Abstract
Objectives. We examined health-related quality of life in adults who became physically active at recommended levels over a 10-year period compared with adults with different physical activity patterns.
Methods. We examined men and women aged 26 to 70 years (mean [SD] = 47.4 [10.1]) in the Doetinchem Cohort Study 3 times between 1995 and 2009. We distinguished participants who became physically active (n = 618), remained active (n = 1286), remained inactive (n = 727), became physically inactive (n = 535), or with varying activity levels (n = 455) over 10 years. We used multivariable linear regression analyses to determine differences in health-related quality of life (survey similar to the 36-Item Short-Form Health Survey) at 10-year follow-up.
Results. Adults who became physically active reported better physical functioning, vitality, and general health after 10 years than did persistently inactive adults and adults who became inactive. They also reported less bodily pain and better social functioning than adults who became inactive. No differences were observed with adults who remained active or with varying activity levels.
Conclusions. Adopting a physically active lifestyle may result in a better health-related quality of life, comparable to remaining physically active over 10 years.
It is often suggested that lifestyle during childhood, adolescence, and middle age will affect health in old age. A lifelong healthy lifestyle is assumed to be the most favorable for health in an aging population.1 Whether adopting a healthy lifestyle during middle age is too late or still effective is unknown. The prospect of better health and health-related quality of life may help motivate adults to change unhealthy lifestyles, and may therefore be important for public health.
Physical inactivity is associated with future health problems such as obesity, diabetes, cardiovascular diseases, stroke, certain types of cancer,2–5 and also with reduced levels of health-related quality of life.6–10 Most evidence regarding physical activity and future health is based on measuring physical activity at one point in time only. However, physical activity is likely to change over the course of life.11,12 Only a minority of the general population remains physically active for longer periods of time during the life course.
In the United States, only 11% of the population remained active during an 8-year period in midlife whereas a majority (59%) remained inactive during this period.12 Physical activity levels were higher in Dutch adults: almost one third of adults were physically active during 10 years, whereas 24% were inactive and 18% became physically active.11 Health effects of becoming active versus remaining inactive over longer periods of time are largely unknown. Two studies in women and university graduates have suggested that improvements in health-related quality of life are likely to occur in those who increased their physical activity levels.13,14 It is not clear whether this is also the case for levels of physical activity that go beyond the physical activity recommendations.
The objective of this study was to examine the relation between long-term physical activity levels and health-related quality of life. We focused on the impact of becoming physically active. We compared adults who were inactive at baseline and became active during 10 years of follow-up with adults who remained physically inactive, remained active, became inactive, and reported varying levels of activity. We hypothesized that adults who became physically active would report a better health-related quality of life after 10 years than adults who remained or became inactive, and a poorer health-related quality of life than adults who had been active and remained active during this period.
METHODS
The Doetinchem Cohort Study is a prospective population-based study on lifestyle, biological risk factors, and health during adulthood. The first examination round (1987–1991) was carried out among 12 405 men and women (initial response 62%) aged 20 to 59 years in Doetinchem, a town in the Eastern part of the Netherlands. Of those 12 405 participants, a random sample of 7769 participants was reinvited once every 5 years to participate in the second, third, fourth, and fifth (ongoing) rounds. Response rates of the second to fifth round were 79%, 75%, 78%, and 79%, respectively (Figure A available as a supplement to the online version of this article at http://www.ajph.org). The study is described in more detail elsewhere.15 Health-related quality of life was measured from the year 1995 onward. Therefore, for the present analyses, we considered the period 1995 to 1999 as t0 (baseline), 2000 to 2004 as t1, and 2005 to 2009 as t2. An ethical review board approved the protocol of the Doetinchem Cohort Study. All participants gave written informed consent.
Measurement of Physical Activity
Physical activity was measured with a self-administered questionnaire designed for the international European Prospective Investigation Into Cancer and Nutrition study and extended with a question on sports and other strenuous leisure-time physical activities.16 Time spent on leisure-time activities (bicycling, gardening) was assessed for summer and winter separately. Respondents were asked about time spent on sports and other strenuous physical activities during a regular week in the previous year. These included open-ended questions on type, frequency, and duration for a maximum of 3 different activities. In accordance with the Dutch guideline for physical activity,17 leisure-time physical activities of at least 4.0 metabolic equivalents were considered.
