Abstract
Based on cross-sectional analyses, it was suggested that hip circumference divided by height1.5 minus 18 (the body adiposity index, BAI), could directly estimate percent body fat without the need for further correction for sex or age. We compared the prediction of percent body fat, as assessed by dual-energy x-ray absorptiometry (PBFDXA), by BAI, BMI, and circumference (waist and hip) measurements among 1151 adults who had a total body scan by DXA and circumference measurements from 1993 through 2006. After accounting for sex, we found that PBFDXA was related similarly to BAI, BMI, waist circumference, and hip circumference. In general, BAI overestimated PBFDXA among men (3.9%) and underestimated PBFDXA among women (2.5%), but the magnitudes of these biases varied with the level of body fatness. The addition of covariates and quadratic terms for the body size measures in regression models substantially improved the prediction of PBFDXA, but none of the models based on BAI could more accurately predict PBFDXA than could those based on BMI or circumferences. We conclude that the use of BAI as an indicator of adiposity is likely to produce biased estimates of percent body fat, with the errors varying by sex and level of body fatness. Although regression models that account for the non-linear association, as well as the influence of sex, age and race, can yield more accurate estimates of PBFDXA, estimates based on BAI are not more accurate than those based on BMI, waist circumference, or hip circumference.
Introduction
Although the limitations of the body mass index (BMI) are well known [1, 2], this index remains widely used as a simple indicator of adiposity, and adults with a BMI of 30 kg/m2 or more are considered to be obese. An alternative index based on hip circumference and height, termed the ‘body adiposity index’ (BAI), was recently proposed [3]:
This ratio was derived from the cross-sectional associations of hip circumference (r=0.60) and height (r= −0.52) with percent body fat calculated from dual-energy x-ray absorptiometry (PBFDXA) among 1733 Mexican-American adults (61%, women). The power of 1.5 was chosen to maximize the correlation between hip ÷ height and PBFDXA (r=0.79) and 18 was the estimated intercept of a linear regression model predicting PBFDXA. It was concluded that BAI could directly estimate body fatness without the need for further adjustment for characteristics such as sex and age [3]. Data presented in a recent letter [4], however, suggests that following stratification by race and sex, BMI may be as strongly correlated with PBFDXA as is BAI.
The use of hip circumference in the numerator of an adiposity index is also surprising. Persons with larger hip circumferences, relative to BMI, are at lower risk for coronary heart disease (CHD) and total mortality [5]. In addition, the protective effect of a large hip circumference, as compared with waist circumference, is also suggested by its use in the denominator of the waist to hip ratio (WHR) [6, 7]. This simple index of fat distribution has been associated with the development of type 2 diabetes [8–10] and CHD [7, 11], but it is not certain if its effects are independent of BMI [12].
The purpose of the current study is to compare the relation of PBFDXA to various body size measures: BAI, BMI, hip circumference, and waist circumference. We also examine whether the prediction of PBFDXA by BAI is more accurate than that achieved by other measures of body size. The analytic sample comprises 1151 adults who participated in studies conducted at the Body Composition Unit of the New York Obesity Nutrition Research Center between 1993 and 20036.
Methods
Design and Analytic Sample
The current study is based on cross-sectional data from 1151 healthy adults (ages, 18 to 110 y) who participated in one of 11 studies conducted at the Body Composition Unit of the New York Obesity Nutrition Research Center. Study participants were examined between 1993 and 2005 (mean, 1997). All studies obtained written informed consent and were approved by the Radiation Safety Committee and Institutional Review Board of St Luke’s-Roosevelt Hospital. Subjects were included in the current analysis if they were healthy and ambulatory, with no known health condition that would that would affect body composition, and had a total body DXA scan to determine percent body fat (PBFDXA) and a hip circumference measurement. The 1151 subjects included in the current analyses were not missing data for any of the examined characteristics.
Examinations, Anthropometry and Laboratory Procedures
Race-ethnicity was based on self-reported data and included information on the race-ethnicity of parents and grandparents. Subjects in the current study were classified into 5 categories: white (37%), black (27%), Hispanic (25%), Asian (8%), and ‘other’ (3%). About 75% of subjects categorized as Hispanic reported family origins in Puerto Rico or the Dominican Republic. Asians were largely of Japanese, Chinese, or Korean descent.
Height was measured to the nearest 0.1 cm with a wall-mounted stadiometer, and body weight to the nearest 0.1 kg using a balance beam scale with the subjects wearing a hospital gown. Waist and hip circumferences were measured using a heavy-duty inelastic plastic fiber tape measure placed directly on the skin at the level of the iliac crest (for waist) and at the maximum extension of the buttocks (for hip) [13]. The intra-class correlations for repeated measurements in the Body Composition Unit were >0.99 for both waist [14] and hip circumference. The BAI was calculated as [hip circumference (cm) ÷ height (m) 1.5] − 18 [3]. BAI estimates of percent body fat in the current study ranged from 13% to 45% among men and from 16% to 60% among women.
