Abstract
Indigenous populations have been identified as vulnerable to climate change. This framing, however, is detached from the diverse geographies of how people experience, understand, and respond to climate-related health outcomes, and overlooks nonclimatic determinants. I reviewed research on indigenous health and climate change to capture place-based dimensions of vulnerability and broader determining factors. Studies focused primarily on Australia and the Arctic, and indicated significant adaptive capacity, with active responses to climate-related health risks. However, nonclimatic stresses including poverty, land dispossession, globalization, and associated sociocultural transitions challenge this adaptability. Addressing geographic gaps in existing studies alongside greater focus on indigenous conceptualizations on and approaches to health, examination of global–local interactions shaping local vulnerability, enhanced surveillance, and an evaluation of policy support opportunities are key foci for future research.
The global climate is changing and will continue to change.1,2 Research is only beginning to examine the potential health implications and indicates significant vulnerabilities.3 Key risks include increasing exposure to infectious diseases, exacerbated water and food insecurity, natural disasters, and population displacement, detailed descriptions of which are provided elsewhere.3,4 Populations will be differentially vulnerable to these potential impacts at global to local levels. Those at highest risk include populations with an existing high burden of ill health, who are sensitive to climate-related health risks, and live in nations with limited technological capacity, weak institutions, high levels of poverty, and political inequality.5
Indigenous populations have been identified as a highly vulnerable group within global discourse on climate change because of habitation in regions undergoing rapid change, and the disproportionate burden of morbidity and mortality faced by many groups. Yet our understanding of the human dimensions of climate change for indigenous populations at a global level is limited. Ford et al.,6 for instance, noted how indigenous-focused content has been largely overlooked in assessment reports of the Intergovernmental Panel on Climate Change (IPCC), other major assessments,3,7,8 and in policy discussions surrounding the United Nations Framework Convention on Climate Change (UNFCCC). Where indigenous issues are captured, indigenous ways of understanding and information about climate–society interactions embedded in myths, stories, tradition, and observations have typically been marginalized. This forms part of what Hulme9,10 and Jasanoff11 described as the civic epistemology of global climate change discourse that prioritizes positivist disciplines at the expense of the interpretative, creating knowledge detached from its local context. As a consequence, indigenous peoples are often viewed as powerless victims of climate change, overlooking how social, cultural, and economic conditions determine how climate change is experienced, understood, and responded to, and downplaying the accumulated knowledge and wisdom embodied in traditional knowledge systems that can provide valuable lessons for adaptation. In this way, climate change is constructed as a problem for society as opposed to a problem of society, directing attention away from the underlying root causes of vulnerability.
In contrast to the global framing of climate change discourse for indigenous populations, there is an increasingly rich and diverse body of scholarship examining vulnerability and adaptation to climate change at a local to regional level, with a number of studies focusing on health. Such case study research typically focuses on particular places, peoples, and cultures, but this work can also be used to identify broader trends in understanding.12–14 I systematically reviewed the scientific and gray literature published over the past 2 decades (1990–2010) on indigenous health and climate change to identify and characterize the systemic or systemwide determinants of vulnerability, examine the sufficiency of our knowledge base, and identify priorities for future research and current action. I identified publications through the use of multiple search engines, with inclusion and exclusion criteria designed to capture studies focusing on impacts, adaptation, and vulnerability but excluding mitigation. Full review methodology is profiled in supplementary data (available as a supplement to the online version of this article at http://www.ajph.org). I then used a vulnerability framework to structure the analysis of included publications, where vulnerability was conceptualized as a function of exposure to climate-related health risks, sensitivity to these risks, and adaptive capacity to address, plan for, or manage them15–17 (see supplementary data for the framework and additional analyses of key trends in publications reviewed, available as a supplement to the online version of this article at http://www.ajph.org).
THE STATUS AND LIMITS OF CURRENT UNDERSTANDING
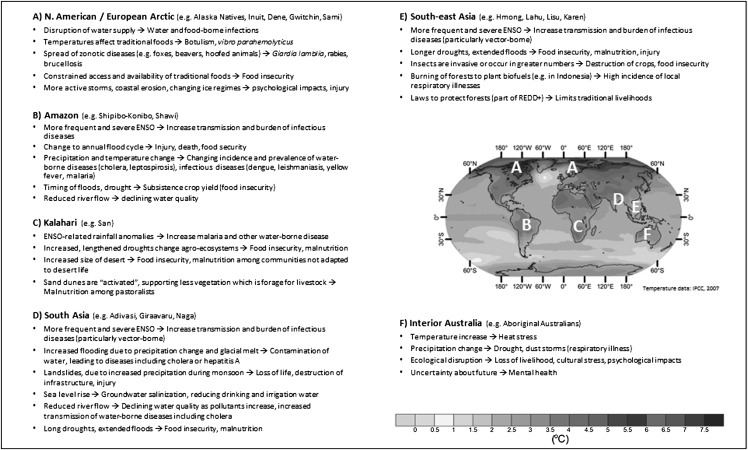
Many indigenous populations face unique exposures and sensitivities to climate change, a function of close relationships with and dependence on land, sea, and natural resources; livelihoods; culture; and habitation in regions that are undergoing rapid climatic and socioeconomic change. These factors create risk profiles that differ significantly from nonindigenous populations, and also among and between indigenous groups (Figure 1).