To determine whether individuals reached the recommended levels, we calculated the total amount of time (hours per week) spent on moderate-to-vigorous leisure-time physical activities and heavy work. To ensure a conservative estimate for cycling and gardening, we used the smallest number of hours per week reported for either summer or winter. We included total time spent in jobs that require heavy physical work, such as the physical activity required in construction work, farming, or cleaning. The Dutch physical activity guideline recommends adults to be physically active at a moderate or higher intensity for a minimum of half an hour a day on at least 5 days a week (i.e., at least 2.5 hours per week).17,18 We set the cut-off point for reaching the recommended levels at 3.5 hours a week spent on at least moderately intense physical activities. There are 2 reasons for this cut-off point: to account for the observation that the amount of activity is usually overreported19 and the fact that we have only data averaged during a week whereas the recommended levels pertain to at least 5 days a week.
We defined 5 different (longitudinal) time patterns of physical activity using data from the 3 consecutive measurements.11 We classified adults who were inactive at t0 but who had become physically active at the second or third measurement as becoming active. We classified adults who were inactive at all 3 measurements as persistently inactive, and adults who were physically active at all 3 measurements as persistently active. We classified adults who were active at t0 and had become inactive at the second or third measurement as becoming inactive. We classified the remaining individuals as adults with varying activity levels, namely those with the following patterns: active–inactive–active or inactive–active–inactive.
Measurement of Quality of Life
We measured health-related quality of life with the Dutch version of the RAND36, which is similar to the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36).20,21 The 8 dimensions of the SF-36 are physical functioning, role limitations because of physical health problems, bodily pain, general health perceptions, vitality, social functioning, role limitations because of emotional problems, and mental health. The validity and reliability of the SF-36 have been established.21 For each dimension, scores are coded, summed, and transformed to a 0-to-100 scale. Higher scores indicate higher levels of functioning or well-being.
During the 10-year follow-up, we defined educational level as the highest education obtained. We distinguished 3 categories: low (intermediate secondary education or less), moderate (intermediate vocational or higher secondary education), and high (higher vocational education or university). We defined work status at t2 as having a paying job (including salaried employment and being self-employed) or not (including being a housewife, retired, unable to work, and other). We defined household composition at t2 as living alone or not living alone (living with a partner, with children, with parents, or with other adults). We categorized smoking behavior at t2 as current smoker or nonsmoker; the latter included exsmokers. We calculated body mass index (BMI, defined as weight in kilograms divided by the square of height in meters) at t2 from measured height and body weight. We categorized BMI as normal (< 25 kg/m2), overweight (25–< 30 kg/m2), and obesity (≥ 30 kg/m2). Six chronic diseases were (self)-reported at all measurements, i.e., diabetes mellitus, myocardial infarction, stroke, cancer, asthma, and persistent chronic low back pain. We constructed dummy variables for chronic disease status at baseline and during follow-up on the basis of having any of these 6 chronic diseases.
Statistical Analyses
A total of 3848 respondents participated in all 3 examination rounds. We excluded women who were pregnant at 1 of the 3 measurements (n = 41) and respondents with missing values on any of the variables used in the analyses (n = 186), leaving 3621 respondents for the analyses (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). We found that 1286 adults were persistently active, 727 adults were persistently inactive, 618 adults were inactive at baseline but became active during the 10-year follow-up period, 535 adults became inactive, and 455 adults had varying physical activity levels.
We summarized characteristics of the study population as means and we determined standard deviations and mean adjusted health-related quality-of-life scores for each physical activity pattern. We performed multivariable linear regression analyses to determine differences in health-related quality of life between adults who became active versus the 4 other physical activity patterns. We observed skewed distributions of residuals for 5 subscales: physical functioning, bodily pain, social functioning scales, and for role limitations because physical and mental health problems. We applied linear regressions using generalized estimated equations with estimation of robust standard errors for these 5 subscales. We adjusted each regression analysis for gender, age, education, living alone status, work status, BMI, smoking, and baseline and chronic disease status during follow-up.
