Abstract
Objectives. We have described national trends for the 5 leading external causes of injury mortality.
Methods. We used negative binomial regression and annual underlying cause-of-death data for US residents for 2000 through 2009.
Results. Mortality rates for unintentional poisoning, unintentional falls, and suicide increased by 128%, 71%, and 15%, respectively. The unintentional motor vehicle traffic crash mortality rate declined 25%. Suicide ranked first as a cause of injury mortality, followed by motor vehicle traffic crashes, poisoning, falls, and homicide. Females had a lower injury mortality rate than did males. The adjusted fall mortality rate displayed a positive age gradient. Blacks and Hispanics had lower adjusted motor vehicle traffic crash and suicide mortality rates and higher adjusted homicide rates than did Whites, and a lower unadjusted total injury mortality rate.
Conclusions. Mortality rates for suicide, poisoning, and falls rose substantially over the past decade. Suicide has surpassed motor vehicle traffic crashes as the leading cause of injury mortality. Comprehensive traffic safety measures have successfully reduced the national motor vehicle traffic crash mortality rate. Similar efforts will be required to diminish the burden of other injury.
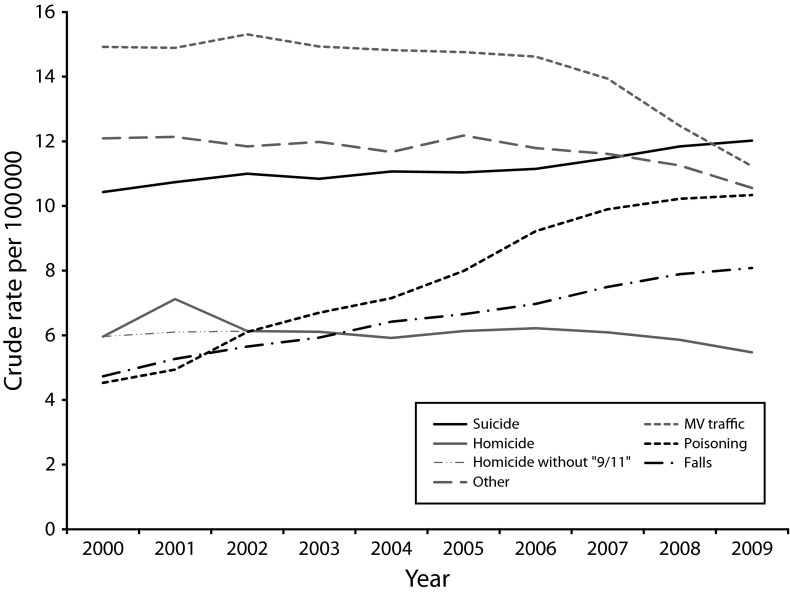
Estimated life expectancy at birth in the United States rose steadily from 73.7 years in 1980 to 78.0 years in 2008.1 However, life expectancy’s 2 fundamental determinants, total disease and injury mortality rates, displayed disparate overall trends (Figure 1).2 The age-adjusted disease mortality rate trended downward throughout the 29-year period, whereas the age-adjusted injury mortality rate reverted upward between 2000 and 2007. Moreover, crude and age-adjusted injury mortality rates shared a common trajectory.
FIGURE 1—
Annual crude and age-adjusted mortality rates from (a) disease and (b) injury: United States, 1980–2008.
Note. ICD = International Classification of Diseases. The vertical dashed lines demarcate the transition between revisions ICD-9 and ICD-10.
The 5 leading external causes of injury deaths comprise 3 unintentional (motor vehicle traffic crashes, poisoning, and falls) and 2 intentional (suicide and homicide) or violence-related categories. They account for more than four fifths of all such deaths nationally.3 The unintentional poisoning mortality rate has been rising rapidly since the 1990s,4,5 with prescription drug overdose deaths now predominant.6 Previous studies also reported a substantial rate increase for unintentional elderly fall mortality7 and a smaller increase for suicide.5 In addition, declining rates have been documented for homicide8 and unintentional motor vehicle traffic crash mortality.9 Two of the national studies examined racial/ethnic differences in unintentional injury mortality trends. The first study found an increase in the rate between 1992 and 2002 for non-Hispanic Whites and a decline for minorities.10 The second study reported a change in the unintentional injury mortality rate between 1999 and 2005, an increase, for non-Hispanic Whites only.11 Both studies reported excess rate increases for this group in various unintentional causes, most notably poisoning and falls. Unknown are how proportionate shares of the leading causes of injury fatalities may have changed during the first decade of the twenty-first century and race/ethnicity and other demographics featured in rate trends.
We have characterized patterns and trends in rates of total combined national unintentional and intentional injury mortality and its 5 leading external causes for the decade 2000–2009. Specifically, we have described and analyzed these rates in terms of time and 4 population-level demographic characteristics: age, gender, race/ethnicity, and major US geographic region. Incorporating recently released data, we addressed the absence of current research on unintentional and intentional injury mortality as a whole.
METHODS
For this observational study, we used annual underlying cause-of-death data from the National Center for Health Statistics (NCHS) to describe national patterns and trends in fatal injury for the period 2000–2009.
Study Design and Data
We accessed NCHS data through the Web-Based Injury Statistics Query and Reporting System, which the Centers for Disease Control and Prevention maintains.3 At their time of death, included decedents were residents of 1 of the 50 states or the District of Columbia.
External causes (intent or mechanism) of injury mortality were coded by NCHS or at the state or city level using NCHS software, in accordance with the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10).12 NCHS implemented ICD-10 coding of mortality statistics in 1999. We examined total unintentional and intentional injury mortality (V01–Y36, Y85–Y87, Y89, *U01–*U03) and 5 specific causes: unintentional motor vehicle traffic crashes (V30–V39 [0.4–0.9], V40–V49 [0.4–0.9], V50–V59 [0.4–0.9], V60–V69 [0.4–0.9], V70–V79 [0.4–0.9], V81.1, V82.1, V83–V86 [0.0–0.3], V20–V28 [0.3–0.9], V29 [0.4–0.9], V12–V14 [0.3–0.9], V19 [0.4–0.6], V02–V04 [0.1, 0.9], V09.2, V80 [0.3–0.5], V87 [0.0–0.8], V89.2); suicide (X60–X84, Y87.0, *U03); homicide (X85–Y09, Y87.1, *U01–*U02); unintentional poisoning (X40–X49); and unintentional falls (W00–W19). These causes are among the fundamental subsets of unintentional and intentional injury mortality recommended in the Global Burden of Diseases, Injuries and Risk Factors Study Operations Manual,13 and delineation of cause, blending intent and mechanism, is commonly used internationally in injury mortality reports.14–20 We disaggregated the data by age (0–4, 5–14, 15–24, 25–34, 35–54, 55–74, ≥ 75 years), gender, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other), and major geographic region (Northeast, South, Midwest, West). We included race/ethnicity to assess possible rate disparities.
