Abstract
Background
Superior-level facet joint violation by pedicle screws may result in increased stress to the level above the instrumentation and may contribute to adjacent segment disease (ASD). Previous studies have evaluated facet joint violations in open or percutaneous screw cases, but there are no reports describing a direct institutional comparison.
Objective
To compare the incidence of superior-level facet violation for open versus percutaneous pedicle screws, and evaluate patient and surgical factors that impact this outcome.
Methods
We reviewed 279 consecutive patients who underwent an index instrumented lumbar fusion from 2007 to 2011 for degenerative spine disease with stenosis with or without spondylolisthesis. We used a CT grading system which represents progressively increasing grades of facet joint violation. Patient and surgical factors were evaluated to determine their impact on facet violation.
Results
Our cohort consisted of 126 open and 153 percutaneous cases. Percutaneous procedures had a higher overall violation grade (p=0.018) and greater incidence of high-grade violations (p=0.0059) compared to open procedures. Bivariate analysis showed significantly greater violations in percutaneous cases for age<65, obesity, pedicle screws at L4, and 1- and 2-level surgeries. Multivariate analysis showed the percutaneous approach and depth of the spine to be independent risk factors for high-grade violations.
Conclusion
This study demonstrates greater facet violations for percutaneously placed pedicle screws compared to open.
Keywords: facet joint violation, open, percutaneous, adjacent segment disease, depth of spine
Introduction
The most widely used technique for instrumented posterior lumbar fusion is the traditional open approach1. However, there is increasing interest in the minimally invasive technique of placing pedicle screws percutaneously. The standard open technique requires extensive dissection of soft tissue and muscle to expose anatomical landmarks, resulting in increased blood loss, greater risk of postoperative infection, and prolonged recovery time1-7. The percutaneous technique attempts to reduce some of these issues by decreasing the operative time and extent of dissection, leading to decreased blood loss, faster recovery time, and less postoperative incisional back pain1, 8-12.
An important consideration in all instrumented pedicle screw cases is preventing the development of adjacent level disease (ASD) by limiting injury to the adjacent level structures, specifically the superior facet. Damage to this facet joint can contribute to increased stress at the adjacent level and possibly lead to radiological and symptomatic adjacent segment stenosis, requiring additional surgery and increased medical costs13, 14. Previous studies report the rates of facet joint violation in open procedures to be 24%-100% depending on the specific screw insertion technique utilized15-17. For percutaneous procedures, rates range from 11-50%18, 19. A recent cadaveric study by Patel et al. found a 58% rate of facet violation with percutaneous pedicle screw insertion20. Overall, there is not a consensus on which approach has a greater incidence of facet joint violations.
To our knowledge there is no study directly comparing facet joint violations in open and percutaneous procedures performed by a surgical team. The purpose of this study was to investigate the incidence of cranial facet joint violations with open and percutaneous pedicle screw insertion methods at a single academic institution with surgeons routinely performing both techniques. Patient and operative characteristics were evaluated to determine whether they impact the rate of facet violation. Postoperative computed tomography (CT) was used in this study to assess facet joint violations, as CT has been shown to be more accurate than plain radiography in detecting the placement of pedicle screws21, 22.
Materials and Methods
Patient Cohort
Institutional review board approval was obtained for this study. We retrospectively reviewed all patients who underwent instrumented lumbar fusion (open or percutaneous) by our six spine surgeons from January 2007 to November 2011 for degenerative spine disease with stenosis with or without spondylolisthesis. Additional inclusion criteria for the study included age greater than 18 years, bilateral pedicle screw fixation, and presence of a postoperative CT scan performed no later than 3 months after surgery. We performed 2 different methods to confirm all patients meeting these criteria were included. We evaluated a list of all surgeries performed at our institution during the study period for these criteria and then checked the medical and radiological records to confirm patients who had postoperative CT. Also, we searched a hospital based database by CPT codes for lumbar instrumentation (22840 and 22842) and coding for CT lumbar spine (72131-72133). Two-hundred and seventy nine patients met our inclusion criteria and were the basis of this study. This cohort included 126 open and 153 percutaneous cases (Table 1). As all patients had screws placed bilaterally, this study evaluated 558 screws. The surgical indications for the procedures included stenosis with spondylolisthesis (51.4%), stenosis with degenerative spine disease and arthropathy (33.2%), degenerative scoliosis with stenosis (12.9%), and stenosis with pseudoarthrosis at a cranial level (2.5%). Also, there were no significant differences between the indications for open and percutaneous cases. Of the 279 patients, 133 (47.7%) were male and 146 (52.3%) were female. The average age for our cohort was 62 years, with ages ranging from 22 to 90 years. Table 1 demonstrates that the percutaneous and open groups had similar baseline and surgical demographics.
