Abstract
Objectives. We compared health outcomes for adults with the General Equivalency Diploma (GED) and regular high school diploma to determine whether GED recipients are equivalent to regular graduates despite research that documents their disadvantages in other outcomes.
Methods. We used 1997 to 2009 National Health Interview Survey cross-sectional data on high school dropouts, graduates, and GED recipients aged 30 to 65 years (n = 76 705). Five general health indicators and 20 health conditions were analyzed using logistic models.
Results. GED recipients had a significantly higher prevalence of every health outcome compared with high school graduates (odds ratios = 1.3–2.7). The GED–high school differences attenuated but remained evident after controlling for health insurance, economic status, and health behaviors. For most conditions, the 95% confidence interval for GED earners overlapped with that for high school dropouts.
Conclusions. The high school equivalency diploma was associated with nonequivalent health: adults with a GED had health comparable to that of high school dropouts, not graduates. GED recipients were at increased risk for many health conditions, and their health should be viewed as distinct from regular graduates. The findings have implications for health and educational policies.
The General Equivalency Diploma (GED) has been available since 1942 as a credential certifying the completion of secondary education, an alternative to a regular high school graduation. The annual number of recipients has been increasing steadily to about half a million in recent years, representing between 10% and 25% of all high school credentials.1–3 A typical test taker is about 25 years old. Approximately 40% of the diplomas are awarded to women, 60% to Whites, and about 18% each to Black and Hispanic adults.4 Over the course of the past 70 years, 18 million adults have earned the GED.4
The GED's value is predicated on the assumption that the degree is comparable to the regular high school diploma. Most population and education statistics, for instance, count GED recipients together with regular graduates.5,6 In some ways, this equivalence assumption is true. The knowledge and cognitive skills required of successful GED test takers are comparable to those of regular graduates.1 College admission procedures almost uniformly accept the GED as a marker of the completion of secondary education.7
In numerous important ways, however, research showed that the outcomes of the GED recipients are not equivalent to those of regular high school graduates. Two benchmark studies published in the 1990s established that adults with a GED had consistently and considerably worse labor market outcomes than regular graduates.8,9 More than a dozen studies since then have corroborated this difference.10–12 Additionally, researchers also documented the GED disadvantage in outcomes such as lower college completion rates,1 higher attrition from the military,9 higher crime rates,13 and higher rates of substance use.13
Little if anything is known about the health of adults with a GED, despite the fact that the links between education in general and health were studied extensively.14–16 One reason why health outcomes among GED recipients had been neglected is that until recently, few representative health surveys distinguished between a GED and a regular high school diploma. Recently, some researchers began examining health-related outcomes. GED recipients were found to have higher rates of smoking and alcohol use compared with graduates,17,18 and possibly also higher rates of depression.13,19 A recent study of mortality found that GED earners had higher risks of dying than regular graduates,20 although only among younger cohorts.
We compared GED and regular high school recipients using 25 health outcomes in a large, nationally representative sample of US working-aged adults. In addition to the GED–high school comparison, we also included high school dropouts in our analyses. GED recipients were assumed to be equivalent to high school graduates in knowledge and ability. In 2 key aspects, however, adults with GEDs were more comparable to high school dropouts: both groups attended school for about 10 years, on average,9 and both groups made the decision to drop out of high school before completion. The inclusion of dropouts allowed us to better describe where the GEDs fall: are they equivalent to high school graduates as they theoretically can be expected to be on the basis of their credentials, or are they similar to the dropouts, to whom they can be compared on the basis of years of schooling and the decision to discontinue secondary schooling?
METHODS
We used the National Health Interview Surveys (NHIS) data collected from 1997 to 2009. The NHIS comprises annual cross-sectional household surveys. The total household response rate exceeded 90% in the earlier interview years; it declined to 82% by 2009.21 Complex sampling design was used to obtain a sample representative of the civilian noninstitutionalized US population. Since 1997, the NHIS question about the highest completed level of schooling has disaggregated regular high school completion versus the GED. We obtained the data via the Integrated Health Interview Surveys, an aggregated source of NHIS compiled by the Minnesota Population Center.22
We defined the analysis sample as US-born adults aged 30 to 65 years who reported their education as 9 to 12 years (high school dropouts), GED, or a high school diploma. The age range (30 to 65 years) was chosen to focus on a working-aged population before the ages when mortality selection complicates drawing conclusions. Respondents who reported having completed any postsecondary education or less than 9 years of education were excluded from analyses. Additional analyses (not shown here because of space constraints but available on request) showed a familiar gradient, whereby adults with 0 to 8 years had worse health than did those with any secondary schooling, and adults with postsecondary schooling generally had better health, especially those with a bachelor's degree or more. The final analytic sample included 76 705 respondents.
