Abstract
Chronic suppurative otitis media (CSOM) is one of the most commonly encountered diseases in otolaryngology practice. Even in this era of powerful antibiotics, CSOM still consumes considerable medical expenditure, especially in the poorer sections of the society. The present prospective study was conducted at the IGM Hospital, Agartala, in North East India towards clinico-microbiologic evaluation of chronic suppurative otitis media. The focus was mainly on aerobic bacteria, involved in active CSOM in adults as well as children. An attempt was made, despite resource and man power constraints, to have a glimpse of the current antibiotic sensitivity pattern, with special reference to ciprofloxacin. However, the main aim of this study is to see the types of aerobic bacteria involved in CSOM, in our region. Aural swabs were collected from 100 ears, from 97 patients complaining of ear discharge, continuous or intermittent, with a non- intact tympanic membrane for at least 12 weeks. Swabs were sent to the hospitals microbiology laboratory for culture and sensitivity tests. Bacteria could be isolated in 53 cases and 47 swabs were culture negative. The commonest bacteria isolated was pseudomonas (20) followed by Staphylococcus aureus (11), E. coli (11), proteus (9) and klebseilla (2). Three patients had bilateral ear discharge of which one had proteus in both ear swabs, one grew proteus in one ear and no growth in the other, and one patient showed no aerobic bacteria in any of his ear swabs. Among the culture positive cases (n = 53) gram negative bacteria were isolated in 79.24% (n = 42) and S. aureus in 11(20.75%) cases. Among 97 patients number of male and female patients was 50 and 47, respectively. Pseudomonas, E. coli, Bacilli proteus and S. aureus were the predominant bacteria involved in CSOM. Out of the 53 positive isolates ciprofloxacin could be tested against 35 i.e., 66%. Ciprofloxacin was sensitive in 26 isolates, intermediately sensitive in 4 and resistant in only five isolates. It is concluded that, gram negative bacteria especially pseudomonas is the commonest bacteria involved in CSOM in this part of north east India. Ciprofloxacin is an important tool in the management of active CSOM as it is cheap, less ototoxic and widely available as topical preparations.
Keywords: Aerobic bacteria, CSOM, Culture and sensitivity, Ciprofloxacin
Introduction
Suppurative otitis media with its unpleasant symptoms and complications may be a catastrophe for the marvellously structured organ, the ear, on which much of our appreciation of life and human activity depends. It is a privilege for an otorhinolaryngologist to preserve, repair and take utmost care of the structure and function of this wonderful organ, in whatever condition it is presented. It is a challenge especially in children to prevent the progress of acute suppurative otitis media to a chronic disease [1].
A WHO/CIBA Foundation workshop [2] in 1996 defined Chronic suppurative otitis media as a stage of disease in which there is chronic infection of the middle ear cleft, i.e., eustachean tube, middle ear and mastoid, and in which a non-intact tympanic membrane (e.g., perforation or tympanostomy tube) and discharge (otorrhoea) are present for at least 2 weeks or more.
Chronic suppurative otitis media (CSOM) was earlier defined as persistent or intermittent infected ear discharge from a non intact, perforated tympanic membrane, at least for 12 weeks. Those cases in which there is only central perforation of tympanic membrane without any discharge, they are referred to as inactive CSOM. There are two main varieties of CSOM viz. mucosal (or tubotympanic) type of CSOM and squamous (or atticoantral) CSOM. Active tubotympanic CSOM was rechristened active mucosal chronic otitis media (COM) for sometime but the international symposium on recent advances in otitis media, in 1999 preferred the term chronic suppurative otitis media (CSOM) to COM which would mean ‘a chronic perforation with chronic otitis media [3].
CSOM is one the most commonly encountered diseases in the day to day practice of otorhinolaryngology. It requires remarkable and patient management, especially in the children of poorer socio-economic strata, as they do not or can not access adequate and persistent treatment for this chronic affliction [4].
Prevalence of CSOM is more in the developing and underdeveloped countries. It is also common among the poorer sections of the developed world. The incidence is highest among low hygiene populations or with overcrowding and malnutrition. In most cases the disease started in childhood when the eustachian tube was incompetent. More bouts of acute otitis media were seen in infants with many siblings in crowded day care facilities where the mother stopped breast feeding early and parents were smoking. Premature and low birth weight babies in lower socio-economic groups were more vulnerable to CSOM and its attendant handicap and complications in later life [1].
