Abstract
We report our experience of technique of V-Y-plasty in treatment of pilonidal sinus. A retrospective study of 25 patients performed from 2005 to 2010 at Deenanath Mangeshkar Hospital and Sassoon General Hospitals, Pune, was performed. The unilateral or bilateral V-Y advancement flap technique was used in the management of these patients. The outcome was assessed on the basis of efficacy of flap surgery in achieving wound healing and recurrence. The follow-up ranged from 6 months to 5 years. The study included 25 cases of pilonidal sinus. Nineteen patients (76%) underwent unilateral V-Y-plasty and six patients (24%) underwent bilateral V-Y-plasty. Eighty-four percent cases were from the age group of 21–30 years. Sixty-eight percent patients were mobilized on the fourth postoperative day and 32% patients were mobilized on the third postoperative day. No recurrence was found in any of the patients. Itching and hypertrophic scar were found in two cases (8%), and decreased sensation was found in one patient (4%). The V-Y advancement flap technique for the treatment of pilonidal sinus is efficient and can reduce recurrence. Unilateral/bilateral V-Y flap achieves suture line away from midline, obliteration of natal fold and coverage of defect without tension. In follow-up none of the patients showed recurrence. This technique has distinctly less morbidity and avoids of multiple dressings, reducing the total cost of the treatment. V-Y advancement flap is distinctly better choice among the available flaps as it is less time-consuming, requires less technical expertise as compared to Z-plasty and perforator flaps, and is reliable and easy to plan.
Keywords: Pilonidal sinus, V-Y advancement flap
Introduction
Pilonidal sinus disease was first reported 150 years ago. Incidence of pilonidal disease is about 26 per 100,000 population [1]. Pilonidal disease occurs predominantly in males, at a ratio of about 4:1. It occurs predominantly in white patients, typically in the late teens to early twenties, decreasing after age 25 and rarely occurs after age 45 [2].
In 1950, pilonidal sinus was thought to be of congenital origin rather than acquired disorder [1]. This seemingly minor disease process has baffled physicians as demonstrated by multiple theories of its etiology and management in the current literature. For a time, the entity was referred as “jeep rider’s disease” [1].
Over the past 25 years, many treatments have been advocated for pilonidal sinus but no consensus has emerged, and there have been a few studies comparing relative treatment cost, discomfort, and time off work. Various methods of treating pilonidal sinus have been evolved since1965 in the form of the following: tract curettage/brushing with excision of follicle opening [3], phenol injection into tract [4], diathermy of pilonidal pit [5], laying open of pilonidal sinus and healing by granulation [6], excision and primary closure [4, 7], and excision up to sacrum and skin flaps [8]. Asymmetric closure appears most promising, as there is fast recovery and low recurrence rate, minimal patient inconvenience, and minimum time off work.
The primary goal of the advancement flap is to transfer the tension of the scar that would result from side-to-side closure to a more cosmetically acceptable site. For creating and maintaining the flap, its dynamics should be understood. Primary motion is movement of flap into the surgical or primary defect. The defect created by the flap movement creates a secondary defect. The objective of any flap is to close the primary defect, while minimizing the size of the secondary defect.
The width of any flap is proportional to the width of the defect. The pedicle or base of the flap connects it to the surrounding tissue. The pedicles contain the flap’s vascular supply; thus, it is critical to its survival. The location of the pedicle base in relation to the distal aspect of the flap is often used to describe the flap; flaps are superiorly, inferiorly, medially, or laterally based. To ensure that the pedicle provides adequate blood flow, the length-to-width ratio of the flaps should not usually exceed 3:1. The thickness of the flap should be proportional to the depth of the defect, and the flap must comprise at least a thin layer of subdermal fat to include the part of vasculature.
Material and Methods
We studied the cases of pilonidal sinus admitted to surgical wards of both the hospitals. Each case was assessed thoroughly for detailed history, general, and local examination. Routine preoperative evaluation was done in each case, which included blood chemistry (blood sugar level, blood urea level and serum electrolytes, pus for culture and sensitivity) and plain X-ray of the abdomen. Each case had undergone appropriate management. Preoperative antibiotics were given to the patient. Postoperative course was carefully observed and critically managed to analyze morbidity, hospital stay, and secondary infections. Postoperative antibiotics were given according to pus culture and sensitivity reports. Complications, both intraoperative and postoperative, were noted. Patients were followed up 6 months to 5 years.