FIGURE 1—
Map of projected surface temperature increase for 2090 to 2099 based on the A1B scenarios with key health risks for indigenous populations noted.
Note. ENSO = El Niño-Southern Oscillation; IPCC = Intergovernmental Panel on Climate Change; REDD+ = reduce emissions from deforestation and forest degradation.
Source. Solomon et al.18
Unique Sensitivity of Indigenous Populations to Climate Change
Understanding of the specific characteristics of climate change–related exposures and sensitivity is greatest for the Arctic and Australia (see data available as a supplement to the online version of this article at http://www.ajph.org). In the Arctic, many climate-related health outcomes are propagated through traditional food cultures, which have significant importance for many indigenous populations globally. There is strong empirical understanding of these links for Inuit and Alaska Natives, with sea ice change already constraining food access with implications for nutrition and cultural well-being.19–24 Warming temperatures have the potential to affect infectious diseases associated with the storing and preparation of traditional foods (e.g., gastroenteritis, food-borne botulism), zoonotic diseases (e.g., giardiasis),25 and traditional plants or remedies.26 Documented health risks facing Australia’s Aboriginal population with climate change are quite different, associated with occupation in high-risk areas where we have a baseline understanding of how the climate is changing.27,28 Studies have typically examined health concerns surrounding extreme events; in particular, cyclones, flooding, and high temperature are prominent concerns.28–31 Other studies have identified sea-level rise and settlement viability, and infectious diseases (e.g., dengue, Murray Valley encephalitis, malaria) as the main risks affecting health.32 Two Australian studies examined the mental health dimensions of climate change,30,33 a topic not examined in other regions yet of key importance given links between access to traditional lands and mental well-being.34,35
Sensitivity to climate-related health outcomes is also determined by the organization and structure of health systems, current burden of ill health, and material conditions and behavioral factors; that is, the social determinants of health. Herein, a number of generalizations across regions and populations can be derived from existing scholarship.
First, traditional approaches to and conceptualizations of health remain central for many indigenous populations, based on an ideological substratum of concepts, notions, and ideas based around interpersonal and environmental relationships, stewardship, life experience and balance, spiritual considerations, family, and oral history.36 The scope for climate change to affect health, therefore, is broader than altering the incidence and prevalence of disease, with potential for a range of indirect impacts, many of which will be associated with sociocultural well-being. “Western” or “allopathic” approaches are also important in contemporary indigenous health systems, and have been credited with increasing life expectancy in many regions through, for example, vaccinations and improved hygiene.37–39 Depending on location and historical relationships with the state, these components of the health system may exhibit a complementary or competitive relationship. Constraints to accessing allopathic health, however, are widely noted across regions, a function of financial, geographic, and cultural barriers including a history (and current experience) of oppression through the medical system for some groups.37,40 These challenges have implications for informing populations about risk avoidance and prevention activities in light of a changing climate.
Second, social and economic disadvantage are evident in continuing and persistent high rates of poverty and burden of ill health for many indigenous populations, and access to education, housing, and employment are typically well below that of nonindigenous populations.38 These conditions increase sensitivity to climate-related health outcomes through a number of pathways, including forcing people to live in suboptimal conditions, engage in dangerous activities, live in areas of high risk, and engage in unhealthy behaviors. For Aboriginal people in Canada and Australia, house overcrowding has been identified as increasing the risk of communicable diseases and favoring transmission of respiratory and gastrointestinal illness—health outcomes that could be affected by projected warming temperatures.27,41–43 Inadequate water infrastructure, common in many remote communities, increases the likelihood of outbreaks of temperature-related waterborne diseases including diarrheal disease and parasitic infections, particularly in low-income nations.22,27,44,45 Among Inuit populations, a high prevalence of food insecurity associated with poverty and high cost of living is expected to increase sensitivity to nutritional deficiency caused by climate change–related stresses on traditional food systems, with women and children identified to be at high risk22,46; similar challenges have been identified for Alaska Native villages,47,48 and among Amazonian communities.49
In poorer regions of the world, although population-specific data are lacking, it is possible to infer significant sensitivity to climate change because of pronounced health inequality among indigenous populations, which experience some of the highest rates of infant mortality, nutritional deficiency, and rates of infectious and parasitic disease globally.38,50 Particularly in frontier zones being affected by rapid resource development, health systems are under significant stress associated with land expropriation, introduction of new diseases, erosion of traditional institutions, marginalization, and exposure to social and political violence.4 In the Amazon, for example, a resurgence of hydrocarbon-related resource development and deforestation is challenging access to and ownership of traditional lands, introducing new diseases, and creating conditions for the spread and reemergence of existing diseases, a number of which have a strong link to temperature and precipitation (e.g., dengue, malaria, leishmaniasis, cholera), with climate projections indicating more favorable future conditions.51–58 For Central Africa’s Batwa population, insufficient resources and a heavy burden of disease are likely to create significant vulnerability to the projected health impacts of climate change.59–62 These challenges are likely to be elevated for Uganda’s Batwa, where eviction from traditional forest lands to high-density fixed settlements with poor sanitation and limited access to water and food has increased exposure and sensitivity to climate-related health risks including malaria and parasitic infections, while violence and discrimination limit access to formal health services.50,63,64 Projections of increased frequency of high-intensity rainfall events could be particularly problematic, with waterborne disease outbreaks (e.g., typhoid, bacillary dysentery, Escherichia coli, and cryptosporidiosis) typically following heavy rainfall events and associated with fecal matter being washed into local water sources.65–67
Significant Adaptive Capacity of Indigenous Populations
The literature indicates that existing sensitivities will result in climate change impacts occurring faster and of greater magnitude for many indigenous populations. Yet indigenous populations may also have significant adaptive capacity. Empirical work, mostly conducted in the Arctic, describes adaptations currently being employed to cope with a rapidly changing environment with a strong focus on food systems and dangers of engaging in harvesting activities. Adaptations are underpinned by traditional knowledge of lands and resources, cultural identity, and strong social and kinship networks, within health systems that combine allopathic and traditional approaches.19–22,24,68 This adaptive capacity is critical for managing the risks of climate change. A number of studies also describe community-based initiatives to raise awareness of climate change impacts and using research to empower communities, and there are examples in the Arctic of the development of surveillance infrastructure for climate-related health outcomes.69 Few studies, however, have examined how non-Arctic groups are responding to the health effects of climate change, and how economic resources, institutions, technology, equity, and information and skills affect this ability.
