Abstract
In the present study, oxidative stress and lymphocytic DNA damage in both pre-op and post-op benign prostrate hyperplasia (BPH) patients with age >50 years was evaluated and compared with normal healthy subjects (controls- without any evidence of disease) of the same sex and age group. From December 2007 to November 2009, oxidative stress in 45 BPH patients were evaluated both before (pre-op patients) and after 7 days of surgery (post-op patients) in terms of measurements of plasma levels of (1) various anti-oxidative enzymes, (2) non-enzymatic antioxidants and (3) malondialdehyde which is a product of lipid peroxidation. The lymphocyte DNA damage was also evaluated by single cell alkaline gel electrophoresis in terms of tail length migration in these patients. These values were compared with their respective control subjects of similar sex and age group. The activities of antioxidant enzymes and the levels of antioxidant, reduced glutathione were found significantly decreased (p < 0.05) in serum samples of pre-operative group of BPH patients as compared to the controls. These altered parameters increased significantly (p < 0.05) and returned to their near normal control values, but not up to baseline values, in post operative patients i.e. after the cancer load was decreased by surgery. Lymphocytic DNA damage was found to be significantly increased in pre-op group as compared to controls and was reduced after surgery in post-op group. The present study therefore, shows significantly increased levels of oxidative stress and DNA damage in BPH patients which were reduced after removal of tumour load. Thus oxidative damage plays an important role in prostate tumourogenesis and timely management of oxidative stress can be of importance in preventing the occurrence of BPH.
Keywords: BPH, Oxidative stress, Antioxidants, Lipid peroxidation, DNA damage
Introduction
Benign prostatic hyperplasia (BPH) is an extremely common disease of ageing men and carries a distressingly high morbidity because of its irritative and obstructive symptoms. The etiology of BPH is not well understood. Though inflammation has been implicated as a primary stimulus for prostate carcinogenesis [1], it is possible that BPH represents an alternate, non malignant pathway of unregulated prostate growth promoted by oxidative stress and inflammatory mediators. This increased propensity may result from deficient DNA repair and frequent DNA base lesions from generation of high levels of reactive oxygen species (ROS) in the prostate cells [2]. Lipid peroxidation of dietary fat and physiological stimulation of the androgen receptor has been shown to increase ROS production [3]. Thus, in the present study, oxidative stress, antioxidant status and lymphocyte DNA damage in both pre-op and post-op BPH patients was evaluated and compared with normal healthy individuals (controls) of same sex and age group without any evidence of disease.
Materials and Methods
Blood samples of 45 patients with age >50 (57–83) years in each group of (1) pre-op BPH and (2) 7th day post-op BPH were procured from surgery OPD and male surgical wards, department of surgery, J.N. Medical College, Aligarh, from December 2007 to November 2009. Blood samples of 45 controls matching same age group and sex with no apparent disease were also collected for comparison with patient samples. Both ethical clearance and patient’s consent were obtained from the Institutional Ethical Committee and the patients respectively, before commencement of the study.
Diagnosis and Inclusion Criteria
Age >50 years, with history of obstructive or irritative urinary symptoms; abnormal digital rectal examination, elevated PSA levels >4 μg/ml, abnormal TRUS and TRUS guided biopsy reports suggestive of BPH.
Exclusion Criteria
Age ≤50 years with past or present history of any malignancy, radiotherapy or chemotherapy.
Surgery/Intervention done in BPH Patients
Transvesical prostatectomy was done.
Collection of Blood Samples
The heparinised blood samples were centrifuged at 3,000 rpm for 20 min and the plasma was collected in eppendorf tubes and was subjected to following biochemical estimations:
Biochemical Parameters
Lipid peroxidation (LPO) The rate of lipid peroxidation (LPO) was determined according to the method of Buege and Aust [4] by estimating MDA formed with 2-thiobarbituric acid (TBA).
Superoxide dismutase (SOD) (E.C.1.15.1.1) Superoxide dismutase was assayed on the method based on the ability of superoxide dismutase to inhibit the autooxidation of pyrogallol at 412 nm [5].
Catalase (CAT) (E.C.1.11.1.6) Catalase activity was determined by the method of Claiborne [6] by following the rate of decomposition of H2O2 at 240 nm.