Table 1. Patient, screw, and violation characteristics: Open versus percutaneous screws.
| Open | Percutaneous | P-value | |
|---|---|---|---|
| Number of screws | 252 | 306 | NA |
| Mean age | 60.1 ± 1.1 | 61.1 ± 1.1 | 0.55 |
| Mean BMI | 30.9 ± 0.55 | 29.4 ± 0.51 | 0.057 |
| Male (n = 133) | 50% (n = 63) | 45.8% (n = 70) | 0.48 |
| Female (n = 146) | 50% (n = 63) | 54.2% (n = 83) | 0.48 |
| Top screws | |||
| L1 (n = 29) | 7.9% (n = 10) | 12.4% (n = 19) | 0.22 |
| L2 (n = 56) | 14.3% (n = 18) | 24.8% (n = 38) | 0.029 |
| L3 (n = 52) | 24.6% (n = 31) | 13.7% (n = 21) | 0.020 |
| L4 (n = 111) | 42.1% (n = 53) | 37.9% (n = 58) | 0.48 |
| L5 (n = 31) | 11.1% (n = 14) | 11.1% (n = 17) | 1.0 |
| Fusion length | |||
| 5 levels (n = 10) | 4.0% (n = 5) | 3.3% (n = 5) | 0.76 |
| 4 levels (n = 33) | 7.1% (n = 9) | 15.7% (n = 24) | 0.028 |
| 3 levels (n = 37) | 13.5% (n = 17) | 13.1% (n = 20) | 0.92 |
| 2 levels (n = 71) | 26.2% (n = 33) | 24.8% (n = 38) | 0.80 |
| 1 level (n = 128) | 49.2% (n = 62) | 43.1% (n = 66) | 0.31 |
| Depth of spine [mm] (SD) | 79.7 ± 19.5 | 71.6 ± 18.4 | 0.0009 |
| Mean facet violation grade | 0.45 ± 0.045 | 0.62 ± 0.053 | 0.018 |
| Incidence grade 1 | 63 (25.0%) | 82 (26.8%) | 0.70 |
| Incidence grade 2 | 18 (7.1%) | 15 (4.9%) | 0.34 |
| Incidence grade 3 | 5 (2.0%) | 26 (8.5%) | 0.0059 |
| Long-term follow-up | 48 (84.2%) | 9 (15.8%) | < 0.001 |
Surgical Team
The surgical team consisted of 6 surgeons who performed percutaneous and open surgeries during the study period (Table 2). Three surgeons performed both percutaneous and open cases, with the others only using one approach. The study surgeons had a median post-training experience of 4.5 years (range: 3 to 24). Of the 4 surgeons who performed percutaneous screws, 2 placed screws through a direct or target view of each pedicle on fluoroscopy while the other two lined up the fluoroscopic images based on the endplates and spinous process. There were no significant differences in violations between these two techniques. Also, no significant differences in the grades of facet joint violations were found between surgeons.
Table 2. Technique and experience of study surgeons.
| Surgeon | Approaches used | Spine fellowship | Years from training/ Fellowship experience |
|---|---|---|---|
| 1 | Perc/Open | No | 3 |
| 2 | Perc/ Open | Yes | 5 |
| 3 | Open | Yes | 24 |
| 4 | Perc | Yes | 9 |
| 5 | Open | Yes | 4 |
| 6 | Perc/Open | Yes | 3 |
Radiographic Evaluation
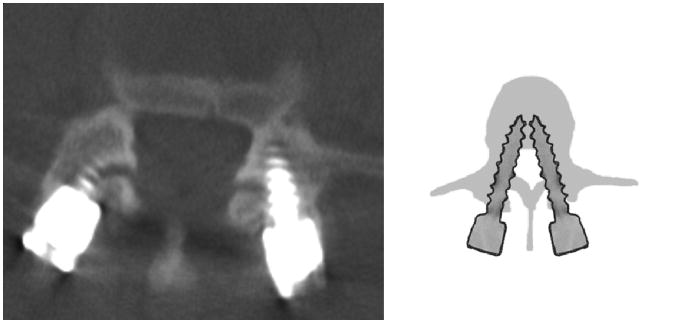
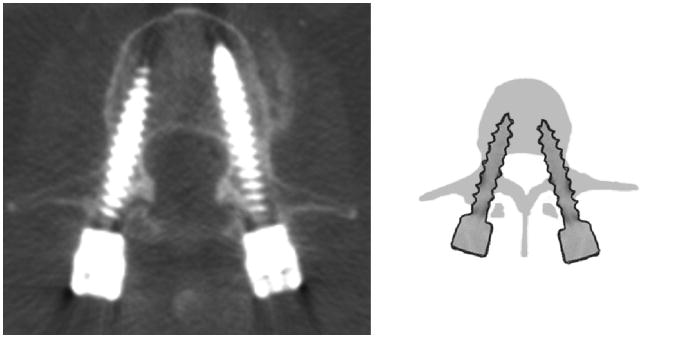
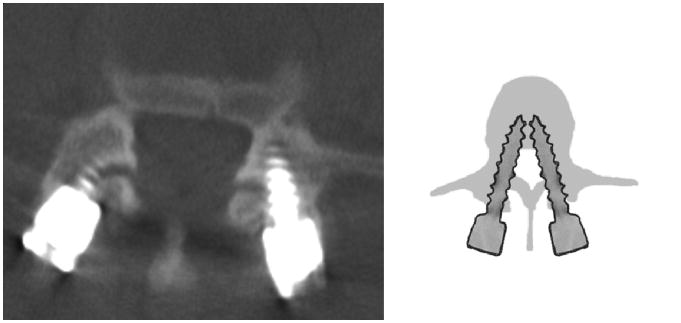
All CT scans were obtained with 0.6mm slices and allowed for coronal and sagittal reconstructions. Postoperative CT scans were primarily acquired for routine hardware evaluations (41.9%). CT scans were also ordered for persistent back or leg pain (28.0%), and the presence of postoperative complications such as new neurological deficit/symptoms, hematoma, or evaluation of surgical site infection (18.3%). The remaining scans (11.8%) were performed for non-neurosurgical indications including abdominal and pelvic pathology and pain. It is important to note that there were no significant differences in the indications for getting a CT scan between percutaneous and open cases. Also, there was no significant difference in facet violations when comparing across indications. The presence of facet violation on the postoperative CT at less than 3 months did not guide any acute management or clearly result in new acute symptoms. The grading criterion for facet joint violation was established prior to radiographic review (Table 3). A screw that was not in the facet and did not encroach upon the facet joint was labeled as a grade 0. If the screw was in the lateral facet but did not enter the articular facet, it was labeled as a grade 1 (Figure 1). Screws that penetrated the articular facet by ≤ 1 mm were assigned a grade 2 violation (Figure 2). Those screws travelling within the articular surface of the facet were given a grade 3 designation (Figure 3). All screws were graded by evaluating axial images together with the coronal and sagittal reconstructed ones.