Surgical Procedure
Wide local excision of the lesion was done after injecting methylene blue and hydrogen peroxide through sinus to remove all remnants during excision. While excising the sinus, care was taken to go vertically down to the fascia only, as extension below it will hamper its blood supply, also to avoid cavity during approximation. En-block removal of multiple sinuses was done.
After minimal debridement, size of defect was reassessed. V-Y design was marked on both sides of defect. Breadth of the flap was equal to length of the defect for first few centimeters and gradually narrowing to form V. The length of the flap was equal to thrice the width of the defect.
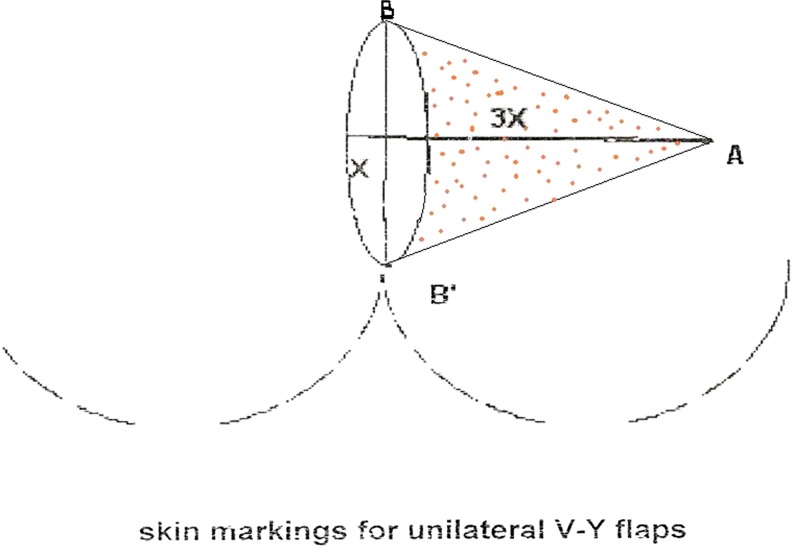
In Fig. 1 it is shown that ‘X’ is width of the defect and ‘3X’ is length of the flap. While creating bilateral flap, length of two flaps has to be unequal, that is, 2X on one side and 3X on other side, so that the suture line is not in midline. While making the design, care was taken to avoid creating an acute angle at corners (Fig. 1).
Fig. 1.
If x is width of the defect 3x should be length of the flap. B-B' is the advancing edge of the flap. Dotted area is the flap
The incision was carried down to the fascia of underlying gluteus maximum muscle. The upper and lower arms of the flaps were elevated and advanced on gluteal muscle toward the midline interdigiting opposite arm. Even a few fibers of gluteus muscle were cut to increase the mobility of the flap. Care was to be taken to avoid undermining of the flap, and thereby reducing the chances of injuring the perforators. After releasing the flap from all sides, it seems to be falling in midline.
The advancing edges were sutured to each other in two layers and initial V was sutured as Y to cover sacral defect with low tension over suture line, which avoids suture breakdown. The advancing edge of the flap was undermined from sacral fascia for about 2–3 cm, so as to be sutured to soft tissue of the opposite side thereby avoiding dead space. After elevating the flap from one side, we assessed feasibility of tension-free closure. When in doubt bilateral flaps of unequal dimensions were used to avoid midline scar and obliteration of natal cleft (Figs. 2, 3, 4, and 5).