Glutathione reductase (GR) (E.C.1.66.4.2) GR was assayed according to the method of Carlberg and Mannervik [7]. This enzyme catalyzes the NADPH dependent reduction of glutathione disulfide to glutathione. The reaction mixture was followed spectrophotometrically at 340 nm.
Glutathione-S-transferase (GST) (E.C 2.5.1.18) GST was assayed according to the method of Habig et al. [8]. Reaction of glutathione and DTNB was followed and absorbance read at 340 nm.
Glutathione (GSH) estimation GSH content using sulfosalicylic acid and DTNB was determined by the method of Jollow et al. [9]. The absorbance of yellow color was recorded at 412 nm.
Alkaline comet assay Comet assay was performed under alkaline conditions essentially according to the procedure of Singh et al. [10]. The parameter taken to assess cellular DNA damage was tail length, (migration of DNA from the nucleus, μm) and was automatically generated by Kornet 5.5 image analysis system. This is a simple technique to assess DNA damage in individual cells.
Statistical analysis
Data was expressed as group mean ± SEM and analyzed by one-way ANOVA for differences among controls and BPH groups. p values less than 0.05 were considered statistically significant.
Results
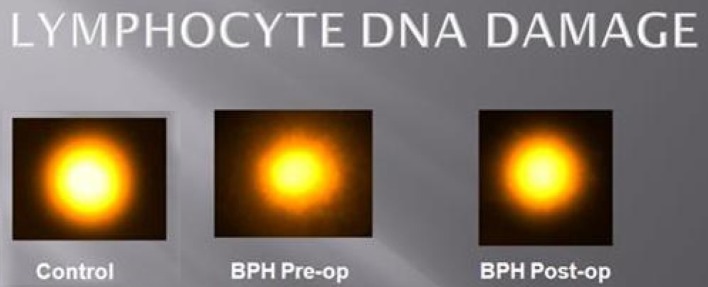
As observed in Table 1; the levels of antioxidative enzymes SOD, CAT, GST and GR and non enzymatic antioxidant GSH were found to be significantly decreased (p < 0.05) in serum samples of pre-operative BPH patients as compared to the controls. These altered values increased significantly (p < 0.05) and returned to their near normal control values, but not reaching baseline values, in post operative patients i.e. after the tumour load was decreased by surgery. Levels of MDA, the product of lipid peroxidation were found to be elevated significantly (p < 0.05) in pre-operative BPH patients as compared to controls, these levels decreased significantly (p < 0.05) in patients who underwent surgery. Lymphocyte DNA damage was also assessed in the same group of patients, in terms of tail length (μm) migration of DNA from nucleus. Tail length (Table 2; Fig. 1) was found to be significantly increased in pre-op BPH patients as compared to controls.
Table 1.
Shows the observed plasma antioxidant enzyme activities and levels of GSH and MDA in different groups of BPH patients and control
| Groups | SOD (unit/mg protein) |
CAT (unit/mg protein) |
GST (unit/mg protein) |
GR (unit/mg protein) |
GSH (μmol/mg protein) |
MDA (nmol/mg protein) |
|---|---|---|---|---|---|---|
| Control | 10.50 ± 0.60 | 1.40 ± 0.08 | 0.98 ± 0.04 | 0.43 ± 0.02 | 1.82 ± 0.10 | 0.030 ± 0.001 |
| Pre-op (BPH) | 6.90 ± 0.40* | 0.90 ± 0.06* | 0.60 ± 0.03* | 0.29 ± 0.01* | 0.98 ± 0.05* | 0.070 ± 0.004* |
| Post-op (BPH) | 9.10 ± 0.50** | 1.15 ± 0.06** | 0.80 ± 0.05** | 0.39 ± 0.03** | 1.45 ± 0.09** | 0.050 ± 0.006** |
Each value represents the mean ± SEM of 45 patients each in pre-op and post-op groups and 45 controls
* p < 0.05 when compared to control group
** p < 0.05 when compared to pre-op BPH patients
Table 2.
Lymphocyte DNA damage measured in terms of tail length in the BPH patients both before and after surgery as compared to control subjects
| Groups | Tail length (μm) |
|---|---|
| Control | 2.50 ± 0.07 |
| Pre-op BPH | 25.10 ± 0.12* |
| Post-op BPH | 15.70 ± 0.54 |
Data represents mean ± SEM of 45 subjects in each group
* p < 0.05, significant when compared to control
Fig. 1.