Table 3. Facet joint violation grading scale.
| Grade 0 | Screw not in facet |
|---|---|
| Grade 1 | Screw in lateral facet but not in facet articulation |
| Grade 2 | Penetration of facet articulation by screw |
| Grade 3 | Screw travels within facet articulation |
Figure 1. Grade 1 violation: screw violates the lateral facet (Bilateral).
Figure 2. Grade 2 violation: screw violates the articular facet surface (Right).
Figure 3. Grade 3 violation: screw lies within the articular facet surface (Bilateral).
The top-level screws were evaluated by 2 different observers for evidence and grade of facet violation. The inter- and intra-observer Pearson r coefficients were 0.98 and 1.0, respectively. Both sides were assessed independently. Patient parameters such as age, gender, and body mass index (BMI) in addition to surgical factors including the level or segment of spine at the top of the construct, the distance from the skin surface to the L4 lamina, and the number of operative levels were recorded. Operative reports and radiographic images were used to confirm whether the screws were placed through an open or percutaneous technique.
The primary outcomes for this study were the mean grade and incidence of facet violation due to open and percutaneous pedicle screw placement. Secondary outcomes included evaluating patient and surgery factors impacting primary outcomes. We also evaluated if facet violations impacted the development of clinically significant adjacent segment. The charts of patients with at least 3 years of follow up were reviewed to determine need for subsequent lumbar surgery due to adjacent level disease. We compared facet violation grade for patients requiring surgery for ASD compared to ones who remained asymptomatic.
Statistical Analysis
Associations between dichotomous surgery type (open vs. percutaneous cases) and other categorical variables (gender, dichotomized BMI, age etc.) were determined using chi-squared tests. Relationships between surgery type and normally distributed continuous variables were examined using Student's t-test. Multivariate analysis of dichotomized outcomes of summary grade of violation variable and surgery type along with risk variables (age (<65 or > 65), gender, BMI (<30 or >30), BMI, depth of spine (distance from skin to L4 lamina), level of cranial aspect of construct, and fusion length) were performed using logistic regression analysis. All analyses were conducted using SAS 9.2 (SAS, SAS Institute Inc, Cary, NC).
Results
Outcomes between open and percutaneous procedures (Tables 1,4,5)
Table 4. Impact of patient and surgery factors on the mean grade of facet violation: Open versus percutaneous screws.
| Risk Factor | Mean Facet Violation | ||
|---|---|---|---|
| Open | Percutaneous | P-value | |
| Age greater than 65 | 0.40 ± 0.066 | 0.46 ± 0.054 | 0.48 |
| Age less than 65 | 0.48 ± 0.060 | 0.76 ± 0.085 | 0.0089 |
| Sex (male) | 0.46 ± 0.062 | 0.66 ± 0.077 | 0.051 |
| Sex (female) | 0.44 ± 0.065 | 0.59 ± 0.072 | 0.15 |
| BMI greater than 30 | 0.44 ± 0.064 | 0.78 ± 0.096 | 0.0031 |
| BMI less than 30 | 0.49 ± 0.069 | 0.53 ± 0.061 | 0.69 |
| Top screws | |||
| L1 | 0.65 ± 0.13 | 0.18 ± 0.064 | <0.001 |
| L2 | 0.31 ± 0.087 | 0.47 ± 0.071 | 0.16 |
| L3 | 0.32 ± 0.072 | 0.45 ± 0.11 | 0.30 |
| L4 | 0.40 ± 0.064 | 0.69 ± 0.089 | 0.0093 |
| L5 | 1.0 ± 0.22 | 1.41 ± 0.24 | 0.22 |
| Fusion length | |||
| 4 levels | 0.28 ± 0.14 | 0.38 ± 0.087 | 0.56 |
| 3 levels | 0.41 ± 0.10 | 0.53 ± 0.095 | 0.42 |
| 2 levels | 0.30 ± 0.061 | 0.58 ± 0.094 | 0.019 |
| 1 level | 0.55 ± 0.076 | 0.81 ± 0.097 | 0.037 |
Table 5. Impact of patient and surgery factors on grade 3 violation: Open versus percutaneous screws.