There is concern expressed in the literature that social, economic, and political transformations—rooted in colonial history, assimilationist policies, and accelerated by globalization—are having implications, many negative, for indigenous populations and their adaptive capacity. Poverty, marginalization, and lack of legal land title are all important contextual factors that affect adaptation and will be key challenges in the future. In Alaska and northern Canada, transformations of identity and community have resulted in loss of control, cultural continuity, and a weakening of traditional knowledge systems and social capital. Notwithstanding these historical conditions, significant progress has been made in developed nations in settling land claims and recognizing indigenous title, national governments have apologized for the colonial practices of history (e.g., Canada, Australia), and devolution of power to indigenous institutions has occurred in some jurisdictions. These developments hold promise for addressing some of the broader determinants of socioeconomic and health inequality that lie at the heart of indigenous vulnerability to climate change.
Poorer nations face more substantial challenges. Particularly in remote regions experiencing significant resource development pressure, indigenous integration into the global economy is occurring often with limited respect for local autonomy, and accompanied by social and political violence. Associated acculturation challenges have been linked to problems of addiction, suicide, and a weakening of social networks and traditional knowledge systems that play an important role in indigenous health systems and contribute to significant adaptive capacity.33 The process of change and how groups experience and respond to outside stresses, however, is dynamic, and one in which indigenous peoples are actively making, remaking, and challenging their circumstances, with varying degrees of success. Inevitably there will be winners and losers, with concern expressed that climate change could exacerbate existing inequalities at community, regional, and national levels.22 In the Peruvian Amazon, for example, Hofmeijer49 describes how socioeconomic changes linked to resource development and improved transportation have enhanced access to regional health centers and monetary resources important for adaptation, but have also undermined traditional knowledge systems. Similarly, working with the Tsiname peoples of the Bolivian Amazon, Reyes-García et al.70 documented increasing access to the market economy leading to a loss of knowledge of folk plant use. The potential health implications of an erosion of traditional knowledge systems in the context of climate change have not been examined outside an Arctic or Australian context, although the loss of response diversity and flexibility embodied in such knowledge systems has relevance for the management, response to, and avoidance of climate-related health risks that are projected to become more problematic in the future.
Gaps in Understanding
Existing scholarship develops a baseline understanding of the characteristics and determinants of vulnerability to the health effects of climate change for indigenous populations in a number of high-income nations, but there are significant geographic disparities. It is estimated that there are approximately 370 million indigenous people globally and at least 5000 distinct groups, with only a small fraction explicitly studied with regard to the health impacts of climate change. We know the least about regions with the largest indigenous populations, including Africa, Asia, and Latin America. It is likely that vulnerability will be high on account of a high burden of ill health, marginalization, and current exposure to climate-related health risks. Population-specific understanding on the nature of vulnerabilities and determinants remains unknown, however, and compromises our ability to safeguard the health of the most vulnerable.71 In particular, adaptation financing provided through the UNFCCC—the United Nations convention that provides a global architecture for responding to climate change—depends upon the identification of urgent and immediate priorities for intervention: information that is generally lacking for indigenous peoples’ health. This deficit is also evident in completed National Adaptation Programs of Action assessments conducted in the least developed countries and funded by the UNFCCC to identify urgent and immediate needs of the poorest nations to adapt to climate change. As of March 2011, 45 of 49 National Adaptation Programs of Action assessments had been submitted, with explicit reference to indigenous populations made in 5 (data available as a supplement to the online version of this article at http://www.ajph.org). In these cases, assessments note the potential for heightened vulnerability among indigenous populations, and identify importance of traditional knowledge for adaptation, but do not focus on health or identify specific concerns or needs for indigenous populations in light of a changing climate.
Although there is a strong bias toward high-income nations in the literature, there are also widespread disparities within and between these nations. In Canada, only 2 indigenous populations are studied, there is no reporting from Scandinavia or Russia, and only 1 paper reports from the conterminous United States. Disparities are also reflected in the nature of studies conducted, with the majority of empirical and adaptation research taking place in the Arctic and reflective of strong climate change signal evident in this region. Few studies have focused on differential vulnerability at a community level or examined high-risk groups (e.g., elderly, children) and research has largely been conducted in remote regions where indigenous peoples are often disadvantaged greatest but where links to traditional livelihoods and activities are strongest.
