Abstract
Preparing medical students to prescribe is a major challenge of undergraduate education. They must develop an understanding of clinical pharmacology and acquire knowledge about drugs and therapeutics, as well as the skills to prescribe for individual patients in the face of multiple variables. The task of delivering the learning required to achieve these attributes relies upon limited numbers of teachers, who have increasingly busy clinical commitments. There is evidence that training is currently insufficient to meet the demands of the workplace. e-Learning provides an opportunity to improve the learning experience. The advantages for teachers are improved distribution of learning content, ease of update, standardization and tracking of learner activities. The advantages for learners are ease of access, greater interactivity and individual choice concerning the pace and mix of learning. Important disadvantages are the considerable resource required to develop e-Learning projects and difficulties in simulating some aspects of the real world prescribing experience. Pre-requisites for developing an e-Learning programme to support prescribing include academic expertise, institutional support, learning technology services and an effective virtual learning environment. e-Learning content might range from complex interactive learning sessions through to static web pages with links. It is now possible to simulate and provide feedback on prescribing decisions and this will improve with advances in virtual reality. Other content might include a student formulary, self-assessment exercises (e.g. calculations), a glossary and an on-line library. There is some evidence for the effectiveness of e-Learning but better research is required into its potential impact on prescribing.
Keywords: education, e-Learning, medical student, patient safety, prescribing, prescribing errors
Introduction
Prescribing is the major intervention that most doctors make to restore or preserve the health of their patients and is the major tool used by most advanced healthcare systems to improve public health. Prescribing also carries risk: there is ample evidence that injudicious prescribing harms the health of a significant minority of patients [1, 2] and that prescribing errors are frequent [3, 4]. Perhaps we should not be surprised that error is common because prescribing is a complex task requiring diagnostic skills, knowledge of medicines, communication skills, an understanding of the principles of clinical pharmacology, appreciation of risk and uncertainty and experience. It is also apparent that prescribers face progressive demands due to important trends including (i) more licensed medicines available, (ii) increasing indications for drug treatment, (iii) greater complexity of treatment regimens leading to ‘polypharmacy’ and (iv) more elderly and vulnerable patients.
For these reasons, providing the training that will allow new doctors to be better prepared to assume their responsibilities as prescribers is arguably the greatest challenge in modern undergraduate medical education. Several independent reports have suggested that improvements need to be made [3, 5–7]. However, delivering improved education in clinical pharmacology and therapeutics (CPT), the discipline that underpins safe and effective prescribing, presents difficulties because:
CPT is a knowledge-rich discipline (e.g. large numbers of drugs) at a time of unprecedented curriculum overload
Best practice in prescribing changes continually as new evidence emerges
Prescribing is a high risk area of clinical practice, making acquisition of practical experience and training problematic
CPT appears throughout the curriculum, complicating the delivery of an integrated and consistent learning pathway
Prescribing integrates knowledge, understanding, skills and judgement
There is a shortage of specialists combining a firm grounding in CPT with prescribing experience and an interest in teaching.
All of these factors have stimulated interest in e-Learning as a solution. The aim of this review is to: (i) discuss how e-Learning can contribute to prescribing education, (ii) identify its advantages and disadvantages and (iii) highlight some examples. We focus on the training of medical students, although the issues discussed are also relevant to those from other professional backgrounds who are learning to prescribe and those who are in postgraduate education. We consider prescribing education to embrace the four domains of the British Pharmacological Society curriculum – the principles of clinical pharmacology, knowledge of the effects and use of drugs, how drugs are applied to the treatment of diseases (therapeutics) and the skills and judgement involved in writing and reviewing prescriptions [8].
What is e-Learning?
The term e-Learning is used in its widest sense to describe all forms of electronically supported learning and teaching. In the modern era it is normally used in relation to electronic support provided by computers, either working in isolation or, more commonly, connected to a network. The learning materials may be provided from within the learners' own educational institution or delivered from other sources on the Internet. e-Learning is a relatively new approach to medical education but is rapidly growing with the increasing availability and portability of computers.
It is worth noting that the mere association of e-Learning with a computer does not mean that the learning process is novel or even an improvement. At its most basic, e-Learning may involve transfer of static pages of text and pictures from a book to web pages (e-Book) or delivery over the Internet of a seminar that might have been delivered face-to-face (e-Seminar). In these situations, e-Learning is merely replicating long-established pedagogical approaches but opens up new possibilities in terms of flexibility for teacher and learner. However, at its most developed, e-Learning can provide new learning opportunities that were simply not possible in the pre-computer age. Examples include user-controlled animations, self-assessment exercises with feedback, on-demand video streaming and podcasts and simulations of real-life events in virtual reality.
The breadth of e-Learning possibilities can be classified sequentially into static content, facilitated learning, partial interactivity and complete virtual reality. Table 1 provides some examples of each in relation to prescribing education. Table 2 lists and defines some common terms and definitions relating to e-Learning.