| Risk Factor | Incidence grade 3 | ||
|---|---|---|---|
| Open | Percutaneous | P-value | |
| Age greater than 65 (n = 236) | 1.1% (n = 1) | 1.4% (n = 2) | 0.82 |
| Age less than 65 (n = 322) | 2.5% (n = 4) | 14.6% (n = 24) | 0.0019 |
| Sex (male) (n = 266) | 2.4% (n = 3) | 8.6% (n = 12) | 0.068 |
| Sex (female) (n = 292) | 1.6% (n = 2) | 8.4% (n = 14) | 0.040 |
| BMI greater than 30 (n = 248) | 2.4% (n = 3) | 13.1% (n = 16) | 0.011 |
| BMI less than 30 (n = 292) | 1.8% (n = 2) | 5.6% (n = 10) | 0.16 |
| L4 (n = 222) | 0.94% (n = 1) | 10.3% (n = 12) | 0.0056 |
| L5 (n = 62) | 14.3% (n = 4) | 38.2% (n = 13) | 0.14 |
| 1 level (n = 256) | 4.0% (n = 5) | 16.7% (n = 22) | 0.0087 |
| Depth of spine | 81.8 ± 2.9 | 90.3 ± 4.1 | 0.37 |
There was a statistically significant difference between percutaneous and open screws with overall grade (0.62 versus 0.45, p = 0.018) and the incidence of grade 3 violations (8.5% versus 2.0%, p = 0.0059). No significant differences were seen in the incidences of grade 1 (25.0% versus 26.8%, p = 0.70) and grade 2 (7.1% versus 4.9%, p = 0.34) violations between the open and percutaneous groups (Table 1).
Factors impacting the primary measures for percutaneous and open screws were explored. Patients under the age of 65 who underwent percutaneous pedicle screw insertion had a significantly higher overall violation grade (0.76 versus 0.48, p = 0.0089) and incidence of grade 3 violations (14.6% versus 2.5%, p = 0.0019) than those who underwent an open procedure. For obese patients (BMI > 30), those who underwent a percutaneous procedure also had a higher overall violation grade per screw (0.78 vs. 0.44, p = 0.0031) and incidence of grade 3 violations (13.1% vs. 2.4%, p = 0.011) (Tables 4 and 5).
Analysis of the top of the fusion construct revealed a significant difference between the percutaneous and open procedures at L4. With the top of the construct at L4, the percutaneous group had a significantly higher overall grade per screw (0.69 versus 0.40, p = 0.0093) and incidence of grade 3 violations (10.3% versus 0.94%, p = 0.0056). Percutaneous screws also had a trend of higher violations at L5, with a higher overall grade per screw (1.41 versus 1.0, p = 0.22) and incidence of grade 3 violations (38.2% versus 14.3%, p = 0.14) (Tables 4 and 5).
The number of operative levels and grade and incidence of facet violation were different between percutaneous and open groups. Those who underwent a 2-level surgery percutaneously had a higher overall violation grade (0.58 vs. 0.30, p = 0.019) and incidence of grade 3 violations (5.3% vs. 0%). Analysis of those who underwent a 1-level procedure also revealed significant differences in the primary measures, with those in the percutaneous group having a significantly higher overall violation grade (0.81 versus 0.55, p = 0.037) and incidence of grade 3 violations (16.7% versus 4.0%, p = 0.0087) (Tables 4 and 5). Finally, no grade 3 violations were found in either group during 3-, 4-, or 5-level surgeries.
Stepwise logistical regression analysis was conducted with age (<65 vs. >= 65), BMI (<30 vs. >= 30), depth of the spine (distance from skin to L4 lamina), level of cranial aspect of construct, and fusion length variables. These results need to be interpreted with caution because of the relatively low incidence of high grade violations. These results revealed factors that independently contributed to a high grade violation including the percutaneous approach and depth of the spine. The odds ratio (OR) for significant risk factors for high grade facet violation was 8.55 (95% CI: 2.51, 29.14) for the percutaneous approach and 1.04 (95% CI: 1.02, 1.07) for depth of the spine. Interestingly, age <65 showed increased risk for high grade violations for percutaneous screws (OR: 8.5; 95% CI: 1.20, 15.95).
The effect of pedicle screw insertion by residents was also evaluated by comparing facet joint violation of screws on each side of the spine. One surgeon employing the open approach had a significantly higher overall violation grade in left-sided screws (0.59 vs. 0.22, p = 0.047). All other surgeons inserting pedicle screws using the open approach had similar overall violation grades between screw sides (p = 0.86, 0.26, 0.17, and 0.98). However, right-sided screws had a significantly higher overall violation grade for one surgeon utilizing the percutaneous technique (0.53 vs. 0.30, p = 0.046). The remaining 3 surgeons performing percutaneous cases had similar violation grades between screw sides (p = 0.79, 0.29, and 0.27).
Facet joint violations in patients who underwent additional lumbar surgery
There were 57 patients in our cohort who had at least 3 years of follow up, most of whom underwent open lumbar fusion surgery (84.2%). Of these patients, 7 (12.3%) had a subsequent lumbar surgery due to symptomatic adjacent level stenosis and degeneration requiring adjacent level decompression with extension of fusion. ASD was diagnosed using CT or MRI, with all patients having mild-moderate facet hypertrophy and degeneration, mild-severe central canal stenosis, and foraminal narrowing. Patients that had additional lumbar surgery had a significantly higher overall violation grade (1.1 versus 0.49, p = 0.0016) and incidence of grade 2 violations (35.7% versus 7.0%, p = 0.0095) compared to all patients with 3 years of follow up. Also, the incidence of grade 3 violations was greater in those who underwent additional surgery, though this difference did not reach statistical significance (7.1% versus 0.88%, p = 0.076). No other patients had symptoms from ASD or required post-operative or remote surgery for other indications.
Discussion
Due to the increasing use of lumbar fusion with pedicle screws, there is concern about the short and long-term complications and consequences of these procedures23-25. Though most of the focus on the complications of pedicle screws is on cortical violation and neurological injury, there is increasing focus of the impact of the top of construct screws on adjacent segment disease (ASD)13, 19, 26. Biomechanical studies show increased intradiscal pressure and facet loading following fusion, accelerating degenerative changes13, 27-29. However, it is also thought that violation of adjacent facet joints by hardware may be a large contributor to post-fusion ASD13, 30. It is therefore important to preserve adjacent facet joints when inserting pedicle screws.