Variables
The main predictor was education, categorized as high school completion, GED, or high school dropout. The dropouts included respondents who reported completing 9 to 12 years of schooling but had no credentials.
Outcomes included 20 health conditions and 5 summary health measures. We used all available outcomes that have been collected continuously since 1997. All measures were self-reported and dichotomous (except self-rated health and bed days, which we dichotomized from 5-point scales for easier interpretation). The conditions ranged from acute illnesses (e.g., cold) to chronic conditions (e.g., hypertension). The summary health measures were self-rated health, activity limitations, functional limitations, needing help with activities of daily living, and more than 8 bed days in the previous year. Appendix A (available as a supplement to the online version of this article at http://www.ajph.org) describes the 25 outcomes in detail. On average, correlation among pairs of outcomes was 0.31, and only a single pair (heart attack and heart disease) exceeded 0.8.
Control variables included in all models were age (continuous, centered on mean of 47 years), gender (male = reference), race/ethnicity (non-Hispanic White = reference, non-Hispanic Black, Hispanic, and “Other”), and the year of interview (continuous, centered on mean year 2003). Marital status was coded as married (reference), widowed, divorced, and never married. We also included 3 sets of measures capturing the main pathways through which education and heath were thought to be linked: access to health care, economic status, and health behaviors.15,16 Health insurance was categorized as insured (reference) versus not insured. Poverty/income ratio was categorized from the ratio of a family's income to the federally defined poverty threshold as low (< 250% of the poverty line), medium (250%–450% of the poverty line), and high (reference, > 450% of the poverty line). Employment status was a nominal variable coded as employed (reference), unemployed, or not in labor force. Smoking was categorized as never smoked (reference), former smoker, and current smoker. Alcohol use was coded as never, former use, and current moderate to light use (reference), and current heavy use. Body size was captured using body mass index (BMI; defined as weight in kilograms divided by the square of height in meters), calculated from self-reported height and weight and used in models as a dichotomous indicator coded as nonobese (reference; BMI < 30) versus obese (BMI ≥ 30).
Analyses
First, univariate and bivariate descriptives summarized the variables in the sample. To compare their distribution across the 3 education groups, we used a design-based F test (Pearson χ2 test of independence corrected for the complex survey sampling design). Second, we estimated a series of 25 logistic models of each outcome on education, controlling for age, gender, race/ethnicity, and the year of interview, to obtain the gross differences in health by the 3 schooling levels. We also estimated the models by gender and age, an important validity check, given that the effect of education on health in general was known to vary across these key demographic groups.1,23–25 The results are presented in Appendix B (available as a supplement to the online version of this article at http://www.ajph.org). Finally, we estimated a nested series for each health outcome, controlling for basic demographics plus (1) health insurance, (2) economic factors, (3) health behaviors, and (4) all covariates together. All multivariate results were presented graphically, as odds ratios (ORs) and 95% confidence intervals (CIs) for the effect of GED and dropout relative to the reference category, high school diploma (tables with complete results are available as a supplement to the online version of this article at http://www.ajph.org).
There were no missing data on basic demographic variables. All other control variables were categorical, and we included a category of “unknown” to avoid deleting cases. Most variables had a low proportion of missing observations, ranging from 0.2% for employment status to 4.8% for obesity information. Poverty/income ratio was an exception, with 20% missing values. All analyses were adjusted for complex sampling design using the svy suite of commands in Stata version 11.0 (StataCorp LP, College Station, TX).
RESULTS
Table 1 shows the distribution of variables by education. For all 25 health indicators, there were significant differences across the 3 education groups: high school graduates had a lower prevalence of all conditions and general health problems than did GED recipients or dropouts. The latter 2 groups were relatively similar; for about half the outcomes, the GED group had a lower prevalence of health than the dropout group. The distribution of demographic, socioeconomic, and lifestyle factors also varied significantly across the education groups. The high school graduates had a more “advantageous” distribution of covariates than did the other 2 education groups: they were more likely to have health insurance, be employed, have higher family income, have healthy body weight, not smoke, and not use alcohol heavily. With regard to most measures, high school dropouts were somewhat disadvantaged relative to GED recipients. A notable exception was smoking; more GED recipients were current or former smokers than were dropouts.