Mean health-related quality of life at baseline differed according to physical activity patterns; therefore we adjusted all analyses for baseline SF-36 scale score. We calculated differences between the adjusted means (and 95% confidence intervals) in health-related quality of life of adults who became active versus adults in the 4 other physical activity patterns by the least squares means option. We expressed differences as the number of standard deviations from the population mean. We tested interaction effects between physical activity patterns and gender and age in the crude regression models (P < .1). Interaction effects occurred only in a few comparisons; therefore, we additionally described results of stratified analyses for these domains only. We used SAS software version 9.2 (SAS Institute, Cary, NC).
RESULTS
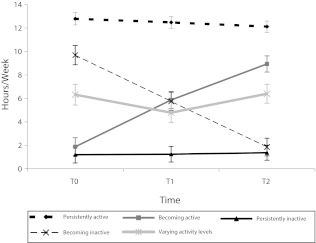
About 48% of the study population were male and the mean age at baseline was 47 years for all 5 physical activity patterns (Table 1). Adults who remained active over the 10-year period spent on average 12 or 13 hours per week on at least moderately intense physical activities, whereas those who remained inactive spent 1 hour only per week on such activities (Figure 1). Adults who became active reported on average 2 hours a week of moderate and vigorous intensity at baseline, and 6 and 9 hours, respectively, per week at the second and third examination. Those who became inactive reported, on average, 10, 6, and 2 hours, respectively, of these activities per week. The mean number of hours of moderate-to-vigorous physical activities among adults with varying levels of activity was quite constant at 5 and 6 hours a week over the 3 rounds. Persistently active adults reported the highest health-related quality of life scores for most domains, except for general health and role limitations because of physical health problems. Adults who became active reported the best general health, and those with varying levels of activity reported the fewest role limitations because of physical health problems (Table 2).
TABLE 1—
Characteristics of the Study Population, Men and Women Aged 26–70 Years: the Doetinchem Cohort Study, 1995–2009
| Characteristic | Becoming Active (n = 618), % or Mean ±SD | Persistently Active (n = 1286), % or Mean ±SD | Persistently Inactive (n = 727), % or Mean ±SD | Becoming Inactive (n = 535), % or Mean ±SD | Varying Activity Levels (n = 455), % or Mean ±SD |
| Gender: male | 48.9 | 48.4 | 49.0 | 45.6 | 48.6 |
| Age at t0, y | 47.3 ±9.7 | 47.3 ±10.1 | 47.9 ±10.2 | 47.4 ±10.5 | 47.0 ±10.2 |
| Highest level of educationa | |||||
| High | 26.8 | 28.5 | 29.8 | 22.4 | 25.3 |
| Moderate | 31.4 | 35.3 | 29.2 | 36.3 | 29.9 |
| Low | 41.8 | 36.2 | 41.0 | 41.3 | 44.8 |
| Living alone at t2 | 11.5 | 11.5 | 14.6 | 14.6 | 12.8 |
| Paid job at t2 | 53.7 | 57.3 | 52.3 | 53.3 | 53.4 |
| Smoking at t2 | 18.6 | 14.9 | 23.7 | 20.0 | 19.6 |
| BMI at t2 | |||||
| Normal (< 25 kg/m2) | 38.9 | 39.3 | 39.5 | 32.3 | 38.0 |
| Overweight (25< 30 kg/m2) | 45.6 | 47.4 | 39.8 | 49.2 | 44.0 |
| Obese (≥ 30 kg/m2) | 15.5 | 13.3 | 20.8 | 18.5 | 18.0 |
| Chronic disease statusb | |||||
| t0 | 18.9 | 19.4 | 24.5 | 24.5 | 24.8 |
| Follow-up | 36.0 | 38.5 | 41.7 | 39.8 | 36.3 |
| Health-related quality of life at t0 | |||||
| Physical functioning | 91.3 ±13.2 | 89.4 ±15.6 | 86.3 ±18.4 | 88.9 ±15.1 | 88.7 ±15.8 |
| Physical role limitations | 85.1 ±30.0 | 83.3 ±30.7 | 81.4 ±32.6 | 83.2 ±30.7 | 83.7 ±31.0 |
| Bodily pain | 81.9 ±20.9 | 81.0 ±21.2 | 79.1 ±22.2 | 79.9 ±21.3 | 79.6 ±22.0 |
| General health | 75.3 ±16.0 | 73.5 ±16.8 | 71.5 ±17.9 | 74.1 ±16.7 | 74.3 ±16.0 |
| Vitality | 69.6 ±16.1 | 67.0 ±17.0 | 65.1 ±17.6 | 67.0 ±17.1 | 67.2 ±15.4 |
| Social functioning | 87.7 ±18.7 | 86.1 ±20.8 | 86.1 ±20.2 | 86.3 ±19.4 | 86.6 ±19.0 |
| Emotional role limitations | 89.4 ±26.7 | 86.2 ±30.2 | 86.6 ±29.2 | 85.9 ±29.6 | 88.2 ±28.1 |
| Mental health | 78.3 ±13.9 | 76.6 ±14.8 | 76.2 ±15.1 | 75.6 ±15.3 | 76.6 ±14.4 |
Note. BMI = body mass index.
