male gender each were statistically significant positive predictors of early onset, alcohol use, alcohol problems, and alcohol abuse, respectively. Unexpectedly, parent problem drinking was a statistically significant negative predictor of alcohol abuse in both groups.
There were four statistically significant group differences in risk factor influences. Although group differences were revealed in the paths from peer deviance to both alcohol problems and alcohol abuse, these paths were statistically non-significant in both groups. Male gender was a significant positive predictor of alcohol abuse in the interventions group, whereas it was a significant negative predictor of alcohol abuse in the control group. Finally, the path from aggression-hostility to alcohol abuse, although positive and statistically significant in the control group, was statistically non-significant in the interventions group.
Discussion
Results identified differential predictors of the multiple dimensions of alcohol involvement and provided evidence that both a link in the alcohol sequence and a prominent risk factor influence were buffered by family preventive interventions. Positive associations in the sequence of alcohol involvement leading from early onset before age 13 to alcohol abuse at age 21 were found, consistent with research indicating that early alcohol initiation is a risk factor for the development of alcohol disorders (9). However, family preventive interventions interrupted this sequence by breaking the link between alcohol problems at age 18 and alcohol abuse at age 21. Whereas this link was positive and statistically significant for control participants, it was not significantly different from zero for intervention participants. Moderation by family interventions was isolated to the point at which alcohol involvement becomes most problematic for young people. Family-focused preventive interventions, such as PDFY and ISFP, may break the sequence of events leading from alcohol problems to alcohol abuse by improving communication, conflict resolution, and coping skills (27;40;41), which represent competencies that might help individuals manage the emerging alcohol problems of adolescence and prevent those problems from escalating to disordered drinking in young adulthood. Without intervention, alcohol problems in adolescence are related to the development of alcohol abuse in early adulthood. This finding suggests that family preventive interventions may help reduce the harms of alcohol involvement by attenuating a key link in the progression to alcohol abuse.
Overall, risk factors differentially predicted the various alcohol outcomes in a similar fashion for both groups. Impulsive behavior was the only significant positive predictor of early onset. Biologically-based theories of personality typically have highlighted the role of disinhibitory psychopathology in the onset of alcohol disorders (42–45); however, current findings are consistent with studies showing that impulsivity plays a role in alcohol initiation (46). Peer deviance was the only significant positive predictor of adolescent alcohol use, perhaps reflecting the correspondence between increased salience of peers (47) and escalation of alcohol use (2) during adolescence. Serious peer deviance appears to conform to the expectation that socialization influences are more strongly related to use than problem use (21).
Parent problem drinking was a positive predictor of adolescent alcohol problems (14). The intergenerational transmission of alcohol problems has been shown to result from a combination of genetic factors and environmental influences (48). Parent problem drinking also predicted alcohol abuse, but the relationship was negative. Given the unexpected and counter intuitive nature of this finding, caution is warranted. Interestingly, male gender was a significant positive predictor of alcohol problems in the interventions group, whereas it was a significant negative predictor in the control group. Supplemental analyses (not reported) showed that this reflects the distribution of responses on certain indicators in this sample (e.g., a higher score on the “trouble remembering” questionnaire item for interventions versus control males). As anticipated (8), males were significantly more likely to meet criteria for alcohol abuse disorder.
Finally, there was one indication that family interventions buffered the link between risk factors and alcohol outcomes. Whereas aggression-hostility had a statistically significant positive association with alcohol abuse in the control group, the association was statistically non-significant in the interventions group. Externalizing problems are well documented risk factors for alcohol involvement (15;16). Current results suggest that such problems, in the form of aggression and hostility, play a particularly important role in the risk for alcohol abuse (49). Moreover, there is an indication that family-focused substance misuse preventive interventions help reduce this risk, perhaps by improving skills or competencies (e.g., conflict resolution skills) that help individuals manage and recover from early adolescent aggressive-hostile tendencies.
Findings support preventive intervention efforts that target multiple risk factors among youth to delay alcohol onset and disrupt the progression to alcohol abuse. Universal substance misuse prevention programs, including PDFY and ISFP, have comparable or stronger effects for high-risk subsamples (50;51), and current findings suggest that it may be beneficial to supplement such programs with selective interventions that target higher-risk youth, such as those who display elevated impulsivity (cf. 52) or those who are children of parents with problem drinking behaviors. Findings regarding peer deviance also support existing intervention efforts to decrease the salience of deviant peer influences and increase youth’s peer resistance skills to prevent adolescent alcohol involvement (27;53).