TABLE 1—
Characteristics of the Analysis Sample (n = 76 705) by Education: United States, National Health Interview Surveys, 1997–2009
| Education |
|||||
| Total, % or Mean (SE) | 9–12 Years, % or Mean (SE) | GED, % or Mean (SE) | HS Graduate, % or Mean (SE) | P | |
| Total | 22.1 | 7.9 | 70.0 | ||
| Health conditions | |||||
| Hypertension | 30.0 | 35.1 | 32.4 | 28.1 | < .001 |
| Coronary heart disease | 3.6 | 5.1 | 4.4 | 3.1 | < .001 |
| Heart attack | 3.4 | 5.0 | 4.4 | 2.7 | < .001 |
| Heart condition | 7.2 | 8.6 | 9.2 | 6.5 | < .001 |
| Emphysema | 2.3 | 4.2 | 3.8 | 1.6 | < .001 |
| Asthma | 10.5 | 13.2 | 14.7 | 9.2 | < .001 |
| Chronic bronchitis, 12 mo | 6.4 | 8.7 | 9.2 | 5.3 | < .001 |
| Cancer (ever) | 6.2 | 6.7 | 7.9 | 5.9 | < .001 |
| Diabetes | 9.5 | 12.1 | 11.5 | 8.5 | < .001 |
| Ulcer | 10.1 | 12.9 | 14.0 | 8.8 | < .001 |
| Stroke | 2.4 | 3.9 | 3.0 | 1.9 | < .001 |
| Failing kidneys, past y | 1.8 | 2.9 | 2.5 | 1.4 | < .001 |
| Liver condition, past y | 1.9 | 2.6 | 3.7 | 1.4 | < .001 |
| Sinusitis in past 12 mo | 17.0 | 17.8 | 19.3 | 16.5 | < .001 |
| Cold in past 2 wk | 13.5 | 16.3 | 15.5 | 12.5 | < .001 |
| Intestinal problem, 2 wk | 5.8 | 6.9 | 8.2 | 5.2 | < .001 |
| Lower back pain, 3 mo | 33.4 | 38.7 | 42.1 | 30.8 | < .001 |
| Migraine, past 3 mo | 18.1 | 21.5 | 24.2 | 16.4 | < .001 |
| Neck pain, past 3 mo | 18.0 | 20.6 | 24.2 | 16.5 | < .001 |
| Vision problems | 11.4 | 14.9 | 16.0 | 9.8 | < .001 |
| General health | |||||
| Any functional limitations | 38.2 | 46.7 | 47.3 | 34.5 | < .001 |
| Any activity limitations | 20.6 | 30.1 | 27.9 | 16.7 | < .001 |
| Needs help with ADLs | 1.7 | 2.6 | 2.1 | 1.4 | < .001 |
| > 8 bed d | 10.1 | 14.0 | 15.0 | 8.3 | < .001 |
| Poor/fair health | 17.9 | 29.0 | 24.2 | 13.7 | < .001 |
| Sample characteristics | |||||
| Interview year | 2002.8 (0.03) | 2002.7 (0.05) | 2003.1 (0.07) | 2002.9 (0.03) | < .001 |
| Age, y | 47.0 (0.04) | 47.5 (0.09) | 45.7 (0.15) | 47.0 (0.05) | < .001 |
| Female | 53.6 | 53.4 | 51.7 | 53.8 | .019 |
| Race/ethnicity | < .001 | ||||
| Non-Hispanic White | 77.6 | 67.0 | 78.5 | 80.8 | |
| Non-Hispanic Black | 15.9 | 23.8 | 12.5 | 13.8 | |
| Hispanic | 5.1 | 7.5 | 7.1 | 4.1 | |
| Other | 1.5 | 1.8 | 2.0 | 1.3 | |
| Married | 52.8 | 44.8 | 46.8 | 56.0 | < .001 |
| Health insurance | < .001 | ||||
| Uninsured | 17.4 | 23.9 | 23.1 | 14.6 | |
| Insured | 82.3 | 75.8 | 76.6 | 85.0 | |
| Unknown | 0.3 | 0.3 | 0.3 | 0.3 | |
| Employment | < .001 | ||||
| Employed | 68.0 | 55.3 | 63.2 | 72.6 | |
| Unemployed | 3.3 | 4.5 | 5.6 | 2.7 | |
| Not in LF | 28.5 | 40.1 | 31.2 | 24.5 | |
| Unknown | 0.2 | 0.1 | 0.1 | 0.2 | |
| Income categorya | < .001 | ||||
| Low | 36.2 | 51.6 | 49.2 | 29.9 | |
| Medium | 26.1 | 19.8 | 23.2 | 28.5 | |
| High | 17.7 | 9.6 | 11.4 | 21.0 | |
| Unknown | 20.0 | 19.0 | 16.2 | 20.7 | |
| Body weightb | < .001 | ||||
| Not obese | 65.7 | 63.3 | 63.5 | 66.8 | |
| Obese | 29.5 | 32.6 | 32.3 | 28.2 | |
| Unknown | 4.8 | 4.1 | 4.3 | 5.0 | |
| Smoking | < .001 | ||||
| Never smoked | 40.5 | 32.5 | 24.7 | 44.9 | |
| Past smoker | 22.2 | 20.8 | 22.9 | 22.6 | |
| Current smoker | 36.2 | 45.9 | 51.6 | 31.4 | |
| Unknown | 1.0 | 0.9 | 0.8 | 1.1 | |
| Alcohol use | < .001 | ||||
| Never | 18.7 | 22.0 | 15.4 | 18.1 | |
| Former | 19.3 | 23.4 | 23.1 | 17.5 | |
| Current moderate use | 55.0 | 47.0 | 53.5 | 57.6 | |
| Current heavy use | 4.4 | 5.1 | 5.9 | 4.0 | |
| Unknown | 2.6 | 2.5 | 2.0 | 2.7 | |
Note. ADLs = activities of daily living; GED = graduate equivalency diploma; HS = high school; LF = labor force. Participants were US-born adults aged 30–65 years. Adjusted for sampling design.
