Abstract
To study the role of infiltrating 2% Lidocaine in Micro ear surgeries performed under general anaesthesia. To measure the impact of infiltration of 2% Lidocaine in post operative pain relief and per operative bleeding. A Double blinded, Prospective randomized comparative study was conducted in a tertiary care referral centre. A total of 30 patients planned for micro ear surgeries under general anaesthesia (Tympanoplasty and Cortical mastoidectomy) for CSOM tubotympanic disease were selected and divided into two groups randomly by the chief senior consultant. Group A patients received local infiltration of 2% Lidocaine with one in 200,000 adrenaline and Group B patients received infiltration of one in 200,000 adrenaline in distilled water alone. Operating surgeon assessed the bleeding in the surgical field using Boezaart’s grading system. Post operative pain was assessed using a visual analog scale. Pain scores of these patients were assessed in the 1st, 4 and 24th h post operatively and recorded. The mean post operative pain score in the 1st h for the patients in Group A was 0.93 and for patients in Group B was two. The difference in the pain scores between the two groups was significant (P < 0.02).The difference in the mean post operative pain scores between the two groups in the 4 and 24th h were not significant (P < 0.1).Per operatively, grade III bleeding was present in 73% of patients in group B and only 33% of patients had grade III bleeding in group A. Infiltration of 2% Lidocaine has a significant impact over the grade of bleeding in the operative field and also on 1st h post operative pain relief. It did not have a significant influence on the pain relief in the 4 and 24th h post operatively.
Keywords: Lidocaine, Local infiltration, Micro ear surgery, General anaesthesia
Introduction
Otolaryngology is an important surgical specialty where the quality of anaesthesia can influence the field of interest and hence it is outcomes. Since the inception of the era of surgery, surgeons have tried to reduce the bleeding in the operative field [1]. Pros and cons of doing micro ear surgeries under general anaesthesia and local anaesthesia have been debated a lot [2].
It is a common practice to infiltrate local anesthetic drugs even in surgeries performed under general anaesthesia [3] and lidocaine is considered merely a carrier of adrenaline [4]. We should remember that Lidocaine is not just a placebo but a drug that can cause toxicity at higher doses [5]. Role of infiltrating various local anesthetic agents in surgeries like tonsillectomy, nasal surgery [6–8], tooth extraction [9] etc. were studied before. The purpose of our study is to evaluate the role of infiltrating 2% Lidocaine in micro ear surgeries performed under general anaesthesia in terms of bleeding in the operative field and post operative pain relief for the patient.
Patients and Methods
This is a randomized, double blinded prospective study done in the Department of Otorhinolaryngology, Head and Neck surgery of a tertiary care referral centre. Study was done between the period of March 2010 to August 2010.
Patients diagnosed to have chronic suppurative otitis media tubotympanic disease between the age group of 10–50 years were selected for the study. Patients with chronic suppurative otitis media attico antral disease, having co-morbid illness such as hypertension, diabetes mellitus, coronary artery disease and coagulation abnormalities were excluded. The patients taking antiplatelet or anti coagulant drugs and those seeking revision ear surgeries were also excluded from the study.
After obtaining an informed consent, background data of the patients selected were recorded in a proforma .The senior author allocated the patients into two groups. Odd number patients were included in group A and even number patients into group B. The operating surgeon and patients were blinded about the groups. Different surgeons including residents performed either tympanoplasty or cortical mastoidectomy under general anaesthesia. The senior author was not part of the operating team of surgeons.
General anaesthesia was induced with 2.5–5 mg of midazolam, 100 μgms of fentanyl and 1–2 mg/kg body weight of propofol. After preoxygenation with facemask ventilation, patients were paralysed with vecuronium at the dose of 0.1 mg/kg. Endotracheal intubation was done with appropriate size endotracheal tube. Anaesthesia was maintained with nitrous oxide and oxygen at the ratio of 1:2 along with 2% isoflurane. Patients heart rate, non invasive blood pressure, oxygen saturation and electrocardiogram were monitored during the mechanical ventilation. Mean arterial pressure of the patient was maintained between 75 and 90 mm of Hg.
All the patients underwent micro ear surgery by post auricular approach. Group A patients received local infiltration of 2% Lidocaine (5 mg/kg) with one in 200,000 adrenaline using a 23 gauge needle. Infiltration was given in the post auricular region and four quadrants of external auditory canal in all patients. Group B patients received infiltration with one in 200,000 adrenaline prepared in distilled water. This was prepared by taking 0.1 ml of 1:1,000 adrenaline in a tuberculin syringe diluted in 20 ml of distilled water.
