Abstract
Objectives. We explored the benefits of using community health worker (CHW) encounter forms to collect data on patient interactions and assessed the effectiveness of these forms in guiding and directing interactions.
Methods. A 1-page standardized encounter form was developed to document topics discussed during visits with diabetes patients. A portion of the form was designed to be used as a script to guide the interaction and assist patients in setting appropriate self-management goals. Data were also collected via CHW work logs and interviews with CHWs and their supervisors to validate findings.
Results. Data were collected for 1198 interactions with 540 patients at 6 community health centers. Self-management goals were set during 62% of encounters. With respect to the most recent self-management goal set, patients who had set a challenging goal were more likely to be in the action stage of change than in other stages. Work logs revealed that CHWs engaged in a number of activities not involving direct patient interactions and thus not captured on encounter forms.
Conclusions. Evaluating and monitoring CHWs’ daily activities has been challenging. Encounter forms have great potential for documenting the work of CHWs with patients.
Community health workers (CHWs) have gained prominence in health care delivery, supporting strategies that recognize the influence of an individual’s community and environment on health outcomes.1 CHWs have proliferated in racial/ethnic minority communities, frequently serving as liaisons between individuals and the health care system.
Many organizations, including the Institute of Medicine, the Centers for Disease Control and Prevention, the American Public Health Association, and the American Association of Diabetes Educators, have acknowledged the contributions of CHWs, particularly as a resource for increasing access to care for vulnerable individuals, and recommend including CHWs as important members of health care teams.2–5 Recent reviews6–8 have demonstrated the impact of CHWs on the delivery of necessary services, including provision of culturally relevant health education, case management, system navigation, and case finding.
Despite these promising developments, evaluating and monitoring CHWs’ daily activities has been challenging. In only a few studies9–11 have CHWs been used to collect data for research and evaluation. These studies have focused on patients’ characteristics and preferences or barriers to receiving care rather than on activities of CHWs and their work with patients.
Davis et al.12 used CHW logs to periodically document services provided to patients living with diabetes in addition to conducting semistructured interviews with a subset of patients receiving those services. This approach was useful in identifying ways in which CHWs assisted patients. Although logs were successful in providing a snapshot of CHWs’ activities, they were not designed to monitor daily activities, provide information for ongoing supervision, or guide interactions between CHWs and patients.12 Recommendations from the CHW literature often include the need for collecting consistent data regarding activities and interactions with patients.13
During the second year of a Massachusetts statewide diabetes health disparities collaborative with support from the Robert Wood Johnson Foundation’s Finding Answers program, we randomly selected 6 of 12 participating community health centers (CHCs) to be assigned specially trained CHWs. We added CHWs to the CHCs’ health care teams to assist patients with self-management goal setting, one of the 6 components of the chronic care model.14,15 CHWs were assigned a population of patients with type 2 diabetes who had been working with a “provider champion” and his or her team for the duration of the collaborative.
We used a diabetes self-management CHW certificate course developed in collaboration with the Central Massachusetts Area Health Education Center Outreach Worker Training Institute to train CHWs. The curriculum for this training was designed to prepare individuals in basic CHW skills, with a focus on supporting patients with diabetes; CHWs were also provided training on assessing patients’ readiness to change their self-care behaviors and facilitating self-management goal setting. In addition, 1-hour conference calls were scheduled every 6 weeks to provide feedback regarding encounter form data, opportunities for networking, and formal presentations on topics of interest identified by either CHWs or their supervisors.
In this study, we explored the effectiveness of using a CHW encounter form to collect data pertaining to patient interactions. We also assessed ways to use these forms to guide and direct interactions.
METHODS
The encounter form was developed for this project by a team of individuals from the University of Massachusetts Medical School, the Massachusetts League of Community Health Centers, and the Outreach Worker Training Institute, a nationally recognized CHW training program. The team included an experienced health services researcher, a physician with experience working in and with CHCs, a research nurse, an experienced CHW, and the director of the Outreach Worker Training Institute.