We have presented our injury mortality data disaggregated by external cause, age, gender, race/ethnicity, and region for 2000 and 2009. We have also portrayed rate trends for the 5 leading causes over the entire observation period, 2000 through 2009. The residual external cause of injury group, other causes, is the difference between the respective number of injury deaths from all causes and total deaths from the 5 designated external causes. We obtained age-adjusted mortality rates from the Web-Based Injury Statistics Query and Reporting System, whose direct standardization procedure employed the US 2000 standard population as the referent.
Statistical Analysis
We performed a negative binomial regression with a log link function to characterize the injury rates and identify demographic and time trends.21 We assumed independent annual rates, the Markov assumption for sequential years. We included year, age, gender, race/ethnicity, and region as independent variables. The age categories 0 to 4 and 5 to 14 years were combined because of small counts in some demographic subgroups. The age group 15 to 24 years was our age referent because of its historical prominence as a high-risk group.15,22 We derived our model selection from the Bayesian information criterion, which chooses the subset of variables that best minimizes a penalized function of the likelihood.21 We have reported 95% confidence intervals (CIs) on the rate ratio (RR) scale for the variables. We explored possible effect modification for the 5 injury subgroups under examination. We used the statistical computing environment R version 2.14.1 for our data analyses (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
The total combined unintentional and intentional injury mortality rate was 10% higher in 2009 than in 2000 (Table 1). Time did not help explain the increase, with adjustment for the 4 selected demographic covariates (Table 2). Regression analysis further showed that only the youngest and oldest age groups differed from the referent, age group 15 to 24 years. Age group 0 to 14 years had a 78% lower adjusted total rate, whereas the rate for the 75 years and older group was 2.8 times higher. The total injury mortality rate in 2009 was 2.2 times higher for males than for females (Table 1). Although the total rate was higher in 2009 than in 2000 for both genders, there was a relatively greater increase for females than for males—16% versus 7%. The regression analysis showed a 60% lower adjusted total injury mortality rate for females (Table 2).
TABLE 1—
Number and Rate of Total Unintentional and Intentional Injury Mortality by Cause and Demographic Characteristics: United States, 2000 and 2009
| Specific Cause,a % |
||||||||||
| Characteristic | Total |
No. | Rateb | Motor Vehicle Traffic Crash | Suicide | Poisoning | Fall | Homicide | Other | |
| 2000 | ||||||||||
| Age, y | ||||||||||
| 0–4 | 3516 | 18.34 | 20.60 | 0.00 | 1.30 | 1.20 | 20.10 | 56.80 | ||
| 5–14 | 3720 | 9.06 | 44.30 | 8.30 | 1.20 | 1.00 | 10.00 | 35.40 | ||
| 15–24 | 23 489 | 59.95 | 43.90 | 17.00 | 4.90 | 1.00 | 21.00 | 12.10 | ||
| 25–34 | 21 514 | 53.93 | 31.20 | 22.30 | 11.10 | 1.40 | 19.40 | 14.70 | ||
| 35–54 | 46 949 | 56.68 | 25.50 | 25.60 | 16.40 | 3.20 | 10.60 | 18.80 | ||
| 55–74 | 21 972 | 51.50 | 28.60 | 23.80 | 4.40 | 11.90 | 5.40 | 25.90 | ||
| ≥ 75 | 26 916 | 162.14 | 15.90 | 11.20 | 1.60 | 32.00 | 1.50 | 37.70 | ||
| Gender | ||||||||||
| Male | 103 254 | 74.79 | 27.50 | 22.90 | 8.80 | 6.90 | 12.40 | 21.50 | ||
| Female | 44 955 | 31.36 | 30.30 | 12.80 | 8.00 | 13.80 | 8.80 | 26.30 | ||
| Race/ethnicity | ||||||||||
| White | 106 605 | 54.03 | 28.30 | 23.10 | 8.60 | 10.80 | 5.10 | 24.20 | ||
| Black | 22 523 | 64.18 | 23.70 | 8.50 | 8.80 | 3.30 | 34.40 | 21.20 | ||
| Hispanic | 13 798 | 39.08 | 34.70 | 12.90 | 9.50 | 5.00 | 21.10 | 16.70 | ||
| Other | 4467 | 32.61 | 35.90 | 19.80 | 4.50 | 6.80 | 12.10 | 20.90 | ||
| Region | ||||||||||
| Northeast | 22 120 | 41.27 | 22.40 | 18.90 | 11.70 | 10.70 | 10.20 | 26.00 | ||
| South | 60 971 | 60.83 | 31.80 | 18.80 | 7.00 | 7.10 | 12.40 | 22.90 | ||
| Midwest | 33 242 | 51.62 | 27.90 | 19.40 | 7.30 | 10.70 | 10.70 | 24.10 | ||
| West | 31 876 | 50.44 | 26.20 | 22.90 | 10.80 | 9.70 | 10.70 | 19.70 | ||
| Total | 148 209 | 52.66 | 28.30 | 19.80 | 8.60 | 9.00 | 11.30 | 23.00 | ||
| Cause-specific rate | ||||||||||
| Crude | 52.66 | 14.92 | 10.43 | 4.53 | 4.73 | 5.96 | 12.09 | |||
| Age-adjusted | 52.75 | 14.89 | 10.44 | 4.53 | 4.82 | 5.90 | 12.17 | |||
| 2009 | ||||||||||
| Age, y | ||||||||||
| 0–4 | 3521 | 16.53 | 12.90 | 0.00 | 1.70 | 1.80 | 19.70 | 63.90 | ||
| 5–14 | 2313 | 5.70 | 37.69 | 11.50 | 2.20 | 1.20 | 13.20 | 34.40 | ||
| 15–24 | 22 217 | 51.57 | 33.50 | 19.70 | 13.70 | 0.90 | 21.90 | 10.30 | ||
| 25–34 | 24 496 | 58.93 | 23.10 | 21.70 | 25.30 | 1.20 | 17.20 | 11.40 | ||