Limitations include the homogenous sample. Also, certain measures were brief and had lower than desired reliability. Most of the assessments were based on adolescent self-reports. A mono-rater bias may have influenced the findings. Additional research with diverse samples that draws on more extensive measures of key constructs collected by multiple raters and methods is needed. Despite these limitations, this study identified differential predictors of the multiple dimensions of alcohol involvement, and showed that family-focused substance misuse preventive interventions disrupt the link between alcohol problems and alcohol abuse.
Table 2.
Correlations, Means, and Standard Deviations: Interventions Group
| Factor - Measured Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Male gender | ||||||||||||||||||||
| 2. PD - Friends break law | .21* | |||||||||||||||||||
| 3. PD - Friends trouble | .17* | .65* | ||||||||||||||||||
| 4. IMP - Let them have it | .23* | .18* | .13* | |||||||||||||||||
| 5. IMP - Say nasty things | .14* | .13* | .06 | .35* | ||||||||||||||||
| 6. IMP - Yell back | .04 | .10* | −.01 | .44* | .59* | |||||||||||||||
| 7. IMP - Tell what I think | .14* | .15* | .10* | .37* | .50* | .52* | ||||||||||||||
| 8. AH - Aggression-Hostility | .10* | .11* | .06 | .19* | .36* | .20* | .23* | |||||||||||||
| 9. AH - Aggression-Hostility (F) | −.02 | .04 | .01 | .07 | .11* | .14* | .09 | .32* | ||||||||||||
| 10. AH - Aggression-Hostility (M) | .04 | .10* | .07 | .19* | .25* | .19* | .17* | .39* | .42* | |||||||||||
| 11. PDK - Problem drinking (F) | .03 | .02 | .05 | .04 | .10 | .13* | .11 | .09 | .15* | .08 | ||||||||||
| 12. PDK - Problem drinking (M) | −.05 | .03 | .04 | .09 | .10 | .14* | .13* | .08 | .20* | .20* | .38* | |||||||||
| 13. Early alcohol onset | .01 | .16* | .11* | .26* | .19* | .25* | .18* | .18* | .05 | .17* | .11 | .11 | ||||||||
| 14. ALC - Quantity-Frequency | .15 | .13 | .10 | .16* | .09 | .13 | .14 | .15 | −.04 | .20* | −.05 | .08 | .32* | |||||||
| 15. ALC - Heavy drinking | .10 | .17* | .03 | .15* | .14* | .12* | .11 | .10 | −.01 | .08 | .00 | .03 | .39* | .51* | ||||||
| 16. PRB - Trouble remembering | .12* | .01 | .07 | .01 | .10 | .02 | .10 | .03 | .08 | .02 | .02 | .09 | .08 | .16 | .22* | |||||
| 17. PRB - Sick or pass out | .04 | .01 | .12* | −.02 | .03 | .00 | .10 | .09 | .11 | .09 | .01 | .09 | .02 | .34* | .24* | .64* | ||||
| 18. PRB - Get into fight | .08 | −.01 | .14* | .04 | .00 | .06 | .06 | .08 | .06 | .06 | .06 | −.01 | .10 | .21* | .23* | .45* | .37* | |||
| 19. PRB - Alcohol service use | .15* | .06 | .01 | .06 | .05 | .03 | .02 | −.01 | .07 | .06 | .25* | −.01 | −.03 | .25* | .25* | .23* | .25* | .28* | ||
| 20. Alcohol abuse | .22* | .02 | .07 | .09 | .10 | .05 | .05 | .00 | .05 | .09 | −.03 | −.12 | .04 | .08 | .01 | −.02 | .06 | −.10 | −.02 | |
| Mean (M) | .49 | 1.37 | 1.21 | 2.32 | 1.95 | 2.45 | 2.35 | 2.08 | 2.41 | 2.56 | 1.39 | 1.18 | .04 | −.06 | .56 | .44 | .42 | .25 | .06 | .19 |
| Standard deviation (SD) | .50 | .83 | .68 | 1.28 | 1.05 | 1.18 | 1.26 | .84 | .80 | .88 | .51 | .31 | .19 | 1.88 | 1.77 | .98 | .88 | .77 | .24 | .39 |
Note. PD = Peer Deviance, IMP = Impulsive Behaviors, AH = Aggression-Hostility, PDK = Parent Problem Drinking, ALC = Alcohol Use, and PRB = Alcohol Problems. (F) denotes father-report and (M) denotes mother-report.
p < .05.