Showing migration of DNA in terms of tail length in pre-op and post-op BPH patients and controls
Discussion
The present study tries to explore the possible impact of oxidative stress and DNA damage on the clinical outcome of BPH patients. The results of the study clearly show that oxidative stress and DNA damage was significant in pre-op BPH patients as compared to controls, which is in agreement with other studies using chromosomal aberrations as the study end point [11]. The cause of enhanced oxidative stress could be the overproduction of free radicals or decrease in the activities of free radical scavenging enzymes like SOD, GST GR and glutathione levels in their circulation, or both. The enhanced free radical levels are also depicted by an increase in MDA levels, a lipid peroxidation product in the pre-op BPH patients as compared to controls. In post-op patients, DNA damage assessed by comet tail length reduced to some extent, but could not reach to control values. The reason could be that the extensive damage caused needed adequate amount of repair which could not be achieved when the hyperplasic tissue load was reduced, revealing that prostate cells may be under persistent oxidative stress, or there can be deficiency of DNA damage repairing enzymes or more time is required for DNA repair than 7 days, the time period of sample collection.
Androgens are required for maintaining the homeostasis of cell proliferation and apoptosis in the prostate gland and undoubtedly play a key role in prostate carcinogenesis [12]. Although androgens do not cause BPH, the development of BPH requires the presence of testicular androgens during prostate development, puberty and aging [13]. Patients castrated before puberty, or who are affected by a variety of genetic diseases that impair androgen action or production, do not develop BPH. Moreover androgen withdrawal leads to partial involution of established BPH [14]. Epidemiologic data suggest that androgens and/or environmental exposures, especially diet rich in dietary fat, play an important role in prostatic carcinogenesis. The possible link between diet and prostate cancer can be oxidative stress; the generation of reactive oxygen species can trigger a host of pro-carcinogenic processes. Androgens are found to increase oxidative stress within human prostate cancer cell lines [15].
In the present study the lipid peroxidation product i.e. MDA levels were found to be increased significantly in pre-op BPH patients. Lipid peroxidation is one of the main manifestations of oxidative damage initiated by ROS and it has been linked to the altered membrane structure and enzyme inactivation. It is initiated by the abstraction of a hydrogen atom from the side chain of polyunsaturated fatty acid in the membrane, which is considered to enhance the process of carcinogenesis [16]. MDA level was found to be decreased after surgery. This clearly indicates that surgical intervention has reduced fatty acid peroxidation in BPH patients, or it could be due to enhanced activities of free radical scavenging enzymes and GSH levels as observed in post-op patients.
However, the mere presence of damage is not proof of a causative link. Although, given the close link between ROS formation and oxidative DNA damage and the importance of DNA damage and mutation in carcinogenesis; it is not a large leap of intuition to link oxidative DNA lesions and cancer. If oxygen radicals do lead to poorer prognosis, then antioxidant may be of therapeutic value, as observed in breast cancer patients too [17]. High plasma concentrations of antioxidants, such as vitamin E, carotenoids and lycopene, have been reported to correlate with reduced DNA damage and low prostate specific antigen concentrations in prostate cells after prostatectomy [18, 19].
Conclusion
Oxidative DNA damage is likely to play an important role in prostate hyperplasia as depicted by decreased activities of free radical scavenging enzymes and glutathione levels, which might have enhanced DNA damage leading to BPH. Thus management of oxidative stress can be of importance in preventing the occurrence and treatment of BPH with the help of diet rich in vitamin A, C, E and various other antioxidants, so that oxidative stress to the tissues is reduced. However, a great deal of work remains to be completed in defining the exact roles of oxidative DNA damage in the pathogenesis of disease. With this established, it might be possible to determine how modulation of DNA repair and management of oxidative stress, might be useful in disease prevention and therapy.