| 35–54 | 57 735 | 67.04 | 17.80 | 26.50 | 29.50 | 3.30 | 8.40 | 14.50 | ||
| 55–74 | 33 067 | 59.50 | 19.50 | 26.40 | 14.10 | 14.30 | 4.50 | 21.20 | ||
| ≥ 75 | 33 728 | 179.61 | 9.80 | 8.70 | 1.90 | 52.10 | 1.10 | 26.30 | ||
| Gender | ||||||||||
| Male | 120 698 | 79.70 | 20.00 | 24.10 | 17.00 | 10.50 | 10.90 | 17.50 | ||
| Female | 56 456 | 36.29 | 18.40 | 13.80 | 19.80 | 21.40 | 6.50 | 20.10 | ||
| Race/ethnicity | ||||||||||
| White | 131 451 | 65.02 | 18.20 | 23.40 | 19.30 | 16.50 | 3.90 | 18.60 | ||
| Black | 22 324 | 57.44 | 19.80 | 9.10 | 13.00 | 5.10 | 34.60 | 18.30 | ||
| Hispanic | 16 826 | 34.75 | 27.40 | 15.30 | 15.40 | 7.40 | 18.90 | 15.70 | ||
| Other | 5658 | 32.21 | 23.20 | 23.70 | 13.90 | 11.80 | 9.90 | 17.40 | ||
| Region | ||||||||||
| Northeast | 25 283 | 45.73 | 16.30 | 19.80 | 19.50 | 16.80 | 8.70 | 18.90 | ||
| South | 73 816 | 65.14 | 22.70 | 19.70 | 16.70 | 11.50 | 10.50 | 18.80 | ||
| Midwest | 37 730 | 56.45 | 17.70 | 20.30 | 17.10 | 16.80 | 8.90 | 19.10 | ||
| West | 40 325 | 56.34 | 17.10 | 24.00 | 19.90 | 14.10 | 8.70 | 16.20 | ||
| Total | 177 154 | 57.70 | 19.50 | 20.80 | 17.90 | 14.00 | 9.50 | 18.30 | ||
| Cause-specific rate | ||||||||||
| Crude | 57.70 | 11.23 | 12.02 | 10.34 | 8.08 | 5.47 | 10.56 | |||
| Age-adjusted | 56.16 | 11.06 | 11.77 | 10.29 | 7.44 | 5.49 | 10.13 | |||
| % rate change 2009 vs 2000 | ||||||||||
| Crude | 9.60 | −24.70 | 15.20 | 128.30 | 70.80 | −8.20 | −12.70 | |||
| Age-adjusted | 6.50 | −24.70 | 12.70 | 127.10 | 54.40 | −7.90 | −16.80 | |||
Percentage shares of total unintentional and intentional injury mortality by cause may not sum to 100 because of rounding.
Rates are per 100 000 population.
TABLE 2—
Rate Ratio for Total Mortality From All Causes of Injury and Selected Causes by Decedent Characteristics: United States, 2000–2009
| All Causes, All Injury, RR (95% CI) | Specific Cause, RR (95% CI) |
|||||
| Characteristic | Motor Vehicle Traffic Crash | Suicide | Poisoning | Fall | Homicidea | |
| Age, y | ||||||
| 0–14 | 0.22 (0.21, 0.23) | 0.16 (0.15, 0.16) | 0.05 (0.04, 0.05) | 0.05 (0.04, 0.05) | 0.34 (0.31, 0.38) | 0.19 (0.18, 0.21) |
| 15–24 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 25–34 | 0.96 (0.92, 1.01) | 0.71 (0.68, 0.74) | 1.18 (1.12, 1.24) | 2.03 (1.87, 2.20) | 1.44 (1.31, 1.58) | 0.94 (0.88, 1.02) |
| 35–54 | 1.02 (0.97, 1.07) | 0.61 (0.59, 0.64) | 1.29 (1.22, 1.35) | 3.59 (3.31, 3.89) | 4.06 (3.72, 4.42) | 0.63 (0.59, 0.68) |
| 55–74 | 0.96 (0.92, 1.01) | 0.67 (0.65, 0.70) | 1.04 (0.99, 1.10) | 1.45 (1.33, 1.58) | 15.89 (14.60, 17.29) | 0.33 (0.31, 0.36) |
| ≥ 75 | 2.85 (2.72, 2.99) | 1.10 (1.06, 1.15) | 1.31 (1.24, 1.39) | 0.75 (0.68, 0.83) | 130.38 (119.93, 141.78) | 0.29 (0.27, 0.32) |
| Gender | ||||||
| Male (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 0.39 (0.38, 0.40) | 0.44 (0.43, 0.45) | 0.23 (0.22, 0.24) | 0.42 (0.40, 0.44) | 0.37 (0.35, 0.39) | 0.33 (0.32, 0.35) |
| Race/ethnicity | ||||||
| White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 1.20b (1.15, 1.24) | 0.92 (0.89, 0.95) | 0.47 (0.45, 0.49) | 1.03 (0.96, 1.11) | 0.68 (0.64, 0.73) | 5.55 (5.22, 5.91) |
| Hispanic | 0.73 (0.70, 0.76) | 0.86 (0.84, 0.89) | 0.43 (0.41, 0.45) | 0.58 (0.54, 0.62) | 0.80 (0.75, 0.85) | 1.92 (1.80, 2.05) |
| Other | 0.64 (0.61, 0.66) | 0.78 (0.75, 0.81) | 0.60 (0.58, 0.63) | 0.32 (0.30, 0.35) | 0.64 (0.60, 0.68) | 1.11 (1.04, 1.19) |
| Region | ||||||
| Northeast (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Midwest | 1.40 (1.35, 1.46) | 1.59 (1.53, 1.64) | 1.32 (1.26, 1.39) | 1.08 (1.00, 1.17) | 1.18 (1.10, 1.26) | 1.30 (1.21, 1.39) |
| South | 1.47 (1.42, 1.53) | 2.14 (2.06, 2.21) | 1.39 (1.33, 1.46) | 1.06 (0.99, 1.14) | 1.02 (0.96, 1.09) | 1.39 (1.31, 1.49) |
| West | 1.46 (1.41, 1.52) | 1.70 (1.65, 1.77) | 1.63 (1.56, 1.71) | 1.33 (1.24, 1.43) | 1.21 (1.13, 1.29) | 1.35 (1.27, 1.44) |
| Year | ||||||
| 2000 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2001 | … | 1.00 (0.95, 1.06) | … | 1.09 (0.97, 1.23) | … | 1.25 (1.13, 1.39) |
| 2002 | … | 1.01 (0.96, 1.07) | … | 1.25 (1.11, 1.40) | … | 1.00 (0.91, 1.11) |
| 2003 | … | 1.00 (0.95, 1.06) | … | 1.37 (1.22, 1.54) | … | 0.98 (0.88, 1.08) |
| 2004 | … | 0.96 (0.91, 1.01) | … | 1.39 (1.24, 1.56) | … | 0.93 (0.84, 1.03) |
| 2005 | … | 0.93 (0.89, 0.99) | … | 1.60 (1.42, 1.80) | … | 0.98 (0.88, 1.08) |
| 2006 | … | 0.93 (0.88, 0.98) | … | 1.79 (1.59, 2.00) | … | 0.96 (0.87, 1.06) |
| 2007 | … | 0.87 (0.82, 0.91) | … | 1.94 (1.73, 2.18) | … | 0.91 (0.82, 1.01) |
| 2008 | … | 0.75 (0.71, 0.79) | … | 1.92 (1.71, 2.16) | … | 0.89 (0.81, 0.99) |
| 2009 | … | 0.69 (0.66, 0.73) | … | 1.96 (1.75, 2.20) | … | 0.86 (0.78, 0.96) |
Note. CI = confidence interval; RR = rate ratio. Ellipses indicate data not included in the final model under the Bayesian information criterion model selection criterion.