Post aural modified William Wilde’s incision was made 10 min after infiltration [4]. Operating surgeon was asked to assess the bleeding in the surgical field during post auricular dissection and middle ear work using Boezaart’s grading system (Table 1) for bleeding [10, 11]. Duration of surgery was defined as the period between the time of incision to the last suture.
Table 1.
Grading system for bleeding in surgical field Boezaart et al. [10]
| Grades | Surgical field |
|---|---|
| I | Cadaveric conditions with minimal suction required |
| II | Minimal bleeding with infrequent suction required |
| III | Brisk bleeding with frequent suction required |
| IV | Bleeding covers surgical field after removal of suction before surgical instrument can perform manoeuvre |
| V | Uncontrolled bleeding |
Post operative pain score was assessed using a visual analog scale of 10 points [12]. This pain score was explained to the patients pre operatively by the staff nurse. The pain scores (X) of the patients were assessed in the 1st, 4 and 24th h post operatively and recorded. Additional dose of analgesic (diclofenac sodium 75 mg intra muscular injection) was given if the pain score was three or more.
The mean pain score (x) as calculated for each group after 1st, 4 and 24th h in the post operative period. Student’s t test was applied and P value was calculated [13]. The observed value was considered significant if the P value is <0.05.
Results
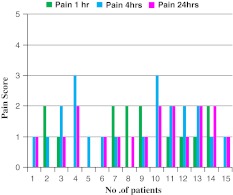
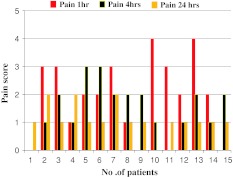
Thirty patients (14 males, 16 females) participated in our study. The mean age group was 32.4 years (range 11–49 years). Fifteen patients were included in each group. The mean duration of the surgery was 2 h 20 min (range 1–3 h 30 min). Pain scores in the 1st, 4 and 24th post operative hours for group A and B are shown in the Figs. 1 and 2. All the patients in group A (Lidocaine group) had a pain score of 2 or less in the 1st post operative hour. None of the patients had a pain score of 3 or more. In group B, six patients had pain score of 3 and above in the 1st post operative hour.
Fig. 1.
Pain scores of patients in Group A
Fig. 2.
Pain scores of patients in Group B
Mean pain score for 1st, 4 and 24th post operative hours for both the groups are shown in Table 2 along with their standard deviations and standard errors. The ‘t’ values were calculated from the actual difference between the mean pain scores of group A and B and standard error (SE). The calculated ‘t’ values for the 1st, 4 and 24th post operative pain scores were 2.6, 0.22 and 0.29, respectively. For a degree of freedom of 28, P value for the pain score during the 1st post operative hour was <0.02, which was significant [13]. The P value for the pain scores during the 4 and 24th post operative hours were <0.1 and hence the difference between the means were not significant.
Table 2.
Mean pain scores, standard deviations and standard errors
| Pain score (h) | Group A mean | Group B mean | Actual difference | Standard deviations Group A (a) |
Standard deviations Group B (b) |
Standard errors √a2/n 1 + b2/n 2 |
|---|---|---|---|---|---|---|
| 1 | 0.93 | 2 | 1.07 | 0.85 | 1.36 | 0.41 |
| 4 | 1.46 | 1.53 | 0.07 | 0.81 | 0.91 | 0.315 |
| 24 | 1.2 | 1.13 | 0.07 | 0.68 | 0.62 | 0.24 |
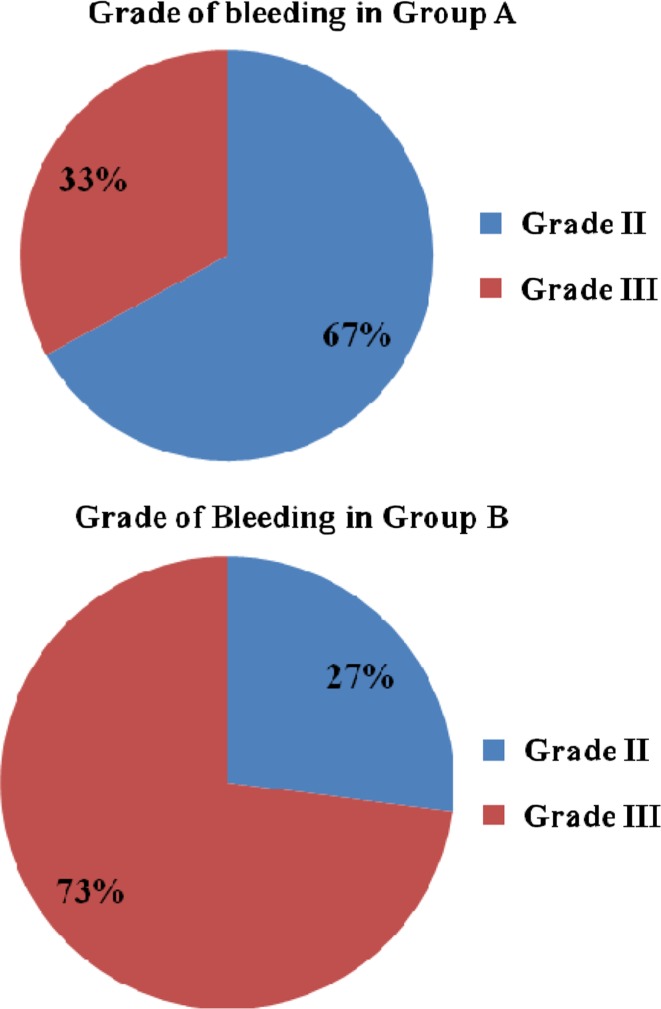
