Abstract
Objectives. We examined the association of race/ethnicity with mortality risk in a national cohort of US veterans clinically diagnosed with traumatic brain injury.
Methods. Between January 1, 2006 and December 31, 2006, we obtained data from a national cohort study of 7885 non-Hispanic White, 1748 Non-Hispanic Black, 314 Hispanic, and 4743 other or missing race/ethnicity veterans clinically diagnosed with traumatic brain injury in Veterans Affairs medical centers and community-based outpatient clinics.
Results. Overall mortality at 48 months was 6.7% in Hispanic, 2.9% in non-Hispanic White, and 2.7% in non-Hispanic Black veterans. Compared with non-Hispanic White, Hispanic ethnicity was positively associated with a higher mortality risk (hazard ratio [HR] = 2.33; 95% confidence interval [CI] = 1.49, 3.64) in the race/ethnicity-only adjusted model. After adjusting for sociodemographic characteristics and comorbidities, Hispanic ethnicity continued to be positively associated (HR = 1.61; 95% CI = 1.00, 2.58) with a higher mortality risk relative to non-Hispanic White ethnicity.
Conclusions. Hispanic ethnicity is positively associated with higher mortality risk among veterans clinically diagnosed with traumatic brain injury. More research is needed to understand the reasons for this disparity.
Traumatic brain injury (TBI) is one of the signature wounds of the current military operations in Iraq and Afghanistan. Individuals with TBI have been found to be 1.5 times more likely to die than are individuals in the general population of similar age, gender, and race, resulting in an estimated average life expectancy reduction of 4 years.1 For the US civilian population hospitalized and rehabilitated for TBI, the strongest predictors of death 1 year after injury have been found to be increasing age, being male, having less education, having a longer hospitalization, having an earlier year of injury, and being in a vegetative state at discharge to rehabilitation.1 Race/ethnicity has been found to be associated with short-term mortality in the civilian population, with conflicting results for Hispanic civilians according to the study population.2–7
A study using Healthcare Cost and Utilization Project data found that relative to White patients, Black and Asian patients had a higher risk of death.2 A study of 164 abuse patients found that Blacks had a higher risk of mortality after adjusting for covariates despite similar severity of injury.3 A study of 17 977 patients with severe TBI found that Asians had a higher risk of mortality relative to Whites whereas Hispanics and Blacks did not.4 A study of 357 patients with TBI admitted to a level-1 trauma center between 2001 and 2004 found that after adjusting for age and an injury severity score, Asians and Blacks had significantly higher mortality than did Whites, with Hispanics having slightly but not significantly lower mortality.5 A study of 56 482 patients with moderate to severe TBI who were hospitalized in level-1 or -2 trauma-designated hospitals between 2000 and 2003 found that compared with Whites, Blacks and Asians had higher mortality rates, with a trend toward significantly higher mortality for Hispanics.6 Finally, a study of prehospital death founded on case reviews from medical examiner referrals in the Bronx borough of New York City found that race-specific mortality was highest for Blacks, intermediate for Hispanics, and lowest for Whites.7
The US Department of Veterans Affairs (VA) strives to be an equal access system for veterans of all races and ethnicities. A study examining mortality from brain injury in the veteran population was conducted for US World War II veterans. The study found that the presence of posttraumatic epilepsy and lower levels of education were associated with an increased risk of death in a Cox proportional hazard model that did not include race.8 Generally Black and Hispanic veterans have been found to have similar or lower mortality rates than those of White veterans for diabetes,9–12 pneumonia,11,13,14 acute myocardial infarction,14 hip fracture,14 gastrointestinal bleeding,14 congestive heart failure,11,14,15, angina,11 chronic obstructive pulmonary disease,11 and chronic renal failure.11 The literature is mixed regarding stroke. One study found risk-adjusted mortality 30 days after hospitalization to be lower for Black than for White veterans. Yet another study16 found a 20% higher likelihood of death among Blacks in a 6-year period at 1 southeastern VA medical center. The only condition for which minority veterans have been found to have worse mortality without opposing evidence is HIV.17
Given the absence of published evidence regarding race/ethnicity and mortality among veterans with TBI, we sought to test our hypothesis that in an equal access system there will be no racial/ethnic disparities in mortality rates among veterans clinically diagnosed with TBI after controlling for relevant covariates.