Table 1.
Classification of e-Learning strategies to support prescribing education
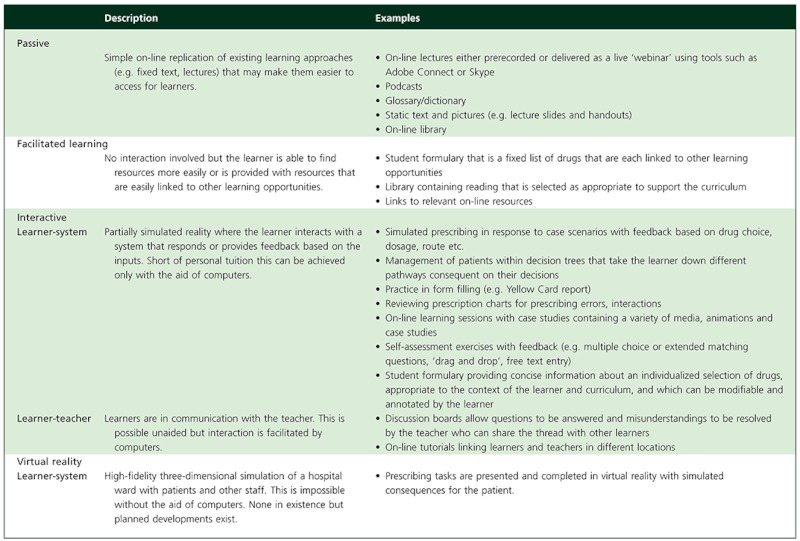 |
Table 2.
Definitions of some common terms related to e-Learning
| e-Learning. Learning and teaching that is computer-based and usually self-paced, and happens at a time and location of the learner's choosing, rather than as a single event at a fixed time provided by the teaching institution. |
| Learning objects (LOs). A unit of learning content that lasts a few minutes for the learner, containing content in the form of text, image, animation, streaming video or audio. LOs are usually self-contained packages of learning that have a clear educational purpose and can be undertaken independently from other learning content. LOs are often reusable in different contexts for multiple learning purposes. LOs can be aggregated into larger collections of content that might form traditional course structures. LOs are tagged with metadata to facilitate their identification, storage and retrieval. A free worldwide repository for learning objects is available at http://www.merlot.org. |
| Metadata. The data used to describe or ‘tag’ LOs so that they can be identified by search engines or learning management systems. Metadata will typically include the learning objectives, the pre-requisites that the learner must have before undertaking the learning object, the learning topic and its place in the curriculum, language, descriptive text, version, instructional content (e.g. text, web pages, images, animation, audio, video), the level of interactivity required of the learner and any technical requirements to view it. |
| Virtual Learning Environment (VLE). A system designed to support e-Learning that enables learners to access learning content through a single, consistent, and intuitive interface. It usually requires learners to identify themselves at login so that their usage and performance can be monitored, their optimal learning pathway (curriculum) and assessments can be signposted, any earned credits recorded, and access rights controlled. The VLE will normally provide interactive LOs organized into modules and courses, reference resources, access to an on-line library, links to outside learning resources, self-assessments, podcasts (series of digital media files that are released episodically and often downloaded through web syndication), wikis (collections of articles that multiple users can add to and edit freely on-line), blogs (web logs; web site entries that are updated with new content from time to time), questionnaires and discussion boards. |
| Blended learning. A mixture of traditional lectures, tutorials, practical and clinical activities with e-Learning approaches (e.g. a lecture is supplemented by an on-line tutorial). |
| Learning Management System (LMS). A similar concept to a VLE but with a greater emphasis on management of the learning process. The LMS will record learner activities and might serve to enforce specific learning pathways and ensure they are completed before progression. Common examples include Moodle, ctools and Blackboard. |
| Sharable Content Object Reference Model (SCORM). A collection of standards and specifications for web-based e-Learning that have been created to maximize the compatibility of LOs with host VLEs and LMSs. |
What are the advantages of e-Learning?
e-Learning has potential advantages over traditional live or real learning environments in terms of both the delivery of the learning by teaching institutions and the experience and outcomes for the learners (Table 3).
Table 3.