Bleeding in the operative field in both the groups was grade II and III. The Percentage of patients who had grade II or III bleeding in group A and B are shown in the Fig. 3. Patients in the group B had more bleeding when compared to patients in group A.
Fig. 3.
Grade of bleeding in Group A and B
Discussion
Blockade of nerve impulses to abolish sensation may be produced by many tertiary amine bases, certain alcohol and variety of other drugs [14]. However, all currently available clinically useful agents are either aminoesters or aminoamides. The prototype drug for aminoamides is Lidocaine and aminoesters is Procaine [15].
Lidocaine is available in various concentrations such as 0.5, 1, 2, 4, 5 and 10% [5, 16–19]. Generally 0.5 and 1% are used for infiltrative anaesthesia, 2% for peripheral nerve blocks, 4 and 10% for topical anesthesia and 5% for spinal anaesthesia [14]. But in our instituitional practice, we generally use 2% Lidocaine with 1:200,000 adrenaline for infiltration.
Local anaesthetic agents are used alone or along with general anaesthesia for minor and major surgeries. The potency and duration of action of these drugs are influenced by the dosage, use of vasoconstrictive agents, vascularity of infiltrative site etc [14]. Dosage of local anaesthetic drugs can be increased by using a large volume or more concentrated solution. As the dosage is increased the time of onset is decreased and duration of action is increased.
Generally the duration of action of 1% Lidocaine for infiltrative anaesthesia is considered to be 1 h without adrenaline and 2 h with adrenaline [14–16]. The mean duration of the surgery in our study was 2 h 20 min (minimum 1 h to maximum of 3 h 30 min). But the patients in Lidocaine group who underwent surgery for 3 h had less immediate post operative pain score.
Afhami and his colleagues had shown in their study that increasing the concentration of Lidocaine can increase the duration of action for the same volume of drug. In his study 1.5% Lidocaine provided 20 h of pain relief [17]. In our study we used 2% Lidocaine in a standardized dose of 5 mg/kg body weight for all patients [5]. We used double the concentration of regularly used 1% Lidocaine which provided pain relief in the 1st h post operatively. But we have found that 2% Lidocaine did not have a significant impact over the 4 and 24th h pain scores.
The post operative pain relief while using a local anaesthetic infiltration not only depends on the duration of action of drug but is also based on preemptive analgesia [18–22]. Pain transmission from the periphery to the central nervous system leads to modification or plasticity of this system resulting in prolonged and pronounced pain perception even after cessation of the painful stimuli [22, 23]. Preemptive analgesia prevents central sensitisation and hyperexcitability of neurons [24]. The intense pain stimulus is not only caused by the mechanical trauma of surgical incision but also the chemical substances and enzymes from the injured tissue [25]. It is important to understand that general anesthesia doesn’t prevent this central sensitisation [26].
The technique of infiltration of local anesthetic drug has a bearing over the post operative pain relief. Proper infiltration of the periosteum of the mastoid cortex needs a mention apart from regular subcutaneous infiltration. One of the reasons for persisting post operative pain even after local anaesthetic infiltration is failure to infiltrate the periosteum [27].