METHODS
We identified 14 690 veterans who were seen at VA medical centers and community-based outpatient clinics between January 1, 2006 and December 31, 2006 with clinically diagnosed TBI (diagnosed at any time) using definitions established in a previous VA study that included all International Classification of Diseases, Ninth Revision (ICD-9) codes used by the Center for Disease Control and Prevention as well as ICD-9 codes for postconcussive syndrome and TBI-related late effects mandated by the VA. 18,19
Measurements
We created a national cohort of veterans with TBI by linking multiple patient and administrative files from 2 large VA databases. These 2 databases, the Veterans Health Administration Decision Support System and Vital Status Files, were linked by scrambled social security number. The Veterans Health Administration Decision Support System is a national automated management information system that uses commercial software to integrate data from clinical and financial systems for both inpatient and outpatient care. Veterans with clinically diagnosed TBI were identified on the basis of having an ICD-9 code for TBI (according to VA coding guidelines with a primary diagnosis of 800.xx, 801.xx, 803.xx, 804.xx, 851.xx, 852.xx, 853.xx, 854.xx, or V57.xx along with a TBI secondary diagnosis code of 800.xx, 801.xx, 803.xx, 804.xx, 851.xx, 852.xx, 853.xx, 854.xx, 310.2, 905.0, or 907.0)19 in the patient treatment file. We used the term “clinically diagnosed TBI” to distinguish from the VA primary care TBI screen that was implemented in the VA for all Operation Enduring Freedom and Operation Iraqi Freedom veterans since September 2007. A positive result on the primary screen is only an indicator of possible TBI. A secondary examination by a specialist is required to confirm TBI. We included only veterans with confirmed TBI in this study. We used these criteria to assemble a retrospective cohort of 14 690 veterans who had an ICD-9 code for clinically diagnosed TBI between January 1, 2006 and December 31, 2006. We collected sociodemographic and clinical variables from the patient treatment file. We obtained date of death from the Vital Status File between January 1, 2006 and December 31, 2009. The main outcome measure was time to death, which was defined as months to death between date of entry into the study in 2006 and date of death or December 31, 2009.
Race/ethnicity was determined by self-report and classified as non-Hispanic White, non-Hispanic Black, Hispanic, and other or missing owing to the large number of veterans with missing race. The race and ethnicity of the patient was taken from the VA 2006 Outpatient Medical SAS, version 9.3, (SAS Institute, Cary, NC) data files. Currently, race can be categorized using the variables race (race or national origin) or race1–race7 (race with collection methods). Using the race variable alone produced a data file with approximately 58% of race identified as other or missing. We created an algorithm using both race and race1–race7 variables to decrease this number to approximately 32%.
We compared socioeconomic and clinical variables across racial groups by using the χ2 test for categorical variables. Other risk factors (covariates) included age, marital status, gender, service connectedness (had a service-related condition), urban residence, VA region of residence, insurance status, and ICD-9–coded comorbidities (substance abuse, anemia, cancer, heart disease, depression, hypertension, hypothyroidism, lung disease, liver disease, and psychoses). Age was categorized into 4 groups (< 50, 50–64, 65–74, and ≥ 75 years). Marital status was classified as married or nonmarried. Gender was classified as male or female.
Service connectedness is the percentage of disability a veteran incurred while in military service. It can range from 0% to 100%. We classified veterans in our study as service connected or nonservice connected. Urban residence was classified as urban or nonurban. VA region of residence was classified into 5 categories: northeastern, mid-Atlantic, southern, midwestern, and western. Insurance status was classified as VA only, Medicare, or private insurance. Important comorbidity variables with high prevalence were defined on the basis of enhanced ICD-9 codes using validated algorithms (substance abuse disorder 303.9, 304.xx, or 305.xx; anemia 280.0, 648.20–648.24, 280.1–281.9, 285.21–285.29, or 285.9; cancer 140.xx–208.xx; coronary heart disease 410.xx–414.xx; depression 300.4, 301.12, 309.0, 309.1, or 311.xx; hypertension 401.xx–405.xx; hypothyroidism 243.xx–244.2, 244.8, or 244.9; lung disease 490.xx–492.8, 493.00–493.92, 494.xx–494.1, 495.0–505.xx, 506.4, 415.11–415.19, 416.0–416.9, or 417.9; liver disease 070.22, 070.23, 070.32, 070.33, 070.44, 070.54, 456.0, 456.1, 456.20, 456.21, 571.0, 571.2, 571.3, 571.40–572.49, 571.5, 571.6, 571.8, 571.9, 572.3, 572.8, or V427.xx; psychoses 295.1, 295.2, 295.3, 295.4, 295.6, or 295.7).20