Education categories defined as high (higher vocational education or university), moderate (intermediate vocational or higher secondary education), and low (intermediate secondary education or less).
Self-reported diabetes mellitus, myocardial infarction, stroke, cancer, asthma, and persistent chronic low-back pain.
FIGURE 1—
Total time spent on moderate to vigorous physical activity per measurement and physical activity pattern among men and women aged 26–70 years: the Doetinchem Cohort Study, 1995–2009.
Note. Whiskers represent 95% confidence intervals.
TABLE 2—
Adjusted Health-Related Quality of Life Scale Scores at t2 for Men and Women Aged 26–70 Years: the Doetinchem Cohort Study, 1995–2009
| Adjusted Scores at t2a |
|||||
| Domain | Becoming Active, Mean (95% CI) | Persistently Active, Mean (95% CI) | Persistently Inactive, Mean (95% CI) | Becoming Inactive, Mean (95% CI) | Varying Activity Levels, Mean (95% CI) |
| Physical functioning | 87.2 (86.1, 88.2) | 88.1 (87.3, 88.8) | 85.5 (84.4, 86.5) | 84.8 (83.4, 86.2) | 87.8 (86.5, 89.1) |
| Physical role limitations | 83.4 (81.0, 85.8) | 85.6 (84.0, 87.1) | 80.8 (78.4, 83.2) | 81.1 (78.3, 83.9) | 86.1 (83.5, 88.7) |
| Bodily pain | 78.1 (76.7, 79.5) | 79.2 (78.2, 80.2) | 77.1 (75.8, 78.4) | 75.2 (73.6, 76.9) | 78.3 (76.5, 80.1) |
| General health | 71.7 (70.6, 72.8) | 70.8 (70.1, 71.6) | 68.8 (67.7, 69.8) | 68.8 (67.6, 70.0) | 70.2 (68.9, 71.5) |
| Vitality | 70.1 (69.0, 71.2) | 70.6 (69.8, 71.4) | 68.4 (67.4, 69.4) | 67.5 (66.3, 68.7) | 69.6 (68.3, 70.9) |
| Social functioning | 88.9 (87.6, 90.2) | 89.5 (88.6, 90.4) | 87.7 (86.4, 89.0) | 86.5 (85.0, 88.1) | 89.2 (87.7, 90.7) |
| Emotional role limitations | 91.0 (89.0, 93.0) | 91.3 (90.0, 92.6) | 89.1 (87.1, 91.0) | 88.2 (85.8, 90.6) | 90.9 (88.6, 93.2) |
| Mental health | 78.6 (77.7, 79.6) | 79.4 (78.8, 80.1) | 78.8 (77.9, 79.7) | 78.1 (77.1, 79.1) | 79.3 (78.2, 80.4) |
Note. CI = confidence interval.
Mean scores adjusted for gender, age, education, living alone, work status, smoking, baseline and follow-up chronic disease status, and baseline score on the Dutch version of the RAND36, which is similar to the Medical Outcomes Study 36-Item Short-Form Health Survey.