Surgeons tried numerous methods to reduce bleeding by proper positioning of the patient, hypotensive anaesthesia & co administration of vasoconstrictive agents [1, 4]. Apart from providing analgesia the local anaesthetic drugs influence the bleeding in the surgical field by influencing the smooth muscles of the peripheral vasculature [14].
In our study, though both the group of patients received vasoconstrictive agent adrenaline, the bleeding was less in group. Usually Lidocaine is considered as a vasodilator which should actually increase the bleeding in the operative field. Tatjana and colleagues have studied the bleeding in the operative field during septoplasty [7]. He had shown that infiltration of Lidocaine with adrenaline has reduced the bleeding proving better visibility of surgical field. The impact of Lidocaine over the bleeding in the surgical field is largely attributed to its systemic effects such as arterial hypotension and lower heart rate rather than the action over the smooth muscles of peripheral vasculature [28]. But in our study we maintained the mean arterial pressure between 75 and 90 mm of Hg. Thus, impact of local infiltration with Lidocaine over the general hemodynamic status of the patients seemed nullified and needs further studies to elucidate its contributions towards attaining hemostasis.
Conclusion
Infiltration of 2% Lidocaine with adrenaline has a significant impact over the 1st h post operative pain score (P < 0.2) and grade of bleeding in the surgical field than using adrenaline alone even in micro ear surgeries performed under general anaesthesia. But it does not have any influence over the 4 and 24th h post operative pain score. To achieve a good post operative pain relief infiltrating the periosteum of mastoid cortex with local anaesthetic drug is imperative. Based on our results, we recommend that infiltration of 2% Lidocaine is useful in micro ear surgeries even if it is performed under general anaesthesia and is better than infiltrating diluted adrenaline alone.
References
- 1.Craig HJL (1997) Anaesthesia. In:Michael G (ed) Scott Brown’s otolaryngology, basic sciences vol 1, 6th edn. Oxford: Butterworth Heinemann, pp 5, 7, 23
- 2.Mirko T. Manual of middle ear surgery. 1. New York: Thieme; 1993. pp. 7–10. [Google Scholar]
- 3.Kaufman E, Epstein JB, Gorsky M, Jackson DL, Kadari A. Preemptive analgesia and local anaesthesia as a supplement to general anaesthesia. Anesth Prog spring. 2005;52:29–38. doi: 10.2344/0003-3006(2005)52[29:PAALAA]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson CG. Principles of temporal bone & skull base surgery. In: Glasscock ME III, Gulya AJ, editors. Glasscock-Shambaugh surgery of ear. 5. Washington: BC Decker; 2003. pp. 264–274. [Google Scholar]
- 5.Tripathi KD. Essentials of medical pharmacology. 4. New Delhi: Jaypee; 2001. pp. 160–169. [Google Scholar]
- 6.Goranovic T, Milic M, Parazajder D, Avdagic E, Nenadic D, Vuckovic B, et al. Haemodynamic effects & visibility of the surgical field after lidocaine infiltration during septoplasty under general anaesthesia. Period Biol. 2009;3(2):267–272. [Google Scholar]
- 7.Mcclymont LG, Crowther JA. Local anaesthetic with vasoconstrictor combinations in septal surgery. J Laryngol Otol. 1988;102:793–795. doi: 10.1017/S0022215100106474. [DOI] [PubMed] [Google Scholar]
- 8.Demiraran Y, Ozturk O, Guclu E, Iskender A, Ergin MH, Tokmak A. Vasoconstrictive & analgesic efficacy of locally infiltrated levobupivacaine for nasal surgery. Anesth Analg. 2008;106:1008–1011. doi: 10.1213/ane.0b013e31816174c3. [DOI] [PubMed] [Google Scholar]
- 9.Leong KJ, Roberts GJ, et al. Perioperative local anaesthetic in young paediatric patients undergoing extractions under outpatient ‘short-case’ general anaesthesia. A double-blind randomised controlled trial. Br Dent J. 2007;17(4):297–303. doi: 10.1038/bdj.2007.724. [DOI] [PubMed] [Google Scholar]