Statistical Methods
In preliminary analyses, we examined crude associations between mortality and all measured covariates in our study population of veterans with clinically diagnosed TBI by using the χ2 test for categorical variables. We used Cox regression methods to model the association between race and time to death. Time to death was defined as the number of months from time of entry into the study in 2006 until time of death or censoring (December 31, 2009). Death was coded as 1 if death occurred and 0 if censored. We created 3 models to provide hazard ratios (HRs) for mortality risk, all adjusted by race/ethnicity and then sequentially by a specific set of covariates. We adjusted the first model for race/ethnicity only, the second model for race/ethnicity and a set of sociodemographic variables, and the third model for race and sociodemographic and comorbid conditions. We used the Kaplan-Meier method to plot the survival function. We conducted all data analyses using SAS version 9.1.3 (SAS Institute, Cary, NC).21
RESULTS
Table 1 shows sociodemographic and clinical characteristics of the study cohort by racial/ethnic group. Mortality rates significantly differed by race, with 6.69% of Hispanic veterans clinically diagnosed with TBI having died compared with 2.93% of non-Hispanic White veterans during the study period. Age, gender, marital status, service connectedness, urban residence, region of residence, and insurance status all differed significantly by race/ethnicity. Hispanic veterans with clinically diagnosed TBI made up the highest percentages of those aged 65 to 74 years (18.15%) and 75 years and older (26.11%), men (98.73%), those who were married (51.91%), those with service connectedness (50.64%), those living in urban areas (90.76%), those living in the southern region (62.74%), and those who had Medicare coverage (33.76%). Hispanic veterans had the lowest percentage of those aged 50 to 64 years (36.94%) and younger than 50 years (18.79%); those living in the northeastern (4.78%), Atlantic (1.27%), and midwest (10.83%) regions; and those who had private insurance (6.69%). Despite having the highest death rates, Hispanic veterans had the lowest presence of substance abuse (4.46%), depression (3.50%), hypertension (6.69%), hypothyroidism (0.32%), lung disease (1.27%), and psychoses (1.91%).
TABLE 1—
Sample Characteristics by Race: Racial/Ethnic Disparities in US Veteran Traumatic Brain Injury Mortality, January 1, 2006–December 31, 2009
| Non-Hispanic White, % (n = 7885) | Non-Hispanic Black, % (n = 1748) | Hispanic, % (n = 314) | Other/Race Missing, % (n = 4743) | |
| Died* | 2.93 | 2.69 | 6.69 | 1.37 |
| Age,* y | ||||
| < 50 | 31.68 | 39.53 | 18.79 | 42.72 |
| 50–64 | 43.06 | 46.00 | 36.94 | 38.39 |
| 65–74 | 11.17 | 7.32 | 18.15 | 9.28 |
| ≥ 75 | 14.09 | 7.15 | 26.11 | 9.61 |
| Married* | 41.45 | 28.95 | 51.91 | 41.03 |
| Male* | 94.08 | 92.91 | 98.73 | 90.81 |
| Service connected* | 48.10 | 42.73 | 50.64 | 40.75 |
| Urban* | 62.50 | 85.58 | 90.76 | 66.43 |
| Region* | ||||
| Northeastern | 12.75 | 10.93 | 4.78 | 9.49 |
| Mid-Atlantic | 19.57 | 27.86 | 1.27 | 16.70 |
| Southern | 23.40 | 31.98 | 62.74 | 23.42 |
| Midwestern | 25.29 | 18.99 | 10.83 | 21.95 |
| Western | 18.92 | 10.24 | 20.38 | 28.25 |
| Insurance type | ||||
| VA only insurance* | 55.29 | 70.14 | 59.55 | 65.91 |
| Medicare* | 31.29 | 18.48 | 33.76 | 19.99 |
| Private insurance* | 13.42 | 11.38 | 6.69 | 14.10 |
| Disorders | ||||
| Substance abuse* | 6.01 | 9.84 | 4.46 | 5.36 |
| Anemia | 0.88 | 1.09 | 0.32 | 0.70 |
| Cancer | 1.19 | 0.80 | 0.64 | 0.84 |
| Heart disease | 0.70 | 0.29 | 1.27 | 0.72 |
| Depression* | 6.34 | 4.41 | 3.50 | 6.81 |
| Hypertension* | 11.29 | 11.56 | 6.69 | 11.95 |
| Hypothyroidism* | 1.27 | 0.40 | 0.32 | 1.27 |
| Lung disease* | 2.82 | 1.66 | 1.27 | 2.30 |
| Liver disease | 1.10 | 0.97 | 0.32 | 0.93 |
| Psychoses* | 5.19 | 6.41 | 1.91 | 4.26 |
Note. VA = Veteran's Affairs. The sample size was n =14 690.
*P ≤ .05.