DXA scans were performed using either a Lunar DPX (software versions 1.3 and 1.5) or Lunar DPX-L (software versions 3 and 4). Quality control for fat and fat-free mass measurement was assessed using soft tissue phantoms of water (coefficient of variation = 1.5% to 1.6%) and alcohol (coefficient of variation = 0.6% to 1.3%). PBFDXA was calculated by dividing the total fat value (kg) by the total body mass as measured by the scanner. As previously reported [15], the equation
PBFDXA-L = −0.5532 + 0.9813 × PBFDPX
was used to convert the DPX estimates to their comparable DPX-L values. DPX-L estimates of percent body fat are used throughout the article.
Both models have been validated for the measurement of fat mass, lean mass, and bone mineral content using the 4-compartment model as a reference [16–18].
Statistical Analyses
Because it has been suggested that BAI is a better index of adiposity than BMI [3], the analyses focus on comparing the relation of PBFDXA to BAI and BMI. We also examine the relation of PBFDXA to waist and hip circumferences to determine if these characteristics are as strongly associated with body fatness as BAI. All analyses were performed using R [19].
Several comparisons examined differences in the magnitudes of the correlations with PBFDXA. For example, to determine if PBFDXA was more strongly associated with levels of BAI than with BMI, we examined the difference between (1) the correlation of PBFDXA and BAI, and (2) the correlation of PBFDXA and BMI. Because BMI and BAI are correlated, we assess the statistical significance of this difference using tests for correlated coefficients [20, 21]; the null hypothesis is that the 2 correlations with PBFDXA are identical. Similar tests were performed to assess whether the waist and hip circumferences were as strongly associated with PBFDXA as was BAI. Several results were confirmed using bootstrap resampling [22]. To adjust for sex and age, we calculated the correlation coefficients using the residuals of linear models that regressed the various body size measures on sex and age. P < 0.01 was used to assess statistical significance.
To assess if BAI could accurately estimate PBFDXA, we first plotted levels of both characteristics for each subject. Bland-Altman plots were then constructed by plotting the observed differences (BAI minus PBFDXA) against the mean of the 2 characteristics [23]. A smoothed lowess [24] curve was added to each plot to indicate the pattern of these differences.
We also compared the ability of various regression models of varying complexity, based on each body size measure, to predict PBFDXA. Age, sex, and race were considered as additional covariates in these models. We examined the R2, the residual standard error (root mean square error), and the median absolute difference between predicted and observed values of PBFDXA.
Results
Descriptive characteristics of the sample are shown in Table 1. Mean ages were 45 y (men) and 48 y (women), and 15% of men and 36% of women were obese (BMI ≥ 30 kg/m2). As compared with women, men had substantially lower mean levels of PBFDXA (21%, men vs. 35%, women) and BAI (24, men vs. 33, women). The higher BAIs of women were attributable to their larger hip circumferences (97 cm, men vs. 102 cm, women) and their lower heights. Overall, 37% of the subjects were white, 27% were black and 25% were Hispanic.
Table 1.
Mean levels of various characteristics, by sex, among adults
| Men (n=383) |
Women (n=768) |
|
|---|---|---|
| Age (years) | 45 ± 19a | 48 ± 19 |
| Weight (kg) | 78 ± 14 | 71 ± 17 |
| Height (m) | 1.73 ± 0.08 | 1.60 ± 0.07 |
| BMI (kg/m2) | 25.8 ± 4.3 | 27.6 ± 6.4 |
| BMI ≥ 30 kg/m2(%) | 15% | 36% |
| Waist circumference (cm) | 89 ± 12 | 84 ± 14 |
| Hip circumference (cm) | 97 ± 10 | 102 ± 14 |
| Body Adiposity Index b | 24. 4 ± 5.1 | 32.5 ± 7.4 |
| Percent Body Fat DXA (%) | 20.5 ± 8.4 % | 35.0 ± 9.8% |
| Race – ethnicity | ||
| %White | 30% | 40% |
| %Black | 21% | 30% |
| %Hispanic | 35% | 20% |
| %Asian | 9% | 8% |
| % Other | 6% | 2% |
Values are mean ± SD or percent
Calculated as (hip circumference (cm) ÷ height (m)1.5) – 18.
Interrelationships among the anthropometric characteristics are shown in Table 2. In analyses of men and women together (n=1151), PBFDXA was more strongly correlated with BAI (r=0.86) than with BMI (r=0.74), and both hip (r=0.76) and waist circumference (r=0.55); p<0.01 for each comparison. (The null hypothesis was that magnitude of the correlation between PBFDXA and BAI was equal to the relation of PBFDXA to each of the other 3 characteristics.) In addition, analysis of all 1151 subjects indicated that PBFDXA was almost as strongly associated with height (r= −0.43) as with weight (r= 0.47).
Table 2.