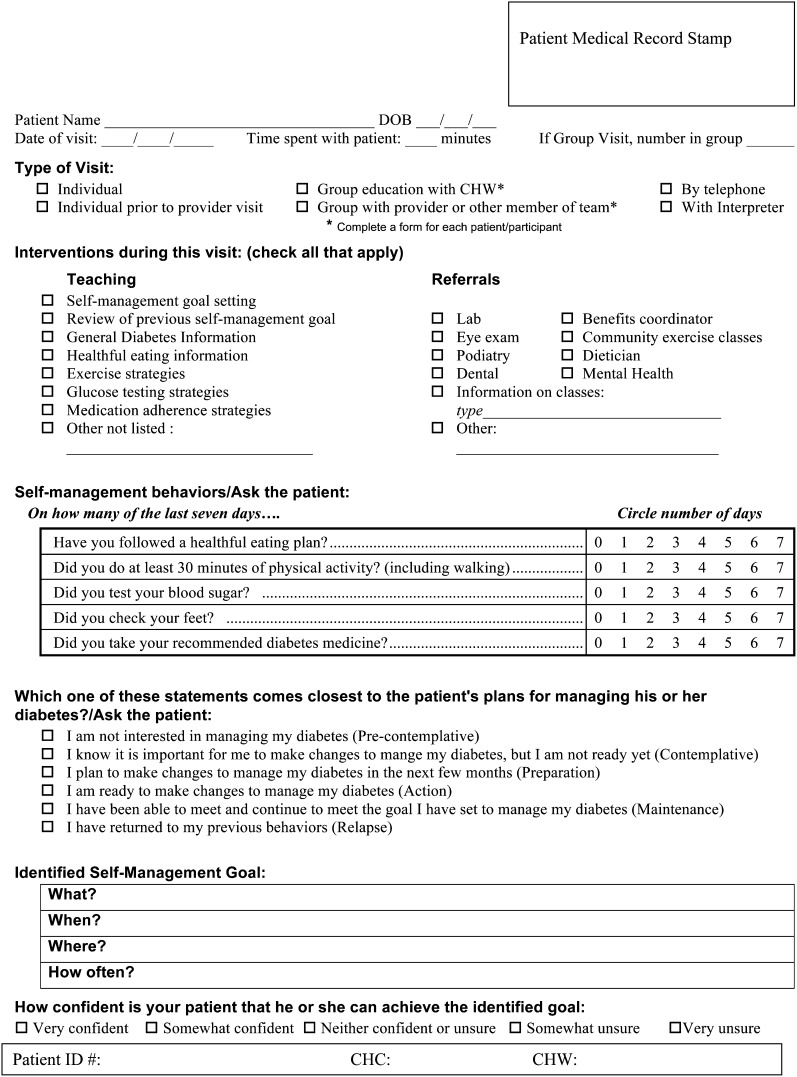
The encounter form was developed as a 1-page standardized interview tool that could be used to document topics discussed during a patient visit and to help guide the interaction. The form included a checklist for teaching activities and referrals, scales to assess patients’ self-care behaviors,16 a patient self-report measure of readiness to change, and a measure of the patient’s perceived ability to accomplish the identified goal (Figure 1). The second half of the form was designed for CHWs to use as a script to guide the interaction and to assist them in helping patients set appropriate, realistic, and achievable self-management goals.
FIGURE 1—
Community health worker encounter form.
We used in-class role-playing activities and at-work practice to pilot test the encounter form with 10 CHWs (all of whom were CHC employees) during their training. Written evaluations were obtained from all CHW trainees. CHWs offered several suggested changes to improve the form, including providing space for patients’ medical record information, simplifying the language defining stages of change, incorporating a confidence scale, and increasing the space available for recording goals.