Acknowledgments
The study was supported by grants AA14702 (National Institute on Alcohol Abuse and Alcoholism), DA10815 (National Institute on Drug Abuse), and MH49127 (National Institute on Mental Health). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. The funding agencies played no role in study design and implementation, data management and analysis, or manuscript preparation.
Footnotes
Conflict of Interest Declaration
None of the authors have a conflict of interest or any financial interest to disclose. Dr. Spoth takes responsibility for the integrity of the data and Dr. Mason takes responsibility for the accuracy of the statistical analyses. All authors had access to the data.
Reference List
- 1.World Health Organization. Global status report on alcohol and health. Geneva, Switzerland: WHO Press; 2011. [Google Scholar]
- 2.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Secondary school students. Vol. 1. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2011. Monitoring the Future national survey results on drug use, 1975–2010. [Google Scholar]
- 3.Spoth RL, Greenberg M, Turrisi R. Preventive interventions addressing underage drinking: State of the evidence and steps toward public health impact. Pediatrics. 2008;121:S311–S336. doi: 10.1542/peds.2007-2243E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhem J, Room R, Montiero M, Gmel G, Graham K, Rehn T, et al. Comparative quantification of health risks: Global and regional burden of disease due to selected major risk factors. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 5.Auerbach KJ, Collins LM. A multidimensional developmental model of alcohol use during emerging adulthood. Journal of Studies on Alcohol. 2006;67:917–25. doi: 10.15288/jsa.2006.67.917. [DOI] [PubMed] [Google Scholar]
- 6.Mason WA, Kosterman R, Haggerty KP, Hawkins JD, Redmond C, Spoth RL, et al. Dimensions of adolescent alcohol involvement as predictors of young adult major depression. Journal of Studies on Alcohol and Drugs. 2008;69:275–85. doi: 10.15288/jsad.2008.69.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1997;9:103–10. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- 8.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64(7):830–42. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 9.Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: Age at onset, duration, and severity. Archives of Pediatrics and Adolescent Medicine. 2011;160:739–46. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- 10.Ellickson PL, Tucker JS, Klein DJ, McGuigan KA. Prospective risk factors for alcohol misuse in late adolescence. Journal of Studies on Alcohol. 2001;62:773–82. doi: 10.15288/jsa.2001.62.773. [DOI] [PubMed] [Google Scholar]
- 11.Colder CR, Chassin L. Affectivity and impulsivity: Temperament risk for adolescent alcohol involvement. Psychology of Addictive Behaviors. 1997;11(2):83–97. [Google Scholar]
- 12.Windle W. A longitudinal study of antisocial behaviors in early adolescence as predictors of late adolescent substance use: Gender and ethnic group differences. Journal of Abnormal Psychology. 1990;99(1):86–91. doi: 10.1037//0021-843x.99.1.86. [DOI] [PubMed] [Google Scholar]
- 13.Ferguson CJ, Meehan DC. With friends like these..: Peer delinquency influences across age cohorts on smoking, alcohol, and illegal substance use. European Psychiatry. 2011;26:6–12. doi: 10.1016/j.eurpsy.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: Putative risk factors, substance use and abuse, and psychopathology. Journal of Abnormal Psychology. 1991;100:427–49. doi: 10.1037//0021-843x.100.4.427. [DOI] [PubMed] [Google Scholar]
- 15.Donovan JE. Adolescent alcohol initiation: A review of psychosocial risk factors. Journal of Adolescent Health. 2004:35. doi: 10.1016/j.jadohealth.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 17.Costa FM, Jessor R, Turbin MS. Transition into adolescent problem drinking: The role of psychosocial risk and protective factors. Journal of Studies on Alcohol. 1999;60:480–90. doi: 10.15288/jsa.1999.60.480. [DOI] [PubMed] [Google Scholar]