A ROADMAP FOR FUTURE RESEARCH AND ACTION
There is an emerging scholarship focusing on indigenous health and climate change, but there is a lot that we do not know. This deficit in understanding is not commensurate with the risks posed by climate change to indigenous health. Insights for indigenous populations can be derived from regional and global studies focusing on nonindigenous populations, but generalizing is problematic for indigenous groups where scholarship indicates that impacts, adaptation, and vulnerability are highly place- and culture-specific, and mediated by worldviews that place significant value on interpersonal and environmental relationships, stewardship, life experience and balance, spiritual considerations, family, tradition, and oral history.6 I outline a roadmap to guide future research and identify how decision makers at various levels can use existing knowledge.
A Global Workplan
Addressing the indigenous health deficit requires a global workplan that develops a sustained process to mobilize resources for research and combines leadership by national and international bodies. Without such a workplan, indigenous health in a changing climate will continue to be neglected. Although the World Health Organization and United Nations Permanent Forum on Indigenous Peoples have noted the special needs of indigenous populations, and a number of initiatives have brought together indigenous peoples and organizations to assert their rights in a changing climate,72,73 the importance and need for studies on indigenous health and climate change is not currently reflected in research agendas articulated in the scientific literature or through international bodies.
From a research and policy standpoint, we need to know how global processes interact with local conditions to create vulnerable (or adaptable) populations in light of a rapidly changing climate, where indigenous people are at greatest risk, what characteristics of a population make them vulnerable or adaptable, and what health risks are most pressing. For those regions and populations where the research need is particularly acute, there is an opportunity to build upon existing information on indigenous livelihoods and the determinants of health to identify and characterize the broad-scale factors likely to affect vulnerability to climate change. Such review-based studies are useful for locating populations or regions where targeted research is required and identifying broader structural conditions that will shape vulnerability,14,41,74,75 and offer a low-cost, rapid entry point for initial research. How these broader factors affect vulnerability at lower scales, however, will not be uniform, depending on location-specific socioeconomic and biophysical factors, and varying at a regional, community, and intracommunity level. This diversity in how climate change will play out locally reinforces the importance of place-based and population-specific studies.12,22,41,76
In identifying research priorities, it is important to begin discussions with indigenous peoples and their organizations, with priorities likely to differ by region and population. The following are key components of a roadmap for future research:
Indigenous conceptualizations on and approaches to health need to be articulated and central to research if we are to focus on relevant health risks and capture the complex, culturally mediated interaction among social, biophysical, and biomedical determinants of vulnerability. In working with communities, it is imperative to recognize the broader structural and colonial factors shaping vulnerability, alternative worldviews, and group-specific conceptualization of health and healthy living. Failure to do so will limit our understanding of vulnerability and likely reduce the effectiveness of policy intervention.10,11,77,78
The collection of baseline data on socioeconomic and biomedical determinants of vulnerability is important. For indigenous populations, we know very little about the incidence and prevalence of most infectious diseases, waterborne illnesses, and food and water insecurity.37,50,79 There is a need to develop an understanding of the sensitivity of health outcomes to climate, including the identification of indicators to measure and monitor, drawing upon both traditional and scientific knowledge.22,80 Data on the social determinants of health are often lacking, including demographics, governance, resource availability, infrastructure, and a host of other factors that influence vulnerability.
There is a need to develop and improve surveillance and environmental monitoring systems (e.g., climate data, vector distributions) that systematically collect information on health outcomes and determinants relevant to indigenous populations and that are necessary to determine the occurrence and spread of health risks.81 Existing surveillance systems provide some coverage, particularly in developed nations, although limitations have been highlighted. New research initiatives should work with indigenous populations to collect information on climate-related health outcomes using this information for future modeling in light of projected climatic conditions where feasible, and also tap the considerable knowledge indigenous populations have in this regard. Building capacity at a local level to support surveillance activity and integrate local needs is essential.22
It is imperative that studies combine fundamental scientific research with an evaluation of opportunities for policy intervention. Proven interventions exist for many climate-related health risks and traditional approaches to health offer a foundation for promoting health and well-being. With recognition of this, a comprehensive evaluation of adaptation needs to examine the effectiveness, desirability, and feasibility of adaptations; assess urgency; evaluate durability of adaptations under different climate and socioeconomic scenarios; and assess equity considerations82,83 working closely with indigenous peoples to this end.
Interdisciplinary approaches to research are required, involving collaborations across the health, natural, and social sciences, and the active engagement of indigenous communities and organizations, health professionals, and policymakers in cooperatively planning, developing, and conducting research. In particular, the humanities and interpretative social sciences have an essential role to play alongside biomedical science in examining the risks posed by climate change to health, and for too long have been neglected in mainstream health and climate change research.10 Thus, indigenous myths and stories, oral tradition, and observations hold valuable information about climate–society interactions, climate-related health risks, and current and future vulnerability and adaptation determinants.6,18,24,43
Many of these research needs have been articulated in the general health and climate change scholarship, and at a global level are captured in the World Health Organization’s Climate Change and Health Work Plan.84 They are even more pertinent in an indigenous context, and offer a means of generating important baseline information on current health risks alongside potential vulnerabilities to climate change.