Income categorized from the ratio of a family's income to the federally defined poverty threshold as low (< 250% of the poverty line), medium (250%–450% of the poverty line), and high (> 450% of the poverty line).
Body weight calculated from self-reported height and weight and used in models as a dichotomous indicator coded as nonobese (body mass index [BMI] < 30 kg/m2) versus obese (BMI ≥ 30 kg/m2).
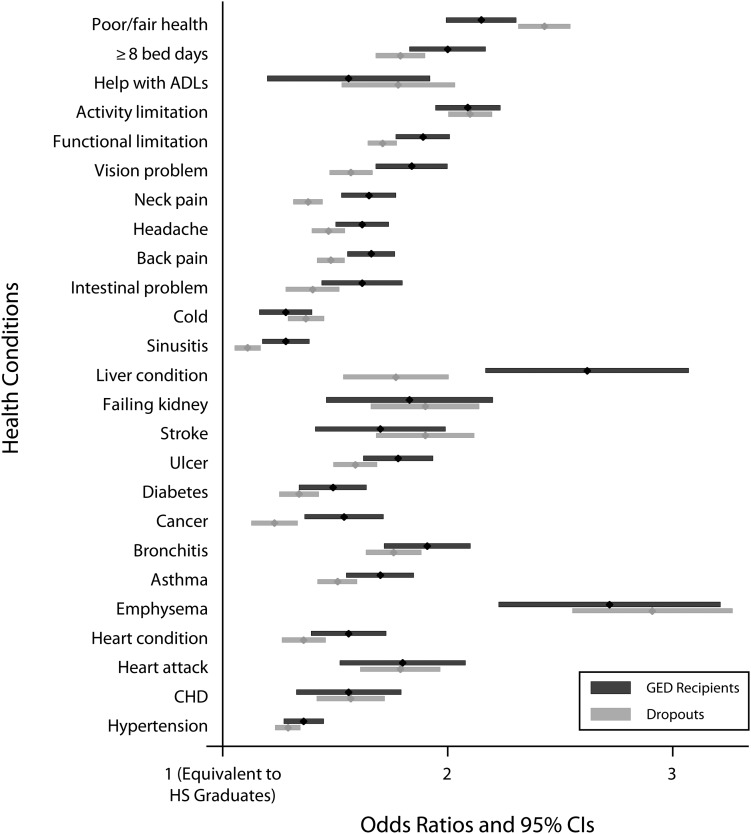
Next, we estimated logistic regression models of each health outcome on GED and dropout indicators relative to the reference (high school graduates), controlling for key demographic characteristics (age, gender, race/ethnicity, and interview year). ORs and 95% CIs are shown graphically in Figure 1. The first finding was that GED recipients were significantly and substantially more likely to report all 25 health outcomes than were high school graduates. The coefficients ranged from OR = 1.28 (95% CI = 1.18, 1.39) for sinusitis to OR = 2.72 (95% CI = 2.26, 3.26) for emphysema. Second, the GED recipients reported health at best comparable to high school dropouts: for 24 outcomes, the two 95% CIs overlapped or the GED recipients had significantly worse outcomes than did the dropouts. The only exception was self-rated health; dropouts were more likely to report poor or fair health than were GED recipients.