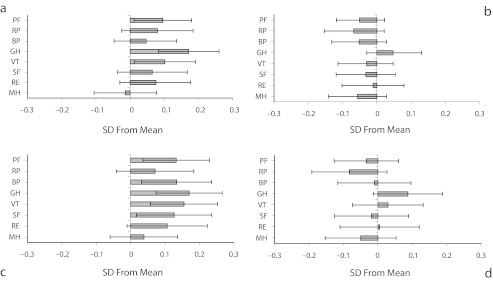
We observed significant differences in health-related quality of life between adults who became active and adults who remained inactive, and between adults who became active and adults who became inactive (Figure 2). Adults who became active during the 10-year follow-up reported better physical functioning, general health, and vitality compared with persistently inactive adults, scoring 1.7 (95% confidence interval [CI] = 0.2, 3.2) points higher for physical functioning, 2.9 (95% CI = 1.4, 4.4) points higher for general health, and 1.7 (95% CI = 0.2, 3.2) points higher for vitality. The scores for bodily pain, social functioning, mental health, and physical and emotional role limitations did not differ. We observed interaction effects with gender for general health, physical functioning, physical role limitations, and mental health. However, in gender-stratified analyses, only the difference in general health was significant in women (women 3.7; 95% CI = 1.6, 5.8; men 1.9; 95% CI = −0.2, 4.1). Although we observed no differences in physical role limitations, women who became active scored 5.9 (95% CI = 1.0, 10.8) points higher for physical role limitations than women who remained inactive.
FIGURE 2—
Adjusted differences in health-related quality of life scores among men and women aged 26–70 years at t2 during the 10-year follow-up between (a) becoming active and remaining inactive, (b) becoming active and remaining active, (c) becoming active and becoming inactive, and (d) becoming active and reporting varying activity levels: the Doetinchem Cohort Study, 1995–2009.
Note. BP = bodily pain; GH = general health; MH = mental health; PF = physical functioning; RE = role limitations emotional; RP = role limitations physical; SF = social functioning; VT = vitality. Adjusted for gender, age, education, living alone, work status, body mass index (defined as weight in kilograms divided by the square of height in meters), smoking, baseline and follow-up chronic disease status, and baseline score on the Dutch version of the RAND36, which is similar to the Medical Outcomes Study 36-Item Short-Form Health Survey. Differences expressed as number of standard deviations from the population mean with corresponding 95% confidence intervals.
Adults who became active reported better physical functioning (2.4; 95% CI = 0.6, 1.7 points higher), general health (2.9; 95% CI = 1.3, 4.5 points higher), vitality (2.6; 95% CI = 1.0, 4.2 points higher), social functioning (2.4; 95% CI = 0.3, 4.4 points higher), and less bodily pain (2.9; 95% CI = 0.7, 5.0 points higher) compared with adults who became inactive. The scores for mental health and physical role limitations did not differ between adults who became active and those who became inactive. We observed fewer role limitations among adults younger than 55 years who became active compared with those who became inactive (4.8; 95% CI = 1.4, 8.3 points higher). Interaction analyses also showed that we only observed better physical functioning and less bodily pain among adults who became active among those aged 55 years or older (8.5; 95% CI = 4.4, 12.6 and 7.8; 95% CI = 3.3, 12.2 points higher, respectively). We observed interaction with gender for vitality, which remained statistically significant in men only (men 4.0; 95% CI = 1.6, 6.3; women 1.2; 95% CI = −1.0, 3.5).
Although adults who became active reported somewhat lower health-related quality of life than those who were persistently active, we observed no significant differences between adults who became active and those persistently active or those with varying levels of activity.
DISCUSSION
Ten-year data on physical activity showed that adults who became active reported a health-related quality of life that was nearly as good as that of adults who were active over the whole study period. Moreover, adults who became physically active reported better physical functioning, general health, and vitality compared with those who remained inactive and also compared with those who were active at baseline but became inactive over the 10-year period. Adults who became physically active also reported less bodily pain and better social functioning than those who became inactive. Moreover, fewer physical role limitations were reported by women who became active compared with persistently inactive women, and fewer emotional role limitations were reported by adults younger than 55 years who became active compared with those who became inactive. Therefore, it seems worthwhile to become physically active during adulthood at levels recommended by current guidelines.