Intercorrelations among the anthropometric characteristics, by sexa
| center | Percent | Body Adiposity | Circumferences |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Body fat | Index | BMI | Hip | Waist | Weight | Height | Age | ||
| Overall | Percent body | 1 | 0.86 | 0.74* | 0.76* | 0.55* | 0.47 | −0.43 | 0.31 |
| Body Adiposity | 0.86 | 1 | 0.83 | 0.84 | 0.63 | 0.48 | −0.55 | 0.35 | |
| BMI | 0.74 | 0.83 | 1 | 0.91 | 0.87 | 0.86 | −0.14 | 0.20 | |
| Men | Percent body fat | 1 | 0.77 | 0.76 | 0.75 | 0.80 | 0.59 | −0.19 | 0.31 |
| Body Adiposity Index | 0.77 | 1 | 0.79 | 0.81 | 0.78 | 0.46 | −0.47 | 0.34 | |
| BMI | 0.76 | 0.79 | 1 | 0.86 | 0.89 | 0.86 | −0.06 | 0.12 | |
| Women | Percent body fat | 1 | 0.82 | 0.85* | 0.83 | 0.81 | 0.78 | −0.07 | 0.34 |
| Body Adiposity Index | 0.82 | 1 | 0.90 | 0.88 | 0.85 | 0.73 | −0.33 | 0.37 | |
| BMI | 0.85 | 0.90 | 1 | 0.92 | 0.92 | 0.92 | −0.06 | 0.22 | |
All correlation coefficients are statistically significant at the 0.001 level (H0: r = 0) with the exception of those between BMI and both height (r= −0.06) and age (r=0.12) among men, and between height and both percent body fat (r= −0.07) and BMI (r= −0.06) among women.
p< 0.01 for difference. P-value assesses whether the correlation between PBFDXA and BAI is equal to the correlation between PBFDXA and BMI, hip circumference, or waist circumference. The null hypothesis is that the correlation between PBFDXA and BAI is equal to the correlation of PBFDXA with each of the other characteristics.
However, stratified analyses in Table 2 indicated that the stronger association between PBFDXA and BAI was largely due to confounding by sex. Among men and women separately, there was little difference in the relation of PBFDXA to levels of BAI, BMI or circumferences, with correlations ranging from r=0.75 (hip circumference) to r=0.80 (waist circumference) among men and from r=0.81 (waist circumference) to r=0.85 (BMI) among women. As assessed by a test for the equality of these correlation coefficients, the only association with PBFDXA that significantly differed from that with BAI was the PBFDXA vs. BMI association. Among women, PBFDXA was more strongly associated with BMI than with BAI (r=0.85 vs. r=0.82); p<0.01 for difference. The magnitudes of the association between PBFDXA and height were also substantially reduced in these stratified analyses.
Controlling for both sex and age (Table 3) indicated that adjusted levels of PBFDXA were more strongly correlated with BMI than with BAI (r=0.80 vs. 0.76, p<0.01 for difference). The difference between the 2 correlation coefficients was most evident among women (r=0.78 (BAI) and r=0.82 (BMI)), whereas there was little difference in the associations among men. Age stratified analyses indicated that BMI was at least as strongly associated with PBFDXA as was BAI, with statistically significant differences (rBMI > rBAI) among 18- to 34-year-olds and those who were at least 60 y of age. PBFDXA was also more strongly associated with BMI than with BAI among both whites and blacks. None of the comparisons in table 3 indicated that PBFDXA was more strongly associated with BAI that with BMI or the circumferences. In some groups (blacks, whites, and older persons) hip circumference was also a stronger correlate of PBFDXA than was BAI.
Table 3.
Sex- and age-adjusteda associations with PBFDXA
| Body Adiposity | Circumferences |
||||||
|---|---|---|---|---|---|---|---|
| Index | BMI | Hip | Waist | Weight | Height | ||
| Overall | --- | 0.76 | 0.80* | 0.78 | 0.76 | 0.73 | −0.03 |
| Sex | Men | 0.74 | 0.76 | 0.74 | 0.76 | 0.63 | −0.08 |
| Women | 0.78 | 0.82* | 0.80 | 0.75 | 0.77 | −0.01 | |
| Age group (y) | 18–34 | 0.79 | 0.83* | 0.80 | 0.81 | 0.77 | −0.01 |
| 35–59 | 0.80 | 0.81 | 0.79 | 0.78 | 0.73 | −0.08 | |
| ≥ 60 | 0.71 | 0.76* | 0.77* | 0.67 | 0.71 | 0.01 | |
| Race | Whites | 0.78 | 0.83* | 0.82* | 0.78 | 0.79 | −0.07 |
| Blacks | 0.76 | 0.82* | 0.83* | 0.77 | 0.78 | 0.01 | |
| Hispanics | 0.71 | 0.73 | 0.75 | 0.70 | 0.70 | 0.02 | |
| Asians | 0.74 | 0.77 | 0.71 | 0.75 | 0.70 | 0.04 | |
Adjusted correlations were calculated using the residuals of various models in which PBFDXA and other characteristics were regressed on sex and age. All adjusted correlations, with the exception of those with height (final column), are statistically significant at the 0.001 level (H0: r = 0).
p< 0.01 for difference in the magnitude of the specified correlation with PBFDXA vs. the correlation with BAI. P-value assesses whether the correlation between PBFDXA and BAI is equal to the correlation between PBFDXA and BMI, hip circumference, or waist circumference. The null hypothesis is that the correlation between PBFDXA and BAI is equal to the correlation of PBFDXA with each of the other characteristics.