A variety of host factors, genetic disorders like Down syndrome, immune deficiencies or paresis, ciliary disorders, cleft palate have been implicated in the causation of CSOM [1].
In this study we collected aural swabs from 100 ears, in 97 patients, and subjected to culture and sensitivity test in order to detect the aerobic bacteria involved in the chronic suppurative otitis media and the drug susceptibility of selected isolated bacteria.
Materials and Method
Collection of Samples
Clearance from concerned authority and informed consent of patients were taken. Patients presenting with chronic or recurrent ear discharge and on clinical examination found to have discharging ears with central perforation of the tympanic membrane were selected for the study.
Samples were collected before administering any antibiotic therapy and from those patients who had not given any history of recent medication for their ear disease. There were 97 patients who were enrolled in this study. Samples from 100 discharging ears were collected at the out patient’s department (OPD) of Ear Nose and Throat, Indira Gandhi Memorial Hospital, Agartala, Tripura.
Specimens for pus culture were collected, under illumination, by swabbing the discharging ears with a sterile cotton swab and sent to the microbiology laboratory of the hospital without delay. Samples collected were inoculated in nutrient agar and Mackonkey medium and incubated for 24 to 48 h at 37°C. On visible growth of bacterial colonies, microscopic and various chemical and enzymatic tests were conducted to identify the bacteria. Side by side an attempt was made to do sensitivity tests, by Kibri Bour disc diffusion method for commonly available and used drugs, especially ciprofloxacin. Even though all the antibiotic discs were always not available, due to resource constraints in our civil hospital, yet a sincere effort was made to do at least ciprofloxacin sensitivity test in as many isolates as possible.
Patients were divided into six age groups: (I) Group A: less than 10 years; (II) Group B: 11–20 years; (III) Group C: 21–30 years; (IV) Group D: 31–40 years; (V) Group E: 41–50 years; (VI) Group F: 51–80 years.
Observations
Out of total 97 patients, 50 (51.54%) were male and 47 (48.45%) were female patients, 83 (85.56%) were Hindus and 14 (14.43%) were Muslims. Patients of scheduled caste (SC) community constituted 44.32%, other backward classes (OBC) constituted 11.34%, general category (GC) 29.89% and there were no scheduled tribe patients among these 97 total patients, presenting with CSOM. As is evident in our study at Tripura 85.56% i.e., 83 out of total 97 patients who participated and presented with symptoms of active mucosal COM belonged to the communities which are recognised as back ward, like the SC and OBC. A significant exception being the scheduled tribes (ST) community, as we did not find any patients among STs who participated in this study.
Group A had 27.83% (27) patients, group B 28.86% (28), group C 20.61%(20), group D 6.18%(6), group E 7.21%(7), group F 7.21%(7) patients. This is the group wise distribution of all the 97 patients who participated in this study. Among the positive cases (n = 53) there were 18 (33.96%) cases in group A, 15 (28.30%) cases in group B, 13 (24.52%) in group C, 1 (1.80%) in group D, 2 (3.77%) in group E, 3 (5.66%) in group F.
A significant observation is that 75 patients out of the 97 patients, who presented with CSOM, were below age of 30 years though it is seen in this study that no age is absolutely immune to this disease.
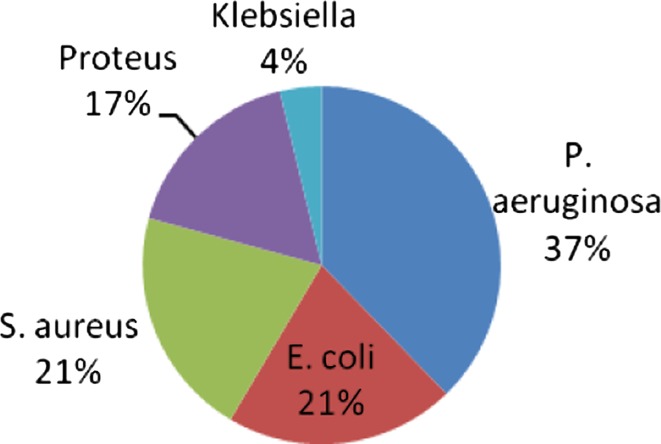
Of the total 53 culture positive cases of aerobic bacteria, Pseudomonas 20 (37.73%) were the commonest bacteria isolated followed by Escherichia coli 11 (20.75%) and Staphylococcus aureus 11 (20.75%) and Proteus 9 (16.98%) and Klebsiella 2 (3.77%) (Fig. 1). It is observed that 42 out of the 53 bacterial isolates, approximately 75%, were of gram negative type in CSOM.