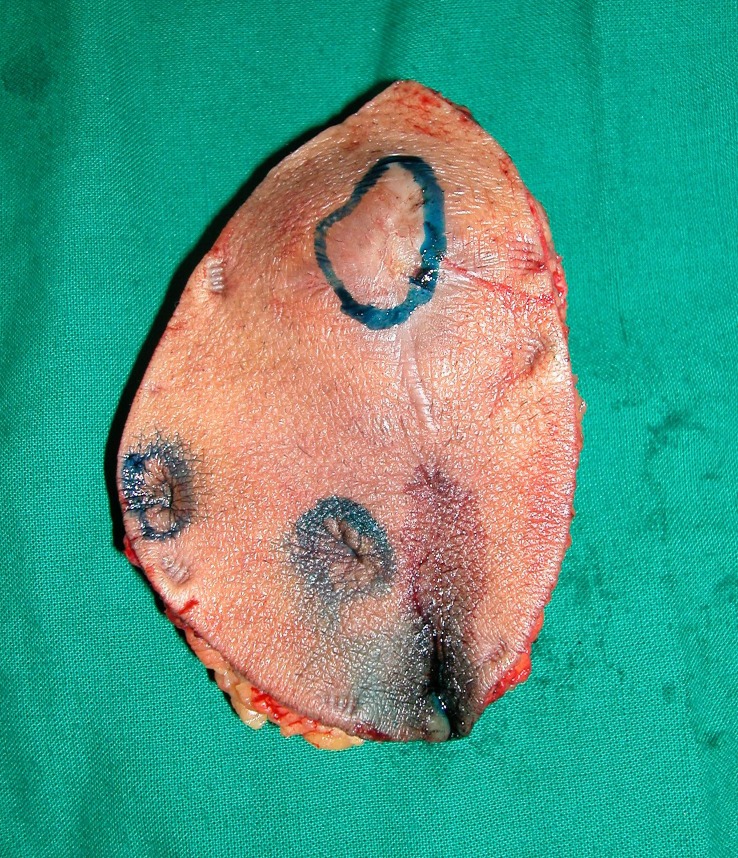
Fig. 2.
Multiple sinus tracts excised
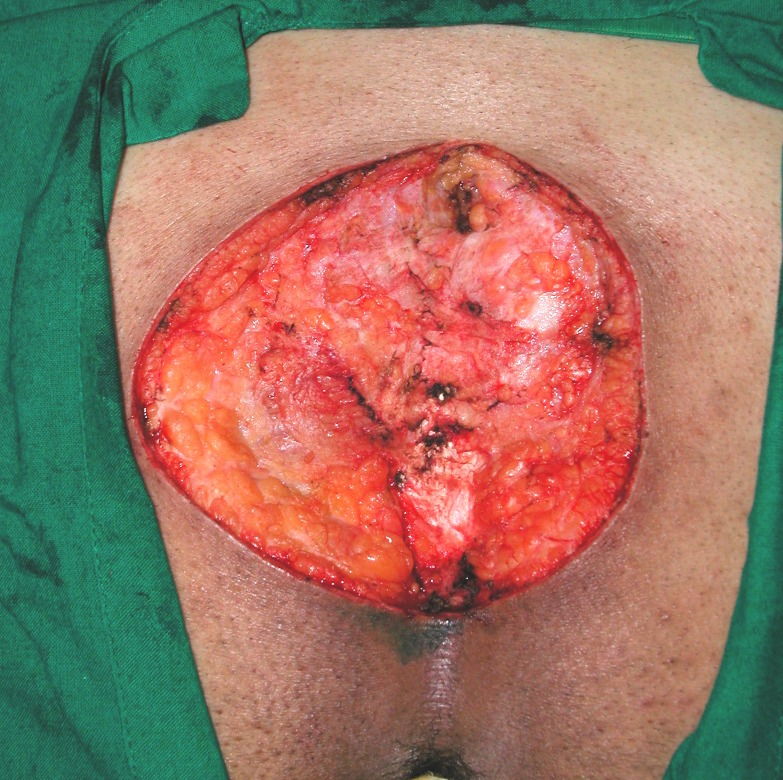
Fig. 3.