What We Can Do With Existing Knowledge
This roadmap for future research recognizes that our current understanding is insufficient and likely to constrain adaptation. Yet this should not be used to justify inaction, and a number of emerging themes from this analysis identify potential entry points for health adaptation. Changing traditional knowledge systems, for example, have been identified as a key driver increasing vulnerability to climate-related health risks in numerous contexts. Efforts to preserve, document, and promote and teach traditional knowledge among younger generations, and strengthen links to traditional activities, offer key adaptation interventions. Addressing socioeconomic and health inequalities between indigenous and nonindigenous populations, securing land tenure, confronting colonial history and current reality, and community empowerment are consistently identified as essential for addressing existing health challenges, which in turn will increase resilience to climate change. These examples of entry points have widespread relevance and, though important for adaptation, also concern ongoing policy initiatives and needs in areas of social, cultural, economic, and health development. Climate change provides additional rationale for these interventions, and is consistent with scholarship that has argued that “mainstreaming” or “normalization” of adaptation is likely to be the most effective means of reducing vulnerability.85–88
A CRITICAL TIME
The international policy architecture for addressing climate change through the UNFCCC is at a critical juncture as signatories debate what will replace the Kyoto Protocol when its implementation period ends in 2012. Reducing greenhouse gas emissions is essential if we are to avoid “runaway” climate change and the crossing of key climate system thresholds.1,3,89 The health impacts of such change would be significant and for some indigenous populations would inevitably result in the loss of homeland, livelihoods, and culture. Adaptation will also be necessary given that we are most likely locked into at least 2 °C of warming globally this century,1,90 with climate change already affecting indigenous health. As part of the Copenhagen (2009) and Cancun (2010) Conference of the Parties meetings to the UNFCCC, industrialized nations pledged to provide $100 billion per year by 2020 to help poorer nations adapt, with an interim target of $30 billion by 2012. Whether the promised funds will materialize, or be additional to overseas development assistance, remains to be seen,91,92 but, regardless, adaptation is increasingly being viewed as a cornerstone of climate policy at international to local levels. For indigenous populations, adaptation offers an opportunity to strengthen livelihoods, culture, and health in the face of multiple stresses, and to (re)assert (inter)nationally recognized “special rights.” To seize this opportunity, however, requires significant effort by indigenous organizations and leaders, political actors, nongovernmental organizations, and the scientific community, to identify and justify what adaptations and support are needed. Public health research—working closely with indigenous populations and organizations—has an important role herein, providing an evidence base of the risks posed by climate change, and determinants of vulnerability and adaptability, and needs a more prominent role in future research activities.
Acknowledgments
This work was carried out with support from the International Development Research Centre, the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada, the Social Sciences and Humanities Research Council of Canada, and ArcticNet.
Thanks to Lea Berrang-Ford, K. C. Bolton, and Michelle Maillet who helped put together the article, along with colleagues on the Indigenous Health Adaptation to Climate Change project (http://www.ihacc.ca). Five reviewers provided detailed and constructive comments.
Human Participant Protection
Institutional review board approval was not needed because no human participants were involved.
References
- 1.New M, Liverman D, Schroder H, Anderson K. Four degrees and beyond: the potential for a global temperature increase of four degrees and its implications introduction. Philos Trans Royal Soc A Math Phys Eng Sci. 2011;369(1934):6–19 [DOI] [PubMed] [Google Scholar]
- 2.Fussel HM. An updated assessment of the risks from climate change based on research published since the IPCC Fourth Assessment Report. Clim Change. 2009;97(3-4):469–482 [Google Scholar]
- 3.Costello A, Abbas M, Allen Aet al. Managing the health effects of climate change. Lancet. 2009;373(9676):1693–1733 [DOI] [PubMed] [Google Scholar]
- 4.Myers SS, Patz JA. Emerging threats to human health from global environmental change. Annu Rev Environ Resour. 2009;34:223–252 [Google Scholar]
- 5.Walpole SC, Rasanathan K, Campbell-Lendrum D. Natural and unnatural synergies: climate change policy and health equity. Bull World Health Organ. 2009;87(10):799–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ford JD, Vanderbilt W, Berrang-Ford L. Authorship in IPCC AR5 and its implications for content: climate change and indigenous populations in WGII. Clim Change. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stern N. Stern Review on the Economics of Climate Change. London, England: HM Treasury; 2006 [Google Scholar]