- 18.Mason WA, Hitchings JE, Spoth RL. Emergence of delinquency and depressed mood throughout adolescence as predictors of late adolescent problem substance use. Psychology of Addictive Behaviors. 2007;21(1):13–24. doi: 10.1037/0893-164X.21.1.13. [DOI] [PubMed] [Google Scholar]
- 19.Sadava SW. Problem behavior theory and consumption and consequences of alcohol use. Journal of Studies on Alcohol. 1985;46:392–7. doi: 10.15288/jsa.1985.46.392. [DOI] [PubMed] [Google Scholar]
- 20.Simons JS. Differential predictors of alcohol use and problems: The role of biopsychological and social-environmental variables. The American Journal of Drug and Alcohol Abuse. 2003;29(4):861–79. doi: 10.1081/ada-120026265. [DOI] [PubMed] [Google Scholar]
- 21.Stice E, Barrera M, Jr, Chassin L. Prospective differential prediction of adolescent alcohol use and problem use: Examining the mechanisms of effect. Journal of Abnormal Psychology. 1998;107(4):616–28. doi: 10.1037//0021-843x.107.4.616. [DOI] [PubMed] [Google Scholar]
- 22.Windle M. Parental, sibling, and peer influences on adolescent substance use and alcohol problems. Applied Developmental Science. 2000;4:98–110. [Google Scholar]
- 23.Brody GH, Murry VM, Kogan SM, Gerrad M, Gibbons FX, Molgaard V, et al. The Strong African American Families Program: A cluster-randomized prevention trial of long-term effects and a mediational model. Journal of Consulting and Clinical Psychology. 2006;74:356–66. doi: 10.1037/0022-006X.74.2.356. [DOI] [PubMed] [Google Scholar]
- 24.Spoth RL, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: School-level growth curve analyses 6 years following baseline. Journal of Consulting and Clinical Psychology. 2004;72(3):535–42. doi: 10.1037/0022-006X.72.3.535. [DOI] [PubMed] [Google Scholar]
- 25.Bauman KE, Foshee VA, Ennett ST. Family Matters: A family-directed program designed to prevent adolescent tobacco and alcohol use. Health Promotion Practice. 2001;2:81–96. [Google Scholar]
- 26.Spoth R, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: Adolescent substance use outcomes 4 years following baseline. Journal of Consulting and Clinical Psychology. 2001;69:627–42. doi: 10.1037//0022-006x.69.4.627. [DOI] [PubMed] [Google Scholar]
- 27.Mason WA, Kosterman R, Haggerty KP, Hawkins JD, Redmond C, Spoth R, et al. Gender moderation and social developmental mediation of the effect of a family-focused substance use preventive intervention on young adult alcohol abuse. Addictive Behaviors. 2009;34:599–605. doi: 10.1016/j.addbeh.2009.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. Journal of Consulting and Clinical Psychology. 2009;77(4):620–32. doi: 10.1037/a0016029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haggerty KP, Kosterman R, Catalano RF, Hawkins JD. Preparing for the Drug Free Years. Washington DC: Office of Juvenile Justice and Delinquency Prevention; 1999. [Google Scholar]
- 30.Molgaard V, Kumpfer KL. The Iowa Strengthening Families Program: For families with pre- and early adolescents. Ames, IA: Social & Behavioral Research Center for Rural Health; 1993. [Google Scholar]
- 31.Spoth R, Redmond C, Shin C. Direct and indirect latent-variable parenting outcomes of two universal family-focused preventive interventions: Extending a public health-oriented research base. Journal of Consulting and Clinical Psychology. 1998;66:385–99. doi: 10.1037//0022-006x.66.2.385. [DOI] [PubMed] [Google Scholar]
- 32.Spoth R, Reyes ML, Redmond C, Shin C. Assessing a public health approach to delay onset and progression of adolescent substance use: Latent transition and loglinear analysis of longitudinal family preventive intervention outcomes. Journal of Consulting and Clinical Psychology. 1999;67:619–30. doi: 10.1037//0022-006x.67.5.619. [DOI] [PubMed] [Google Scholar]
- 33.Robins LN, Helzer J, Cottler L, Goldring E. The Diagnostic Interview Schedule Version III-R. St. Louis, MO: Washington University School of Medicine; 1989. [Google Scholar]
- 34.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. text rev. [Google Scholar]