The advantages and disadvantages of e-Learning as an educational approach
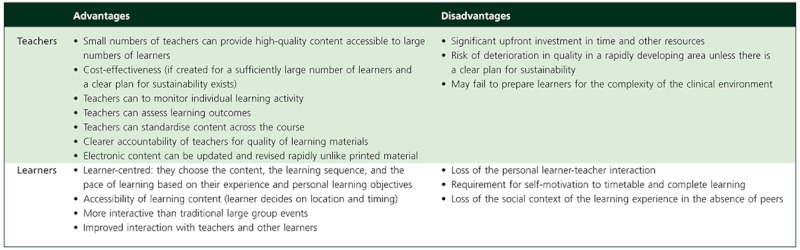 |
Teachers are attracted to e-Learning by the opportunity to enhance the accessibility of their learning material. No longer are they restricted to brief events in a crowded educational timetable but can make material constantly available to users anywhere in the world. This is a particularly attractive proposition for clinical pharmacologists, who are few in number but are often charged with delivering a large part of the curriculum. Teachers are also able to update and amend content at any time and can signpost those changes or highlight the appearance of new material. This responsiveness to the needs and wishes of learners is particularly attractive for prescribing education, which evolves more rapidly than other areas in the medical curriculum. Careful use of templates allows better standardization of the content, providing a more coherent feel to the learning process than is possible in standard lecture courses. A learning management system (LMS) makes it possible to monitor the access and progress of learners through the content, as well as assessing their acquisition of knowledge to ensure that learning has occurred. It also makes teachers more accountable for their material, which is scrutinized during the learning process and can be instantly rated. All of these features can help to reduce the overall administrative burden of course delivery. Teachers and their institutions might also see e-Learning as a cost-effective option, although this depends on the numbers of learners and a plan for sustainability of the material. It may also be increasingly the only practical solution as medical education is devolved progressively from major academic centre venues to primary care.
Learners are attracted to e-Learning because it puts them at the centre of the learning process. Rather than being passive recipients during educational events, they can choose the content that they access, the order in which it is tackled, and the pace of the learning based on their experience and personal learning objectives. The content is readily accessible so they can choose the location and timing of the learning to suit their personal commitments. A good quality e-Learning experience may also provide the learner with more personal interaction than is normally possible at a traditional large group event. The LMS should also mean that learners have improved access to teachers and are less isolated from other learners. The clearly visible structure and organization of an e-Learning course may also be better suited to the achievement of the learning outcomes identified in modern competency-based education.
What are the disadvantages of e-Learning?
There are some important disadvantages that are worth considering (Table 3). While e-Learning provides an excellent route for the delivery of knowledge of the principles of clinical pharmacology, drugs and therapeutics, it may be less able to provide the practical training required to prescribe. This involves making judgements based not only on knowledge but also the nuances and uncertainties that are inherent in real clinical practice. Nevertheless, it seems likely that some of these hurdles will be overcome if virtual environments are able to simulate the reality of the workplace. Although e-Learning has the potential to be cost-effective, the up-front investment is considerable in terms of time and resources and can be justified only if there is a clear plan for sustainability. Many e-Learning efforts end in failure because the time commitment for maintenance is underestimated. A final but important disadvantage is the absence of the clinical role model or mentor, which remains a valuable part of medical education.
How can we create good e-Learning to support prescribing education?
There are several pre-requisites for developing a successful e-Learning programme to support education in CPT and prescribing. These include:
Academic expertise. Prescribing (including clinical pharmacology) represents a large proportion of the medical curriculum and some medical schools may not have sufficient expertise to provide the breadth of materials required. For that reason, regional and national collaboration is probably the optimal approach to building a high quality resource and several examples now exist [9–11]. In addition to knowledge, content authors will need enthusiasm, imagination and an ability to perceive the learning challenge from the student's perspective.
Time and institutional support. The initial investment in time and effort to create good e-Learning materials is considerable and represents much more than converting PowerPoint presentations to web pages. To be able to do this the academic experts will require time and recognition of the importance of the work.
Virtual learning environment (VLE). Any e-Learning content must be accessible to learners and this will normally require an institutional VLE with authenticated access that serves as a conduit to the materials. This may include a formal LMS that controls the order of access, and records the completion of learning and the results of any assessments.
Learning technology services. Few academics will possess the necessary expertise to create and then ‘platform’ the learning materials. They will usually provide text and pictures within a pre-specified template, which is then transformed into an interactive e-Learning session by an instructional designer, sometimes with the help of a graphic designer. The programming team will then ensure that the final content is uploaded and provide technical support for users.
Curriculum. The essence of good e-Learning is that it is planned and logical, and based around clear learning outcomes. These determine the learning content, the order in which it is taken and the assessments that are provided. For this reason it is necessary to have an agreed curriculum that is broken down into a logical hierarchy. The British Pharmacological Society has published such guidance [8], which underpins the organization of Prescribe, its e-Learning initiative (Figure 1) [9].
Figure 1.
