Abstract
Duplication of internal jugular vein (IJV) is rare. It is the larger channel draining the cranial cavity. We encountered duplication of the IJV while cervical node clearance in a patient with squamous cell carcinoma of left margin of the tongue. IJV divides into two parts anterior and posterior after descending about 2.5 cm from the jugular foramen. IJV is an important landmark in neck surgery. Knowledge of its variations is essential to avoid complications during surgery and to avoid misinterpretation in CT angiography.
Keywords: Internal jugular vein, Duplication, Variations, Jugular veins
Introduction
Internal jugular vein (IJV) is one of the most important major veins draining the cranial cavity. Duplication or fenestration of the IJV is usually an incidental finding in most of the cases reported. The condition is rare. Vascular fenestrations are reported in vertebral, basilar, middle and anterior cerebral arteries but not in any other vein than IJV. Here we have reported duplication of IJV on left side.
Case Report
A 45 year old male patient with T2 N1 well differentiated squamous cell carcinoma of left margin of tongue. Tongue had local wide excision and ipsilateral modified radical neck dissection (IJV and accessory nerve saving) on left side. During cervical node clearance duplication of left IJV was observed.
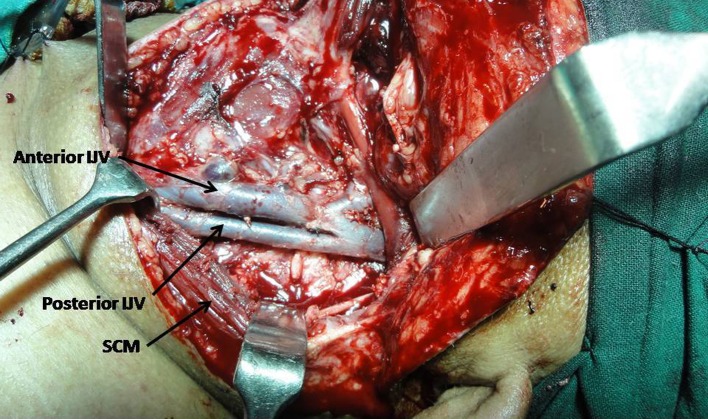
The IJV emerged as a single trunk from the jugular foramen, which then splits into two parts anterior and posterior, after descending an about 2.5 cms from the base of the skull within carotid sheath (Fig. 1). Both the parts rejoin to form a single trunk in the lower part of the neck just before joining the subclavian vein to form a brachiocephalic vein. Left brachiocephalic trunk was formed by left IJV and subclavian vein. The anterior vein was running parallel and receives superior thyroid vein. Both the IJVs are of the same caliber.
Fig. 1.
Illustration showing duplication of the IJV. SCM Sternocleidomastoid Muscle, IJV Internal Jugular Vein
No structure was observed passing between the two IJVs. No phlebectasia of IJV was observed.
Discussion
IJV drains blood from skull, brain, superficial face and much of the neck. It descends in the neck within carotid sheath and unites with the subclavian vein behind the sternal end of the clavicle to form brachiocephalic vein [1].
Duplication of the IJV may be unilateral or bilateral. Unilateral duplication more commonly observed [2]. Duplication of IJV may be partial or complete. The partial venous duplication takes place at variable heights [3]. Sometimes the partial duplication may be seen in the form of inverted ‘Y’ appearance, on conventional venography or longitudinally reformed CT [4–7], demonstrated fenestrated IJV in two cases of by means of CT angiography.
Duplicated IJV may have subclinical presentation or may be seen in the form of swelling in the neck which may be mistaken for the laryngocele or branchial cyst [8]. Wong et al. [8] reported bilateral duplication of IJV associated with clinical symptoms like intermittent neck swelling, dyspnoea and dysphagia.
Duplication of the IJV most of the time associated with phlebectasia of IJV. Phlebectasia is a local fusiform, soft, non-pulsatile swelling in the cervical region which increases during Vasalva maneuver [2–4, 7, 9, 10]. Rossi and Tortori-Donati [2], reported duplication associated with phlebectasia of IJV in a 2 year old girl by colour doppler and MRA. In the present case no such association was observed. There are two dilatations in its course, the superior bulb of IJV or the jugular bulb of Haller and oval inferior bulb of IJV just before its end [3].
Embryologically IJV develops from precardinal veins. The primary blood vessels of head and neck consists of close meshed capillary plexus, drained on each side by the precardinal vein, which is at first continuous cranially with a transitory primordial hind brain which is soon replaced by the primary head vein to become continuous with the precardinal vein [1]. Etiology is still unclear. Three hypothetical explanations have been suggested to describe the duplicated IJV; vascular, neural and bony hypothesis. Vascular theory is most commonly adopted. Paucity or absence of muscular layer in the vein might be responsible for the duplication [2].