Post excisional defect
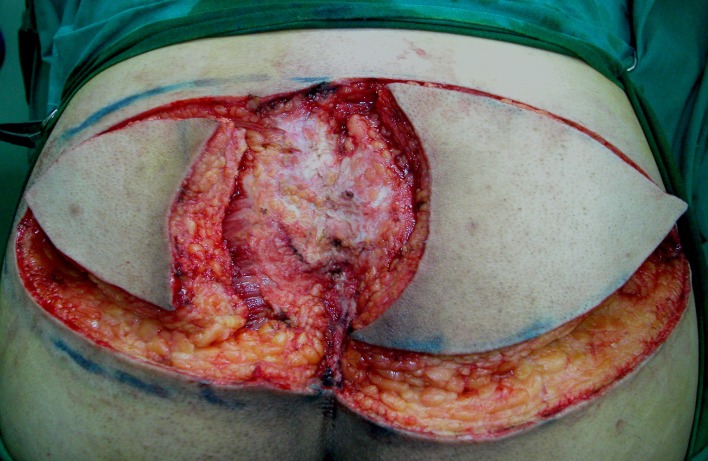
Fig. 4.
Unequal bilateral advancement flaps raised
Fig. 5.
Post operative picture after complete healing
The use of perforator-based advancement flap principle, in repair of relatively large pilonidal sinus, helps in efficient redistribution of available tissue in addition to reducing tension along the suture line. Also, the suture line is not in midline, so chances of recurrence at the suture site are minimal.
Fasciocutaneous V-Y advancement flap can be modified according to the local defect size as unilateral, bilateral, bilateral equal, and unequal V-Y advancement flap.
No drain was kept in any of the patients as there was no dead space.
The mean operative time for flap surgery was 1 h. The average post-operative stay was 4 days.
After suture removal, patients were advised oil massage for flaps, application of silicon gel for scars, and shaving or depilation in some forms such as cream, hair remover, and laser in natal cleft.
Results
In our study, pilonidal sinus was found to be most common in the age group between 21 and 30 years.
Unilateral V-Y-plasty was done in 19 patients (76%) and bilateral was done in six patients (24%).
Total duration of hospitalization ranged from 3 to 5 days and average duration of hospitalization was 4 days.
Average day of mobilization was the third postoperative day.
The average period for healing was 8 days.
During follow-up, done for all cases in January 2011, we observed complaint of itching at the operative site of scar and its hypertrophy in two cases (8%). Reduced sensation over flap skin was found in one patient (4%).
In our retrospective study, there was no recurrence over the period of follow-up ranging from 6 months to 5 years.
Postoperatively, 21 patients (84%) did massage over the scar. Two patients (8%) were applying silicon gel sheet. One patient (4%) was using silicon cream to prevent hypertrophy over the scar. Twenty-one patients (84%) were doing regular hair trimming, and three patients (12%) were doing shaving postoperatively. One patient (4%) underwent four settings of laser for hair removal (Table 1).
Table 1.
Masterchart of 25 patients
| sr. no | Age | Sex | Type of V-Y plasty | Complication | Duration of hospitalization in days | Post op care | Hair removal | Post op mobilization (days) | Time for healing (in days) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Recurrence | Itching | Hypertropic scar/keloid | Loss of sensations | |||||||||
| 1 | 22 | M | Unilateral | No | Yes | No | No | 3 | Massage | Trimming | 3 | 7 |
| 2 | 27 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 3 | 8 |
| 3 | 37 | M | Unilateral | No | No | Yes | No | 4 | Massage | Trimming | 4 | 7 |
| 4 | 23 | M | Bilateral | No | No | No | No | 5 | Massage | Shaving | 4 | 8 |
| 5 | 40 | M | Bilateral | No | No | No | No | 4 | Massage | Shaving | 4 | 8 |
| 6 | 35 | M | Bilateral | No | No | No | No | 4 | Massage | Trimming | 4 | 7 |
| 7 | 26 | F | Unilateral | No | No | No | No | 3 | Massage | Laser hair removal | 3 | 7 |
| 8 | 30 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 4 | 6 |
| 9 | 32 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 3 | 7 |
| 10 | 30 | M | Bilateral | No | No | Yes | No | 4 | Massage | Shaving | 4 | 8 |
| 11 | 26 | M | Unilateral | No | Yes | No | No | 3 | Massage | Trimming | 3 | 7 |
| 12 | 23 | M | Unilateral | No | No | No | Yes | 3 | Massage | Trimming | 4 | 8 |
| 13 | 28 | M | Bilateral | No | No | No | No | 4 | Silicon gel sheet | Trimming | 4 | 8 |
| 14 | 27 | M | Unilateral | No | No | No | No | 3 | Silicone gel ointment | Trimming | 3 | 7 |
| 15 | 29 | M | Unilateral | No | No | No | No | 3 | Silicon gel sheet | Trimming | 3 | 8 |
| 16 | 21 | M | Unilateral | No | No | No | No | 4 | Massage | Trimming | 3 | 7 |
| 17 | 24 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 4 | 8 |
| 18 | 23 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 4 | 7 |
| 19 | 21 | M | Bilateral | No | No | No | No | 4 | Massage | Trimming | 4 | 7 |
| 20 | 24 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 4 | 7 |
| 21 | 27 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 4 | 7 |