A sensitivity analysis, which removed the effect of 9/11 mortality on the homicide trend, led to year falling out of the model. However, parameter estimates for age, gender, race/ethnicity, and region showed no significant change in magnitude and direction.
A sensitivity analysis, which eliminated the influence of homicide on the racial/ethnic profile of injury mortality, showed that reported parameter estimates remained of similar magnitude and direction, except for Black race/ethnicity (RR = 0.86; 95% CI = 0.83, 0.89).
The total injury mortality rate for Whites was 20% higher in 2009 than in 2000 but 11% lower for Blacks and Hispanics (Table 1). In the regression analysis, Blacks had a 20% higher adjusted rate relative to Whites (Table 2). However, after homicide was eliminated from the model in a sensitivity analysis, Blacks had a 14% (0.86; 95% CI = 0.83, 0.89) lower adjusted rate relative to Whites. Whites had a total injury mortality rate that was 38% higher than that of Hispanics in 2000 and 87% higher in 2009 (Table 1), a direction supported by the regression results (Table 2). Maintaining rank order, all 4 major regions registered a higher total injury mortality rate in 2009 than in 2000 (Table 1). The Northeast had a lower adjusted rate than did the other regions (Table 2).
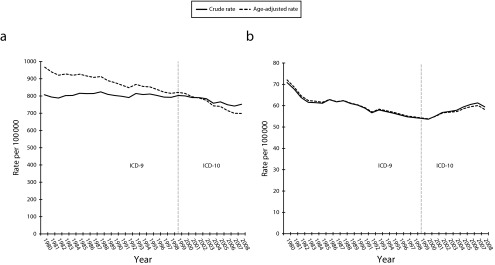
The 5 leading causes of injury mortality increased their combined share of the total from 77% in 2000 to 82% in 2009 (Table 1). Motor vehicle traffic crashes were the leading cause between 2000 and 2008, but these were surpassed by suicide in 2009 (Figure 2). The motor vehicle traffic mortality rate was 25% lower in 2009 than in 2000 (Tables 1 and 2), a downward trend reinforced in the regression analysis (Table 2). There was a decreasing gradient in the adjusted rate from 25 to 34 years to 55 to 74 years relative to 15 to 24 years. Females and all 3 minority groups had lower rates relative to males and Whites, respectively. Although we considered model sensitivity to region, its exclusion only minimally affected the magnitude and direction of remaining reported RRs.
FIGURE 2—
Rates for leading causes of total unintentional and intentional injury mortality: United States, 2000–2009.
Note. MV = motor vehicle.
Trending gradually upward (Figure 2), the suicide rate was 15% higher in 2009 than in 2000 (Table 1). The adjusted suicide rates were higher at 25 to 34 years, 35 to 54 years, and 75 years and older than was the rate for their referent, the 15 to 24 years age group (Table 2). Females had a 77% lower adjusted rate than did males, and Hispanics and Blacks had 57% and 53%, respectively, lower rates than did Whites. The Midwest, South, and West had adjusted suicide rates that were, respectively, 32%, 39%, and 63% higher than the rate for the Northeast.
Poisoning became the third leading cause of injury mortality by 2003, surpassing homicide (Figure 2). Its mortality rate was 128% higher in 2009 than in 2000 (Table 1), a sharp rise also evident in the generally increasing gradient of the adjusted poisoning mortality RRs for year when compared with 2000 (Table 2). Age groups 25 to 34 years, 35 to 54 years, and 55 to 74 years all showed higher adjusted poisoning mortality rates than did their referent, age group 15 to 24 years, and the 0 to 14 years age group showed a much lower rate. Females had a 58% lower adjusted poisoning mortality rate than did males. Although Blacks and Whites were not differentiated in the regression results, Hispanics had a 42% lower rate than did Whites.
In 2004, falls moved past homicide to become the fourth leading cause of injury mortality (Figure 2). Although the unadjusted fall mortality rate trended strongly upward over the observation period (Figure 2), there was no statistical evidence for a time trend (Table 2). However, a strong positive gradient emerged in the adjusted fall mortality rates across the age spectrum. Females had a 63% lower rate than did males, and the rate was at least 20% lower for minorities than for Whites.
Homicide, the third leading cause of injury mortality between 2000 and 2002, ranked fifth behind both poisoning and falls between 2004 and 2009 (Figure 2). Generally flat across the observation period (Figure 2), the homicide rate was 8% lower in 2009 than in 2000 (Table 1). The adjusted homicide rate showed a strong annual decline from the 2000 baseline rate (Table 2). Although removal of “9/11” (the September 11, 2001, terrorist attack in New York City) homicide deaths eliminated year as a predictor, RRs for other predictors showed little change. All age groups had a lower adjusted homicide rate than did the 15 to 24 years group referent, except the equivalent 25 to 34 years group (Table 2). The adjusted rate for females was 67% lower than for males and at least 11% higher for the 3 minority groups than for Whites. Adjusted homicide rates for the Midwest, South, and West were 30% to 40% higher than was the rate for the Northeast.