Fig. 1.
Pie chart showing percentage of different bacterial isolates
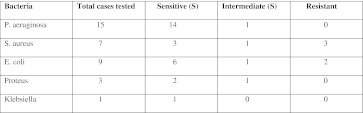
Ciprofloxacin could be tested against 35 out of 53 positive isolates. Among all the gram negative cases ciprofloxacin sensitivity was tested in 28 cases out of which 23 cases were sensitive and three were intermediately sensitive. Therefore, on an average, majority of the gram negative cases in which ciprofloxacin were tested it was found to be effective (Fig. 2).
Fig. 2.
Ciprofloxacin sensitivity among bacterial isolates
In 15 out of the 20 pseudomonas cases in whom ciprofloxacin was tested it was almost 100% effective.
Ciprofloxacin sensitivity for other bacterial isolates was as shown in Fig. 2.
Discussion
The chronic otitis media (COM) is defined as a permanent perforation of the tympanic membrane, which does not close by itself, and an inflammatory reaction in the mucosa of the middle ear. Two main forms of COM are distinct: the chronic suppurative otitis media and the cholesteatomatous COM. Bacterial infection is often the cause of exacerbation and treatment failure in CSOM [5].
In the present study 97 patients of different age groups presenting with the complaints of continuous or intermittent ear discharge for at least 3 months and who on otoscopy revealed central perforations of their tympanic membrane, without any sign of cholesteatoma, were selected. One hundred aural swabs were collected in the ENT out patients department in Indira Gandhi Memorial Hospital (IGMH), Agartala. These aural swabs were collected in sterile test tubes, with sterile cotton swabs, under direct illumination. Culture sensitivity tests, especially against ciprofloxacin, for only the aerobic bacteria were tried in the Microbiology Laboratory of the IGMH. As all the antibiotic discs were not always available and because of man power shortage ciprofloxacin sensitivity could be tested in 35 out 53 bacterial isolates. However, that is the reason of keeping the antibiotic sensitivity test as a secondary goal. The anaerobic and fungal cultures could not be done because of lack of facilities. As we do not have an animal house, like many of the other civil hospitals, fresh blood could not be arranged for preparing blood agar.
Out of the 100 swabs 53 yielded positive cultures, on nutrient agar and Mackonkey medium, for different aerobic bacteria and 47 was culture negative. There were no fungal isolates on these media. The commonest bacteria isolated were Pseudomonas aeruginosa followed by S. aureus, E. coli and proteus. This is not different from many other studies, conducted worldwide, in which the commonest organisms implicated in CSOM were P. aeruginosa, S.aureus, proteus and other enteric bacteria. The present study revealed that 79.24% isolates were gram negative aerobic bacteria, as was found in other studies [6]. A review of studies of microorganisms implicated in CSOM of at least 2 weeks duration found that in children, as in adults, the most commonly isolated organism is P. aeruginosa. Pseudomonas aeruginosa is an opportunistic extracellular pathogen which thrives in the warm damp external auditory meatus of CSOM patients [7].
Almost, 70% cases in this study belonged to SC, OBC and Muslim communities. Traditionally CSOM has been described as the disease of the people of the poorer socio economic and disadvantaged sections, where there is overcrowding, more siblings under the age of five, malnourishment, poor sanitation and inadequate access to health care facilities; especially in children [8]. The present study too shows that 55 out of 97 patients were less than 20 years of age, so it is clear that children and adolescents constitute the maximum patient population of CSOM.
Quinolones, especially ciprofloxacin was found to be effective in eradicating majority of the gram negative bacteria, in which it was tested. In fact in this study it is seen that a cheaper drug like ciprofloxacin is almost 100% successful as far as P. aeruginosa is concerned. A randomised controlled trial of 0.3% ciprofloxacin drops against framycetin, gramicidin and dexamethasone drops for CSOM in a paediatric Australian Aboriginal population found a significantly higher rate of elimination of ear discharge in the ciprofloxacin group [9]. Since pseudomonas is the predominant bacteria usually associated with CSOM therefore it can be concluded that ciprofloxacin ear drops can be tried as a first line of treatment in CSOM, in this part of India, though emergence of ciprofloxacin resistant pseudomonas in CSOM are being reported in other parts of the Asian continent [10].