- 35.Conger RD. Iowa Youth and Families Project. Ames, IA: Iowa State University Center for Family Research in Rural Mental Health; 1989. [Google Scholar]
- 36.Conger RD, Conger KJ. Resilience in Midwestern families: Selected findings from the first decade of a prospective, longitudinal study. Journal of Marriage and the Family. 2002;64:361–73. [Google Scholar]
- 37.Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- 38.Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods. 2004;9(4):466–91. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Byrne BM, Shavelson RJ, Muthén BO. Testing for the equivalence of factor covariance and mean structures: The issue of partial measurement invariance. Psychological Bulletin. 1989;105(3):456–66. [Google Scholar]
- 40.Kosterman R, Hawkins JD, Spoth R, Haggerty KP, Zhu K. Effects of a preventive parent-training intervention on observed family interactions: Proximal outcomes from Preparing for the Drug Free Years. Journal of Community Psychology. 1997;25(4):337–52. [Google Scholar]
- 41.Redmond C, Spoth R, Shin C, Lepper HS. Modeling long-term parent outcomes of two universal family-focused preventive interventions: One-year follow-up results. Journal of Consulting and Clinical Psychology. 1999;67(6):975–84. doi: 10.1037//0022-006x.67.6.975. [DOI] [PubMed] [Google Scholar]
- 42.Cloninger CR. Neurogenetic adaptive mechanisms in alcoholism. Science. 1987;236:410–6. doi: 10.1126/science.2882604. [DOI] [PubMed] [Google Scholar]
- 43.Gray JA. Perspective on anxiety and impulsivity: A commentary. Journal of Research in Personality. 1987;21:493–509. [Google Scholar]
- 44.Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, et al. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. American Journal of Psychiatry. 2003;160:1078–85. doi: 10.1176/appi.ajp.160.6.1078. [DOI] [PubMed] [Google Scholar]
- 45.Zuckerman M, Kuhlman DM. Personality and risk-taking: Common biosocial factors. Journal of Personality. 2000;68:999–1029. doi: 10.1111/1467-6494.00124. [DOI] [PubMed] [Google Scholar]
- 46.McGue M, Iacono WG, Legrand LN. Origins and consequences of age at first drink. I. Associations with substance-use disorders, disinhibitory behavior, and psychopathology, and P3 amplitude. Alcohol: Clinical and Experimental Research. 2001;25:1156–65. [PubMed] [Google Scholar]
- 47.Steinberg L, Morris AS. Adolescent development. Annual Review of Psychology. 2001;52(83):110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- 48.Rhee SH, Hewitt JK, Young SE, Corley RP, Crowley TJ, Stallings MC. Genetic and environmental influences on substance initiation, use, and problem use in adolescents. Archives of General Psychiatry. 2003;60:1256–64. doi: 10.1001/archpsyc.60.12.1256. [DOI] [PubMed] [Google Scholar]
- 49.Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence and later substance use, abuse, and dependence: Results of a 25-year longitudinal study. Drug and Alcohol Dependence. 2007;88S:S14–S26. doi: 10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 50.Griffin KW, Botvin GJ, Nichols TR, Doyle MM. Effectiveness of a universal drug abuse prevention approach for youth at high risk for substance use initiation. Preventive Medicine. 2003;36(1):1–7. doi: 10.1006/pmed.2002.1133. [DOI] [PubMed] [Google Scholar]
- 51.Spoth R, Redmond C, Shin C, Lepper HS, Haggerty KP, Wall M. Risk moderation of parent and child outcomes in a preventive intervention: A test and replication. American Journal of Orthopsychiatry. 2010;68(4):565–79. doi: 10.1037/h0080365. [DOI] [PubMed] [Google Scholar]
- 52.Palmgreen P, Donohew L, Lorch EP, Hoyle RH, Stephenson MT. Television campaigns and adolescent marijuana use: Tests of sensation seeking targeting. American Journal of Public Health. 2001;91(2):292–6. doi: 10.2105/ajph.91.2.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hansen WB, Graham JW. Preventing alcohol, marijuana, and cigarette use among adolescents: Peer pressure resistance training versus establishing conservative norms. Preventive Medicine. 1991;20(3):414–30. doi: 10.1016/0091-7435(91)90039-7. [DOI] [PubMed] [Google Scholar]