References
- 1.Nelson WG, Marzo AM, Isaacs WB. Prostate cancer. N Engl J Med. 2003;349:366–381. doi: 10.1056/NEJMra021562. [DOI] [PubMed] [Google Scholar]
- 2.Malins DC, Johnson PM, Barker EA, Polissar NL, Wheeler TM, Anderson KM. Cancer-related changes in prostate DNA as men age and early identification of metastasis in primary prostate tumors. Proc Natl Acad Sci USA. 2003;100:5401–5406. doi: 10.1073/pnas.0931396100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ripple MO, Henry WF, Rago RP, et al. Prooxidant–antioxidant shift induced by androgen treatment of human prostate carcinoma cells. J Natl Cancer Inst. 1997;89(1):40–48. doi: 10.1093/jnci/89.1.40. [DOI] [PubMed] [Google Scholar]
- 4.Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978;52:302–310. doi: 10.1016/S0076-6879(78)52032-6. [DOI] [PubMed] [Google Scholar]
- 5.Marklund SL. Extracellular superoxide dismutase in human tissues and human cell lines. J Clin Invest. 1984;74:1398–1403. doi: 10.1172/JCI111550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Claiborne A. Catalase activity. In: Green Wald RA, editor. CRC handbook of methods for oxygen radical research. Boca Raton: CRC Press; 1985. p. 283–4.
- 7.Carlberg I, Mannervik B. Purification and characterization of the flavoenzyme glutathione reductase from rat liver. J Biol Chem. 1975;250:5475–5480. [PubMed] [Google Scholar]
- 8.Habig WH, Pabst MJ, Jacoby WH. Glutathione-S-transferases: the first step in mercapturic acid formation. J Biol Chem. 1974;249:7130–7139. [PubMed] [Google Scholar]
- 9.Jollow DJ, Mitchell JR, Zampaglione N, Gillete JR. Bromobenzene induced liver necrosis: protective role of glutathione and evidence for 3,4-bromobenzene oxide as the hepatotoxic intermediate. Pharmacology. 1974;11:151–169. doi: 10.1159/000136485. [DOI] [PubMed] [Google Scholar]
- 10.Singh NP, McCoy MT, Tice RR, Schneider EL. A simple technique for quantitation of low levels of DNA damage in individual cells. Exp Cell Res. 1988;175:184–191. doi: 10.1016/0014-4827(88)90265-0. [DOI] [PubMed] [Google Scholar]
- 11.Roy A. Mechanisms of ageing and development. Cell. 2000;124:987–988. [Google Scholar]
- 12.Taplin ME, Ho SM. Clinical review 134: the endocrinology of prostate cancer. J Clin Endocrinol Metab. 2001;86:3467–3477. doi: 10.1210/jc.86.8.3467. [DOI] [PubMed] [Google Scholar]
- 13.McConnell JD. Prostatic growth: new insights into hormonal regulation. Br J Urol. 1995;76(Suppl 1):5–10. [PubMed] [Google Scholar]
- 14.McConnell JD, Barry MJ, Bruskewitz RC, et al. Benign prostatic hyperplasia: diagnosis and treatment. Clinical practice Guideline, number 8. Rockville: Agency for Health Care Policy and Research. Public Health Service, U.S. Department of Health and Human Services; 1994. [PubMed]
- 15.Fleshner NE, Klotz LH. Diet, androgens, oxidative stress and prostate cancer susceptibility. Cancer Metastasis Rev. 1998–1999;17(4):325–30. [DOI] [PubMed]
- 16.Bergendi L, Benes L, Ferencik M. Chemistry, physiology and pathology of free radicals. Life Sci. 1999;65:1865–1874. doi: 10.1016/S0024-3205(99)00439-7. [DOI] [PubMed] [Google Scholar]
- 17.Suhail N, Bilal N, Khan HY, Hasan S, Sharma S, Khan F, Mansoor T, Banu N. Effect of vitamins C and E on antioxidant status of breast-cancer patients undergoing chemotherapy. J Clin Pharm Ther. 2012;37(1):22–26. doi: 10.1111/j.1365-2710.2010.01237.x. [DOI] [PubMed] [Google Scholar]
- 18.Albanes D, Heinonen OP, Huttunen JK, et al. Effects of alpha-tocopherol and beta-carotene supplements on cancer incidence in the alpha-tocopherol beta-carotene cancer prevention study. Am J Clin Nutr. 1995;62(Suppl 6):1427S–1430S. doi: 10.1093/ajcn/62.6.1427S. [DOI] [PubMed] [Google Scholar]
- 19.Gann PH, Ma J, Giovannucci E, et al. Lower prostate cancer risk in men with elevated plasma lycopene levels: results of a prospective analysis. Cancer Res. 1999;59:1225–1230. [PubMed] [Google Scholar]