A thorough review of the literature demonstrates that it is unclear whether open or percutaneous pedicle screw placement results in more facet violations. Moshirfar et al. evaluated 204 patients who underwent open screw placement and found that 24% of cases had cranial facet joint violations16. Another study by Shah et al. evaluating facet joint violation during open procedures found violations in 37 of 106 patients (35%)17. The incidence of facet joint violation varies depending on the method of pedicle screw insertion, as a study by Chen et al. revealed a 100% incidence of facet violation using the Roy-Camille method but only 36% when the Weinstein method was used15. A few studies have also evaluated percutaneous pedicle screw placement on facet joint violations. Knox et al. evaluated 61 patients and found 7 patients (11.5%) with superior-level facet violations while a study by Park et al. found a 50% incidence of violations after reviewing 184 pedicle screws (92 cases)18, 19. Also, a cadaveric study performed to evaluate facet violations with percutaneous pedicle screw placement found a 58% incidence of violations after the placement of 28 screws20. Thus, the literature is unclear on which surgical approach results in more facet joint violations, and risk factors that increase the incidence of facet violation are also poorly defined.
Comparison of facet joint violation between open and percutaneous approaches
We describe a direct comparison of the incidence of superior level facet joint violations for percutaneous and open techniques performed at a single institution in surgeons skilled at both procedures. In our series, the overall violation grade (p = 0.018) and incidence of grade 3 violations (p = 0.0059) were significantly higher in those patients who underwent percutaneous pedicle screw placement compared to those in the open group. Additionally, the likelihood of having a high-grade violation with percutaneous placement was significantly higher (OR: 8.55; 95% CI [2.51, 29.14]). We hypothesize that there were was a higher violation grade and greater incidence of grade 3 violations for the percutaneous cases, as these cases rely on radiographic and limited tactile feedback for determination of screw entry site and trajectory. In contrast, the open approach allows for direct visualization of the facet. An incorrect or too medial starting point on the facet joint makes it impossible to avoid getting a higher grade violation. In some cases, it is possible to feel the tools on the transverse process and not on the facet, but certain patient factors could make this maneuver more difficult as described below. Even with perfect fluoroscopic images, a slightly poor choice of entry site or too much medial angulation can result in a violation. The low incidences of grade 1 and 2 violations in this study indicate that experienced surgeons can avoid facet injury with both percutaneous and open approaches. However, the differences in primary outcomes for overall grade and grade 3 violations reflect that certain factors predispose percutaneous cases to facet violation.
Patient factors including age and BMI may contribute to increased difficulty in avoiding the facet with percutaneous cases. For example, patients younger than 65 had a higher incidence of facet violation grade and incidence of grade 3 violations. The likelihood of high grade violations in these patients was significantly higher for percutaneously inserted screws. A possible explanation is that these younger patients have greater skin elasticity, and muscle strength, density and thickness compared to elderly patients31-35. Younger patients also have firmer muscles, as the lower paraspinal muscles undergo fatty replacement in an age-progressive manner31. This stronger tissue may make it more difficult to get the tactile sensation needed to palpate and avoid the facet for an entry site. Also, the increased resistance from the muscle may make it difficult for the surgeon to get appropriate medial angulation of the screw from a properly selected entry site, leading the surgeon to move the entry site more medially starting on the facet. Also, obese patients (BMI>30) had increased violations for percutaneous cases. Obese patients may have poorer quality radiological intra-operative images, which are absolutely important for percutaneous screw placement35, 36. Additionally, the distance from the skin to the spine may be increased in obese patients, therefore increasing the length of the instruments and decreasing tactile sensation for feeling the facet joint and ideal entry site, making appropriate angulation more difficult to achieve. This study reveals the depth of the spine to be an independent risk factor for high grade violations (OR: 1.04; 95% CI [1.02, 1.07]). Traditional open methods avoid these issues by direct tissue dissection and retraction, and exposure of the facet.
Evaluation of operative parameters revealed more facet joint violations in the percutaneous group for screws at L4, and 1-2 level surgeries. More violations at L4 may be due to the typical increased lordosis at this level resulting in greater depth and lower lumbar screw skin incisions being very close to one another if not at same location, limiting ideal screw placement due to the close proximity of the other lower level screw hardware extending out of the skin37. Additionally, patients have a higher prevalence of facet joint arthropathy and hypertrophy at the L3-L4 and L4-5 facets, therefore increasing the risk of facet joint violation with pedicle screw insertion38. A larger facet may be harder to avoid for percutaneous techniques, as it is difficult to get lateral enough to avoid the facet and also try to get appropriate medial angulation to cannulate the pedicle. The percutaneous approach may have had more facet joint violations for 1-2 level surgeries, as these procedures in our population mostly involved pedicle screw insertion at L4 and L5 or the most commonly arthritic levels19, 38. Others have noted difficulty with placement of percutaneous screws at these levels19, 36. With cases with 3 or more instrumented levels, the surgeon could have had a warming up effect and had a better appreciation of the individual's facet anatomy to avoid the top of the construct joint. Additionally, multiple levels permit better incision location selection, allowing easier anatomic localization for screw insertion37.