CHWs received training regarding implementation of the final encounter form. Training included in-class role-playing, class discussions of the importance of using the encounter form for every patient interaction, use of the form as a script with patients, collection of data on patients’ self-care behaviors, and recording of patients’ self-management goals. Finally, as part of the training, CHWs were instructed that interactions should be patient directed and that some interactions might not require the use of all sections of the form.
Work Logs
Encounter forms were used during the intervention to monitor the number of and types of encounters CHWs had with patients. We observed that number of encounters per week decreased after the first quarter of the intervention. To assess comprehensively the activities of CHWs and the fidelity of the intervention, we developed a work log to collect information regarding activities CHWs engaged in that did not involve direct patient interactions. The work logs, which captured activities for a 1-week period of time, included information pertaining to team meetings, chart auditing, and telephone calls to referring agencies. CHWs completed the logs twice during the 13 months of the project intervention.
Additional Follow-Up Interviews
We spoke with CHWs and their direct supervisors 6 weeks and 6 months after the completion of training, either in person or via telephone. We collected feedback regarding consistent use of the encounter form as well as the perceived efficacy of the form.
Theoretical Framework
To facilitate CHWs’ efforts to help patients with stage-based goal setting, we used the transtheoretical model in developing the encounter form. This model, which focuses on individuals’ readiness to change their behaviors,17 comprises 5 stages: precontemplation, contemplation, preparation, action, and maintenance. We also included a sixth stage, relapse, so that we could collect information on patients who had regressed to previous behaviors. To help patients set realistic, achievable goals, we trained CHWs to recognize patients’ stage of change and confidence in achieving their goals. During pilot testing of the encounter form, CHWs requested simpler language defining the stages of change. We created concrete statements to assist CHWs in assessing patients’ stages (Figure 1).
Data Collection and Analyses
CHWs completed encounter forms for each patient interaction during a 13-month time frame (June 1, 2007, to June 30, 2008). We developed a Microsoft Access 2007 (Microsoft Corp, Redmond, WA) database to collect encounter form data. Data were collected and reviewed monthly by the evaluation team, after which they were imported into SPSS version 15 (SPSS Inc, Chicago, IL) for further descriptive analysis. We used frequency distributions to describe interactions, the χ2 test to measure associations between categorical variables, and the t test for continuous outcome measures to compare groups.
We combined reported stages of change into 4 categories excluding relapse: precontemplative/contemplative, preparation, action, and maintenance. We compared the combined stages of change with self-management goals set, dichotomized into less challenging goals and more challenging goals. We defined less challenging goals as keeping appointments, checking blood sugars, checking feet, and taking medications. More challenging goals that required behavioral changes were defined as changing diet, exercising, losing weight, and quitting smoking.
RESULTS
CHWs collected encounter form data for 1198 interactions with 540 patients at 6 CHCs. Forty-nine percent of patients had a single recorded encounter, 24% had 2, 10% had 3, and 17% had 4 or more. Almost half (49%) of these encounters were 15 minutes or less in duration. Most encounters occurred with a patient individually (94%), and encounters were approximately evenly divided between face-to-face (48%) and telephone (52%) encounters (Table 1). Although CHWs had been assigned a population of patients with type 2 diabetes who had been working with the provider champion for the duration of the collaborative, almost 40% of encounters involved patients who had not been assigned to CHWs as part of their population of focus.