As physical activity is not a stable feature over time, it is remarkable that we observed such strong and consistent health effects of physical activity on the basis of single measurements.22,23 We identified 2 other studies with longitudinal measurements of physical activity, both showing a better health-related quality of life for adults who became physically active.13,14 Wolin et al. observed that women who increased their level of physical activity over 10 years reported a better health-related quality of life on all domains after 10 years compared with those who maintained their level of physical activity, among 63 152 middle- and old-aged women.14 Their findings for physical functioning, vitality, and general health were in line with ours, but we did not find differences for all domains of quality of life. Recently, Sanchez-Villegas et al. showed that remaining physically active or becoming more physically active resulted in a better health-related quality of life in 4206 middle-aged university graduates after 8 years compared with those with decreasing levels of physical activity.13 Their findings showed improvements after becoming active in particular in the mental domains of health-related quality of life. Improvements in mental domains were not confirmed in our study, except for social functioning.
Long-term physical activity patterns were also investigated in relation to physical functioning assessed by performance tests, confirming the positive effects on physical functioning both of remaining active and of becoming active.1,24,25 The finding that increased levels of physical activity are particularly associated with a better health-related quality of life in women is confirmed in other studies, but a clear explanation is lacking.26,27
We found no studies that assessed the impact of maintaining recommended physical activity levels over several years in relation to health-related quality of life. By categorizing active and inactive adults according to recommended levels, our findings can be easily translated to interventions that aim to promote physical activity in inactive adults. A disadvantage of this approach could be that small increases in the duration of activities—for instance, an increase of only 15 minutes per week—may result in being classified as active instead of inactive. However, Figure 1 shows that adults who became active at recommended levels had quite a large increase in the number of hours spent on moderate intensity, from on average 2 hours a week at baseline to 9 hours a week after 10 years.
Our hypothesis that adults who became physically active report a better health-related quality of life after 10 years compared with adults who remained and became inactive was confirmed for physical functioning, general health, and vitality. Literature supports the finding that higher physical activity levels are associated more consistently with better physical functioning and vitality than other domains,8,9,22 but support for an association between physical activity and mental health is also present.13,28 Why we did not observe associations with the mental domain is unclear and is contrary to earlier analyses that showed that a 1-hour-per-week increase in physical activity over 5 years was associated with better mental health in men.28 Current findings are based on a longer follow-up than most studies, suggesting that better physical functioning is long lasting whereas better mental health may be more short term and not sustained. Different intensities of activities may also explain discrepancies with other studies because it is known that higher-intensity sports cause a release of hormones such as endorphins, leading to feelings of well-being.29
Our second hypothesis, that adults who become active would still report a poorer health-related quality of life compared with adults who were active during the whole 10-year period because of an accumulation of favorable health effects,30 was not supported by our findings. This may constitute an optimistic message for inactive adults. An explanation for this could be that the favorable effect of physical activity on health-related quality of life is more a direct effect than a cumulative effect.31 The number of hours per week spent on moderate-to-vigorous physical activities reported at the third measurement of persistently active adults and those with varying activity levels most closely resembled those of adults who became active (Figure 1). We subsequently observed no differences in health-related quality of life between those patterns. Direct effects of physical activity on health-related quality of life is also supported by the finding that adults who became inactive reported lower health-related quality of life on most domains.
Long-term prospective studies such as the Doetinchem Cohort Study provide a wealth of opportunities to study dynamics in lifestyles and their effects on health during the life course. Strengths of this study are the prospective data collection, good participation rates, and the use of an extensive and identical questionnaire to measure physical activity at 3 successive examinations. However, some limitations should be taken into account when one is interpreting the findings. Self-reported physical activity levels usually overestimate actual physical activity levels.19 With the use of the lowest number of hours for winter and summer, we minimized overestimation in our study. However, to be able to capture all elements of physical activity that might influence long-term health, more detailed measurements and a more objective assessment of physical activity are needed.
Measurements of physical activity and health-related quality of life after 10 years occurred concurrently. Therefore, a causal relationship between becoming physically active and a better quality of life cannot be established on the basis of our findings. For instance, the reason that adults became inactive could be the occurrence of health problems. We adjusted analyses for chronic disease status at baseline and follow-up, for the most prevalent chronic diseases. However, the lack of information on less-prevalent diseases could lead to some residual confounding by chronic disease status.
Like in other prospective studies, more healthy participants tended to remain in the study during extended follow-ups. Nonrespondents were more frequently overweight, lower educated, smokers, and inactive compared with complete cases.32 The prevalence of being persistently active may be slightly overestimated because of this; however, the associations between physical activity patterns and health-related quality of life are usually not affected by small violations of representativeness.