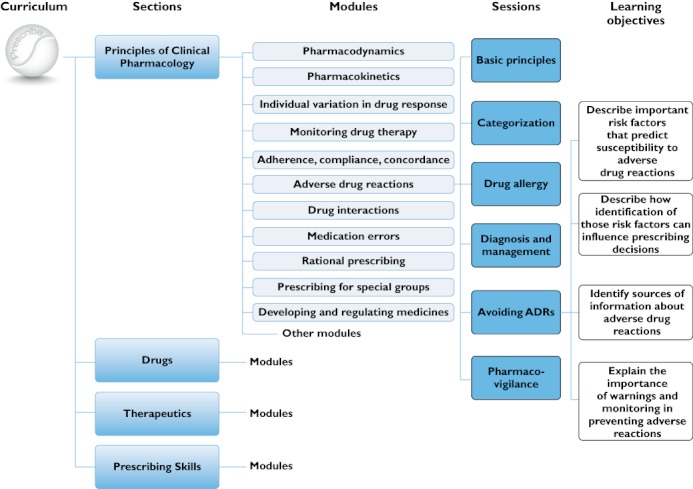
The breakdown of the Prescribe e-Learning programme (based on the British Pharmacological Society curriculum) into sections, modules, learning sessions and individual learning objectives
What e-Learning content would support prescribing education?
The content of an e-Learning programme for prescribing might include a mixture of traditional interactive e-Learning sessions with other supporting activities.
e-Learning sessions. These will normally be relatively brief interactive learning activities lasting for around 20–30 min to avoid exceeding the learner's attention span. Each will contain one or two ‘learning objects’ that tackle a small number of clearly defined learning objectives. They will normally be voluntary, so they must compete for the learner's attention. To secure this, the authors must provide material that is pitched at a level commensurate with existing knowledge and relevant to the learning needs identified by the curriculum. A good session will highlight the learning objectives it will address and any prior learning that is required (Figure 2). The quality of the subsequent learning experience will then be influenced by the factual accuracy of the content, the clarity of the text and layout (instructional design), how well the illustrations complement the text and facilitate understanding (graphic design), the amount of interactivity and the ease of navigation (Figure 3). The temptation to use all the possibilities of modern computing should be avoided as the novelty soon wears off and gratuitous use of multimedia can distract attention. In addition to the learning content, sessions should also contain ‘knowledge checks’ that ensure learners are acquiring important knowledge (e.g. pharmacokinetic handling of a drug), and case studies that allow them to use that knowledge to solve simulated clinical problems (e.g. identifying the likely cause of an adverse drug reaction). Sessions will normally end with a summary of key learning points and links to further learning activities. Finally, a valuable part of any e-Learning system is a simple way for learners to provide feedback; it fosters learner engagement and quickly identifies weaknesses and opportunities for improvement. The end result should ideally be a learning environment that users want to (rather than have to) access.
Figure 2.
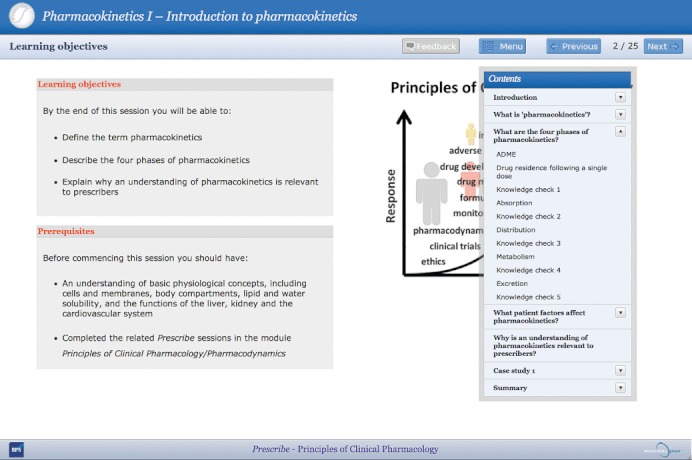
The beginning of a learning session in Prescribe. Note the clearly stated learning objectives and prerequisites, the simple navigation buttons and drop down menu allowing learners to navigate easily around the session and return to specific pages, the regular knowledge checks to assess uptake of the content, the case study to contextualize the learning and the feedback button allowing learners to provide page-specific feedback
Figure 3.