TABLE 1—
Descriptive Data Collected in Encounter Forms: Massachusetts, 2007–2008
| Encounters (n = 1198), No. (%) or Mean ±SD | |
| Length of encounter, min | |
| ≤ 15 | 585 (49) |
| 16–30 | 405 (34) |
| 31–60 | 123 (10) |
| > 60 | 85 (7) |
| Type of encounter | |
| Individual: overall | 1128 (94) |
| Individual: in person | 541 (48) |
| Individual: telephone | 587 (52) |
| Group | 70 (6) |
| Type of information provideda | |
| General diabetes information | 469 (39) |
| Healthful eating strategies | 350 (29) |
| Exercise strategies | 245 (21) |
| Glucose testing strategies | 228 (19) |
| Medication adherence strategies | 150 (13) |
| Other, not listed | 485 (41) |
| Type of referral provided | |
| Laboratory or blood work | 175 (15) |
| Eye examination | 98 (8) |
| Podiatry | 65 (5) |
| Dental | 15 (1) |
| Community exercise program | 17 (1) |
| Mental health | 10 (< 1) |
| Information on classes | 7 (< 1) |
| Stage of changeb | 644 (54) |
| Precontemplative | 8 (1) |
| Contemplative | 30 (5) |
| Preparation | 157 (24) |
| Action | 253 (39) |
| Maintenance | 183 (28) |
| Relapse | 13 (2) |
| Type of self-management goalb | 746 (62) |
| Keeping/scheduling appointment | 190 (26) |
| Monitoring blood sugar | 179 (24) |
| Diet | 158 (21) |
| Exercise | 113 (15) |
| Other | 106 (14) |
| Level of confidence in achieving goalb | 659 (55) |
| Very confident | 333 (28) |
| Somewhat confident | 244 (20) |
| Neither confident nor unsure | 69 (6) |
| Somewhat unsure | 10 (1) |
| Very unsure | 3 (< 1) |
| Diabetes self-care activities,c d | |
| Following healthful eating plan | 2.8 ±2.8 |
| With ≥ 30 min exercise | 2.0 ±2.5 |
| Testing blood sugar | 3.0 ±3.2 |
| Checking feet | 2.6 ±3.1 |
| Taking diabetes medication | 3.9 ±3.4 |
Total exceeds 100% because multiple responses could be selected.
Percentages are of total collected
Number of days spent on these activities in the preceding 7 days.
Self-management goals were set during 62% (n = 746) of encounters, with the most common goals related to keeping or scheduling appointments (26%). In encounters in which patients reported their stage of change (n = 644), 39% reported being in the action stage, 28% reported being in the maintenance stage, and 24% reported being in the preparation stage. In encounters in which patients reported their level of confidence in achieving their goal (n = 659), 51% were very confident, 37% were somewhat confident, and 11% were neither confident nor unsure. With respect to the most recent self-management goal set, the 250 patients who had a more challenging goal set at their last encounter were more likely to be in the action stage than in the precontemplative/contemplative, preparation, or maintenance stage (P < .001; Table 2).
TABLE 2—
Patients’ Stage of Change, Type of Self-Management Goal Set, and Level of Confidence in Achieving Goal: Massachusetts, 2007–2008
| Contemplative,a No. (%) | Preparation, No. (%) | Action, No. (%) | Maintenance, No. (%) | |
| Self-management goalb,c | ||||
| More difficult | 4 (31) | 9 (16) | 75 (64) | 31 (50) |
| Less difficult | 9 (69) | 49 (84) | 42 (36) | 31 (50) |
| Total | 13 (100) | 58 (100) | 117 (100) | 62 (100) |
| Level of confidencec,d | ||||
| Confident | 6 (30) | 105 (85) | 205 (94) | 146 (94) |
| Unsure | 14 (70) | 19 (15) | 12 (6) | 10 (6) |
| Total | 20 (100) | 124 (100) | 217 (100) | 156 (100) |
Includes respondents who were in either the precontemplative or contemplative stage.
Most recent reported goal set by patient.
Significant difference among patients at different stages of change (P < .001).
Includes all encounters with a self-management goal set.
When stage of change was compared with a 2-level measure of confidence in goal achievement (very or somewhat confident vs neither confident nor unsure or somewhat or very unsure), patients who were in the action and maintenance stages were more likely to report being confident that they could accomplish their goal than were patients who were in other stages (P < .001; Table 2). No statistical differences were observed when dichotomized self-management goals (less challenging vs more challenging) were compared with dichotomized levels of confidence.