This is the first study examining the association between becoming active over a period of 10 years versus other long-term physical activity patterns and health-related quality of life. The findings suggest a health benefit of becoming physically active during adult age. Higher levels of health-related quality of life may be achieved by public health strategies supporting inactive adults to adopt and maintain a physically active lifestyle during adulthood.
Acknowledgments
The Doetinchem Cohort Study is funded by the National Institute for Public Health and the Environment, which works under the authority of the Ministry of Health, Welfare and Sport of the Netherlands.
The authors would like to thank the epidemiologists and fieldworkers of the Municipal Health Service in Doetinchem for their contribution to the data collection for this study.
Note. The funding source had no involvement in analyses and interpretation of the data, writing of the report, or decision to submit the article.
Human Participant Protection
The Doetinchem Cohort Study was approved according to the guidelines of the Helsinki Declaration by the external Medical Ethic Committee of the Netherlands Organization of Applied Scientific Research Institute and of the University of Utrecht (5th round). All participants gave written informed consent.
References
- 1.Pluijm SM, Visser M, Puts MTet al. Unhealthy lifestyles during the life course: association with physical decline in late life. Aging Clin Exp Res. 2007;19(1):75–83 [DOI] [PubMed] [Google Scholar]
- 2.Friedenreich CM, Neilson HK, Lynch BM. State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer. 2010;46(14):2593–2604 [DOI] [PubMed] [Google Scholar]
- 3.Kesaniemi YK, Danforth E, Jr, Jensen MD, Kopelman PG, Lefebvre P, Reeder BA. Dose-response issues concerning physical activity and health: an evidence-based symposium. Med Sci Sports Exerc. 2001;33(6, Suppl):S351–S358 [DOI] [PubMed] [Google Scholar]
- 4.Wendel-Vos GC, Schuit AJ, Feskens EJet al. Physical activity and stroke. A meta-analysis of observational data. Int J Epidemiol. 2004;33(4):787–798 [DOI] [PubMed] [Google Scholar]
- 5.Physical Activity Guidelines Advisory Committee Physical Activity Guidelines Advisory Committee Report, 2008. Washington, DC: US Department of Health and Human Services; 2008 [DOI] [PubMed] [Google Scholar]
- 6.Blomstrand A, Bjorkelund C, Ariai N, Lissner L, Bengtsson C. Effects of leisure-time physical activity on well-being among women: a 32-year perspective. Scand J Public Health. 2009;37(7):706–712 [DOI] [PubMed] [Google Scholar]
- 7.Hillsdon MM, Brunner EJ, Guralnik JM, Marmot MG. Prospective study of physical activity and physical function in early old age. Am J Prev Med. 2005;28(3):245–250 [DOI] [PubMed] [Google Scholar]
- 8.Savela SL, Koistinen P, Tilvis RSet al. Physical activity at midlife and health-related quality of life in older men. Arch Intern Med. 2010;170(13):1171–1172 [DOI] [PubMed] [Google Scholar]
- 9.Sun Q, Hu FB, Grodstein F. Invited commentary—physical activity benefits various aspects of healthy aging: comment on “Physical activity at midlife and health-related quality of life in older men.” Arch Intern Med. 2010;170(13):1172–1173 [DOI] [PubMed] [Google Scholar]
- 10.Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F. Physical activity at midlife in relation to successful survival in women at age 70 years or older. Arch Intern Med. 2010;170(2):194–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Picavet HSJ, Wendel-Vos GC, Vreeken HL, Schuit AJ, Verschuren WMM. How stable are physical activity habits among adults? The Doetinchem Cohort Study. Med Sci Sports Exerc. 2011;43(1):74–79 [DOI] [PubMed] [Google Scholar]
- 12.Parsons TJ, Manor O, Power C. Changes in diet and physical activity in the 1990s in a large British sample (1958 birth cohort). Eur J Clin Nutr. 2005;59(1):49–56 [DOI] [PubMed] [Google Scholar]