We created intermediate regression models to examine the effect of specific sets of covariates on the association between risk of mortality and race among veterans with clinically diagnosed TBI. Table 2 shows the HR and 95% confidence intervals (CIs) for 3 such sequentially built models. The first model, adjusted only for race, showed an association of Hispanic ethnicity (HR = 2.33; 95% CI = 1.49, 3.64) with higher mortality risk compared with non-Hispanic White ethnicity. In the second model, adjusted for sociodemographic characteristics, Hispanic ethnicity (HR = 1.62; 95% CI = 1.02, 2.60) continued to be positively associated with a higher mortality risk than did non-Hispanic White ethnicity. In addition, increasing age, female gender, service connectedness, and insurance status were significantly associated with mortality risk. Mortality risk was positively associated with being aged 50 to 64 (HR = 4.27; 95% CI = 2.65, 6.88), 65 to 74 (HR = 9.81; 95% CI = 5.83, 16.49), and 75 years or older (HR = 16.87; 95% CI = 10.25, 27.76), compared with those who were younger than 50 years. Mortality risk was also positively associated with service connectedness (HR = 1.00; 95% CI = 1.001, 1.006) and negatively with female gender (HR = 0.19; 95% CI = 0.06, 0.60). Veterans who had Medicare coverage in addition to VA care were estimated to have a higher mortality risk (HR = 1.58; 95% CI = 1.22, 2.05) compared with VA care alone.
TABLE 2—
Adjusted Mortality Using Cox Proportional Hazard: Racial/Ethnic Disparities in US Veteran Traumatic Brain Injury Mortality, January 1, 2006–December 31, 2009
| Model 1 (Race), HR (95% CI) | Model 2 (Race, Demographics), HR (95% CI) | Model 3 (Race, Demographics, Comorbidities), HR (95% CI) | |
| Race | |||
| Hispanic | 2.33* (1.49, 3.64) | 1.62* (1.02, 2.60) | 1.61* (1.00, 2.58) |
| Non-Hispanic Black | 0.92 (0.67, 1.25) | 1.24 (0.90, 1.72) | 1.25 (0.90, 1.73) |
| Other/unknown race | 0.46* (0.35, 0.61) | 0.62* (0.47, 0.82) | 0.62* (0.47, 0.82) |
| White (Ref) | 1.00 | 1.00 | 1.00 |
| Age, y | |||
| < 50 (Ref) | 1.00 | 1.00 | 1.00 |
| 50–64 | 4.27* (2.65, 6.88) | 4.27* (2.64, 6.89) | |
| 65–74 | 9.97* (5.94, 16.70) | 9.81* (5.83, 16.49) | |
| ≥ 75 | 16.87* (10.25, 27.76) | 16.67* (10.13, 27.44) | |
| Married | 0.91 (0.73, 1.12) | 0.91 (0.73, 1.13) | |
| Female | 0.19* (0.06, 0.60) | 0.19* (0.06, 0.60) | |
| Service connected | 1.00* (1.00, 1.01) | 1.35* (1.10, 1.67) | |
| Region | |||
| Urban | 1.10 (0.87, 1.39) | 1.10 (0.87, 1.39) | |
| Region 1 northeastern | 0.92 (0.64, 1.32) | 0.92 (0.64, 1.33) | |
| Region 2 mid-Atlantic | 1.22 (0.90, 1.65) | 1.24 (0.91, 1.68) | |
| Region 4 midwestern | 0.99 (0.73, 1.35) | 1.00 (0.73, 1.36) | |
| Region 5 western | 0.94 (0.68, 1.30) | 0.95 (0.69, 1.31) | |
| Insurance | |||
| Medicare | 1.58* (1.22, 2.05) | 1.60* (1.23, 2.07) | |
| Private insurance | 0.98 (0.65, 1.47) | 0.98 (0.65, 1.46) | |
| Disorders | |||
| Substance abuse | 1.12 (0.67, 1.89) | ||
| Anemia | 1.31 (0.58, 2.98) | ||
| Cancer | 0.95 (0.44, 2.05) | ||
| Heart disease | 2.34* (1.18, 4.63) | ||
| Depression | 0.48* (0.24, 0.97) | ||
| Hypertension | 0.75 (0.54, 1.03) | ||
| Hypothyroidism | 0.87 (0.35, 2.14) | ||
| Lung disease | 1.81* (1.12, 2.92) | ||
| Liver disease | 1.74 (0.76, 3.97) | ||
| Psychoses | 1.09 (0.66, 1.82) |
Note. CI = confidence interval; HR = hazard ratio. Service connected is rounded to 2 decimal places of actual number (HR = 1.004; CI = 1.001, 1.006). The sample size was n = 14 690.
*P ≤ .05.