- 8.World Development Report—Development and Climate Change. Washington, DC: World Bank; 2010 [Google Scholar]
- 9.Hulme M. Problems with making and governing global kinds of knowledge. Global Environ Change Hum Policy Dimens. 2010;20(4):558–564 [Google Scholar]
- 10.Hulme M. Meet the humanities. Nat Clim Change. 2011;1(4):177–179 [Google Scholar]
- 11.Jasanoff S. A new climate for society. Theory Cult Soc. 2010;27(2-3):233–253 [Google Scholar]
- 12.Ford JD, Keskitalo ECH, Smith Tet al. Case study and analogue methodologies in climate change vulnerability research. WIREs Clim Change. 2010;1(3). [Google Scholar]
- 13.Ford JD, Pearce T. What we know, do not know, and need to know about climate change vulnerability in the western Canadian Arctic: a systematic literature review. Environ Res Lett. 2010;5(1):1–9 [Google Scholar]
- 14.Turner BL, II, Kasperson RE, Matson PAet al. A framework for vulnerability analysis in sustainability science. Proc Natl Acad Sci U S A. 2003;100(14):8074–8079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smit B, Wandel J. Adaptation, adaptive capacity, and vulnerability. Glob Environ Change. 2006;16:282–292 [Google Scholar]
- 16.Ebi KL, Kovats SR, Menne B. An approach for assessing human health vulnerability and public health interventions to adapt to climate change. Environ Health Perspect. 2006;114(12):1930–1934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford JD, Smit B. A framework for assessing the vulnerability of communities in the Canadian Arctic to risks associated with climate change. Arctic. 2004;57(4):389–400 [Google Scholar]
- 18.Solomon S, Qin D, Manning, Met al. Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, England: Cambridge University Press; 2007 [Google Scholar]
- 19.Beaumier MC, Ford JD. Food insecurity among Inuit females exacerbated by socio-economic stresses and climate change. Can J Public Health. 2010;101(3):196–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford JD. Vulnerability of Inuit food systems to food insecurity as a consequence of climate change: a case study from Igloolik, Nunavut. Reg Environ Change. 2009;9(2):83–100 [Google Scholar]
- 21.Ford JD, Beaumier M. Feeding the family during times of stress: experience and determinants of food insecurity in an Inuit community. Geogr J. 2011;177(1):44–61 [DOI] [PubMed] [Google Scholar]
- 22.Furgal C, Seguin J. Climate change, health and community adaptive capacity: lessons from the Canadian north. Environ Health Perspect. 2006;114(12):1964–1970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldhar C, Ford J, Berrang-Ford L. Prevalence of food insecurity in a Greenlandic community and the importance of socio-economic-environmental stressors. Int J Circumpolar Health. 2010;69(3):285–303 [DOI] [PubMed] [Google Scholar]
- 24.Ford JD, Smit B, Wandel J. Vulnerability to climate change in the Arctic: a case study from Arctic Bay, Canada. Glob Environ Change. 2006;16(2):145–160 [Google Scholar]
- 25.Parkinson AJ, Evengard B. Climate change, its impact on human health in the Arctic and the public health response to threats of emerging infectious diseases. Glob Health Action. 2009:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kellogg J, Wang JZ, Flint Cet al. Alaskan wild berry resources and human health under the cloud of climate change. J Agric Food Chem. 2010;58(7):3884–3900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green D. Climate Change and Health: Impacts on Remote Indigenous Communities in Northern Australia. 2008. Available at: http://www.garnautreview.org.au/ca25734e0016a131/WebObj/03-CIndigenous/$File/03-C%20Indigenous.pdf. Accessed April 19, 2012 [Google Scholar]
- 28.Green D, Alexander L, McLnnes K, Church J, Nicholls N, White N. An assessment of climate change impacts and adaptation for the Torres Strait Islands, Australia. Clim Change. 2010;102(3-4):405–433 [Google Scholar]
- 29.Green D, Billy J, Tapim A. Indigenous Australians’ knowledge of weather and climate. Clim Change. 2010;100(2):337–354 [Google Scholar]
- 30.Hunter E. “Radical hope” and rain: climate change and the mental health of indigenous residents of northern Australia. Australas Psychiatry. 2009;17(6):445–452 [DOI] [PubMed] [Google Scholar]
- 31.Cook GD, Woodward E. Climate Change and Indigenous Communities of the Kakadu Region. Darwin, Australia: Department of the Environment, Waterm Heritage and the Arts; 2008. Internal report 567 [Google Scholar]
- 32.Johnston FH, Bailie RS, Pilotto LS, Hanigan IC. Ambient biomass smoke and cardio-respiratory hospital admissions in Darwin, Australia. BMC Public Health. 2007;7:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berry HL, Butler JRA, Burgess Pet al. Mind, body, spirit: co-benefits for mental health from climate change adaptation and caring for country in remote Aboriginal Australian communities. N S W Public Health Bull. 2010;21(5-6):139–145 [DOI] [PubMed] [Google Scholar]
- 34.Cunsolo-Willox A, Harper S, Landman K, Houle K, Ford J, Rigolet Inuit Community Government. “The land enriches our soul”: on environmental change, affect, and emotional health and well-being in Nunatsiavut, Canada. Emotion Space Society. In press [Google Scholar]
- 35.Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. 2010;55(2):123–132 [DOI] [PubMed] [Google Scholar]