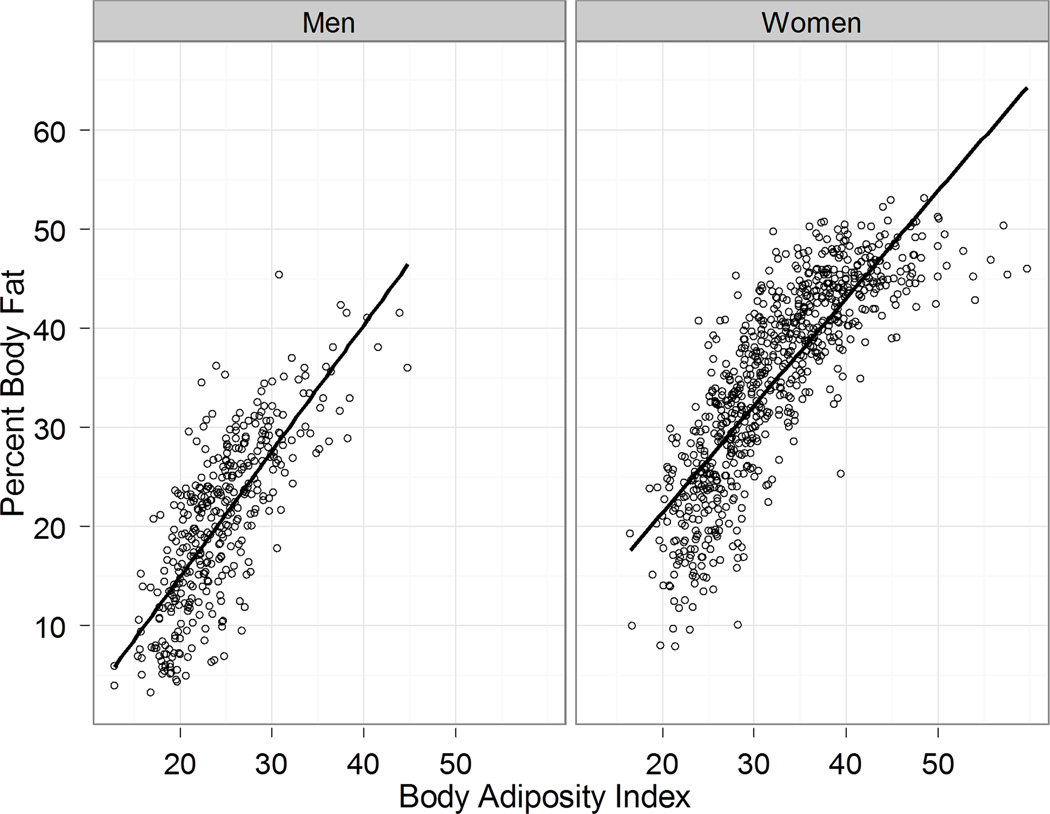
Figure 1 shows levels of BAI and PBFDXA for the 383 men and 768 women. If BAI provided an unbiased estimate of body fatness, the points would be scattered symmetrically around the line of identity. The overall standard deviation of the difference between BAI and PBFDXA was 6.3%, but these differences varied by sex. Among men, the mean difference (BAI minus PBFDXA) was 3.9%, but among women, the mean difference was −2.4%. The bias in using BAI to estimate PBFDXA also varied by the level of body fatness with the over-estimation of percent body fat by BAI most evident at low levels of body fatness.
Figure 1.
Levels of PBFDXA vs. BAI (x-axis) for men (left panel) and women (right panel), with the diagonal line indicating the line of identity (i.e., PBFDXA = BAI). If BAI were a good, unbiased estimator of PBFDXA, the points would cluster around the line of identify, without a discernible pattern.