FIGURE 1—
Odds ratios of 25 health indicators for General Equivalency Diploma (GED) and dropouts, relative to high school graduates: United States, National Health Interview Surveys, 1997–2009.
Note: ADLs = activities of daily living; CHD = coronary heart disease; CI = confidence intervals; GED = General Equivalency Diploma; HS = high school. Models adjust for age, gender, race/ethnicity, and the year of interview.
Appendix B shows and briefly discusses results from models stratified by gender and age, the 2 key population characteristics. We estimated these models as validity checks to explore whether the results might be driven primarily by 1 gender or age group. The GED odds ratios were significant in all groups for most outcomes, suggesting that the GED disadvantage was pervasive across different population subgroups.
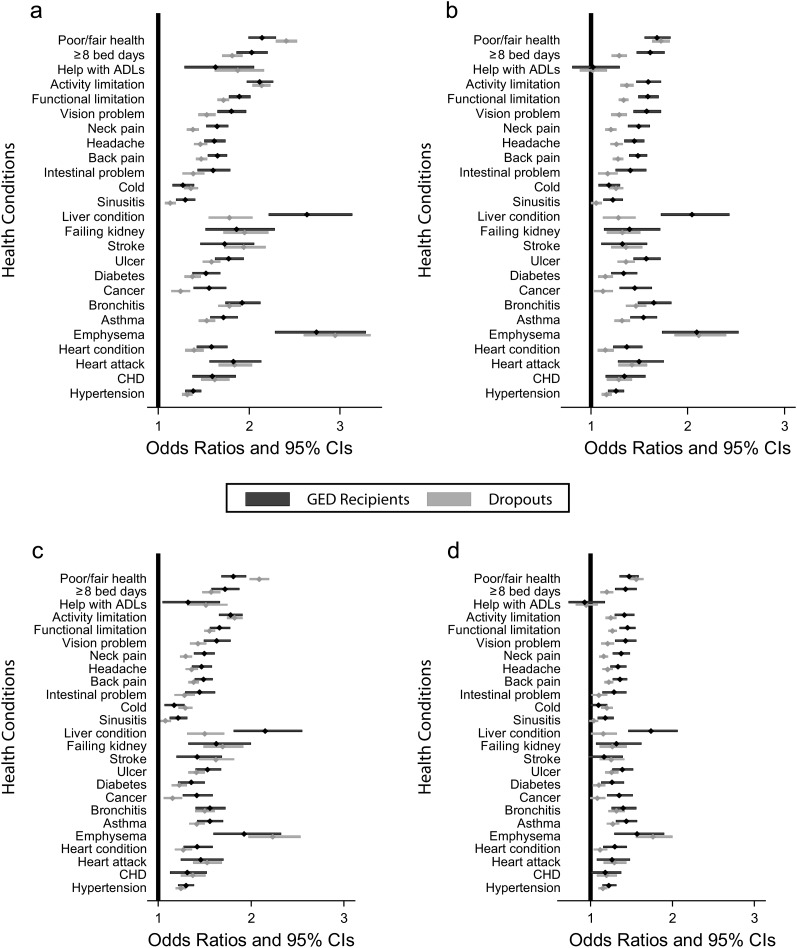
In Figure 2 we adjusted for the different distribution of health insurance (Figure 2a), economic status (Figure 2b), health behaviors (Figure 2c), and all covariates together (column 4 in Table 1). Taking health insurance into account had only a small effect on the GED–high school difference in health. On average, the 25 coefficients attenuated only about 3% (full tables and calculations are available as a supplement to the online version of this article at http://www.ajph.org). Adjusting for economic factors explained a larger proportion (30%) of the group differences; income and employment status had an independent and relatively similar impact on the change in the coefficients. Health behaviors, included in Figure 2c, also explained a sizeable part (about 25%) of the GED–high school difference. Of the 3 health behaviors we studied, smoking had a larger explanatory power than obesity or alcohol use on the GED–high school difference for most outcomes. Finally, we included all 3 sets of covariates in models shown in Figure 2d. Jointly, these covariates explained about 50% of the GED disadvantage. However, the GED–high school difference was not significant or only marginally significant in only 4 of the 25 outcomes, As shown in Figure 2, the GED recipients were either comparable to dropouts or worse off for every examined outcome, except self-rated health (Figure 2c).
FIGURE 2—
Odds ratios of 25 health indicators for GED and dropouts, relative to high school graduates, adjusted for (a) health insurance, (b) economic status, (c) health behaviors, and (d) all covariates: United States, National Health Interview Surveys, 1997–2009.