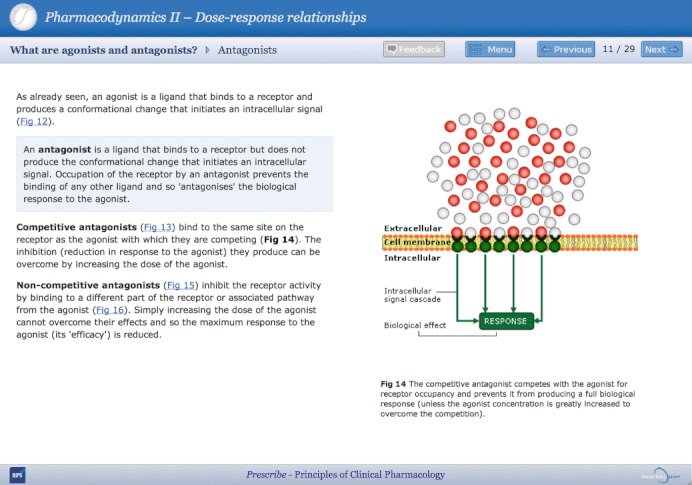
A content page from a Prescribe learning page. e-Learning content pages should avoid overload with factual information and be supplemented with simple illustrations or animations that make potentially complicated scientific principles accessible to the learner
Other areas of interactive e-Learning content to support prescribing might be:
Student formulary. The use of a student formulary has been advocated as a means of trying to focus learning around a core list of 80 to 100 drugs that are in common use and might act as exemplars for other drugs [12–14]. The intention is to avoid information overload and set realistic goals for students. While this list might be presented as a simple list of drugs, the concept offers opportunities to provide an interactive e-Learning tool [15]. Rather than a simple factual list the formulary entries might include information written with learners in mind, reinforcing common pharmacological principles where possible and linking to other resources. Its purpose is to support learning rather than be a reference resource for prescribing. In keeping with the principles of the WHO curriculum, students might be encouraged actively to develop their own formulary of personal or ‘P-drugs’ as the course progresses [16]. Students might also take responsibility for making amendments, allowing the formulary to serve as a wiki.
Prescribing skills. Practical prescribing skills have traditionally been learnt in an ad hoc way during clinical attachments but it is evident from recent surveys that this approach has, in some cases, provided very little or poor quality experience [3, 5–7]. The gap between student apprentice prescribing and early postgraduate prescribing is still far too great. e-Learning provides the potential to ease this transition and provide more of the ‘learning curve’ within the undergraduate curriculum. There are now some programmes available that allow prescriptions to be written in a virtual environment with rapid scoring and feedback provided (Figure 4). The fidelity of these simulations is likely to improve and they have the advantages of requiring no specific organization of the clinical environment and posing no potential risk to patients.
Calculation skills. The ability to perform calculations is important for only a minority of prescriptions but the consequences of error can be particularly serious. On-line practice is easy to deliver and has been shown to be a valuable tool for improving dose calculation skills [17].
Other skills. On-line environments might offer the opportunity to practise filling in common documentation related to medicines, including Yellow Card reports and medication error reports. It is also possible to present prescription charts for review or data requiring interpretation (e.g. paracetamol concentrations).
Self-assessment. Students value self-assessment highly and we advocate including ‘knowledge checks’ in all on-line learning sessions as a means of keeping their attention. However, it is also helpful to pose formative self-assessment exercises with feedback as a means of checking comprehension as well as recall; this directs and reinforces learning as well as allowing students and teachers to assess progression [18].
Discussion boards. Discussion boards or chat rooms are a simple means of tackling learner misperceptions for the benefit of all, as well as stimulating active discussion and collaborative exploration of learning topics. They also help educators to reflect on and improve their own teaching.
Figure 4.
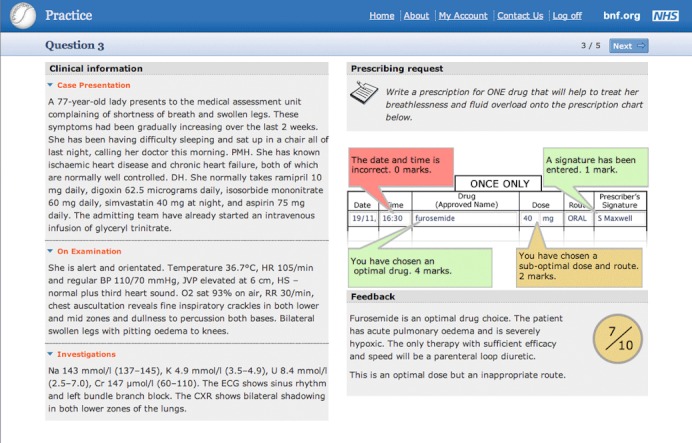
A simulated prescribing exercise with feedback. Learners are presented with clinical information and a clear prescribing request. After entering and submitting a prescription they are given a score and targeted feedback
An e-Learning programme to support prescribing might also contain other less interactive resources that would support the overall learning programme. These include:
Streamed lectures, tutorials and podcasts. These might be events provided by the host institution or those produced by others. It is also possible to use modern technologies to provide live broadcasts of lectures or ‘face-to-face’ tutorials.
Resources. This might include a library containing materials such as guideline documents, papers, slides and handouts supporting the teaching programme.
Glossary. This might comprise a list of definitions of key terms relevant to prescribing.
Links to other materials. Hyperlinks to other materials that provide the background to learning with a brief description to alert the learner to their utility. These might include national and local formularies, drug databases and other e-Learning materials.
Where does e-Learning fit into the wider learning programme?