The third and final model adjusted for comorbidities as well as sociodemographic characteristics and race/ethnicity. The HR estimates for race/ethnicity were very similar to the second model, with Hispanic ethnicity (HR = 1.61; 95% CI = 1.00, 2.58) continuing to be positively associated with a higher mortality risk than was non-Hispanic White ethnicity. Age, gender, and service connectedness continued to be significant, with approximately the same HRs found for model 2. Mortality risk was positively associated with being aged 50 to 64 (HR = 4.27; 95% CI = 2.64, 6.89), 65 to 74 (HR = 9.97; 95% CI = 5.94, 6.70), and 75 years or older (HR = 16.87; 95% CI = 10.25, 27.76) compared with being aged 50 years. Mortality risk was also positively associated with service connectedness (HR = 1.35; 95% CI = 1.10, 1.67) and Medicare coverage (HR = 1.60; 95% CI = 1.23, 2.07) and negatively associated with female gender (HR = 0.19; 95% CI = 0.06, 0.60). Comorbidities significantly associated with increased mortality were heart disease (HR = 2.34; 95% CI = 1.18, 4.63) and lung disease (HR = 1.81; 95% CI = 0.76, 3.97), whereas depression (HR = 0.48; 95% CI = 0.24, 0.97) was found to be negatively associated with mortality risk.
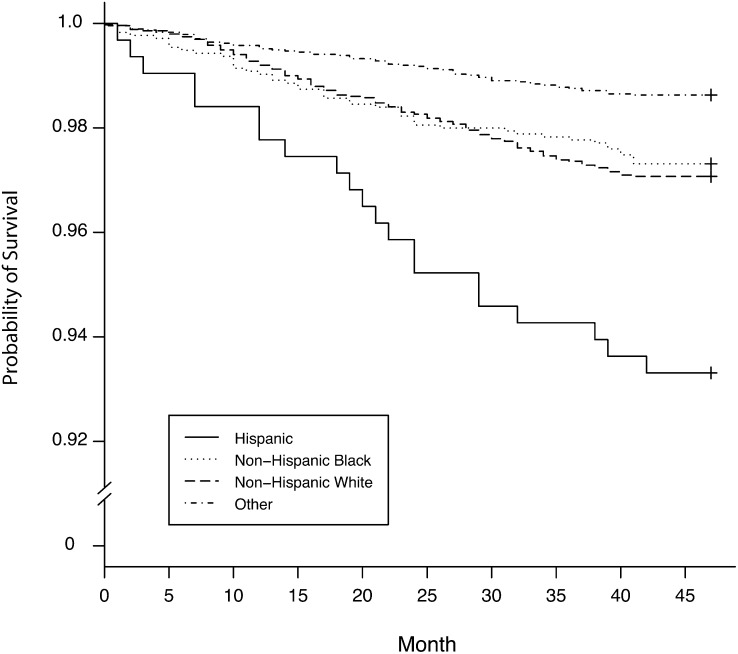
The 3 sequential models indicate that association between Hispanic ethnicity and higher mortality risk among veterans with clinically diagnosed TBI is robust to model specification. The higher mortality risk for Hispanic veterans is also apparent in the survival curve for time to death by race/ethnicity shown in Figure 1.
FIGURE 1—
Survival curve for time to death by race/ethnicity: racial/ethnic disparities in US veteran traumatic brain injury mortality, January 1, 2006–December 31, 2009.
DISCUSSION
We observed a significant difference in mortality rates in Hispanic veterans with clinically diagnosed TBI compared with non-Hispanic White veterans despite lower prevalence of comorbidities among Hispanic veterans. This is an important finding because the only previously documented condition for which minority veterans had higher mortality rates was HIV.