Examination of pedicle screws inserted by residents only revealed significant differences in open and percutaneous cases involving two surgeons, with no significant differences being found for the entire group. While intuitively it is more challenging to instruct residents using the percutaneous technique, increased facet joint violations were not seen when examining all percutaneous cases. Though this technique heavily relies on tactile feedback to determine the ideal entry site, intraoperative fluoroscopy and surgeon instruction aids in the safe insertion of percutaneous pedicle screws.
Due to the complexities of placing percutaneous pedicle screws, technologies such as intraoperative navigation are of great interest. While many studies have demonstrated more accurate pedicle screw placement during open procedures with the use of computer-assisted image guidance, few studies have examined the utility of this technology in minimally invasive cases39-42. A study by Nakashima et al. compared pedicle screw placement precision with the use of the 3D fluoroscopic method and conventional fluoroscopy43. Of 150 screws implanted using the 3D fluoroscopy-based image guidance, 7.3% were classified as exposed screws, with no cases involving pedicle perforation. However, of 150 screws inserted under conventional fluoroscopy, 12% were exposed and 3.3% perforated the pedicle. Similarly, 3D fluoroscopy has been shown to significantly reduce minimally invasive pedicle screw misplacement and the incidence of electromyography (EMG) warnings compared to using preoperative CT images merged to intraoperative 2-dimensional fluoroscopy44. Further studies are needed to evaluate the use of these technologies for the avoidance of facet joint violations.
Development of Adjacent Segment Disease
As facet joint violation may be a factor for the development of adjacent segment disease, we evaluated the violation grades of those who underwent further lumbar surgery as a result of symptomatic ASD. It was seen that the overall violation grade (p = 0.0016) and the incidence of grade 2 violations (p = 0.0095) were significantly higher in these patients. Though the incidence of grade 3 violations in this group was not statistically significant, it was 8-fold higher compared to those who did not develop ASD. These preliminary results may implicate facet joint violations as a contributor in the development of ASD. However, a multitude of other factors such as the length of the fusion construct may also contribute to the development of ASD. As we did not control for these factors, the exact impact of facet joint violations on this outcome is unclear. Also, the small number of patients with long-term follow-up is inadequate to make conclusive statements regarding the development of ASD in patients with facet joint violations. Additional studies are needed to identify independent predictive factors for ASD.
Grading System for Facet Joint Violation
Several papers categorize different facet violations, but there has not been any consistently used scale that takes into consideration that different types of facet joint violations may differ in severity and contribution to future outcomes. Thus, we used a descriptive grading scheme based on progressive violation of the facet to more accurately document this injury. This new scale differentiates between screws that lie in the lateral facet joint, those that penetrate the facet articulation, and those that travel within the articulation. We hypothesize that greater injury to the articulation would result in greater risk of future adjacent disease. Biomechanical studies show that the nature of each of these facet violations may significantly affect spine biomechanics, as screws placed even in the proximity of the articular surface may cause increases in intradiscal pressure and facet contact force14. The impact of the lower grade violations remains to be determined. We cannot advocate for further use of this scale until it is validated in future studies.
Limitations
A limitation of this study is its retrospective nature and the limits of recall bias and not perfectly matched groups. However, we have tried to minimize these biases by selecting patients with the same indication for lumbar fusion. Additionally, as patients were selected due to the presence of postoperative CT scans, this study was more likely to include and describe patients with poorer outcomes by selecting only patients who had the need for this image modality. However, we show the most common indication for postoperative CT scans to be for routine follow-up as some study surgeons order scans following every fusion procedure. Additionally, our rates of facet violation are similar to those found in the literature. Also, although we suggest that facet joint violations contribute to the development of post-fusion ASD, the small sample size of patients with long term follow-up does not allow for conclusive statements about the role of facet joint violations in this outcome and there are many other factors which may contribute to this effect. As ASD is typically a remote complication, we plan to follow all of the 279 patients (of the current cohort) to 3-5 years, allowing for more conclusive evidence concerning the development of ASD as a possible result of facet joint violation and other factors. Finally, the grading scale used in this study for facet joint violations was developed for descriptive purposes. This scale has not yet been validated and future studies are needed to determine the impact of violations of various grades on outcome. Therefore, the role of lower grade (grade 1 and 2) violations on facet joint damage and subsequent ASD remains unclear.
Conclusion
The results of this study show that percutaneous pedicle screw insertion is associated with a higher incidence of higher grade facet joint violation compared to the traditional open approach. The incidence of facet violation is greater with percutaneous screws in patients who are under the age of 65 and in the obese, and in 1 or 2 level fusion surgeries and ones ending cranially at L4. The depth of the spine is also an independent risk factor for high grade facet violation. As facet joint violation may increase the risk of ASD, it is important to limit or reduce these injuries. This study will help spine surgeons limit this complication by providing knowledge of patient and operative factors with greatest risk. This study also demonstrates that experienced spine surgeons in the techniques of open or percutaneous screw placement are good at avoiding facet injury in the majority of cases with a low incidence of clinically relevant violations.
This is a very interesting paper that highlights some of the technical challenges with placing percutaneous pedicles screws using standard fluoroscopy. The authors demonstrate that higher grade superior facet disruptions occur in percutaneous screw placement as compared to traditional open techniques. Independent risk factors for high grade 3 disruptions include BMI > 30, age < 65, cranial screw placement at L4, increased depth of tissue to the spine, and 2 level percutaneous screw placement. I believe that as spine surgeons, we should look at advanced technologies for instrumentation placement, especially in minimally invasive procedures, such as navigation in reducing superior facet disruption and the incidence of adjacent segment disease and revision surgery. The authors have presented a worthy paper of discussion among the community of spine surgeons as we continue to evolve into more minimally invasive procedures.