- 10.Boezaart AP, Vander MJ, Coetzee A. Comparison of sodium nitroprusside & esmolol induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth. 1995;42:373–376. doi: 10.1007/BF03015479. [DOI] [PubMed] [Google Scholar]
- 11.Wormald PJ. Endoscopic sinus surgery anatomy three dimensional reconstruction & surgical technique. 1. New York: Thieme; 2007. p. 8. [Google Scholar]
- 12.Morisaki H, Masuda J, Fukushima K, Iwao Y, Suzuki K, Matsushima M. Wound infiltration with lidocaine prolongs post operative analgesia after haemorrhoidectomy with spinal anaesthesia. Can J Anaesth. 1996;43:914–918. doi: 10.1007/BF03011804. [DOI] [PubMed] [Google Scholar]
- 13.Park K. Park’s textbook of preventive and social medicine. 17. Jabalpur: Banaridas B; 2002. pp. 611–616. [Google Scholar]
- 14.Miller’s RD. Anaesthesia, vol 1. 6. Philadelphia: Elsevier; 2005. p. 582. [Google Scholar]
- 15.Malamed SF. Handbook of local anesthesia. 5. St Louis: Mosby; 2004. pp. 53–59. [Google Scholar]
- 16.Barash P. Clinical anaesthesia. 6. Philadelphia: Lippincott; 2009. p. 541. [Google Scholar]
- 17.Afhami MR, Salmasi PH. Studying analgesic effects of preincisional infiltration of lidocaine as a local anaesthetic with different concentrations on post operative pain. Pak J Med Sci. 2009;25(5):822–824. [Google Scholar]
- 18.Lowenstein L, Zimmer EZ, Deutsch M, Paz Y, Yaniv D, Jakobi P. Preoperative analgesia with local lidocaine infiltration for abdominal hysterectomy pain management. Eur J Obstet Gynecol Reprod Biol. 2006;136:239–242. doi: 10.1016/j.ejogrb.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Pavlin DJ, Howrath KD, Pavlin EG, Sima K. Preincisional treatment to prevent pain after ambulatory hernia surgery. Anesth Analg. 2003;97:1627–1632. doi: 10.1213/01.ANE.0000090150.65393.E9. [DOI] [PubMed] [Google Scholar]
- 20.Ahmet C, Gokhan Y, Orhan EM, Sizlan A. Preemptive analgesia application in acute appendicitis. Indian J Surg. 2005;67(2):90–93. [Google Scholar]
- 21.Di Marco P, Grippaudo FP, Rocca GD, Vita RD. Preemptive analgesia in reduction mammoplasty. Scan J Plast Reconstr Hand Surg. 2001;3:297–300. doi: 10.1080/028443101750523212. [DOI] [PubMed] [Google Scholar]
- 22.Woolf CJ, Chong MS. Preemptive analgesia treating post operative pain by preventing establishment of central sensitisation. Anesth Analg. 1993;77:362–379. doi: 10.1213/00000539-199377020-00026. [DOI] [PubMed] [Google Scholar]
- 23.Cook AJ, Woolf CJ, Wall PD, Mcmohan SB. Dynamic receptive field plasticity in rat spinal cord dorsal horn following C-primary afferent inputs. Nature. 1987;325:151–153. doi: 10.1038/325151a0. [DOI] [PubMed] [Google Scholar]
- 24.Woolf CJ. Recent advances on the pathophysiology of acute pain. Br J Anaesth. 1989;63:139–146. doi: 10.1093/bja/63.2.139. [DOI] [PubMed] [Google Scholar]
- 25.Woolf CJ. Evidence for central component of post injury pain hypersensitivity. Nature. 1983;308:686–688. doi: 10.1038/306686a0. [DOI] [PubMed] [Google Scholar]
- 26.Rawal N. Analgesia for day care surgery. British J Anaesth. 2001;87(1):73–87. doi: 10.1093/bja/87.1.73. [DOI] [PubMed] [Google Scholar]
- 27.Gottschalk A, Smith DS, Jobes DR, Kennedy SK, Lally SE, et al. Preemptive epidural analgesia & recovery from radical prostatectomy—A randomised controlled trial. JAMA. 1998;279:1076–1082. doi: 10.1001/jama.279.14.1076. [DOI] [PubMed] [Google Scholar]
- 28.Enlund M, Mentell O, Krekmanov L. Unintentional hypotension from lidocaine infiltration during orthognathic surgery & general anaesthesia. Acta Anaesthesiol Scand. 2001;45:294–297. doi: 10.1034/j.1399-6576.2001.045003294.x. [DOI] [PubMed] [Google Scholar]