We believe that, although e-Learning has an important contribution to make to prescribing education, it should form part of a blended learning solution that also includes lectures and tutorials, as well as many hours spent in clinical environments where real prescriptions are written and reviewed. e-Learning can provide excellent background preparation but all trainee prescribers should have regular experience of making prescribing decisions based on real clinical encounters and writing prescriptions using relevant documentation. They should also take all opportunities to review and reflect on prescriptions for medicines that patients are already taking.
It is obvious that the scale of an e-Learning programme should not be out of proportion to the time available or the overall curriculum content. Learners are already overloaded by access to numerous large educational resources. The essence of a good programme is provision of a coherent, manageable, stimulating and realistic experience that is tied to the curriculum learning outcomes.
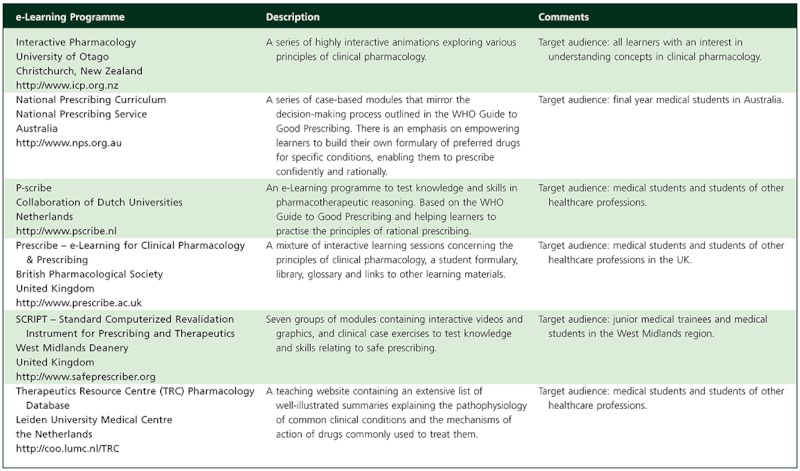
What examples of e-Learning for prescribers exist?
The pressing need for more support for education in clinical pharmacology and prescribing, combined with technological advances and the growth of the Internet, has led to the creation of several e-Learning collections. These cover various aspects of pharmacology, clinical pharmacology and preparation for prescribing and some are listed in Table 4.
Table 4.
Examples of e-Learning resources relevant to clinical pharmacology and prescribing
 |
Will e-Learning deliver better prescribers?
The major potential investment of resource requires us consider whether e-Learning is an effective educational strategy. Evaluation can be conveniently divided into two basic domains: the quality of the e-Learning experience and the outcomes that it produces. The former is a more subjective judgement made on the basis of the academic credibility of the content, its layout and relevance to the intended learning outcomes, the quality assurance, the ease of navigation, the use of multimedia elements, the interactivity of the experience, the requirements for computing skills or specific software and the accessibility of the content for the intended user groups. These parameters can be judged by academic experts (e.g. clinical pharmacologists), who will focus on the validity of the content, but also by learners (e.g. medical students), who will be more interested in the learning experience and accessibility. However, the subjective satisfaction of either group is not a guarantee of successful learning. A course may be full of excellent content but be rated poorly by users. Conversely, a course that is highly entertaining in its use of interactive graphics but superficial in its content may be rated highly.
e-Learning might be judged more objectively by examining the outcomes in terms of knowledge acquisition (e.g. drugs), skills (e.g. ability to write a prescription) and attitudes or behaviours that it produces. These can be assessed within the content and by other self-assessment exercises that are placed within the LMS. However, these assessments tend to focus on short term gains and are often not externally valid in the workplace. The true test of any educational resource in CPT or prescribing will be whether its benefits translate into fewer adverse drug reactions and prescribing errors and better patient outcomes. Unfortunately, it will be difficult to deliver this evidence because any study would be time consuming, costly and complicated. The numerous confounding factors in real-life practice and the complexity of identifying and judging the endpoints have tended to restrict evaluations to short term follow-up in controlled conditions. The increasing move to electronic prescribing in hospitals will make it easier in the future to follow learners from the educational to the clinical environment.
There are some theoretical reasons for optimism. Good e-Learning supports ‘adult learning theory’[19], which suggests that effective learning is an active experience requiring motivation, organization, self-direction and interaction, and one that should be focused upon the active learner rather than the teacher. Active learners will engage more effectively with the content and maintain their interest and motivation [20]. e-Learners have been shown to have retention rates at least equivalent to traditional learners and the process itself is more cost-effective [21, 22]. A recent survey suggested that around half of UK medical schools currently employ an identifiable e-Learning strategy to support prescribing education [23]. We believe that more will take advantage of this mode of learning in the future with uptake being supported by the emergence of a coupled online assessment in the form of the new national Prescribing Skills Assessment [18].
How will e-Learning be used in the future?