Daniel Refai, Atlanta, Georgia
This article reports a retrospectively reviewed cohort of 126 open and 153 percutaneously instrumented lumbar fusion cases by six neurosurgeons. The grades of facet violation of the 558 screws at the upper most level of the constructs were evaluated by post-operative CT scans. Patients undergoing percutaneous procedures and obese patients (BMI>30) who had percutaneous procedures had a higher overall proximal facet violation grade.
The effect of upper facet violation on adjacent segment disease is still unclear. The authors found that among the 57 patients who had at least 3 years follow-up in this study, 7 patients underwent additional lumbar surgery for adjacent level disease and they had a significantly higher overall facet violation grade than those who did not require additional surgeries. As minimally invasive techniques become more widespread, this study reminds surgeons to pay attention to avoid upper facet violation so as to decrease possible adjacent segment disease. More complete long-term follow-up of the entire cohort can further elucidate the impact of upper facet violation on the proximal adjacent segment.
Tsung-Hsi Tu, Praveen Mummaneni, San Francisco, California
Footnotes
Disclosure: The authors have no financial or institutional interest in any of the drugs, materials, or devices described in this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine. 2007;32(5):537–543. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- 2.Stonecipher T, Wright S. Posterior lumbar interbody fusion with facet-screw fixation. Spine. 1989;14(4):468–471. doi: 10.1097/00007632-198904000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Styf JR, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine. 1998;23(3):354–358. doi: 10.1097/00007632-199802010-00014. [DOI] [PubMed] [Google Scholar]
- 4.Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999;24(10):1023–1028. doi: 10.1097/00007632-199905150-00017. [DOI] [PubMed] [Google Scholar]
- 5.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine (Phila Pa 1976) 1996;21(8):941–944. doi: 10.1097/00007632-199604150-00007. [DOI] [PubMed] [Google Scholar]
- 6.Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bunger CE. 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine (Phila Pa 1976) 1997;22(24):2813–2822. doi: 10.1097/00007632-199712150-00004. [DOI] [PubMed] [Google Scholar]
- 7.Rantanen J, Hurme M, Falck B, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine (Phila Pa 1976) 1993;18(5):568–574. doi: 10.1097/00007632-199304000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine. 2009;34(13):1385–1389. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 9.Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. Journal of neurosurgery. 2002;97(1 Suppl):7–12. doi: 10.3171/spi.2002.97.1.0007. [DOI] [PubMed] [Google Scholar]
- 10.Guiot BH, Khoo LT, Fessler RG. A minimally invasive technique for decompression of the lumbar spine. Spine. 2002;27(4):432–438. doi: 10.1097/00007632-200202150-00021. [DOI] [PubMed] [Google Scholar]
- 11.Khoo LT, Palmer S, Laich DT, Fessler RG. Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery. 2002;51(5 Suppl):S166–161. [PubMed] [Google Scholar]
- 12.Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. 2002;49:499–517. [PubMed] [Google Scholar]
- 13.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine. 2004;29(17):1938–1944. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 14.Kim HJ, Chun HJ, Moon SH, et al. The Biomechanical Effect of Pedicle Screws' Insertion Angle and Position on the Superior Adjacent Segment in One Segment Lumbar Fusion. Spine (Phila Pa 1976) 2011 Nov 14; doi: 10.1097/BRS.0b013e31823f2115. [DOI] [PubMed] [Google Scholar]
- 15.Chen Z, Zhao J, Xu H, Liu A, Yuan J, Wang C. Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J. 2008;17(11):1476–1480. doi: 10.1007/s00586-008-0776-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moshirfar A, Jenis LG, Spector LR, et al. Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine (Phila Pa 1976) 2006;31(22):2624–2629. doi: 10.1097/01.brs.0000240691.35707.e8. [DOI] [PubMed] [Google Scholar]
- 17.Shah RR, Mohammed S, Saifuddin A, Taylor BA. Radiologic evaluation of adjacent superior segment facet joint violation following transpedicular instrumentation of the lumbar spine. Spine (Phila Pa 1976) 2003;28(3):272–275. doi: 10.1097/01.BRS.0000042361.93572.74. [DOI] [PubMed] [Google Scholar]
- 18.Park Y, Ha JW, Lee YT, Sung NY. Cranial facet joint violations by percutaneously placed pedicle screws adjacent to a minimally invasive lumbar spinal fusion. Spine J. 2011;11(4):295–302. doi: 10.1016/j.spinee.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Knox JB, Dai JM, 3rd, Orchowski JR. Superior segment facet joint violation and cortical violation after minimally invasive pedicle screw placement. Spine J. 2011;11(3):213–217. doi: 10.1016/j.spinee.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 20.Patel RD, Graziano GP, Vanderhave KL, Patel AA, Gerling MC. Facet Violation with the Placement of Percutaneous Pedicle Screws. Spine (Phila Pa 1976) 2011;36(26):E1749–1752. doi: 10.1097/BRS.0b013e318221a800. [DOI] [PubMed] [Google Scholar]