| 22 | 25 | M | Unilateral | No | No | No | No | 4 | Massage | Trimming | 4 | 8 |
| 23 | 27 | M | Unilateral | No | No | No | No | 4 | Massage | Trimming | 4 | 8 |
| 24 | 28 | F | Unilateral | No | No | No | No | 4 | Massage | Trimming | 4 | 8 |
| 25 | 30 | M | Unilateral | No | No | No | No | 3 | Massage | Trimming | 4 | 7 |
Discussion
Pilonidal sinus is a chronic intermittent disorder of the sacrococcygeal region and its treatment, usually surgical, remains controversial [9]. Factors implicated in its etiology are large buttocks with deep natal cleft [9–11], adolescent or young males with positive family history, folliculitis at another site, obesity [12], occupations requiring prolonged sitting, traveling or driving, excessive body hair [13], and poor local hygiene [13]. Although various modalities of treatment have been described, no consensus has emerged as all have met with varying degrees of recurrence [14]. The two main factors were responsible for recurrence due to hair penetration, namely, the depth of the cleft and the presence of a portal of entry for hairs in the midline (the wound) [14].
Surgical treatment of chronic pilonidal sinus by excision of the diseased tissue down to the presacral fascia is generally accepted, but the management of the remaining defect is still a matter of debate. Many methods have been described such as (1) open excision, (2) primary closure, and (3) excision and flap closure.
Open excision and healing by the secondary intention technique is associated with long hospitalization, wound dressing daily, increased postoperative morbidity, loss of work days, and poor cosmetic outcome due to wide unacceptable scars [15]. Primary closure of the wound is a simple technique, but it has a high recurrence rate (5–7%) [16] due to continuing deep natal cleft [17]. Excision with local flap procedures has the lowest recurrence rates, but they are more technically demanding and their use is generally restricted to recurrent complex pilonidal sinus [18].
In this study, there was no recurrence in the flap method. This could be explained by placing the scars away from the midline, thus avoidance of portal entry of hairs in the midline (the wound) and flattening the natal cleft to reduce friction, local warmth, moisture, and hair accumulation.
In this study, no case reported flap necrosis [17, 19, 20]. To address the flap survival of the technique, gluteal perforator vessels could have contributed to its viability in penetrating through the fascia to the overlying skin [21]. Pilonidal sinus never begins on a convex surface and the primary source of surgical failures is the shape of the gluteal cleft, which creates the moist, warm, bacteria-friendly environment and thus reducing the depth of the concave fold that harbors the problem [10, 19, 22, 23].
The Z-plasty procedure has been described by Monro and MacDermot [24]. The disadvantage of this procedure is that the part of the wound is in the midline, which is the main cause of recurrence. Besides the flap tip, necrosis has been reported. Z-plasty requires back cuts and incisions at specific angles and is not supplied by robust perforators like V-Y-plasty, technically demanding as geometrical planning is involved.
The W-plasty technique has been described by Roth and Moorman [25], but some part of the wound was in midline and recurrence rate was high (8%) [26].
The Limberg flap is another transposition technique; it is suitable only for closure of rhomboid defects with angles of 60 and 120° and the flap depends on the looseness of adjacent skin. Reported complication and recurrence rates are 6 and 4%, respectively [26]. The Limberg flap scores in simplicity, but it needs excessive mobilization. It also needs an expert surgeon and more excision of a normal skin for making the rhomboid shape of 60 and 120°.
Closure of the defect with Limberg flap seems to be elliptical rotation flap at first glance [27]; however, it creates a line of tension along the radius of the arc that may necessitate back cuts. This decreases the blood supply to the flap. It has recurrence rate of 8% [28].