Note. ADLs = activities of daily living; CHD = coronary heart disease; CI = confidence interval; GED = General Equivalency Diploma.
DISCUSSION
The GED credential was designed to be equivalent to a regular high school diploma. It was treated as such in multiple spheres, from the collection of educational data to college admission procedures. Increasingly, however, research showed that GED recipients were worse off than were high school graduates in various outcomes, from the labor market to college completion rates. A surprising gap in this literature was health, one of the most important outcomes linked to education.
This study examined whether working-aged GED earners had health that was equivalent to the health of regular high school graduates, or whether it was closer to that of dropouts, who resembled the GED earners in not completing regular secondary schooling. We studied 25 health indicators, from chronic conditions to acute illness and multiple general health indicators. Compared with regular high school graduates, the adult GED recipients were significantly and substantially worse off in all outcomes. They were 30% to more than 250% more likely to report various health conditions and about twice as likely to report functional limitations, activity limitations, or poor or fair health. The GED–high school difference was smaller for acute illnesses like recent cold or sinusitis and larger for conditions associated with specific health behaviors like alcohol use and smoking (liver disease and emphysema, respectively). The GED disadvantage was evident in both genders, as well as among younger and older adults.
Taking into account previously documented economic and lifestyle differences between GED recipients and regular graduates1,8,9,17,18 explained about half of the health differentials, although the gaps remained significant for most outcomes. Income, employment status, and smoking had the most explanatory impact, whereas the lower rate of health insurance among GED earners played only a minor role in health inequality.
Additionally, adults with a GED were statistically indistinguishable from high school dropouts for most outcomes. With the exception of self-rated health, where dropouts were more likely to report fair or poor health, GED recipients reported health conditions and limitations at least as frequently as the dropout group.
The disadvantage of GED recipients relative to high school graduates and the GED earners similarity to high school dropouts generally corroborated econometric and educational literature, which considered other outcomes like labor market or tertiary education. With respect to health conditions, we were aware of only 1 previous study (with a relatively small sample of adults aged 40–45 years) in which the author analyzed the sum of illnesses and found that GED recipients reported a comparable number of illnesses as high school graduates.19 It was not clear why these results differed from ours—perhaps there was insufficient power in the analyses because of the modest sample size.
The key question was why were adults with a GED so much worse off than high school graduates in terms of health—why, despite the assumption of credential equivalency, do they resemble the dropout group instead? We could draw on 3 models linking schooling and health in an attempt to explain this discrepancy: the quantity model, the credential model, and the selection model. In the social determinants of health literature, the first 2 models were proposed in the late 1990s.15,26 The quantity model, related to the human capital model in econometrics,27,28 suggested that schooling develops skills, abilities, and resources that enable individuals to achieve a healthy life.15,29 Under the credential model, it was argued that a diploma opened occupational pathways that lead to a corresponding social and economic status, which in turn influences health. An alternative perspective was recently proposed by Heckman et al.,1 Cameron and Heckman,8 and Heckman and Rubinstein30 specifically to understand the GED–high school differences in various outcomes. They argued that GED recipients differed from regular graduates in noncognitive characteristics like persistence in reaching goals, self-efficacy, or the ability to delay gratification.30–32 Heckman et al.1,12 proposed that the limitations within these personality characteristics caused the GED earners to drop out of high school in the first place, and also affected their outcomes in later life. Unlike the quantity or credential models that assume a causal effect of schooling on health, this is a selection argument, suggesting that individual (noncognitive) characteristics determine both their educational outcome, as well as their adult health status.
Although our study could not directly discriminate among these models, our results could provide suggestive evidence that could inform the theoretical developments. In support of the quantity model, GED recipients might have worse health than graduates because they attended school for a shorter period of time—about a mean of 2 years less than regular graduates.9 It was unclear how this quantity deficit might operate, however, because GED recipients and regular graduates demonstrated comparable cognitive skills and knowledge.1,32 Regarding the credential model, numerous econometric studies showed that the GED was not an equivalent credential in the labor market. To the degree that the nonequivalence occurs in other social markets,1,10,12 or that the labor market outcomes play an important role in adult health, our results were also consistent the credentialing perspective. Some argued that the GED gives a “mixed signal,” marking comparable cognitive but lesser noncognitive skills to potential employers.30 Of course, this nonequivalence of the GED directly contradicted the premise underlying the existence of the GED testing program. Finally, our findings were also not inconsistent with the selection perspective. It was quite possible that the GED recipients had lower noncognitive skills such as persistence, which might have caused them to drop out of high school and also affected their health. The selection perspective might also help explain why the GED recipients had a higher prevalence of some conditions like liver disease, back pain, or neck pain than did high school dropouts. Perhaps for these outcomes, the noncognitive skills might be particularly important, such as the ability to maintain a healthy level of alcohol use, affecting liver disease. Another possibility was that the different personality characteristics affected health reporting in the GED group, making them more likely to report chronic pain than the dropout group.