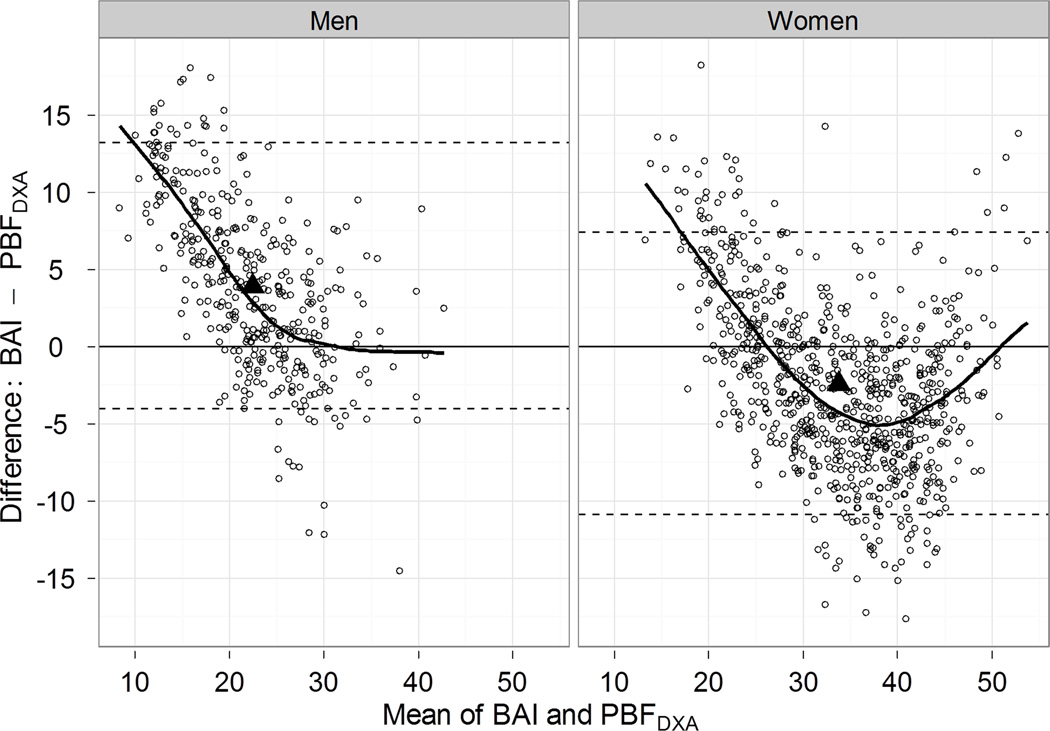
The agreement between BAI and PBFDXA is further examined in Bland-Altman plots (Figure 2), in which the difference (BAI minus PBFDXA) vs. the mean is plotted for each person. Although BAI generally over-estimated PBFDXA among men, the over-estimation was more than 10% among men with low levels of body fatness, but close to 0 among men with levels of body fatness above 25%. (The lines in Figure 2 are loess curves, showing smoothed estimates of the difference by levels of body fatness.) BAI also over-estimated PBFDXA among women at low levels of body fatness, but underestimated PBFDXA (points below y=0 in plot) at moderate to high levels. Overall, BAI over-estimated PBFDXA among 75% of men and under-estimated PBFDXA among 70% of women.
Figure 2.
Bland-Altman plots for difference (BAI - PBFDXA, y-axis) vs. mean (BAI + PBFDXA, x-axis); men are in the left panel, and women in the right panel. The fitted line was smoothed by loess, and indicates the estimated difference (BAI - PBFDXA) at each level of body fatness. The horizontal lines indicate a difference of 0, along with 95% confidence intervals for the observed difference. The solid triangle shows the mean body fatness (based on the 2 variables) and the mean difference (BAI - PBFDXA).
Table 4 examines the prediction accuracy of PBFDXA by the 4 body size measures (BAI, BMI, and the 2 circumferences) in various regression models. In models based on only a single linear term for each body size measure (model #1), BAI was the strongest predictor of PBFDXA, with a R2 of 0.74. (The estimates for hip circumference ÷ height1.5 in this model, however, were −31 (intercept) and 1.28 (slope), values that differ substantially from those reported (−18 and 1.0) by Bergman et al. [3].) Allowing for different intercepts for men and women (model #2) reduced the differences among the body size measures, with multiple R2s ranging from 0.77 (waist circumference and BAI) to 0.79 (BMI). An examination of the residuals from model #2, however, indicated that the errors varied with the level of body fatness, and non-linear terms were therefore included in the model #3, slightly increasing the multiple R2s. Subsequent inclusion of age (model #4) and race-ethnicity (model #5) further increased the R2 values, with the highest R2s seen for BMI (0.84 to 0.85). Of the various models (#5), those based on either BMI or hip circumference were better (p<0.01) predictors of percent body fat than was the model containing BAI.
Table 4.
Various models comparing the prediction of PBFDXA by BAI, BMI, Hip circumference or waist circumference
| Model |
R2 |
Residual Standard Errora |
Median, Absolute Error |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors of PBFDXA | BAI | BMI | Hip | Waist | BAI | BMI | Hip | Waist | BAI | BMI | Hip | Waist | |
| 1 | Linear term | 0.74 | 0.55* | 0.58* | 0.30* | 6.0 | 7.7* | 7.5* | 9.7* | 4.0 | 5.8 | 5.2 | 7.6 |
| 2 | Linear term + sex | 0.77 | 0.79b | 0.78 | 0.77 | 5.5 | 5.3 | 5.5 | 5.5 | 3.6 | 3.6 | 3.7 | 3.7 |
| 3 | Linear and non-linear terms + Sex |
0.80 | 0.83* | 0.79 | 0.79 | 5.2 | 4.8* | 5.2 | 5.3 | 3.4 | 3.2 | 3.5 | 3.4 |
| 4 | Model #3 + age | 0.80 | 0.84* | 0.81 | 0.79 | 5.1 | 4.6* | 5.1 | 5.3 | 3.3 | 3.0 | 3.3 | 3.4 |
| 5 | Model #3 + age + race | 0.81 | 0.85* | 0.83* | 0.80 | 5.1 | 4.5* | 4.8* | 5.2 | 3.3 | 2.9 | 3.1 | 3.3 |
The overall standard deviation of PBFDXA was 11.6 and the standard deviation of the difference between BAI and PBFDXA was 6.3
The estimated equations predicting PBFDXA were −13.6 + 1.32*BMI among men, and −1.5 + 1.32*BMI among women
p<0.01 for comparison of model R2 and standard error vs. those obtained in the model based on BA
Discussion
Our results indicate that BAI is a stronger correlate of PBFDXA than is BMI only in analyses that fail to control for sex or age. Stratification by sex eliminates this difference, with PBFDXA being related similarly (r=0.75 to 0.80 among men and r=0.81 to 0.85 among women) to BAI, BMI, waist circumference, and hip circumference. Further adjustment for age confirmed that BAI was not a stronger correlate of PBFDXA than were these other body size measures. Although differences in the magnitudes of the correlations with PBFDXA were relatively small, in several instances (e.g., women), the observed correlation with BMI was stronger (p<0.01) than that with BAI.