Our findings are, however, consistent with the civilian literature on short-term mortality from TBI.6,7 Hispanics were found to have a higher (trending toward significant) mortality than were non-Hispanic White individuals in a study of 56 482 patients with moderate to severe TBI who were hospitalized in level-1 or -2 trauma-designated hospitals between 2000 and 2003.6 Another study of prehospital death founded on case reviews from medical examiner referrals in the Bronx borough of New York City found that race-specific mortality was highest for Blacks, intermediate for Hispanics, and lowest for Whites.7
Our findings are also consistent with racial/ethnic disparities in various functional outcomes among civilians with TBI.22–27 A study of 58 729 individuals in the National Trauma Data Bank with severe blunt TBI found that after adjusting for potential confounders, minority patients were 15% less likely to be placed in rehabilitation.22 A study of 3056 individuals in the Traumatic Brain Injury Model Systems National Database found that despite similar functional status at inpatient rehabilitation discharge and after controlling for confounders, Hispanic ethnicity was associated with poorer functional outcomes 1 year after injury as measured by the Disability Rating Scale, the Functional Independence Measure Instrument, and the Community Integration Questionnaire (CIQ).23 Another study of 4929 individuals hospitalized between 1989 and 2004 from the TBI Model Systems Database found that at discharge and 1 year after injury, Hispanics and Blacks had worse Disability Rating Scale, Functional Independence Measure, and CIQ outcomes than did non-Hispanic Whites, but there were no significant differences between Hispanics and Blacks.24 A study of 211 patients with blunt TBI from the TBI Clinical Trials Network found that minority patients experienced worse long-term functional outcomes in all domains that reached statistical significance in post-TBI standard of living, engagement in leisure activities, and return to work or school.25 Another study of Rehabilitation Services Administration case service report data for fiscal year 2004 of 7366 persons with TBI found that non-Hispanic White individuals (53%) had appreciably higher competitive employment rates than did Native Americans (50%), Asian Americans (44%), non-Hispanic Black individuals (51%), and Hispanics (41%).26 Finally, a study of 151 individuals with mild to severe TBI recruited from consecutive admissions to the neurosurgery service of a county level-1 trauma center found that non-Hispanic Black individuals had lower CIQ scores than did non-Hispanic White individuals; non-Hispanic Black and Hispanic individuals had lower scores than did non-Hispanic White individuals on the Home Integration Scale; and non-Hispanic Black individuals had lower scores than did non-Hispanic White and Hispanic individuals on the CIQ Productive Activity Scale.27
There is scant literature regarding the effects of TBI on language that could be potentially relevant for multilingual individuals, as may be the case for many veterans of Hispanic ethnicity. A review of the literature found that the outcome of brain injury may be influenced by factors such as cerebral representation of a secondary language, method of language acquisition, age of acquisition, premorbid language proficiency, and style of learning in individuals.28 A study assessing the Behavioral Assessment of Dysexecutive Syndrome and the Wisconsin Card Sorting Test, tests commonly used to assess executive function in individuals with TBI, found statistically significant differences for race/ethnicity on the profile scores (raw scores), standard scores, and the Zoo Map subset of the Behavioral Assessment of Dysexecutive Syndrome. The authors concluded that caution should be taken when administering and interpreting Behavioral Assessment of Dysexecutive Syndrome for individuals with TBI from diverse cultural and linguistic backgrounds.29 A recent study in the civilian population at a level-1 trauma center found that after controlling for education and whether actively practicing religion, Spanish-speaking Hispanics reported a greater percentage of misconceptions regarding TBI than did English-speaking Hispanics and Blacks.30 Studies indicate a variety of likely root causes of disparities, including racial differences in patients’ medical knowledge and information sources, trust and skepticism, and levels of participation in health care interactions and decisions and social support and resources; clinician judgment or bias; the racial or cultural milieu of health care settings; and differences in the quality of care at facilities attended by different racial groups.31
The other significant finding of higher mortality risk positively associated with Medicare coverage is also consistent with previous studies. Dual users of the VA and the commercial health system have been found to have an increased attributable risk of death (15.6%) compared with those who are VA users only.32,33 The VA is a safety net for uninsured veterans, and commercial insurance is not associated with mortality among veterans with TBI although Medicare is associated with a worse outcome. Although some conditions may be treated with equal quality of care by either VA or civilian providers, certain conditions targeted as priority, such as TBI, may be better suited for treatment inside the VA.
The final significant finding that comorbid depression is associated with a decreased risk of mortality is consistent with a previous study that showed that persistent recognition of depression (a documented diagnosis of depression on repeat clinic visits) is associated with lower mortality risk.9 Because VA guidelines mandate annual screening for depression in primary care and patients identified through the screening process usually receive ongoing depression treatment, persistent recognition of depression (i.e., according to repeated documentation of ICD-9 codes for depression) may be a surrogate for depression treatment.
Our study has numerous limitations. The cohort is for 1 year of veterans clinically diagnosed with TBI although this cohort was followed for 4 years. We included only clinically diagnosed TBI and not TBI detected via the VA primary screen but not yet confirmed clinically. Our data did not allow us to ascertain the cause of death. We did not have data on other potentially important factors associated with mortality such as time between injury and diagnosis, branch of military, Department of Defense or civilian treatment, severity, Glasgow Coma Score, discharge disposition, education, and family support. We had a high number of missing race/ethnicity values that we controlled for by including missing as a race/ethnicity category. Because the missing race group has a much lower death rate overall and lower HR after controlling for covariates, we do not believe we had a problem with bias. Despite these limitations, our 3 models indicate that our finding that Hispanic ethnicity is associated with higher mortality is robust to model specification.