- 21.Farber GL, Place HM, Mazur RA, Jones DE, Damiano TR. Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine. 1995;20(13):1494–1499. doi: 10.1097/00007632-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Learch TJ, Massie JB, Pathria MN, Ahlgren BA, Garfin SR. Assessment of pedicle screw placement utilizing conventional radiography and computed tomography: a proposed systematic approach to improve accuracy of interpretation. Spine. 2004;29(7):767–773. doi: 10.1097/01.brs.0000112071.69448.a1. [DOI] [PubMed] [Google Scholar]
- 23.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. Jama. 2010;303(13):1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Babu MA, Coumans JV, Carter BS, et al. A review of lumbar spinal instrumentation: evidence and controversy. J Neurol Neurosurg Psychiatry. 2011;82(9):948–951. doi: 10.1136/jnnp.2010.231860. [DOI] [PubMed] [Google Scholar]
- 25.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States' trends and regional variations in lumbar spine surgery: 1992-2003. Spine (Phila Pa 1976) 2006;31(23):2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheh G, Bridwell KH, Lenke LG, et al. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976) 2007;32(20):2253–2257. doi: 10.1097/BRS.0b013e31814b2d8e. [DOI] [PubMed] [Google Scholar]
- 27.Guigui P, Wodecki P, Bizot P, Lambert P, Chaumeil G, Deburge A. Long-term influence of associated arthrodesis on adjacent segments in the treatment of lumbar stenosis: a series of 127 cases with 9-year follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(6):546–557. [PubMed] [Google Scholar]
- 28.Hambly MF, Wiltse LL, Raghavan N, Schneiderman G, Koenig C. The transition zone above a lumbosacral fusion. Spine (Phila Pa 1976) 1998;23(16):1785–1792. doi: 10.1097/00007632-199808150-00012. [DOI] [PubMed] [Google Scholar]
- 29.Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K. Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine. 2000;25(14):1837–1842. doi: 10.1097/00007632-200007150-00016. [DOI] [PubMed] [Google Scholar]
- 30.Krag MH. Biomechanics of thoracolumbar spinal fixation. A review. Spine (Phila Pa 1976) 1991;16(3 Suppl):S84–99. doi: 10.1097/00007632-199103001-00014. [DOI] [PubMed] [Google Scholar]
- 31.Hadar H, Gadoth N, Heifetz M. Fatty replacement of lower paraspinal muscles: normal and neuromuscular disorders. AJR Am J Roentgenol. 1983;141(5):895–898. doi: 10.2214/ajr.141.5.895. [DOI] [PubMed] [Google Scholar]
- 32.Parkkola R, Kormano M. Lumbar disc and back muscle degeneration on MRI: correlation to age and body mass. J Spinal Disord. 1992;5(1):86–92. doi: 10.1097/00002517-199203000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Osanai O, Ohtsuka M, Hotta M, Kitaharai T, Takema Y. A new method for the visualization and quantification of internal skin elasticity by ultrasound imaging. Skin Res Technol. 2011 Feb 23; doi: 10.1111/j.1600-0846.2010.00492.x. [DOI] [PubMed] [Google Scholar]
- 34.Gerhardt LC, Lenz A, Spencer ND, Munzer T, Derler S. Skin-textile friction and skin elasticity in young and aged persons. Skin Res Technol. 2009;15(3):288–298. doi: 10.1111/j.1600-0846.2009.00363.x. [DOI] [PubMed] [Google Scholar]
- 35.Kim MC, Chung HT, Cho JL, Kim DJ, Chung NS. Factors affecting the accurate placement of percutaneous pedicle screws during minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2011;20(10):1635–1643. doi: 10.1007/s00586-011-1892-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park Y, Ha JW, Lee YT, Sung NY. Percutaneous placement of pedicle screws in overweight and obese patients. Spine J. 2011;11(10):919–924. doi: 10.1016/j.spinee.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 37.Mobbs RJ, Sivabalan P, Li J. Technique, challenges and indications for percutaneous pedicle screw fixation. J Clin Neurosci. 2011;18(6):741–749. doi: 10.1016/j.jocn.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 38.Abbas J, Hamoud K, Peleg S, et al. Facet joints arthrosis in normal and stenotic lumbar spines. Spine (Phila Pa 1976) 2011;36(24):E1541–1546. doi: 10.1097/BRS.0b013e318210c889. [DOI] [PubMed] [Google Scholar]
- 39.Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. European spine journal. 2000;9(3):235–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Merloz P, Tonetti J, Pittet L, Coulomb M, Lavallee S, Sautot P. Pedicle screw placement using image guided techniques. Clinical orthopaedics and related research. 1998(354):39–48. doi: 10.1097/00003086-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Rajasekaran S, Vidyadhara S, Ramesh P, Shetty AP. Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine (Phila Pa 1976) 2007;32(2):E56–64. doi: 10.1097/01.brs.0000252094.64857.ab. [DOI] [PubMed] [Google Scholar]
- 42.Amiot LP, Lang K, Putzier M, Zippel H, Labelle H. Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine (Phila Pa 1976) 2000;25(5):606–614. doi: 10.1097/00007632-200003010-00012. [DOI] [PubMed] [Google Scholar]
- 43.Nakashima H, Sato K, Ando T, Inoh H, Nakamura H. Comparison of the percutaneous screw placement precision of isocentric C-arm 3-dimensional fluoroscopy-navigated pedicle screw implantation and conventional fluoroscopy method with minimally invasive surgery. Journal of spinal disorders & techniques. 2009;22(7):468–472. doi: 10.1097/BSD.0b013e31819877c8. [DOI] [PubMed] [Google Scholar]
- 44.Wood M, Mannion R. A comparison of CT-based navigation techniques for minimally invasive lumbar pedicle screw placement. Journal of spinal disorders & techniques. 2011;24(1):E1–5. doi: 10.1097/BSD.0b013e3181d534b8. [DOI] [PubMed] [Google Scholar]