We believe that the influence of e-Learning will continue to grow because of the increasingly crowded curriculum and the progressively improving virtual reality environment, and that it will revolutionize the preparation of undergraduates to become prescribers because of its cost-effectiveness (if done on a collaborative national scale). However, compared with traditional education, e-Learning requires a different set of teaching competencies (teachers function as facilitators of learning rather than lecturers) and institutions need to foster these. In our experience, writing a good e-Learning session takes many more hours of endeavour and planning than creating a traditional lecture and draws on many more skills. The commitment to e-Learning will need to be recognized and rewarded as scholarship within academia. This might be through publication of e-Learning materials in a national on-line peer-reviewed repository, user feedback, peer-reviewed publications and membership of learned groupings.
e-Learning will increasingly deliver an individualized educational experience (adaptive learning) [24] rather than the extremes of one-size fits all or totally self-directed learning. The learning environment will be able to track performance (e.g. prescribing in renal impairment) and provide personalized learning content that matches it. Each learner will have a unique learning experience that identifies their needs and uses their time most efficiently. e-Learning will also provide greater opportunities to create networks of learners (collaborative learning) using technologies such as weblogs, message boards, chats, e-mail and teleconferencing [25]. These will have advantages as medical education is moved further from academic centres towards primary care and will empower education in more disadvantaged countries.
Advances in computer technology will increasingly allow more sophisticated virtual environments to be made available on standard personal computers [26]. Such technologies are already delivering popular online games (e.g. Second Life) and will, in the future, provide high-fidelity simulations of patient encounters in clinical practice [27], including prescribing.
Conclusions
Educating medical students to prescribe safely and effectively is a major challenge in modern medical education. Clinical pharmacology, the traditional discipline underpinning rational prescribing, is less visible in some curricula and training to prescribe and supervise medicines use is suboptimal. e-Learning has the potential to address some of these issues, especially when combined with traditional teacher-led activities. e-Learning may have a particular role in explaining complicated concepts in clinical pharmacology, improving knowledge via student formularies, enhancing therapeutic decision making and providing simulated prescribing exercises. Although the initial investment is significant, if done collaboratively it should be cost-effective, stimulating and highly appreciated by students. There remain unanswered questions about the effectiveness of e-Learning in prescribing education and these must await further evaluation.
Competing Interests
SM was supported by the Department of Health for the Prescribe project in its early stages and continues to develop and edit educational material for this e-Learning initiative. JM was employed by the Department of Health as a module editor for the Prescribe project in its early stages and continues to develop and edit educational material for this e-Learning initiative for the British Pharmacological Society, by whom he is paid a fee as a consultant.
Acknowledgments
The resources illustrated in Figures 2 to 4 were developed with the support of the UK Department of Health.
REFERENCES
- 1.National Patient Safety Agency. National Reporting and Learning Systems. 2012. Quarterly data summaries. Available at http://www.nrls.npsa.nhs.uk/resources/collections/quarterly-data-summaries/ (last accessed 13 May 2012)
- 2.Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. Br Med J. 2004;329:15–9. doi: 10.1136/bmj.329.7456.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.EQUIP Dornan T, Ashcroft D, Heathfield H, Lewis P, Miles J, Taylor D, Tully M, Wass V. An in-depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education: EQUIP study. Final report to the General Medical Council. University of Manchester: School of Pharmacy and Pharmaceutical Sciences and School of Medicine. 2009. Available at: http://www.pharmacy.manchester.ac.uk/cip/CIPPublications/commissionedreports/prescribing_errors_prevalence_incidence.pdf (last accessed 16 May 2012)
- 4.Ryan C, Davey P, Francis J, Johnston M, Ker J, Lee AJ, MacLeod MJ, Maxwell S, McKay G, McLay J, Ross S, Webb D, Bond C. The prevalence of prescribing errors amongst junior doctors in Scotland. Basic Clin Pharmacol Toxicol. 2011;109:35. [Google Scholar]
- 5.Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, Davies C, Baldauf B, Allen M, Johnson N, Morrison J, Donaldson M, Whitelaw M, Field M. How prepared are medical graduates to begin practice? A comparison of three diverse UK medical schools. Final summary and conclusions for the GMC Education Committee, 15th December 2008. Available at http://www.gmc-uk.org/about/research/research_commissioned.asp (last accessed 16 May 2012)