We also compared patients’ reported diabetes self-management behaviors at their most recent visit. Patients reporting that in the preceding 7 days they followed a healthy eating plan every day, did at least 30 minutes of physical activity every day, and took their recommended diabetes medicine every day were more likely to be higher on the stages of change continuum than were patients who did not engage in these behaviors every day (P < .001, P = .05, and P < .001, respectively).
We compared behaviors at the first and last encounters for the 171 patients who had had more than 1 encounter with a CHW and had answered diabetes self-management behavior questions at 2 or more visits (mean interval between encounters = 147 days, SD = 93). One of the 5 self-reported behaviors assessed—foot care—demonstrated a significant preintervention-to-postintervention improvement. Patients reported an increase in the number of days (in the preceding 7 days) on which they had checked their feet (preintervention mean = 3.7, SD = 3.4; postintervention mean = 4.8, SD = 2.9; P = .001). Also, there was a tendency for patients to report an increase in the number of days on which they had tested their blood sugar. However, this increase was not significant at the .05 level (preintervention mean = 4.3, SD = 2.9; postintervention mean = 4.9, SD = 2.7; P = .065).
We found no differences between phone and face-to-face encounters in type of goal set (more difficult or less difficult). Among the 346 patients with self-care activities recorded for at least 1 encounter, those who had an individual face-to-face encounter were more likely than those contacted via phone to report checking their feet often in the preceding 7 days (mean = 4.9 days, SD = 2.8, vs mean = 4.24 days, SD = 3.1; P = .028). There were no differences in other self-care activities.
Work Log
Information from work logs revealed that CHWs engaged in several activities that did not involve direct patient interactions and, as a result, were not captured on encounter forms. The 3 most common activities reported by CHWs were reviewing or updating patients’ medical records, spending time meeting with team members, and making phone calls not involving patients. Infrequent activities not consistently performed across sites included making home visits, researching health information for patients, completing patient mailings, and performing data entry.
Follow-Up Interviews
CHWs and their direct supervisors (n = 6) reported consistent use of the encounter form at interviews conducted 6 weeks and 6 months after completion of training. In addition, 4 of the 6 supervisors noted that the CHC was including the encounter form in patients’ medical records. All CHWs expressed that the encounter form was helpful, with one noting, “I think it is easy to use and helps trigger the appropriate questions to ask.” Another stated that “the questions are very easy to be able to communicate with the patient.” Two CHWs believed that including additional space for visit notes would have been helpful.
DISCUSSION
We believe that this methodology for documenting the content of interactions between CHWs and patients living with a chronic illness offers opportunities to both guide encounters and monitor activities conducted by CHWs. The training provided to the CHWs for this project centered on assessing patients’ readiness to change their behaviors and facilitating patients’ self-management goal setting. This process included a brief assessment of patients’ stage of change and encouragement to them to begin with small goals to foster a sense of accomplishment as well as building motivation to set additional goals.
CHWs were encouraged to have patients focus on making changes that they had some confidence they could achieve. They were able to assist patients in setting self-management goals and promote goals that were consistent with patients’ reported stage of change. It is important to note that the detailed information gleaned from our project would not have been available without use of the encounter form. The literature describing CHW interventions has identified the need to collect consistent data on CHW–patient interactions for evaluation purposes13; the encounter form was successful in providing such information and could be helpful in demonstrating the value of CHWs as members of the health care team.
The encounter form was not only instrumental in collecting data about CHW activities; the form’s structured nature also helped provide direction and cues during interactions, as evidenced by feedback from the participating CHWs. In addition, there was potential for supervisors of CHWs to acquire information for feedback and oversight of activities. We were successful in using the encounter form to monitor the intervention, to provide feedback to both CHWs and their supervisors, and to identify additional training needs during the intervention, conducted via periodic conference calls.