The incidence of the anomaly was reported to be approximately 4 per 1,000 unilateral neck dissections [3]. Onco-surgery necessitates the visualization of the IJV for functional or radical cervical lymph node clearance signifies the importance of visualization of this anatomical variation during surgery. IJV is therefore serves as an important landmark during most of the cervical operations [11]. Knowledge of exact position and possible variations prevents the further complications during the surgery.
The IJV is a principal deep vein of the neck and return route for intracranial blood [3]. IJV is an important landmark in most cervical operations. The surgeon should know the exact position and possible variations to prevent complications.
Duplication may occur because of the structures passing between the anterior and posterior IJVs like lateral branch of accessory nerve [12], C2–C3 anterior primary rami, subscapular artery [13]. In present case no structure was observed passing between the anterior and posterior IJVs.
Conclusion
IJV is an important landmark during head and neck surgery. Possible developmental variations should be kept in mind to avoid misinterpretation during CT angiography and lymph node clearance. Care should be taken while Central line placement in such cases.
Contributor Information
Madan Kapre, Phone: +91-9423105960, Email: madankapre@gmail.com.
Ashutosh S. Mangalgiri, Phone: +91-9993366621, Email: ashutoshmangalgiri@yahoo.co.in
References
- 1.Standring S. Gray’s anatomy. 40. Churchill Livingstone: Elsevier; 2008. pp. 595–614. [Google Scholar]
- 2.Rossi A, Tortoni–Donati P. Internal jugular vein phlebectasia and duplication: case report with magnetic resonance angiography features. Pediatr Radiol. 2001;31:134. doi: 10.1007/s002470000350. [DOI] [PubMed] [Google Scholar]
- 3.Prades JM, Timoshenko A, Dumollard JM, et al. High duplication of the internal jugular vein: clinical incidence in the adult and surgical consequences, a report of three clinical cases. Surg Radiol Anat. 2002;24:129–132. doi: 10.1007/s00276-002-0020-y. [DOI] [PubMed] [Google Scholar]
- 4.Som PM, Shugar JMA, Sacher M, Lanzieri CF. Internal jugular vein phlebectasia and duplication: CT features. J Comput Assist Tomogr. 1985;9:390–392. doi: 10.1097/00004728-198503000-00035. [DOI] [PubMed] [Google Scholar]
- 5.Yokomori K, Kubo K, Kanamori Y, et al. Internal jugular vein phlebectasia in two siblings: manometric and histopathologic studies of the pathogenesis. J Pediatr Surg. 1990;25:762–765. doi: 10.1016/S0022-3468(05)80014-4. [DOI] [PubMed] [Google Scholar]
- 6.Park JY, Lee IH, Song CJ. Fenestrated internal jugular vein: case report. J Korean Soc Radiol. 2011;64:227–229. [Google Scholar]
- 7.Towbin AJ, Kanal E. A review of two cases of fenestrated internal jugular veins as seen by CT angiography. Am J Neuroradiol. 2004;25:1433–1434. [PMC free article] [PubMed] [Google Scholar]
- 8.Wong BY, Strachan DR, Loney EL. Duplication of internal jugular veins: case report. J Laryngol Otol. 2010;124:341–344. doi: 10.1017/S0022215109990855. [DOI] [PubMed] [Google Scholar]
- 9.Alaani A, Webster K, Pracy JP. Duplication of internal jugular vein and relation to the spinal accessory nerve. Br J Oral Maxillofac Surg. 2005;43:528–531. doi: 10.1016/j.bjoms.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Paolo B, Giuseppe C, Giulio G, Gianpaolo T, Raffaele R. Internal jugular vein duplication. Indian J Plast Surg. 2009;42:273–274. doi: 10.4103/0970-0358.59303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uecker FC, Wüstenberg E, Zahnert T. High duplication of an internal jugular vein. Laryngo-Rhino-Otol. 2007;86(8):592–594. doi: 10.1055/s-2006-945094. [DOI] [PubMed] [Google Scholar]
- 12.Prakash A, Prakash S, Shrestha BL, Baskota DK, Sinha BH (2009) Duplication of internal jugular vein: a rare case report and review of literature. Internet J Otorhinolaryngol 9(1)
- 13.Downie SA, Schalop L, Mazurek JN, Savitch G, Lelonek GJ, Olson TR. Bilateral duplicated internal jugular veins: case study and literature review. Clin Anat. 2007;20:260–266. doi: 10.1002/ca.20366. [DOI] [PubMed] [Google Scholar]