Given the absence of published evidence regarding race/ethnicity and mortality among veterans with TBI, we sought to determine whether race/ethnicity is associated with mortality risk among veterans clinically diagnosed with TBI after controlling for relevant covariates. We found that Hispanic ethnicity was associated with an approximately 60% higher mortality rate after controlling for sociodemographic and clinical confounders. Our findings are novel for the VA but are consistent with evidence from the civilian population with TBI. Between 2000 and 2009, incidence of TBI in the military more than doubled (from 10 963 to 27 862 per year) and as of September 2010, Hispanics are the second highest ethnicity/race experiencing military deaths (10.6%), slightly higher than non-Hispanic Blacks (9.7%).34 This finding suggests that further research is needed to understand the factors that explain differential mortality among Hispanics and strategies to decrease the mortality differential among veterans with TBI. National VA data are limited in the variables they contain, which could be associated with the disparities found in this study. Further research needs to be conducted using chart abstraction in combination with survey data to identify explanatory factors for differential mortality by race/ethnicity in veterans with TBI accounting for pertinent patient, provider, and facility characteristics.
Acknowledgments
This study was funded by the Veterans Health Administration Health Services Research and Development (HSR&D) program (grant REA 08-261).
We acknowledge and appreciate the resources provided by the Center for Disease Prevention and Health Interventions for Diverse Populations HSR&D program and the Ralph H. Johnson Veterans Affairs Medical Center. We acknowledge the assistance of Gregory Gilbert in the preparation of Figure 1 and the editorial assistance of Hollis Weidenbacher as well as the valuable suggestions of anonymous reviewers.
Note. The funding agency did not participate in the design and execution of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, and approval of the article. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Human Participant Protection
This study was approved by the Ralph H. Johnson Veterans Affairs Medical Center and Medical University of South Carolina institutional review board.
References
- 1.Harrison-Felix CL, Whiteneck GG, Jha A, DeVivo MJ, Hammond FM, Hart DM. Mortality over four decades after traumatic brain injury rehabilitation: a retrospective cohort study. Arch Phys Med Rehabil. 2009;90(9):1506–1513 [DOI] [PubMed] [Google Scholar]
- 2.Arthur M, Hedges JR, Newgard CD, Diggs BS, Mullins RJ. Racial disparities in mortality among adults hospitalized after injury. Med Care. 2008;46(2):192–199 [DOI] [PubMed] [Google Scholar]
- 3.Martin CA, Care M, Rangel EL, Brown RL, Garcia VF, Falcone RA. Severity of head computed tomography scan findings fail to explain racial differences in mortality following child abuse. Am J Surg. 2010;199(2):210–215 [DOI] [PubMed] [Google Scholar]
- 4.Berry C, Ley EJ, Mirocha J, Salim A. Race affects mortality after moderate to severe traumatic brain injury. J Surg Res. 2010;163(2):303–308 [DOI] [PubMed] [Google Scholar]
- 5.Sorani MD, Lee M, Kim H, Meeker M, Manley GT. Race/ethnicity and outcome after traumatic brain injury at a single, diverse center. J Trauma. 2009;67(1):75–80 [DOI] [PubMed] [Google Scholar]
- 6.Bowman SM, Martin DP, Sharar SR, Zimmerman FJ. Racial disparities in outcomes of persons with moderate to severe traumatic brain injury. Med Care. 2007;45(7):686–690 [DOI] [PubMed] [Google Scholar]
- 7.Bruns J, Hauser WA. The epidemiology of traumatic brain injury: a review. Epilepsia. 2003;44(10):2–10 [DOI] [PubMed] [Google Scholar]
- 8.Corkin S, Sullivan EV, Carr A. Prognostic factors for life expectancy after penetrating head injury. Arch Neurol. 1984;41(9):975–977 [DOI] [PubMed] [Google Scholar]
- 9.Richardson LK, Egede LE, Mueller M. Effect of race/ethnicity and persistent recognition of depression on mortality in elderly men with type 2 diabetes and depression. Diabetes Care. 2008;31(5):880–881 [DOI] [PubMed] [Google Scholar]
- 10.Lynch CP, Gebregziabher M, Echols C, Gilbert GE, Zhao Y, Egede LE. Racial disparities in all-cause mortality among veterans with type 2 diabetes. J Gen Intern Med. 2010;25(10):1051–1056 Published online June 8, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jha AK, Shlipak MG, Hosmer W, Frances CD, Browner WS. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. JAMA. 2001;285(3):297–303 [DOI] [PubMed] [Google Scholar]