In addition to revealing other activities they were engaged in (which led to the development of the work log), conference calls allowed CHWs to express a need to identify strategies for contacting difficult-to-reach patients, specifically those who did not keep appointments or return phone calls. This feedback from CHWs after reviewing data from their encounters resulted in the development and delivery of additional training sessions with an experienced CHW who worked primarily with homeless substance abusers.
The distribution of stages of change in encounters in which stage of change was recorded (n = 644) revealed that patients in a large percentage of encounters reported being in the action or maintenance stage (68%), with only a few reporting being in the precontemplative or contemplative stage (6%). This finding differs from what has been reported as the “rule of thumb for at-risk populations: 40% in Precontemplation, 40% in Contemplation, and 20% in Preparation.”17(p38)
A possible explanation for this result is that CHCs had been participating in a statewide diabetes health disparities collaborative in the year preceding the deployment of CHWs. During that period, CHCs focused on achieving strategic system change by applying the chronic care model, an evidence-based conceptual framework developed by Wagner et al. that includes self-management as a key construct.15 Participation in this collaborative may have initiated the process of both providers and patients moving toward making changes.
An additional explanation may be that the concrete statements we developed to define stages of change was too restrictive and may not have perfectly captured each individual’s stage. However, patients who were identified as being in the action stage were more likely to set a challenging self-management goal, and patients higher on the stages of change continuum were more likely to report engaging in daily physical activity, healthy eating, and taking their medication, all of which are consistent with the stages of change conceptualized in the transtheoretical model.17
The encounter form has great potential for documenting the work of CHWs with patients, particularly as practices transform into the patient-centered medical home model. According to this model, care should be team based and culturally competent and should include patient empowerment to improve health behaviors, especially in the case of those with chronic illnesses such as diabetes.19 Including data from CHW encounter forms in patients’ medical records could alert providers as to patients’ readiness to change and offer an opportunity to reinforce their change behaviors more efficiently according to their needs and desires.
The encounter form has additional potential to improve the effectiveness of research interventions that include CHWs. Assessments of the fidelity of such interventions are challenging given the range of potential tasks completed by CHWs as part of the health care team, particularly if they are called on to provide services that perhaps are not the focus of the intervention, such as data entry, chart review, language interpretation, or assistance to providers during clinical encounters.
This study, although one of the first to our knowledge in which an encounter form has been used to describe and quantify the work performed by CHWs in the field, involves some limitations. For example, the form was designed specifically for engaging CHWs working with patients living with diabetes. Thus, without major modifications, the form may not be appropriate for use by CHWs engaged primarily in outreach work, patient navigation, or benefit management. However, we do believe that the form could be easily customized for CHWs working with patients experiencing other chronic illnesses, such as HIV, cardiovascular disease, or depression, and would be useful in assisting patients in setting self-management goals.
Because there were no direct observations of CHWs as they met with patients and used the encounter form, we cannot be certain that all activities were recorded accurately. However, it is important to note that CHWs used the forms with a large number of patients who were not in their assigned population of focus, thus indicating the perceived usefulness of the tool. Both CHWs and their supervisors reported consistent use of the form.
In addition, the evaluation team monitored and reviewed encounter form data monthly and was able to quickly address quality concerns. For example, CHWs reported, via a regularly scheduled conference call held every 6 weeks during the intervention, that they frequently estimated the duration of encounters only after they had taken place. Adding a start and end time, particularly in an electronic medical record template, would allow more accurate measurement of encounter durations and work efficiency. This is a potential area for future research.
Telephone encounters between patients and CHWs may be easier to conduct and require less time to complete. We did not conduct a cost–benefit analysis. Our goal was to use a patient-centered approach to supporting behavioral change. However, a face-to-face encounter might have more impact given that CHWs could engage in more extensive teaching (e.g., showing patients how to track blood pressure over time).