Perforator-based flaps require meticulous technique and expertise. These flaps are having the long learning curve and having the risk of terminal necrosis.
V-Y advancement flap is easier to perform. The flap has an excellent blood supply and can be raised safely without dissecting of the pedicle. We feel that this is robust flap, which can be quickly harvested, and has got a lesser learning curve.
In our series of 25 patients, all the cases yielded positive results. There were no recurrences at maximum of 5-year follow-up. We suggest use of unilateral or bilateral VY flaps in management of primary or recurrent pilonidal sinus disease.
Our technique is simple and reliable and offers an effective and elegant alternative to the more classic operations for pilonidal sinus as it has the advantage of being tension-free closure without leaving dead space, thus increasing patient comfort and wound healing, and decreases the length of hospital stay with early return to work.
It does not only remove the existing sinus but also eliminate factors that predispose to formation of another sinus by placing the scars away from the midline and flattening the natal cleft, and it is useful for recurrent cases after a failed surgical procedure and it gives good cosmetic results without any early or delayed recurrence.
Conclusions
V-Y-plasty is distinctly better choice among the flaps as it is less demanding and is not operator dependent. So, we conclude that pilonidal sinus, which is found more commonly in hairy, obese males with sedentary life style, is treated more effectively, with no recurrence rate and less complications by wide local excision followed by asymmetric closure by unilateral or bilateral V-Y fasciocutaneous advancement flap.
Acknowledgements
We would like to thank Deparments of Surgery at Deenanath Mangeshkar and Sassoon General Hospitals Pune for their continuing support.
References
- 1.Sebastian M (1997) Pilonidal cysts and sinuses. In: Principles of surgery, pp 1330–4, 1234–5
- 2.Klass AA. The so-called pilonidal sinus. Can Med Assoc J. 1956;75:737–742. [PMC free article] [PubMed] [Google Scholar]
- 3.Berry DP. Pilonidal sinus disease. J Wound Care. 1992;1(3):29–32. doi: 10.12968/jowc.1992.1.3.29. [DOI] [PubMed] [Google Scholar]
- 4.Stansby G, Greatorex R. Phenol treatment of pilonidal sinus of the natal cleft. Br J Surg. 1989;76(7):729–730. doi: 10.1002/bjs.1800760727. [DOI] [PubMed] [Google Scholar]
- 5.Jacobsen P (1959) Pilonidal disease: management without excision. Am Acad GP xix:3 [PubMed]
- 6.Kronberg I, Christensen KI, Zimmerman-Nielson O. Chronic pilonidal disease: a randomised trial with complete three year follow up. Br J Surg. 1986;72:303–304. doi: 10.1002/bjs.1800720418. [DOI] [PubMed] [Google Scholar]
- 7.Jones DJ. ABC of colorectal diseases. Pilonidal sinus. BMJ. 1992;305:410–412. doi: 10.1136/bmj.305.6850.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sondenaa K, Diab R, Nesvik I, et al. Influence of failure of primary wound healing on subsequent recurrence of pilonidal sinus. Eur J Surg. 2002;168(11):614–618. doi: 10.1080/11024150201680007. [DOI] [PubMed] [Google Scholar]
- 9.Hull TL, Wu J. Pilonidal disease. Surg Clin North Am. 2002;82:1169–1185. doi: 10.1016/S0039-6109(02)00062-2. [DOI] [PubMed] [Google Scholar]
- 10.Bascom J, Bascom T. Failed pilonidal sinus surgery: new paradigm and new operation leading to cures. Arch Surg. 2002;137:1146–1150. doi: 10.1001/archsurg.137.10.1146. [DOI] [PubMed] [Google Scholar]