- 36.Pedersen D, Baruffati V. Healers, deities, saints and doctors—elements for the analysis of medical systems. Soc Sci Med. 1989;29(4):487–496 [DOI] [PubMed] [Google Scholar]
- 37.Montenegro RA, Stephens C. Indigenous health 2—indigenous health in Latin America and the Caribbean. Lancet. 2006;367(9525):1859–1869 [DOI] [PubMed] [Google Scholar]
- 38.Stephens C, Porter J, Nettleton C, Willis R. Indigenous health 4—disappearing, displaced, and undervalued: a call to action for indigenous health worldwide. Lancet. 2006;367(9527):2019–2028 [DOI] [PubMed] [Google Scholar]
- 39.Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet. 2009;374(9683):65–75 [DOI] [PubMed] [Google Scholar]
- 40.Macchi M. Indigenous and Traditional Peoples and Climate Change: Issues Paper. Gland, Switzerland: International Union for Conservation of Nature; 2008 [Google Scholar]
- 41.Ford JD, Berrang-Ford L, King M, Furgal C. Vulnerability of Aboriginal health systems in Canada to climate change. Global Environ Change Hum Policy Dimens. 2010;20(4):668–680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Green D. Climate Change and Health: Impacts on Remote Indigenous Communities in Northern Australia. Aspendale, Victoria, Australia: Commonwealth Scientific and Industrial Research Organisation; 2006 [Google Scholar]
- 43.Green D, Jackson S, Morrison J. Risks from Climate Change to Indigenous Communities in the Tropical North of Australia. Canberra, Australia: Department of Climate Change and Energy Efficiency; 2009 [Google Scholar]
- 44.Parkinson AJ, Butler JC. Potential impacts of climate change on infectious diseases in the Arctic. Int J Circumpolar Health. 2005;64(5):478–486 [DOI] [PubMed] [Google Scholar]
- 45.Harper SL, Edge V, Wallace C, Berke O, McEwen S. Comparison of trends in weather, water quality, and infectious gastrointestinal illness in two Inuit communities in Nunatsiavut, Canada: potential implications for climate change. EcoHealth. 2011;8(1):93–108 [DOI] [PubMed] [Google Scholar]
- 46.Richmond CAM, Ross NA. Social support, material circumstance and health behaviour: influences on health in First Nation and Inuit Communities of Canada. Soc Sci Med. 2008;67(9):1423–1433 [DOI] [PubMed] [Google Scholar]
- 47.Loring PA, Gerlach SC. Food, culture, and human health in Alaska: an integrative health approach to food security. Environ Sci Policy. 2009;12(4):466–478 [Google Scholar]
- 48.White DM, Gerlach SC, Loring P, Tidwell AC, Chambers MC. Food and water security in a changing arctic climate. Environ Res Lett. 2007;2(4). [Google Scholar]
- 49.Hofmeijer I. “The Lakes Are Crying and the Fish Are Scarce”: Community Identified Climate Change and Health Priorities in Panaillo—A Report Supporting the Development of the IHACC Research Program. Montreal, Quebec: Department of Geography, McGill University; 2010 [Google Scholar]
- 50.Ohenjo N, Willis R, Jackson D, Nettleton C, Good K, Mugarura B. Indigenous health 3—health of indigenous people in Africa. Lancet. 2006;367(9526):1937–1946 [DOI] [PubMed] [Google Scholar]
- 51.Finer M, Orta-Martinez M. A second hydrocarbon boom threatens the Peruvian Amazon: trends, projections, and policy implications. Environ Res Lett. 2010;5(1). [Google Scholar]
- 52.Maheu-Giroux M, Casapia M, Soto-Calle VEet al. Risk of malaria transmission from fish ponds in the Peruvian Amazon. Acta Trop. 2010;115(1-2):112–118 [DOI] [PubMed] [Google Scholar]
- 53.Githeko AK, Woodward A. International consensus on the science of climate and health: the IPCC Third Assessment Report. : McMichael A, Haines A, Slooff R, Kovats S, Franco E, Climate Change and Human Health. Geneva, Switzerland: World Health Organization; 2003:43–57 [Google Scholar]
- 54.Miranda J, Cabezas C, Maguiña C, Valdivia J. [Hypothermia during the phenomenon of El Niño, 1997–1998.] Rev Peru Med Exp Salud Publica. 2003;20:200–205 [Google Scholar]
- 55.Bravo W, Bravo F. [The effect of the phenomenon of El Niño in dermatological diseases.] Folia Dermatol Peru. 2001;12:29–36 [Google Scholar]
- 56.Checkley W, Epstein LD, Gilman RHet al. Effects of EI Niño and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet. 2000;355(9202):442–450 [DOI] [PubMed] [Google Scholar]
- 57.Chamberlin J, Laughlin L, Romero Set al. Epidemiology of endemic Bartonella bacilliformis: a prospective cohort study in a Peruvian mountain valley community. J Infect Dis. 2002;186(7):983–990 [DOI] [PubMed] [Google Scholar]
- 58.Fraser BJ. Climate change impacts revealed: disease in Peru. Sci Am. 2009;186:983–990 [Google Scholar]
- 59.Wandiga SO, Opondo M, Olago Det al. Vulnerability to epidemic malaria in the highlands of Lake Victoria basin: the role of climate change/variability, hydrology and socio-economic factors. Clim Change. 2010;99(3-4):473–497 [Google Scholar]
- 60.Orlove B, Roncoli C, Kabugo M, Majugu A. Indigenous climate knowledge in southern Uganda: the multiple components of a dynamic regional system. Clim Change. 2010;100(2):243–265 [Google Scholar]
- 61.Apuuli B, Wright J, Elias C, Burton I. Reconciling national and global priorities in adaptation to climate change: with an illustration from Uganda. Environ Monit Assess. 2000;61:145–159 [Google Scholar]
- 62.Uganda National Adaptation Programmes of Action Climate Change. Kampala, Uganda: Government of Uganda and United Nations Environment Program; 2007 [Google Scholar]
- 63.World Directory of Minorities and Indigenous Peoples—Uganda: Batwa. Kampala, Uganda: Minority Rights Group International; 2008 [Google Scholar]