Examination of possible effect modification revealed an especially noteworthy finding for homicide that involved age, gender, and race/ethnicity. Compared with White counterparts, both Black and Hispanic males showed decreasing RRs with increasing age. This trend was strongest among Black males. Decreasing monotonically, their rate was 20.6 times higher at 15 to 24 years than was that of White counterparts (95% CI = 18.51, 22.94), 16.3 times higher at 25 to 34 years (95% CI = 14.50, 18.23), and 7.6 times higher at 35 to 54 years (95% CI = 6.82, 8.55). The homicide rate for Hispanic males showed a similar trend. At 15 to 24 years, it was 6 times higher than the rate for corresponding White males (95% CI = 5.49, 6.82), 3.6 times higher at 25 to 34 years (95% CI = 3.16, 3.99), and 2.4 times higher at 35 to 54 years (95% CI = 2.11, 2.66). Conversely, Black and Hispanic females showed rate increases relative to White counterparts across the same age range. Black females aged 15 to 24 years had a homicide rate twice that of corresponding Whites (2.15; 95% CI = 1.90, 2.43), and 4.4 and 7.9 times higher at 25 to 34 years (95% CI = 3.86, 4.96) and 35 to 54 years (95% CI = 6.43, 9.61), respectively. Hispanic females aged 15 to 24 years had a rate that was 21% lower than that for White opposites (95% CI = 0.69, 0.90), 53% higher at 25 to 34 years (95% CI = 1.34, 1.75), and 2.1 times higher at 35 to 54 years (95% CI = 1.68, 2.56).
DISCUSSION
The national injury mortality mosaic underwent a substantial transformation during the first decade of the twenty-first century. Embedded in the 10-year net increase of 10% in the total combined unintentional and intentional injury mortality rate were a 25% decrease in the unintentional motor vehicle traffic crash mortality rate and 128%, 71%, and 15% increases in the unintentional poisoning, unintentional fall, and suicide mortality rates, respectively. A global public health problem,20 suicide has emerged as the leading cause of total unintentional and intentional injury mortality in the United States, followed by motor vehicle traffic crashes, poisoning, falls, and homicide. Our finding that suicide now accounts for more deaths than do traffic crashes echoes similar findings for the European Union,17 Canada,18 and China.19
We employed a negative binomial regression procedure for analyzing demographic patterns and time trends in the rates of total combined unintentional and intentional injury mortality and its 5 leading causes. Only 2 age groups varied in their adjusted total injury mortality rates from referent individuals aged 15 to 24 years. The 0 to 14 years age group had a 78% lower rate, and the 75 years and older group had an almost 3-fold higher rate. Being older than the referent was generally associated with higher adjusted rates of suicide, poisoning, and fall mortality and lower adjusted rates of homicide and motor vehicle traffic mortality. Females had rates at least 56% lower than those of males across the board. Whites had a lower adjusted homicide rate than those of the 3 minority groups, but the highest adjusted suicide, motor vehicle traffic, and fall mortality rates. Blacks shared the highest adjusted rate of total injury mortality with Whites owing to their high homicide rate. These 2 groups also had the highest adjusted poisoning mortality rates. The Northeast had lower adjusted rates of total injury, suicide, motor vehicle traffic crash, and homicide mortality than did the West, Midwest, and South.
Our parsimonious statistical model retained year (time) for only 3 of the 6 injury mortality groups that we examined, namely, motor vehicle traffic crashes, poisoning, and homicide. The homicide finding was accounted for by an anomaly, the 9/11 terrorist attacks. Given the escalation of the crude rate, depicted in Figure 2, year surprisingly did not predict the fall mortality rate. This outcome underscores the predictive strength of the demographic covariates, particularly age.
Unintentional poisoning exhibited by far the largest rate increase among the 5 leading causes of injury mortality. In 2008, drug overdoses represented 75% of unintentional poisoning deaths nationally, with prescription drugs representing 74% of the share.23 Moreover, overdoses of prescription opioid analgesics represented 74% of the prescription drug-related deaths,23 with this share increasing.6 Various supply and demand factors are implicated in the prescription drug epidemic. On the supply side, there has been a well-documented increase in opioid prescribing, with a concomitant 402% increase in individual use of prescription opioids between 1997 and 2007.24 Clinical guidelines published in 1997, which supported increased consideration of opioid analgesics in treating patients with chronic pain, may have contributed to this increase.25 Likely a factor in the epidemic of fatal overdoses from opioids was the aggressive pharmaceutical campaign to promote their use in general, and OxyContin use in particular.26 Signaling ready access, the opioid source for a majority of abusers does not appear to be illegal markets, rogue Internet pharmacies, doctor shopping, or prescription drug rings. In 2009 to 2010, 71% of persons aged 12 years or older using pain relievers nonmedically in the past 12 months reported that they obtained the drugs from a relative or friend, 17% through a prescription from a single doctor, 4% from a drug dealer or other stranger, and less than 1% through the Internet.27
Uninformed and misinformed societal attitudes toward recreational use of prescription opioids may be a demand-side driver of the epidemic. For example, the majority of adolescents responding to a national survey believed that using an opioid medication without a prescription did not pose a great health risk.28 Harboring adverse intergenerational implications for abuse of prescription drugs, the adolescents also reported that their parents were less likely to talk to them about the risks of using such drugs than the risks of using alcohol, marijuana, and cocaine. The literature and our research findings jointly support a multipronged approach for curbing the epidemic of fatal prescription drug overdoses. Several promising prevention and control strategies have recently been implemented, including Prescription Drug Monitoring Programs, the Food and Drug Administration’s Opioid Drugs and Risk Evaluation and Mitigation Strategies, provider prescribing guidelines, and single provider–single pharmacist “lock-in” programs.29–31 However, their health impact remains a vital empirical question.
Distinguishing intentional from unintentional injury is important for surveillance, prevention, treatment, and rehabilitation,32 a distinction that can be quite elusive in verifying suicides.33 Apparently nonrandom across decedent demographics and methods,34,35 undercounting suicide likely distorts rates and differentials. Among factors plausibly exacerbating suicide case ascertainment in the twenty-first century are the secular decline in the combined clinical and forensic autopsy rate,36,37 rare use of psychological autopsies in helping medicolegal authorities resolve the manner of death in cases of equivocal intent,38 and extant disparities and underresourcing of the emergency healthcare39,40 and death investigation systems.41,42 No agency analogous to the police exists to assist medical examiner and coroner offices to investigate suicides,38 thus complicating their case ascertainment relative to homicides. Implying differential fastidiousness and thoroughness, investigations of suicide, poisoning, drowning, and other injury deaths are far less likely than are homicide investigations to include a forensic autopsy.36 The rise and magnitude of the suicide rate, including the growing toll associated with military service, reinforce the charge of the National Action Alliance for Suicide Prevention43 to optimize the effectiveness of the National Strategy for Suicide Prevention.38
The escalation in the unintentional fall mortality rate between 2000 and 2009 disproportionately affected older persons, males, and Whites. Determinants are largely unknown, and similar unexplained changes have been reported for Finland, especially Finnish men.44 A sensitivity analysis of definition of age category confirmed that steep rate rises in fall mortality occurred in every 5-year age group. Rates escalated with age, whether years were single or grouped. Thus, the overall fall mortality rate increase seems unlikely to be an artifact of reporting changes, although fall deaths among older people are known to be undercounted.45 A supplemental analysis of Web-Based Injury Statistics Query and Reporting System data on unintentional nonfatal falls for the period 2001 through 2010 showed an analogous increase in the hospitalization rate (42%) for people aged 55 years and older.3
Following a sharp decrease during the 1990s,8 the homicide rate generally remained stable over the observation period. The stark exception was the 9/11 spike in 2001. A relatively lower homicide rate is consonant, for example, with concentrated police deterrence that targets repeat violent offenders,46 the High Intensity Drug Trafficking Areas Program,47 and Cease Fire, a comprehensive public health model aimed chiefly at reducing firearm-related violence among the young.48 Vulnerable minorities continue to show large excess homicide rates. Opposite age gradients evident among Black and Hispanic males and females, relative to White counterparts, are intriguing and warrant in-depth investigation. Community-based studies in current and former hotspots would enlighten homicide patterns and prevention, as would comparative multilevel assessments of cohort effects, emergency healthcare, drug trafficking and gang activities, criminal justice and mental health policies, police and judicial practices, and conditions of incarceration, civil commitment, rehabilitation, probation, and parole.