- 13.Sanchez-Villegas A, Ara I, Dierssen T, de la Fuente C, Ruano C, Martinez-Gonzalez MA. Physical activity during leisure time and quality of life in a Spanish cohort: SUN (Seguimiento Universidad de Navarra) Project. Br J Sports Med. 2012;46(6):443–448 [DOI] [PubMed] [Google Scholar]
- 14.Wolin KY, Glynn RJ, Colditz GA, Lee IM, Kawachi I. Long-term physical activity patterns and health-related quality of life in U.S. women. Am J Prev Med. 2007;32(6):490–499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verschuren WM, Blokstra A, Picavet HS, Smit HA. Cohort profile: the Doetinchem Cohort Study. Int J Epidemiol. 2008;37(6):1236–1241 [DOI] [PubMed] [Google Scholar]
- 16.Pols MA, Peeters PH, Ocke MC, Slimani N, Bueno-de-Mesquita HB, Collette HJ. Estimation of reproducibility and relative validity of the questions included in the EPIC Physical Activity Questionnaire. Int J Epidemiol. 1997;26(Suppl 1):S181–S189 [DOI] [PubMed] [Google Scholar]
- 17.Kemper HGC, Ooijendijk WTM, Stiggelbout M. Agreement on the Dutch recommended level of physical activity [in Dutch]. Tijdschr Soc Gezondheidsz. 2000;78:180–183 [Google Scholar]
- 18.Ainsworth BE, Haskell WL, Whitt MCet al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9, Suppl):S498–S504 [DOI] [PubMed] [Google Scholar]
- 19.Wilcox S, King AC. Self-favoring bias for physical activity in middle-aged and older adults. J Appl Soc Psychol. 2000;30(9):1773–1789 [Google Scholar]
- 20.van der Zee KI, Sanderman R. Measuring general health status with the RAND-36, a manual [in Dutch]. Groningen, The Netherlands: Noordelijk Centrum voor Gezondheidsvraagstukken, Rijksuniversiteit Groningen; 1993.
- 21.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston, MA: New England Medical Center, The Health Institute; 1993 [Google Scholar]
- 22.Bize R, Johnson JA, Plotnikoff RC. Physical activity level and health-related quality of life in the general adult population: a systematic review. Prev Med. 2007;45(6):401–415 [DOI] [PubMed] [Google Scholar]
- 23.Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No. 2):23–35 [DOI] [PubMed] [Google Scholar]
- 24.Brach JS, FitzGerald S, Newman ABet al. Physical activity and functional status in community-dwelling older women: a 14-year prospective study. Arch Intern Med. 2003;163(21):2565–2571 [DOI] [PubMed] [Google Scholar]
- 25.Visser M, Pluijm SM, Stel VS, Bosscher RJ, Deeg DJ. Physical activity as a determinant of change in mobility performance: the Longitudinal Aging Study Amsterdam. J Am Geriatr Soc. 2002;50(11):1774–1781 [DOI] [PubMed] [Google Scholar]
- 26.Morimoto T, Oguma Y, Yamazaki S, Sokejima S, Nakayama T, Fukuhara S. Gender differences in effects of physical activity on quality of life and resource utilization. Qual Life Res. 2006;15(3):537–546 [DOI] [PubMed] [Google Scholar]
- 27.Tessier S, Vuillemin A, Bertrais Set al. Association between leisure-time physical activity and health-related quality of life changes over time. Prev Med. 2007;44(3):202–208 [DOI] [PubMed] [Google Scholar]
- 28.Wendel-Vos GC, Schuit AJ, Tijhuis MA, Kromhout D. Leisure time physical activity and health-related quality of life: cross-sectional and longitudinal associations. Qual Life Res. 2004;13(3):667–677 [DOI] [PubMed] [Google Scholar]
- 29.Goldfarb AH, Hatfield BD, Armstrong D, Potts J. Plasma beta-endorphin concentration: response to intensity and duration of exercise. Med Sci Sports Exerc. 1990;22(2):241–244 [PubMed] [Google Scholar]
- 30.Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. J Epidemiol Community Health. 2003;57(10):778–783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blane D, Higgs P, Hyde M, Wiggins RD. Life course influences on quality of life in early old age. Soc Sci Med. 2004;58(11):2171–2179 [DOI] [PubMed] [Google Scholar]
- 32.Blokstra A, Smit HA, Verschuren WMM. Changes in lifestyle factors and risk factors for chronic diseases with ageing: the Doetinchem Study 1987–2002 [in Dutch]. Bilthoven, The Netherlands: National Institute of Public Health and the Environment; 2010.