A significant 47% swabs did not grow any aerobic bacteria and they were culture negative; probably indicating that an attempt to establish infrastructure for anaerobic and fungal culture as well as allergic diagnostic tests should be made. However, with all the draw backs and resource crunch in our civil hospital we were successful in having a glimpse of the aerobic bacteria involved in CSOM, in our part of the country and efficacy of ciprofloxacin in the management of CSOM could also be tested to a significant extent. Otologists trained in allergic diagnostics tests have realized that allergic otitis media superimposed on CSOM is a definite and not uncommon clinical entity, the permanent central perforation of tympanic membrane allowing dusts, moulds and pollens to easily enter and sensitize the middle ear mucosa [11]. Similarly in some studies anaerobes and fungus were isolated in small to significant number of patients [12].
It is concluded that gram negative aerobic bacteria especially pseudomonas is significantly associated with CSOM, in this part of north east India and ciprofloxacin is a preferable tool in the treatment of CSOM because of its lower cost, lack of ototoxicity and ubiquitous availability as topical and oral preparations.
References
- 1.Roger FG (1997) Acute and chronic suppurative otitis media. In: David AA, Michael JC, Alan GK (eds) Scott-Brown’s otolaryngology, vol 6, 6th edn. Butterworth Heinemann, London, pp 1–25
- 2.Prevention of hearing impairment from chronic otitis media. WHO/PDH/98.4. London: CIBA Foundation; 1996. [Google Scholar]
- 3.Bluestone CD, Gates GA, Klein JO, Lim DJ, Mogi G, Ogpra PL, et al. Definitions, terminology and classification of otitis media. Ann Otol Rhinol Laryngol. 2002;111:8–18. doi: 10.1177/00034894021110s304. [DOI] [PubMed] [Google Scholar]
- 4.Saini S, Gupta N, Aparna, Seema, Sachdeva OP. Bacteriological study of paediatric and adult chronic suppurative otitis media. Indian J Pathol Microbiol. 2005;48(3):413–416. [PubMed] [Google Scholar]
- 5.Pajor A, Durko M, Jankowski A, Bartoszko-Tyczkowska A, Stanczyk R. Bacteriological evaluation in chronic otitis media. Otolaryngol Poland. 2006;60(5):757–763. [PubMed] [Google Scholar]
- 6.Yang Y, Gong S, Liu Y. The clinical investigation of bacteriology of chronic suppurative otitis media. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2001;15(12):550–552. [PubMed] [Google Scholar]
- 7.Wintermeyer SM, Nahata MC. Chronic suppurative otitis media. Ann Pharmacother. 1994;28:1089–1099. doi: 10.1177/106002809402800915. [DOI] [PubMed] [Google Scholar]
- 8.Bowell JB, Nienhuis TG. Patterns of persistent otitis media in the first year of life in Aboriginal and non-Aboriginal Australian. Ann Otol Rhinol Laryngol. 1996;105:893–900. doi: 10.1177/000348949610501110. [DOI] [PubMed] [Google Scholar]
- 9.Couzos S, Lea T, Mueller R, Murray R, Culbong M. Effectiveness of ototopical antibiotics for chronic otitis media in Aboriginal children: a community-based, multicentre, double-blind randomised controlled trial. Med J Australia. 2003;179:185–190. doi: 10.5694/j.1326-5377.2003.tb05496.x. [DOI] [PubMed] [Google Scholar]
- 10.Jang CH, Park SY. Emergence of ciprofloxacin-resistant pseudomonas in chronic suppurative otitis media. Clin Otolaryngol Allied Sci. 2004;29(4):321–323. doi: 10.1111/j.1365-2273.2004.00835.x. [DOI] [PubMed] [Google Scholar]
- 11.Derlacki EL. Aural manifestations of allergy. Ann Otol Rhinol Laryngol. 1951;61:179. doi: 10.1177/000348945206100116. [DOI] [PubMed] [Google Scholar]
- 12.Albert RR, Job A, Kuruvilla G, Joseph R, Brahmadathan KN, John A. Outcome of bacterial culture from mastoid granulations: is it relevant in chronic ear disease. J Laryngol Otol. 2005;119(10):774–778. doi: 10.1258/002221505774481219. [DOI] [PubMed] [Google Scholar]