We speculated on possible reasons for our findings, but additional data would be necessary to provide firm explanations. It would be desirable to have information on the adults’ cognitive and noncognitive skills for a direct test of the selection hypothesis. Additionally, it is important to gain a better understanding of reasons why high school dropouts choose to take the GED test. At the test sites, the test takers reported educational and employment reasons,4,33 but more detail might shed light on the characteristics of the GED recipients, which would be helpful to understand their lower-than-expected health. Another avenue for further research is to expand the theoretical framework linking educational attainment and health. We mainly considered access to health care, economic status, and health behaviors. Because of data constraints, we omitted a wide range of other factors, such as social environment and physical environment, as well as information about genetic endowment, which were posited in literature as important determinants of health.34 Testing a broader range of explanatory factors promises to identify additional pathways through which the GED and other credentials translate into adult health.
The relatively poor health of GED earners has clear implications for public health debates as well as for further research on health inequalities by education. The number of US adults who report the GED as their highest schooling credential is between 5 and 8 million. It is telling that the precise number is unknown—GEDs are simply counted as high school diplomas in the US Census, National Center for Educational Statistics, and other major data collection agencies.6,35 A necessary first step to learning more about the outcomes of the GED recipients is to collect information about GED as separate from a regular diploma. Understanding the health outcomes of this large group will contribute to educational policies currently aimed at decreasing high school attrition and increasing the number of GED test takers among dropouts. Our results showed that the worse health outcomes of GED recipients were partly a result of their worse health behaviors, especially smoking, but also obesity and alcohol use. This finding suggested a direct avenue for interventions: stepped-up efforts to reach adults who earned a GED with smoking cessation or weight loss programs. Finally, the findings also matter within the continued critical discussion about the benefits and merits of the GED by documenting that one of the most desirable resources (health) did not seem to improve when dropouts earned a GED. Policy efforts to decrease the high school dropout rate might be more important to long-term health than helping dropouts earn a GED.
Acknowledgments
The author wishes to thank Bethany G. Everett, Zhenchao Qian, Jennifer E. Glick, Matthew Painter, and anonymous reviewers for their helpful comments.
Human Participant Protection
This study is based on a secondary analysis of publicly available data so institutional review board approval for protection of participants was not needed.
References
- 1.Heckman JJ, Humphries JE, Mader NS. The GED. : NBER Working Paper Series. Cambridge, MA: NBER; 2010 [Google Scholar]
- 2.Snyder TD, Dillow SA. Digest of Education Statistics 2009 (NCES 2010-013). Washington, DC: National Center for Education Statistics, Institute of Education Sciences, US Department of Education; 2010 [Google Scholar]
- 3.Tyler J, Lofstrom M. Is the GED an effective route to postsecondary education for school dropouts? Econ Educ Rev. 2010;29(5):813–825 [Google Scholar]
- 4.American Council on Education 2009 GED Testing Program Statistical Report. Washington, DC: GED Testing Service, American Council on Education; 2010 [Google Scholar]
- 5.Planty M, Hussar W, Snyder T, Kena G, KewalRamani Aet al. The Condition of Education 2009 (NCES 2009-081). Washington, DC: National Center for Education Statistics IoES, US Department of Education; 2009 [Google Scholar]
- 6.Snyder TD, Dillow SA. Digest of Education Statistics 2010 (NCES 2011-015. Washington, DC: National Center for Education Statistics, Institute of Education Sciences, US Department of Education; 2011 [Google Scholar]
- 7.American Council on Education GED Testing Program Statistical Report. Washington, DC: 2009. Available at: http://www.acenet.edu/Content/NavigationMenu/ged/pubs/2009ASR.pdf. Accessed February 10, 2012 [Google Scholar]
- 8.Cameron SV, Heckman JJ. The nonequivalence of high school equivalents. J Labor Econ. 1993;11(1):1–47 [Google Scholar]