Although it has been suggested [3] that BAI can provide an estimate of percent body fat without the need for further adjustment, our results indicate that these estimates will be systematically biased by sex and the level of fatness. On average, BAI over-estimated PBFDXA by 4% among men and under-estimated PBFDXA among women by 2.5%, biases that are fairly similar to the those reported among subjects in the Fels Longitudinal Study [25]. Although BAI was found to under-estimate PBFDXA by about 7% among 132 women [26], this may have been due to their high BMIs (mean, 35.0 kg/m2 ). Because the bias associated with BIA varies substantially by the level of body fatness (Figure 2), it would be expected that sex differences across studies would vary somewhat depending upon study-specific levels of fatness. It should also be noted that bias in estimating percent body fat by BAI in the study of Bergman et al. [3] varied by the level of fatness (Figure 4), but this was not discussed.
The simplicity of BAI has also been emphasized, but it is uncertain whether it is easier to calculate percent body fat from [hip circumference (cm) ÷ height (m) 1.5] − 18 than estimating body fatness from regression models. Our results (model #2, Table 4), for example, indicate that subtracting 13.6 (men) or 1.5 (women) from 1.32 × BMI would more accurately predict PBFDXA than does BAI. However, if one desired to use hip circumference ÷ height1.5 to predict PBFDXA, our results indicate that the estimates for the best-fitting regression line are −31 (intercept) and 1.28 (slope), values that differ substantially from those reported (−18 and 1.0) by Bergman et al [Bergman '11], but very similar to estimates in the Fels Study (−33 and 1.26) [25]. However, the prediction of percent body fat from either BAI or BMI (based on only a linear term) should be interpreted cautiously as estimates are likely to vary systematically with the level of body fatness.
These findings extend previous studies of adults [27–29] that have showed that (1) BAI is less strongly associated with skinfold thicknesses and risk factors (lipids, insulin, glucose, and blood pressure) than is BMI, and (2) the hip circumference is as strongly correlated with levels of skinfolds and risk factors as BAI. The similarity of the associations with hip circumference and BAI in the current study likely result from weak relation of body fatness to height among adults that we and others [30–32] have observed. It has long been assumed that an optimal index of adult obesity would show little correlation with height [33, 34].
As has been suggested by Schulz and Stefan [35], it is likely that the original derivation of BAI [3] was strongly confounded by sex. The potential for confounding is emphasized in our results, as well as in an analysis of 3851 adults from Baton Rouge [4] that found that PBFDXA was more strongly correlated with BAI than with BMI only in an analysis that combined men and women together. The effects of confounding in the study by Bergman et al. [3] are also evident in the stronger relation of PBFDXA to height (r= −0.52) than to weight (r=0.23). Although the inverse association between PBFDXA and height resulted in standardizing hip circumference for height [3], this association was based on an analyses that grouped men and women together. Because women are generally shorter than men and have more body fat, an analysis of the association between height and body fatness would greatly overstate the strength of the association. In the current study, for example, the unadjusted correlation between height and PBFDXA was r = −0.43 (Table 2), but associations were reduced to |r| < 0.10 in sex-specific analyses that adjusted for age. Similar associations have also been observed in NHANES 1999–2004 (DF, unpublished observation), with height being inversely correlated with PBFDXA (r= −0.50) among all adults (n=12,957) while sex-specific correlations are r= −0.02 (men) and r= −0.10 (women). Analyses of body fatness that do not control for sex should be interpreted very cautiously.
There are several potential limitations of the current study. Our sample is not representative of the general population, and levels of BMI and hip circumferences were lower than those in the study of Bergman et al. [3]. Furthermore, although DXA estimates of body fatness are highly correlated with those from methods such as the 4-compartment model and neutron activation [36], there can be large differences for an individual subject. DXA estimates of percent body fat also can also vary by manufacturer and across models. Estimates of body fatness may also vary systematically, with DXA underestimating the body fatness of leaner persons and overestimating the body fatness of obese persons [37]. Although the use of two different pencil-beam DXA systems in the current study likely resulted in additional errors, a previous study [38] found good agreement (CV=4.4%) in estimates of fat mass between the two systems. Although there can also be differences in the measurement of hip circumference, the maximum extension of the buttocks was measured in the current study and in the analysis of Bergman et al. [3].
In summary, we found that after accounting for the differences in body fatness between men and women, PBFDXA is not more strongly correlated with BAI than levels of BMI, waist circumference, or hip circumference. Although differences in the relation of these body size measures to PBFDXA, were relatively small, in several instances, the adjusted associations with BMI or hip circumference were significantly (p<0.01) stronger than those with BAI. If the accurate measurement of weight (and calculation of BMI) is difficult, circumference measurements could be considered, but the use of BAI has no advantage over the use of either waist or hip circumference.