- 11.Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1996;83:1452–1455. doi: 10.1002/bjs.1800831040. [DOI] [PubMed] [Google Scholar]
- 12.Akinci OF, Bozer M, Uzunkoy A. Incidence and etiological factors in pilonidal sinus among Turkish soldiers. Eur J Surg. 1999;165:339–342. doi: 10.1080/110241599750006875. [DOI] [PubMed] [Google Scholar]
- 13.Bose B, Candy J. Radical cure of pilonidal sinus by Z-plasty. Am J Surg. 1970;120:783–786. doi: 10.1016/S0002-9610(70)80049-6. [DOI] [PubMed] [Google Scholar]
- 14.Armstrong JH, Barcia PJ. Pilonidal sinus disease. The conservative approach. Arch Surg. 1994;129:914–919. doi: 10.1001/archsurg.1994.01420330028006. [DOI] [PubMed] [Google Scholar]
- 15.Fuzun M, Bakir H, Soylu M, Tansug T, Kaymak E, Harmancioglu O. Which technique for pilonidal sinus—open or closed? Dis Colon Rectum. 1994;37:1148–1150. doi: 10.1007/BF02049819. [DOI] [PubMed] [Google Scholar]
- 16.Khanzada TW, Samad A. Recurrence after excision and primary closure of pilonidal sinus. Pak J Med Sci. 2007;23(3):375–379. [Google Scholar]
- 17.Iesalnieks I, Furst A, Rentsch M, Jauch KW. Primary midline closure after excision of a pilonidal sinus is associated with a high recurrence rate. Chirurg. 2003;74:461. doi: 10.1007/s00104-003-0616-8. [DOI] [PubMed] [Google Scholar]
- 18.Khatri V, Espinosa MH, Amin AK. Management of recurrent pilonidal sinus by simple V-Y Fasciocutaneous flap. Dis Colon Rectum. 1994;37:1232–1235. doi: 10.1007/BF02257787. [DOI] [PubMed] [Google Scholar]
- 19.Nessar G, Kayaalp C, Seven C. Elliptical rotation flap for pilonidal sinus. Am J Surg. 2004;187:300–303. doi: 10.1016/j.amjsurg.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Lamke LO, Larsson J, Nylen B. Treatment of pilonidal sinus by radical excision and reconstruction by rotation flap surgery of Z-plasty technique. Scand J Plast Reconstr Surg. 1979;13:351–353. doi: 10.3109/02844317909013081. [DOI] [PubMed] [Google Scholar]
- 21.Koshima I, Moriguchi T, Soeda S, Kawata S, Ohta S, Ikeda A. The gluteal perforator-based flap for repair of sacral pressure sores. Plast Reconstr Surg. 1993;91:678–683. doi: 10.1097/00006534-199304000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Lamke LO, Larsson J, Nylen B. Treatment of pilonidal sinus by radical excision and reconstruction by rotation flap surgery of Z-plasty technique. Scand J Plast Reconstr Surg. 1979;13:351–353. doi: 10.3109/02844317909013081. [DOI] [PubMed] [Google Scholar]
- 23.Quinodoz PD, Chilcott M, Grolleau JL, Chavoin JP, Costagliola M. Surgical treatment of sacrococcygeal pilonidal sinus disease by excision and skin flaps: the toulouse experience. Eur J Surg. 1999;11:1061–1065. doi: 10.1080/110241599750007900. [DOI] [PubMed] [Google Scholar]
- 24.Monro SR, MacDermot FT. The elimination of causal factors in pilonidal sinus treated by Z-plasty. Br J Surg. 1965;52:177–181. doi: 10.1002/bjs.1800520306. [DOI] [PubMed] [Google Scholar]
- 25.Roth RF, Moorman WL. Treatment of pilonidal sinus and cyst by conservative excision and W-plasty closure. Plast Reconst Surg. 1977;60:412–415. doi: 10.1097/00006534-197760030-00015. [DOI] [PubMed] [Google Scholar]
- 26.Urhan MK, Kucukel F, Topgul K, Ozer I, Sari S. Rhomboid excision and Limberg flap for managing pilonidal sinus. Dis Colon Rectum. 2002;45:656–659. doi: 10.1007/s10350-004-6263-4. [DOI] [PubMed] [Google Scholar]
- 27.Cherry JK. Primary closure of pilonidal sinus. Surg Gynecol Obst. 1986;126:1263–1269. [PubMed] [Google Scholar]
- 28.Aston SJ, Beasley RW, Thorne CHM. Grabb and Smith’s plastic surgery. 5. Philadelphia: Lippincott-Raven; 1997. p. 17. [Google Scholar]