- 12.Young BA, Maynard C, Boyko EJ. Racial differences in diabetic nephropathy, cardiovascular disease, and mortality in a national population of veterans. Diabetes Care. 2003;26(8):2392–2399 [DOI] [PubMed] [Google Scholar]
- 13.Frei CR, Mortensen EM, Copeland LAet al. Disparities of care for African-Americans and Caucasians with community-acquired pneumonia: a retrospective cohort study. BMC Health Serv Res. 2010;10:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volpp KG, Stone R, Lave JRet al. Is thirty-day hospital mortality really lower for Black veterans compared with White veterans? Health Serv Res. 2007;42(4):1613–1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deswal A, Petersen NJ, Souchek J, Ashton CM, Wray NP. Impact of race on health care utilization and outcomes in veterans with congestive heart failure. J Am Coll Cardiol. 2004;43(5):778–784 [DOI] [PubMed] [Google Scholar]
- 16.Ellis C, Zhao Y, Egede LE. Racial/ethnic differences in stroke mortality in veterans. Ethn Dis. 2009;19(2):161–165 [PubMed] [Google Scholar]
- 17.McGinnis KA, Fine MJ, Sharma RKet al. Understanding racial disparities in HIV using data from the veterans aging cohort 3-site study and VA administrative data. Am J Public Health. 2003;93(10):1728–1733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 19.Carlson KF, Nelson D, Orazem RJ, Nugent S, Cifu DX, Sayer NA. Psychiatric diagnoses among Iraq and Afghanistan war veterans screened for deployment-related traumatic brain injury. J Trauma Stress. 2010;23(1):17–24 [DOI] [PubMed] [Google Scholar]
- 20.Quan H, Sundararajan V, Hafon Pet al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139 [DOI] [PubMed] [Google Scholar]
- 21.SAS/STAT, Version 9.1.3 [computer program] Cary, NC: SAS Institute; 2008 [Google Scholar]
- 22.Shafi S, de la Plata CM, Diaz-Arrastia Ret al. Ethnic disparities exist in trauma care. J Trauma. 2007;63(5):1138–1142 [DOI] [PubMed] [Google Scholar]
- 23.Arango-Lasprilla JC, Rosenthal M, DeLuca J, Cifu DX, Hanks R, Komaroff E. Functional outcomes from inpatient rehabilitation after traumatic brain injury: how do Hispanics fare? Arch Phys Med Rehabil. 2007;88(1):11–18 [DOI] [PubMed] [Google Scholar]
- 24.Arango-Lasprilla JC, Rosenthal M, Deluca Jet al. Traumatic brain injury and functional outcomes: does minority status matter? Brain Inj. 2007;21(7):701–708 [DOI] [PubMed] [Google Scholar]
- 25.Staudenmayer KL, Diaz-Arrastia R, Oliveira A, Genitello LM, Shafi S. Ethnic disparities in long-term functional outcomes after traumatic brain injury. J Trauma. 2007;63(6):1364–1368 [DOI] [PubMed] [Google Scholar]
- 26.Catalano D, Pereira AP, Wu M-Y, Ho H, Chan F. Service patterns related to successful employment outcomes of persons with traumatic brain injury in vocational rehabilitation. NeuroRehabilitation. 2006;21(4):279–293 [PubMed] [Google Scholar]
- 27.Sander AM, Pappadis MR, Davis LCet al. Relationship of race/ethnicity and income to community integration following traumatic brain injury: investigation in a non-rehabilitation trauma sample. NeuroRehabilitation. 2009;24(1):15–27 [DOI] [PubMed] [Google Scholar]
- 28.Marrero MZ, Golden CJ, Epse-Pfeifer P. Bilingualism, brain injury, and recovery: implications for understanding the bilingual and for therapy. Clin Psychol Rev. 2002;22(3):465–480 [DOI] [PubMed] [Google Scholar]
- 29.Proctor A, Zhang J. Performance of three racial/ethnic groups on two tests of executive function: clinical implications for traumatic brain injury (TBI). NeuroRehabilitation. 2008;23(6):529–536 [PubMed] [Google Scholar]
- 30.Pappadis MR, Sander AM, Struchen MA, Leung P, Smith DW. Common misconceptions about traumatic brain injury (TBI). J Head Trauma Rehabil. Published online August 30, 2010 [DOI] [PubMed] [Google Scholar]
- 31.Saha S, Feeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23(5):654–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wolinsky FD, Miller TR, An H, Brezinski PR, Vaughn TE, Rosenthal GE. Dual use of Medicare and the Veterans Administration: are there adverse health outcomes? BMC Health Serv Res. 2006;6:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Helmer D, Sambamoorthi U, Shen Yet al. Opting out of an integrated healthcare system: dual-system use is associated with poorer glycemic control in veterans with diabetes. Prim Care Diabetes. 2008;2(2):73–80 [DOI] [PubMed] [Google Scholar]
- 34.Fischer HUS. Military casualty statistics: Operation New Dawn, Operation Iraqi Freedom, and Operation Enduring Freedom. Congressional Research Service; 2010. Available at: http://www.fas.org/sgp/crs/natsec/RS22452.pdf. Accessed September 28, 2010 [Google Scholar]