Of the 5 external causes of injury mortality that we examined, only motor vehicle traffic crashes yield a universal success story. Profound absolute and relative 10-year reductions in traffic deaths can be attributed to a constellation of protective elements, but may also reflect economically induced declines in road exposure.49 Unique within the spectrum of injury prevention, motor vehicle traffic safety is the object of a wide array of national, state, and local evidence-based interventions that are ethically defensible, integrated, systematic, and sustained. Targeting road systems, vehicles, operators, passengers, and pedestrians, these interventions combine engineering, education, economics, policy, legislation, regulations, enforcement, rapid emergency response, and enhanced trauma care systems.50–54 Nonetheless, injury prevention is a moving target. Still greater progress in motor vehicle traffic safety is being impeded by newer challenges, such as driver and pedestrian misuse of cell phones and headphones,55,56 and persistent ones like intoxicated drivers,57 variable implementation of motorcycle helmet use laws,58 and differential quality of emergency care.59
Limitations
This study has the following limitations. First, it relied on the quality of information recorded on the death certificate. Second, we did not factor political and economic conditions into our trend analysis, because these lay beyond the scope of our study. Third, racial/ethnic differentials in injury mortality rates are imperfect owing to usual self- or familial-reporting of race/ethnicity in the census-based population denominators and third-party reporting on death certificates, the numerator data source.60,61 Fourth, our results could have been affected by unexamined heterogeneity in manner and cause-of-death reporting, as might emanate from variable training, resources, philosophies, procedures, and practices of medical examiners and coroners42 and differential and respective exposure of physicians and funeral directors to official handbooks on the death certification62 and on registration processes.63 Finally, our rate breakdowns may be minimally affected by missing data on Hispanic origin for up to 0.6% of cases by year and by masking data on small cells.
Our analytic focus was injury mortality delineated by a blend of intent and mechanism. We derived selected causes by differentiating 1 level of intentionality. All remained in the top 5 causes of combined unintentional and intentional injury mortality throughout the observation period. Our conceptualization of causal categories is highly germane to injury surveillance and for planning, designing, and evaluating injury prevention programs internationally and in the United States.14,64 Differentiation of injury intentionality has clinical, medicolegal, and public health significance,32 and ICD-10 coding rules give precedence to intent or manner of injury death over injury mechanism.12 Salient in recent US government mortality statistics,65 although not universally applied across states,66,67 an alternative conceptualization of injury mortality causes is derived from mechanism alone. It shows poisoning as the leading cause of injury mortality, followed by motor vehicle traffic crashes.68
Conclusions
Our national study indicates that injury mortality is a complex medical, forensic, and public health problem. Impelled by the declining disease mortality rate, life expectancy at birth for the US population increased 1.8 years between 2000 and 2009, from 76.81 to 78.6.69 Contrasting with disease mortality, the injury mortality rate trended upward during most of that decade. Disproportionately affecting the younger population, injury mortality, morbidity, and disability could all be markedly reduced through wider application of the theory, principles, and practices of injury prevention and control.15,64 Elimination of injury would augment population life expectancy by only a year or 2, but it would extend the mean length of life of those whose deaths were averted by a projected 3 decades.70
Our findings provide a comparative context for clinicians, public health professionals, state and county health departments, legislatures, and corporations to accord higher priority to the etiology and prevention of injury. The injury mortality rate shifted upward over the past decade, with substantial rises in the rates for poisoning, falls, and suicide. Comprehensive and sustained traffic safety measures have apparently substantially diminished the motor vehicle traffic mortality rate, and similar attention and resources are needed to reduce the burden of other injury.
Acknowledgments
The Centers for Disease Control and Prevention (grant 5R49CE001170) and the National Institute on Alcohol Abuse and Alcoholism (grant R01AA18707) partially supported this research.
Note. The sponsors had no involvement in the design and conduct of the research, the collection, management, analysis, and interpretation of the data, and the preparation, review, and approval of the article.
Human Participant Protection
No protocol approval was needed for this study because the data were obtained from a secondary source.
References
- 1.US Census Bureau. The 2012 Statistical Abstract: Life Expectancy. Available at: http://www.census.gov/compendia/statab/2012/tables/12s0105.pdf. Accessed March 5, 2012.
- 2.Centers for Disease Control and Prevention. Wide-Ranging Online Data for Epidemiologic Research. Available at: http://wonder.cdc.gov/controller/datarequest/D67. Accessed November 29, 2011.
- 3.Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System. Available at: http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html. Accessed January 26, 2012.