Acknowledgments
DF was responsible for the data analyses, interpretation of the results, and writing the manuscript. JT, FP, SH, JW, RP, HB, and DG were involved in the interpretation of the results and in revisions of the manuscript.
Abbreviations
- BAI
body adiposity index
- DXA
dual-energy x-ray absorptiometry
- PBFDXA
percent body fat calculated from dual-energy x-ray absorptiometry
- WHR
waist to hip ratio
Footnotes
The findings and conclusions in this report are those of the authors and not necessarily those of CDC.
None of the authors have a personal or financial conflict of interest.
References
- 1.Prentice AM, Jebb SA. Beyond body mass index. Obes. Rev. 2001;2:141–147. doi: 10.1046/j.1467-789x.2001.00031.x. [DOI] [PubMed] [Google Scholar]
- 2.Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am. J. Epidemiol. 1996;143:228–239. doi: 10.1093/oxfordjournals.aje.a008733. [DOI] [PubMed] [Google Scholar]
- 3.Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity (Silver Spring) 2011;19:1083–1089. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barreira TV, Harrington DM, Staiano AE, Heymsfield SB, Katzmarzyk PT. Body adiposity index, body mass index, and body fat in white and black adults. JAMA. 2011;306:828–830. doi: 10.1001/jama.2011.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heitmann BL, Lissner L. Hip Hip Hurrah! Hip size inversely related to heart disease and total mortality. Obes. Rev. 2011;12:478–481. doi: 10.1111/j.1467-789X.2010.00794.x. [DOI] [PubMed] [Google Scholar]
- 6.Molarius A, Seidell JC. Selection of anthropometric indicators for classification of abdominal fatness--a critical review. Int. J. Obes. Relat. Metab. Disord. 1998;22:719–727. doi: 10.1038/sj.ijo.0800660. [DOI] [PubMed] [Google Scholar]
- 7.Canoy D. Coronary heart disease and body fat distribution. Curr. Atheroscler. Rep. 2010;12:125–133. doi: 10.1007/s11883-010-0092-9. [DOI] [PubMed] [Google Scholar]
- 8.Stevens J, Couper D, Pankow J, Folsom AR, Duncan BB, Nieto FJ, et al. Sensitivity and specificity of anthropometrics for the prediction of diabetes in a biracial cohort. Obes. Res. 2001;9:696–705. doi: 10.1038/oby.2001.94. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am. J. Clin. Nutr. 2005;81:555–563. doi: 10.1093/ajcn/81.3.555. [DOI] [PubMed] [Google Scholar]
- 10.Schulze MB, Heidemann C, Schienkiewitz A, Bergmann MM, Hoffmann K, Boeing H. Comparison of anthropometric characteristics in predicting the incidence of type 2 diabetes in the EPIC-Potsdam study. Diabetes Care. 2006;29:1921–1923. doi: 10.2337/dc06-0895. [DOI] [PubMed] [Google Scholar]
- 11.Taylor AE, Ebrahim S, Ben-Shlomo Y, Martin RM, Whincup PH, Yarnell JW, et al. Comparison of the associations of body mass index and measures of central adiposity and fat mass with coronary heart disease, diabetes, and all-cause mortality: a study using data from 4 UK cohorts. Am. J. Clin. Nutr. 2010;91:547–556. doi: 10.3945/ajcn.2009.28757. [DOI] [PubMed] [Google Scholar]
- 12.Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang J, Thornton J, Kolesnik S, Pierson R., Jr Anthropometry in body composition: an overview. Ann N.Y. Acad. Sci. 2000;904:317–326. doi: 10.1111/j.1749-6632.2000.tb06474.x. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Thornton JC, Bari S, Williamson B, Gallagher D, Heymsfield SB, et al. Comparisons of waist circumferences measured at 4 sites. Am. J. Clin. Nutr. 2003;77:379–384. doi: 10.1093/ajcn/77.2.379. [DOI] [PubMed] [Google Scholar]
- 15.Davidson LE, Wang J, Thornton JC, Kaleem Z, Silva-Palacios F, Pierson RN, et al. Predicting fat percent by skinfolds in racial groups: Durnin and Womersley revisited. Med. Sci. Sports Exerc. 2011;43:542–549. doi: 10.1249/MSS.0b013e3181ef3f07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evans EM, Saunders MJ, Spano MA, Arngrimsson SA, Lewis RD, Cureton KJ. Body-composition changes with diet and exercise in obese women: a comparison of estimates from clinical methods and a 4-component model. Am. J. Clin. Nutr. 1999;70:5–12. doi: 10.1093/ajcn/70.1.5. [DOI] [PubMed] [Google Scholar]
- 17.Heymsfield SB, Wang J, Heshka S, Kehayias JJ, Pierson RN. Dual-photon absorptiometry: comparison of bone mineral and soft tissue mass measurements in vivo with established methods. Am. J. Clin. Nutr. 1989;49:1283–1289. doi: 10.1093/ajcn/49.6.1283. [DOI] [PubMed] [Google Scholar]
- 18.Prior BM, Cureton KJ, Modlesky CM, Evans EM, Sloniger MA, Saunders M, et al. In vivo validation of whole body composition estimates from dual-energy X-ray absorptiometry. J. Appl. Physiol. 1997;83:623–630. doi: 10.1152/jappl.1997.83.2.623. [DOI] [PubMed] [Google Scholar]
- 19.R Development Core Team. R. A language and environment for statistical computing (version 2.14.1). R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0. 2012. [Google Scholar]
- 20.Neill JJ, Dunn OJ. Equality of dependent correlation coefficients. Biometrics. 1975;31:531–543. [Google Scholar]
- 21.Revelle W. psych: Procedures for Psychological, Psychometric, and Personality Research. R package version 1.0-95. 2011 http://personality-projectorg/r/psychmanual.pdf.