- 6.Skills for Health. Bristol: Skills for Health; 2009. Junior Doctors in the NHS: Preparing Medical Students for Employment and Post-Graduate Training. [Google Scholar]
- 7.Heaton A, Webb DJ, Maxwell SR. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008;66:128–34. doi: 10.1111/j.1365-2125.2008.03197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross S, Maxwell SRJ. Prescribing and the core curriculum for tomorrow's doctors: BPS Curriculum in Clinical Pharmacology and Prescribing for Medical Students. Br J Clin Pharmacol. 2012 doi: 10.1111/j.1365-2125.2012.04186.x. in this edition [if accepted] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.British Pharmacological Society. Prescribe: eLearning in Clinical Pharmacology and Prescribing. Available at http://www.prescribe.ac.uk (last accessed 16 May 2012)
- 10.Smith A, Tasioulas T, Cockayne N, Misan G, Walker G, Quick G. Construction and evaluation of a web-based interactive prescribing curriculum for senior medical students. Br J Clin Pharmacol. 2006;62:653–9. doi: 10.1111/j.1365-2125.2006.02651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franson KL, Dubois EA, de Kam ML, Cohen AF. Measuring learning from the TRC pharmacology E-Learning program. Br J Clin Pharmacol. 2008;66:135–41. doi: 10.1111/j.1365-2125.2008.03167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maxwell S, Walley T. Teaching safe and effective prescribing in UK medical schools: a core curriculum for tomorrow's doctors. Br J Clin Pharmacol. 2003;55:496–503. doi: 10.1046/j.1365-2125.2003.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Safe Prescribing Working Group. Outcomes of the Medical Schools Council Safe Prescribing Working Group. 2008. Available at http://www.medschools.ac.uk/AboutUs/Projects/Documents/Outcomes%20of%20the%20Medical%20Schools%20Council%20Safe%20Prescribing%20Working%20Group.pdf (last accessed 16 May 2012)
- 14.Baker E, Pryce Roberts A, Wilde K, Walton H, Suri S, Rull G, Webb A. Development of a core drug list towards improving prescribing education and reducing errors in the UK. Br J Clin Pharmacol. 2011;71:190–8. doi: 10.1111/j.1365-2125.2010.03823.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maxwell SRJ, McQueen DS, Ellaway R. eDrug: a dynamic interactive electronic drug formulary for medical students. Br J Clin Pharmacol. 2006;62:673–81. doi: 10.1111/j.1365-2125.2006.02777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Vries TPGM, Henning RH, Hogerzeil HV, Fresle DA. Guide to Good Prescribing – A Practical Manual. Geneva: World Health Organization; 1994. [Google Scholar]
- 17.McQueen DS, Begg MJ, Maxwell SRJ. eDrugCalc: an on-line self-assessment package to enhance medical students' drug dose calculation skills. Br J Clin Pharmacol. 2010;70:492–9. doi: 10.1111/j.1365-2125.2010.03609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mucklow J, Bollington L, Maxwell S. Assessing prescribing competence. Br J Clin Pharmacol. 2012 doi: 10.1111/j.1365-2125.2011.04151.x. (doi: 10.1111/j.1365-2125.2011.04151.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knowles M. In: The Modern Practice of Adult Education. From Pedagogy to Andragogy. 2nd edn. Prentice Hall/Cambridge: Englewood Cliffs; 1980. [Google Scholar]
- 20.Clark D. Psychological myths in e-learning. Med Teach. 2002;24:598–604. doi: 10.1080/0142159021000063916. [DOI] [PubMed] [Google Scholar]
- 21.Smith SF, Roberts NJ, Partridge MR. Comparison of a web-based package with tutor-based methods of teaching respiratory medicine: subjective and objective evaluations. BMC Med Educ. 2007;7:41. doi: 10.1186/1472-6920-7-41. doi: 10.1186/1472-6920-7-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chumley-Jones HS, Dobbie A, Alford CL. Web-based learning: sound educational method or hype? A review of the evaluation literature. Acad Med. 2002;77(Suppl.):S86–S93. doi: 10.1097/00001888-200210001-00028. [DOI] [PubMed] [Google Scholar]
- 23.O'Shaughnessy L, Haq I, Maxwell A, Llewelyn M. Teaching of clinical pharmacology and therapeutics in UK medical schools: current status in 2009. Br J Clin Pharmacol. 2010;70:143–8. doi: 10.1111/j.1365-2125.2010.03665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piemme TE. Computer-assisted learning and evaluation in medicine. JAMA. 1988;260:367–72. [PubMed] [Google Scholar]
- 25.Wiecha J, Barrie N. Collaborative online learning: a new approach to distance CME. Acad Med. 2002;77:928–29. [PubMed] [Google Scholar]
- 26.De Ponti R, Marazzi R, Ghiringhelli S, Salerno-Uriarte JA, Calkins H, Cheng A. Superiority of simulator-based training compared with conventional training methodologies in the performance of transseptal catheterization. J Am Coll Cardiol. 2011;58:359–63. doi: 10.1016/j.jacc.2011.02.063. [DOI] [PubMed] [Google Scholar]
- 27.Wilkerson W, Avstreih D, Gruppen L, Beier KP, Woolliscroft J. Using immersive simulation for training first responders for mass casualty incidents. Acad Emerg Med. 2008;15:1152–9. doi: 10.1111/j.1553-2712.2008.00223.x. [DOI] [PubMed] [Google Scholar]