- 64.Namara A. GEF Case Study of Creation and Implementation of National Parks and of Support to Batwa on Their Livelihoods, Wellbeing and Use of Forest Products. GEF Impact Evaluation: Global Environment Facility. Kampala, Uganda: United Nations Development Programme; 2007 [Google Scholar]
- 65.Gasana J, Morin J, Ndikuyeze A, Kamoso P. Impact of water supply and sanitation on diarrheal morbidity among young children in the socioeconomic and cultural context of Rwanda (Africa). Environ Res. 2002;90(2):76–88 [DOI] [PubMed] [Google Scholar]
- 66.Morse TD, Nichols RAB, Grimason AM, Campbell BM, Tembo KC, Smith HV. Incidence of cryptosporidiosis species in paediatric patients in Malawi. Epidemiol Infect. 2007;135(8):1307–1315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dingle K. “Our Health Needs a Healthy Environment”: Community Identified Climate Change and Health Priorities Among the Batwa of Uganda—A Report Supporting the Development of the IHACC Research Program. Montreal, Quebec: Department of Geography, McGill University; 2010 [Google Scholar]
- 68.Wesche SD, Chan HM. Adapting to the impacts of climate change on food security among Inuit in the Western Canadian Arctic. EcoHealth. 2010;7(3):361–373 [DOI] [PubMed] [Google Scholar]
- 69.Parkinson AJ, Bruce MG, Zulz T. International Circumpolar International Surveillance, an Arctic network for surveillance of infectious diseases. Emerg Infect Dis. 2008;14(1):18–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Reyes-García V, Vadez V, Byron Eet al. Market economy and the loss of folk knowledge of plant uses: estimates from the Tsimane’ of the Bolivian Amazon. Curr Anthropol. 2005;46(4):651–656 [Google Scholar]
- 71.Protecting Health From Climate Change. Geneva, Switzerland: World Health Organization; 2008 [Google Scholar]
- 72.United Nations University Indigenous peoples, marginalized populations and climate change. 2011. Available from: http://www.unutki.org/default.php?doc_id=187. Accessed March 1, 2011
- 73.Ford JD, Smith T, Berrang-Ford L. Canadian federal support for climate change and health research compared with the risks posed. Am J Public Health. 2011;101(5):814–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Adger WN. Vulnerability. Glob Environ Change. 2006;16:268–281 [Google Scholar]
- 75.Few R. Health and climatic hazards: framing social research on vulnerability, response and adaptation. Glob Environmen Change Hum Policy Dimens. 2007;17(2):281–295 [Google Scholar]
- 76.Hess JJ, Malilay JN, Parkinson AJ. Climate change. The importance of place. Am J Prev Med. 2008;35(5):468–478 [DOI] [PubMed] [Google Scholar]
- 77.Radcliffe SA, Watson EE, Simmons I, Fernandez-Armesto F, Sluyter A. Environmentalist thinking and/in geography. Prog Hum Geogr. 2010;34(1):98–116 [Google Scholar]
- 78.Cameron ES. Securing indigenous politics: a critique of the vulnerability and adaptation approach to the human dimensions of climate change in the Canadian Arctic. Glob Environ Change. In press [Google Scholar]
- 79.Smylie J, Anderson I, Ratima M, Crengle S, Anderson M. Indigenous health performance measurement systems in Canada, Australia, and New Zealand. Lancet. 2006;367(9527):2029–2031 [DOI] [PubMed] [Google Scholar]
- 80.St Louis ME, Hess JJ. Climate change impacts on and implications for global health. Am J Prev Med. 2008;35(5):527–538 [DOI] [PubMed] [Google Scholar]
- 81.Campbell-Lendrum D, Corvalan C, Neira M. Global climate change: implications for international public health policy. Bull World Health Organ. 2007;85(3):235–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ebi KL, Semenza JC. Community-based adaptation to the health impacts of climate change. Am J Prev Med. 2008;35(5):501–507 [DOI] [PubMed] [Google Scholar]
- 83.Füssel HM. Assessing adaptation to the health risks of climate change: what guidance can existing frameworks provide? Int J Environ Health Res. 2008;18(1):37–63 [DOI] [PubMed] [Google Scholar]
- 84. Climate Change and Health: Report by the Secretariat. World Health Organization, 2009. Report no. A62/11.
- 85.Dovers S. Normalizing adaptation. Glob Environ Change. 2009;19(1):4–6 [Google Scholar]
- 86.Huq S, Reid H, Konate M, Rahman A, Sokona Y, Crick F. Mainstreaming adaptation to climate change in least developed countries (LDCs). Clim Policy. 2004;4(1):25–43 [Google Scholar]
- 87.Klein RTJ, Ericksen SEH, Naess LOet al. Portfolio screening to support the mainstreaming of adaptation to climate change into development assistance. Norwich, UK: Tyndall Centre; 2007. Working paper 102 [Google Scholar]
- 88.Ebi KL, Burton I. Identifying practical adaptation options: an approach to address climate change-related health risks. Environ Sci Policy. 2008;11(4):359–369 [Google Scholar]
- 89.Rockström J, Steffen W, Noone Ket al. A safe operating space for humanity. Nature. 2009;461(7263):472–475 [DOI] [PubMed] [Google Scholar]
- 90.Rogelj J, Chen C, Nabel Jet al. Analysis of the Copenhagen Accord pledges and its global climatic impacts—a snapshot of dissonant ambitions. Environ Res Lett. 2010;5(3). [Google Scholar]
- 91.Hulme M. Will foreign-aid pledges materialize? Nature. 2011;469(7330):299. [DOI] [PubMed] [Google Scholar]
- 92.Donner SD, Kandlikar M, Zerriffi H. Preparing to manage climate change financing. Science. 2011;334(6058):908–909 [DOI] [PubMed] [Google Scholar]