- 9.Boesel D, Alsalam N, Smith TM. Educational and Labor Market Performance of GED Recipients: Research Synthesis. Washington, DC: National Library of Education, Office of Educational Research and Improvement, US Department of Education; 1998 [Google Scholar]
- 10.Tyler JH. Economic benefits of the GED: lessons from recent research. Rev Educ Res. 2003;73(3):369–403 [Google Scholar]
- 11.Tyler JH, Murnane RJ, Willett JB. Who benefits from a GED? Evidence for females from high school and beyond. Econ Educ Rev. 2003;22(3):237–247 [Google Scholar]
- 12.Heckman JJ, LaFontaine PA. Bias-corrected estimates of GED returns. J Labor Econ. 2006;24(3):661–700 [Google Scholar]
- 13.Ou S-R Do GED recipients differ from graduates and school dropouts? Findings from an inner-city cohort. Urban Educ. 2008;43(1):83–117 [Google Scholar]
- 14.Ross CE, Wu CL. The links between education and health. Am Sociol Rev. 1995;60(5):719–745 [Google Scholar]
- 15.Mirowsky J, Ross CE. Education, Social Status, and Health. New York: Aldine de Gruyter; 2003 [Google Scholar]
- 16.Cutler DM, Lleras-Muney A. Education and health: evaluating theories and evidence. : Schoeni RF, House JS, Kaplan GA, Pollack H, Making Americans Healthier: Social and Economic Policy as Health Policy. New York, NY: Russel Sage Foundation; 2008: 29–60 [Google Scholar]
- 17.Kenkel D, Lillard D, Mathios A. The roles of high school completion and GED receipt in smoking and obesity. J Labor Econ. 2006;24(3):635–660 [Google Scholar]
- 18.Schoenborn CA, Adams PF. Health behaviors of adults: United States, 2005-2007. : Vital Health Statistics. Washington, DC: National Center for Health Statistics; 2010 [PubMed] [Google Scholar]
- 19.Caputo RK. The GED as a predictor of mid-life health and economic well-being. J Poverty. 2005;9(4):73–97 [Google Scholar]
- 20.Rogers RG, Everett BG, Zajacova A, Hummer RA. Educational degrees and adult mortality risk in the United States. Biodemography Soc Biol. 2010;56(1):80–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NCHS 2008 NHIS Public Use Data Release: Survey Description. Available at: ftp.cdc.gov/pub/health_statistics/nchs/Dataset_Documentation/NHIS/2009/srvydesc.pdf. Accessed April 19, 2011
- 22.Minnesota Population Center and State Health Access Data Assistance Center Integrated Health Interview Series: Version 2.0. Available at: http://www.ihis.us. Accessed January 31, 2010
- 23.Hill TD, Needham BL. Gender-specific trends in educational attainment and self-rated health, 1972-2002. Am J Public Health. 2006;96(7):1288–1292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu H, Hummer RA. Are educational differences in U.S. self-rated health increasing? An examination by gender and race. Soc Sci Med. 2008;67(11):1898–1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dupre ME. Educational differences in health risks and illness over the life course: a test of cumulative disadvantage theory. Soc Sci Res. 2008;37(4):1253–1266 [DOI] [PubMed] [Google Scholar]
- 26.Ross CE, Mirowsky J. Refining the association between education and health: the effects of quantity, credentials, and selectivity. Demography. 1999;36(4):445–460 [PubMed] [Google Scholar]
- 27.Becker GS. Human Capital: A Theoretical and Empirical Analysis, with Special Reference to Education. New York: Columbia University Press; 1964 [Google Scholar]
- 28.Grossman M. The human capital model. : Anthony JC, Joseph PN, Handbook of Health Economics. New York: Elsevier; 2000:347–408 [Google Scholar]
- 29.Mirowsky J, Ross CE. Education, personal control, lifestyle and health. Res Aging. 1998;20(4):415–449 [Google Scholar]
- 30.Heckman JJ, Rubinstein Y. The importance of noncognitive skills: lessons from the GED testing program. Am Econ Rev. 2001;91(2):145–149 [Google Scholar]
- 31.Heckman JJ. Schools, skills, and synapses. Econ Inq. 2008;46(3):289–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heckman JJ, Stixrud J, Urzua S. The effects of cognitive and noncognitive abilities on labor market outcomes and social behavior. J Labor Econ. 2006;24(3):411–482 [Google Scholar]
- 33.American Council on Education Who Took the GED?: GED 2000 Statistical Report. Annapolis Junction, MD: GED Testing Service, Center for Adult Learning and Educational Credentials, American Council on Education; 2001 [Google Scholar]
- 34.Evans RG, Stoddart GL. Producing health, consuming health care. Soc Sci Med. 1990;31(12):1347–1363 [DOI] [PubMed] [Google Scholar]
- 35.US Census Bureau Statistical Abstract of the United States: 2011. 130th ed. Washington, DC: US Census Bureau; 2011:175, Table 271 [Google Scholar]