- 4.Fingerhut LA, Cox CS. Poisoning mortality, 1985–1995. Public Health Rep. 1998;113(3):218–233 [PMC free article] [PubMed] [Google Scholar]
- 5.Rockett IRH, Hobbs G, De Leo Det al. Suicide and unintentional poisoning mortality trends in the United States, 1987–2006: two unrelated phenomena? BMC Public Health. 2010;10:705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warner M, Chen LH, Makuc DM, Anderson RN, Minino AM. Drug Poisoning Deaths in the United States, 1980–2008. Hyattsville, MD: National Center for Health Statistics; 2011. NCHS Data Brief no. 81 [Google Scholar]
- 7.Hu G, Baker SP. Recent increases in fatal and non-fatal injury among people aged 65 years and over in the USA. Inj Prev. 2010;16(1):26–30 [DOI] [PubMed] [Google Scholar]
- 8.McCall PL, Parker KF, MacDonald JM. The dynamic relationship between homicide rates and social, economic, and political factors from 1970 to 2000. Soc Sci Res. 2008;37(3):721–735 [DOI] [PubMed] [Google Scholar]
- 9.Cummings P, Rivara FP, Olson CM, Smith KM. Changes in traffic crash mortality rates attributed to use of alcohol, or lack of a seat belt, air bag, motorcycle helmet, or bicycle helmet, United States, 1982–2001. Inj Prev. 2006;12(3):148–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paulozzi LJ, Ballesteros MF, Stevens JA. Recent trends in mortality from unintentional injury in the United States. J Safety Res. 2006;37(3):277–283 [DOI] [PubMed] [Google Scholar]
- 11.Hu G, Baker SP. Trends in unintentional injury deaths, U.S., 1999–2005: age, gender, and racial/ethnic differences. Am J Prev Med. 2009;37(3):188–194 [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. International Classification of Diseases. 10th revision. Geneva, Switzerland. Available at: http://www.cdc.gov/nchs/icd/icd10.htm. Accessed December 4, 2011.
- 13.Institute of Population Health Metrics. Global Burden of Diseases, Injuries and Risk Factors Study Operations Manual. Table 2, P. 81. Available at: http://www.globalburden.org/gbdops.html. Accessed May 22, 2012.
- 14.Barss P, Smith GS, Baker SP, Mohan D. Injury Prevention: An International Perspective. Epidemiology, Surveillance, and Policy. New York: Oxford University Press; 1998 [Google Scholar]
- 15.Rockett IRH. Injury and violence: a public health perspective. Popul Bull. 1998;53(4):1–40 [PubMed] [Google Scholar]
- 16.Peden M, McGee K, Sharma G. The Injury Chartbook: A Graphical Overview of the Global Burden of Injuries. World Health Organization; 2002. Available at: http://whqlibdoc.who.int/publications/924156220X.pdf. Accessed June 11, 2012.
- 17.Kuratorium für Verkehrssicherheit. Injuries in the European Union. Statistics Summary 2005–2007. Vienna; November 2009. Available at: http://ec.europa.eu/health/healthy_environments/docs/2009-idb-report_screen.pdf. Accessed May 29, 2012.
- 18.SMARTRISK. The Economic Burden of Injury in Canada. Toronto, ON; 2009. Available at: http://www.smartrisk.ca/downloads/burden/Canada2009/EBI-Eng-Final.pdf. Accessed May 29, 2012.
- 19.World Health Organization. A Leading Cause of Death and Disability in China. Western Pacific Region. Available at: http://www2.wpro.who.int/china/sites/injury_prevention. Accessed June 4, 2012.
- 20.Centers for Disease Control and Prevention. Worldwide Injuries and Violence. Available at: http://www.cdc.gov/injury/global. Accessed May 29, 2012.
- 21.Faraway JJ. Extending the Linear Model With R. Boca Raton, FL: Chapman & Hall/CRC; 2006 [Google Scholar]
- 22.Baker SP, O’Neill B, Ginsburg MJ, Li G. The Injury Fact Book. 2nd ed. New York: Oxford University Press; 1992 [Google Scholar]
- 23.Centers for Disease Control and Prevention Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492 [PubMed] [Google Scholar]
- 24.Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician. 2010;13(5):401–435 [PubMed] [Google Scholar]
- 25.American Society of Anesthesiologists Practice guidelines for chronic pain management. A report by the American Society of Anesthesiologists Task Force on Pain Management, Chronic Pain Section. Anesthesiology. 1997;86(4):995–1004 [PubMed] [Google Scholar]
- 26.Van Zee A. The promotion and marketing of OxyContin: commercial triumph, public health tragedy. Am J Public Health. 2009;99(2):221–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD; 2011. NSDUH series H-41, HHS publication SMA 11–4658.
- 28.MetLife Foundation. 2010 Partnership Attitude Tracking Study: Teens and Parents. Available at: http://www.drugfree.org/wp-content/uploads/2011/04/FULL-REPORT-FINAL-PATS-Teens-and-Parent-April-6-2011-1.pdf. Accessed February 20, 2012.
- 29.Brennan MJ, Stanos S. Strategies to optimize pain management with opioids while minimizing risk of abuse. PM R. 2010;2(6):544–558 [DOI] [PubMed] [Google Scholar]
- 30.Mailloux AT, Cummings SW, Mugdh M. A decision support tool for identifying abuse of controlled substances by ForwardHealth Medicaid members. J Hosp Mark Public Relations. 2010;20(1):34–55 [DOI] [PubMed] [Google Scholar]
- 31.Gilson AM, Fishman SM, Wilsey BL, Casamalhuapa C, Baxi H. Time series analysis of California’s Prescription Monitoring Program: impact on prescribing and multiple provider episodes. J Pain. 2012;13(2):103–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bennett KM, Vaslef SN, Shapiro ML, Brooks KR, Scarborough JE. Does intent matter? The medical and societal burden of self-inflicted injury. J Trauma. 2009;67(4):841–847 [DOI] [PubMed] [Google Scholar]
- 33.Goldsmith SK, Pellmar TC, Bunney WE. Reducing Suicide: A National Imperative. Washington, DC: National Academies Press; 2002 [PubMed] [Google Scholar]
- 34.Platt S, Backett S, Kreitman N. Social construction or causal ascription: distinguishing suicide from undetermined deaths. Soc Psychiatry Psychiatr Epidemiol. 1988;23(4):217–221 [DOI] [PubMed] [Google Scholar]
- 35.Rockett IRH, Wang S, Stack Set al. Race/ethnicity and potential suicide misclassification: window on a minority suicide paradox? BMC Psychiatry. 2010;10:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoyert DL. The Changing Profile of Autopsied Deaths in the United States, 1972–2007. Hyattsville, MD: National Center for Health Statistics; 2011. NCHS Data Brief no. 67 [Google Scholar]
- 37.Kapusta ND, Tran US, Rockett IRHet al. Declining autopsy rates and suicide misclassification: a cross-national analysis of 35 countries. Arch Gen Psychiatry. 2011;68(10):1050–1057 [DOI] [PubMed] [Google Scholar]
- 38.US Public Health Service National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, DC: Department of Health and Human Services; 2001 [PubMed] [Google Scholar]
- 39.Institute of Medicine Emergency Medical Services at the Crossroads. Washington, DC: National Academies Press; 2006 [Google Scholar]
- 40.Institute of Medicine Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2006 [Google Scholar]
- 41.Hanzlick R. The conversion of coroner systems to medical examiner systems in the United States: a lull in the action. Am J Forensic Med Pathol. 2007;28(4):279–283 [DOI] [PubMed] [Google Scholar]
- 42.Committee on Identifying the Needs of the Forensic Sciences Community, National Research Council Strengthening Forensic Science in the United States: A Path Forward. Washington, DC: National Academies Press; 2009 [Google Scholar]
- 43.SAMHSA News Release. U.S. Accelerates Suicide Prevention With National Action Alliance Leadership; 2010. Available at: http://www.samhsa.gov/newsroom/advisories/1009103715.aspx. Accessed February 1, 2012.