- 22.Canty A, Ripley B. boot: Bootstrap R (S-Plus) Functions. R package version 1.3-2. 2011 Available at http://cranr-projectorg/web/packages/boot/index.html.
- 23.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999;8:135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 24.Cleveland WS. Visualizing data. Murray Hill, NJ: Hobart Press; 1993. [Google Scholar]
- 25.Johnson W, Chumlea WC, Czerwinski SA, Demerath EW. Concordance of the recently published body adiposity index with measured body fat percent in European-American adults. Obesity (Silver Spring) 2011 doi: 10.1038/oby.2011.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elisha B, Rabasa-Lhoret R, Messier V, Abdulnour J, Karelis AD. Relationship between the body adiposity index and cardiometabolic risk factors in obese postmenopausal women. Eur. J. Nutr. 2012 doi: 10.1007/s00394-011-0296-y. [DOI] [PubMed] [Google Scholar]
- 27.Freedman DS, Ogden CL, Blanck HM. The relation of the hip to height adiposity index to skinfold thicknesses and risk factor levels among adults in NHANES III. 2012 (Submitted) [Google Scholar]
- 28.Freedman DS, Blanck HM, Dietz WH, DasMahapatra P, Srinivasan SR, Berenson GS. Is the body adiposty index (hip circumference / height^1.5) more strongly related to skinfold thicknesses and risk factor levels among 18- to 49-year-olds: the Bogalusa Heart Study. Br J Nutr. 2012 doi: 10.1017/S0007114512000979. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gomes de Lima J, Nobrega LH, Barbosa Camara de Souza A. Body Adiposity Index indicates only total adiposity, not risk. Obesity (Silver Spring) 2012 doi: 10.1038/oby.2012.3. [DOI] [PubMed] [Google Scholar]
- 30.Micozzi MS, Albanes D, Jones DY, Chumlea WC. Correlations of body mass indices with weight, stature, and body composition in men and women in NHANES I and II. Am. J. Clin. Nutr. 1986;44:725–731. doi: 10.1093/ajcn/44.6.725. [DOI] [PubMed] [Google Scholar]
- 31.Flegal KM. Ratio of actual to predicted weight as an alternative to a power-type weight-height index (Benn index) Am. J. Clin. Nutr. 1990;51:540–547. doi: 10.1093/ajcn/51.4.540. [DOI] [PubMed] [Google Scholar]
- 32.Knapik JJ, Burse RL, Vogel JA. Height, weight, percent body fat indices of adiposity for young men and women entering the U.S. Army. Aviat. Space Environ. Med. 1983;54:223–231. [PubMed] [Google Scholar]
- 33.Benn RT. Some mathematical properties of weight-for-height indices used as measures of adiposity. Br. J. Prev. Soc. Med. 1971;25:42–50. doi: 10.1136/jech.25.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Billewicz WZ, Kemsley WF, Thomson AM. Indices of adiposity. Br. J. Prev. Soc. Med. 1962;16:183–188. doi: 10.1136/jech.16.4.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schulze MB, Stefan N. The body adiposity index and the sexual dimorphism in body fat. Obesity (Silver Spring) 2011;19:1729. doi: 10.1038/oby.2011.153. [DOI] [PubMed] [Google Scholar]
- 36.Toombs RJ, Ducher G, Shepherd JA, De Souza MJ. The Impact of Recent Technological Advances on the Trueness and Precision of DXA to Assess Body Composition. Obesity (Silver Spring) 2011 doi: 10.1038/oby.2011.211. [DOI] [PubMed] [Google Scholar]
- 37.Van Der Ploeg GE, Withers RT, Laforgia J. Percent body fat via DEXA: comparison with a four-compartment model. J. Appl. Physiol. 2003;94:499–506. doi: 10.1152/japplphysiol.00436.2002. [DOI] [PubMed] [Google Scholar]
- 38.Soriano JM, Ioannidou E, Wang J, Thornton JC, Horlick MN, Gallagher D, et al. Pencil-beam vs fan-beam dual-energy X-ray absorptiometry comparisons across four systems: body composition and bone mineral. J. Clin. Densitom. 2004;7:281–289. doi: 10.1385/jcd:7:3:281. [DOI] [PubMed] [Google Scholar]