Finally, we did not include a comparison group of CHWs not using our encounter form, which would have allowed us to explore differences in the quality of interactions, nor did we collect data from patients to assess their perceptions regarding use of the form. Encounter forms may need to be supplemented with other tools (e.g., work logs) to ensure fidelity to the goals of an intervention. CHWs joined primary care teams that had already been involved in transforming chronic care management practices. Those joining a health care team unfamiliar with CHWs might encounter more difficulty in being accepted as part of the team, leading to lower levels of effectiveness.
In conclusion, our results indicate that CHWs can successfully collect data on their interactions with patients and that these data are useful for evaluation purposes as well as providing needed oversight and supervision of activities. Use of CHW encounter forms could help meet the recognized need for collecting measurable and consistent data regarding CHWs’ roles and interactions with patients,13 as well as assist providers in more efficiently addressing behavior change.
Acknowledgments
Funding for this project was provided by a grant from the Robert Wood Johnson Foundation (Finding Answers: Disparities Research for Change) and by Commonwealth Medicine, University of Massachusetts Medical School.
Human Participant Protection
The institutional review board of the University of Massachusetts Medical School approved the study protocol. Participants provided verbal informed consent.
References
- 1.Fisher EB, Brownson CA, O’Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. Am J Public Health. 2005;95(9):1523–1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Community health workers: critical connections in communities. Available at: http://www.cdc.gov/diabetes/projects/comm.htm. Accessed April 2, 2012
- 4.Recognition and Support for Community Health Workers’ Contributions to Meeting Our Nation’s Health Care Needs. Washington, DC: American Public Health Association; 2002 [Google Scholar]
- 5.American Association of Diabetes Educators Position statement: diabetes community health workers. Diabetes Educ. 2003;29(5):818–824 [DOI] [PubMed] [Google Scholar]
- 6.Norris SL, Chowdhury FM, Van Le Ket al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23(5):544–556 [DOI] [PubMed] [Google Scholar]
- 7.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs. 2002;19(1):11–20 [DOI] [PubMed] [Google Scholar]
- 8.Zuvekas A, Nolan L, Tumaylle C, Griffen L. Impact of community health workers on access, use of services, and patient knowledge and behavior. J Ambul Care Manage. 1999;22(4):33–44 [DOI] [PubMed] [Google Scholar]
- 9.Tomlinson M, Solomon W, Singh Yet al. The use of mobile phones as a data collection tool: a report from a household survey in South Africa. BMC Med Inform Decis Mak. 2009;9:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onwujekwe O, Dike N, Ojukwa Jet al. Consumers stated and revealed preferences for community health workers and other strategies for the provision of timely and appropriate treatment of malaria in southeast Nigeria. Malar J. 2006;5:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kobetz E, Menard J, Barton Bet al. Barriers to breast cancer screening among Haitian immigrant women in Little Haiti, Miami. J Immigr Minor Health. 2010;12(4):520–526 [DOI] [PubMed] [Google Scholar]
- 12.Davis KL, O’Toole ML, Brownson CA, Llanos P, Fisher EB. Teaching how, not what: the contributions of community health workers to diabetes self-management. Diabetes Educ. 2007;33(suppl 6):208S–215S [DOI] [PubMed] [Google Scholar]
- 13.Cherrington A, Ayala GX, Amick H, Scarinci I, Allison J, Corbie-Smith G. Applying the community health worker model to diabetes management: using mixed methods to assess implementation and effectiveness. J Health Care Poor Underserved. 2008;19(4):1044–1059 [DOI] [PubMed] [Google Scholar]
- 14.Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004;13(4):299–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20(6):64–78 [DOI] [PubMed] [Google Scholar]
- 16.Toobert DJ, Hampson SE, Glasgow RE. The Summary of Diabetes Self-Care Activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950 [DOI] [PubMed] [Google Scholar]
- 17.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48 [DOI] [PubMed] [Google Scholar]
- 18.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4 [PubMed] [Google Scholar]
- 19.Rogers J. Assembling patient-centered medical homes—the care principles. Fam Med. 2007;39(10):697–699 [PubMed] [Google Scholar]