- 44.Kannus P, Parkkari J, Niemi S, Palvanen M. Fall-induced deaths among elderly people. Am J Public Health. 2005;95(3):422–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Langlois JA, Smith GS, Baker SP, Langley JD. International comparisons of injury mortality in the elderly: issues and differences between New Zealand and the United States. Int J Epidemiol. 1995;24(1):136–143 [DOI] [PubMed] [Google Scholar]
- 46.McGarrell EF, Chermak S, Wilson JM, Corsaro N. Reducing homicide through a “lever–pulling” strategy. Justice Q. 2006;23(2):214–231 [Google Scholar]
- 47.Office of National Drug Policy. High Intensity Drug Trafficking Areas (HIDTA) Program. Available at: http://www.whitehouse.gov/ondcp/high-intensity-drug-trafficking-areas-program. Accessed February 1, 2012.
- 48.Webster DW, Whitehill Mendel J, Vernick JS, Parker EM. Evaluation of Baltimore’s Safe Streets Program. Effects on Attitudes, Participants’ Experiences, and Gun Violence. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; 2012 [Google Scholar]
- 49.Sivak M, Schoettle B. Toward understanding the recent large reductions in U.S. road fatalities. Traffic Inj Prev. 2010;11(6):561–566 [DOI] [PubMed] [Google Scholar]
- 50.Wagenaar AC, Zobeck TS, Williams GD, Hingson R. Methods used in studies of drink–drive control efforts: a meta-analysis of the literature from 1960 to 1991. Accid Anal Prev. 1995;27(3):307–316 [DOI] [PubMed] [Google Scholar]
- 51.National Center for Injury Prevention and Control Prevention of Motor Vehicle-Related Injuries: A Compendium of Articles From the Morbidity and Mortality Weekly Report, 1985–1996. Atlanta, GA: Centers for Disease Control and Prevention; 1997 [Google Scholar]
- 52.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283(15):1990–1994 [DOI] [PubMed] [Google Scholar]
- 53.Shafi S, Nathens AB, Elliott AC, Gentilello L. Effect of trauma systems on motor vehicle occupant mortality: a comparison between states with and without a formal system. J Trauma. 2006;61(6):1374–1378 [DOI] [PubMed] [Google Scholar]
- 54.Miller TR, Bhattacharya S, Zaloshnja E. Fruits of 20 years of highway safety legislative advocacy in the United States. Ann Adv Automot Med. 2011;55:357–363 [PMC free article] [PubMed] [Google Scholar]
- 55.Wilson FA, Stimpson JP. Trends in fatalities from distracted driving in the United States, 1999 to 2008. Am J Public Health. 2010;100(11):2213–2219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lichenstein R, Smith DC, Ambrose JL, Moody LA. Headphone use and pedestrian injury and death in the United States: 2004–2011. Inj Prev. 2012; Epub ahead of print [DOI] [PubMed] [Google Scholar]
- 57.Roudsari B, Ramisetty-Mikler S, Rodriguez LA. Ethnicity, age, and trends in alcohol-related driver fatalities in the United States. Traffic Inj Prev. 2009;10(5):410–414 [DOI] [PubMed] [Google Scholar]
- 58.Coben JH, Steiner CA, Miller TR. Characteristics of motorcycle-related hospitalizations: comparing states with different helmet laws. Accid Anal Prev. 2007;39(1):190–196 [DOI] [PubMed] [Google Scholar]
- 59.Institute of Medicine Regionalizing Emergency Care: Workshop Summary. Washington, DC: National Academies Press; 2010 [PubMed] [Google Scholar]
- 60.Buescher PA, Gizlice Z, Jones-Vessey KA. Discrepancies between published data on racial classification and self-reported race: evidence from the 2002 North Carolina live birth records. Public Health Rep. 2005;120(4):393–398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Noymer A, Penner AM, Saperstein A. Cause of death affects racial classification on death certificates. PLoS ONE. 2011;6(1):e15812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.National Center for Health Statistics. Physicians’ Handbook on Medical Certification of Death, 2003 Revision. Hyattsville, MD; 2003. DHHS publication no. PHS 2003–1108.
- 63.National Center for Health Statistics. Funeral Directors’ Handbook on Death Registration and Fetal Death Reporting, 2003 Revision. Hyattsville, MD; 2004. DHHS publication no. PHS 2005–1109.
- 64.Gielen AC, Sleet DA, DiClemente RJ. Injury and Violence Prevention: Behavioral Science Theories, Methods, and Applications. San Francisco: Jossey-Bass; 2006 [Google Scholar]
- 65.Centers for Disease Control and Prevention. 10 Leading Causes of Death by Age Group, United States—2009. Available at: http://www.cdc.gov/Injury/wisqars/pdf/10LCD-Age-Grp-US-2009-a.pdf. Accessed June 12, 2012.
- 66.Iowa Department of Public Health. The Burden of Injury in Iowa, Comprehensive Injury Report, 2002–2006; December 2008. Available at: http://www.idph.state.ia.us/bh/common/pdf/injury_prevention/burden_of_injury_full_report.pdf. Accessed June 11, 2012.
- 67.Wisconsin Department of Health and Family Services’ Injury Prevention Program. The Burden of Injury in Wisconsin; fall 2006. Available at: http://www.dhs.wisconsin.gov/health/injuryprevention/pdffiles/injuryreport.pdf. Accessed June 11, 2012.
- 68.Paulozzi L, Dellinger A, Degutis L. Lessons from the past. Inj Prev. 2012;18(1):70. [DOI] [PubMed] [Google Scholar]
- 69.Murphy SL, Xu J, Kochanek KD. Deaths: preliminary data for 2010. Natl Vital Stat Rep. 2012;60(4):1–69 [PubMed] [Google Scholar]
- 70.Rockett IRH. Injury elimination and survival: a cross-national study. Public Health. 1998;112(1):27–30 [PubMed] [Google Scholar]