Abstract
Objectives. To inform prevention policy, we estimated the economic benefits to health, production, and leisure in the 2008 Australian population of a realistic target reduction in per capita annual adult alcohol consumption.
Methods. We chose a target of 6.4 liters annually per capita on average. We modeled lifetime health benefits as fewer incident cases of alcohol-related disease, deaths, and disability adjusted life years. We estimated production gains with surveyed participation and absenteeism rates. We valued gains with friction cost and human capital methods. We estimated and valued household production and leisure gains from time-use surveys.
Results. A reduction of 3.4 liters of alcohol consumed annually per capita would result in one third fewer incident cases of disease (98 000), deaths (380), working days lost (5 million), days of home-based production lost (54 000), and a A$ 789-million health sector cost reduction. Workforce production had a A$ 427 million gain when we used the friction cost method. By contrast, we estimated a loss of 28 000 leisure days and 1000 additional early retirements.
Conclusions. Economic savings and health benefits from reduced alcohol consumption may be substantial—particularly in the health sector with reduced alcohol-related disease and injury.
Excessive alcohol consumption is a global public health issue.1,2 In Australia, excessive alcohol intake is defined as consuming greater than 75 milliliters of alcohol per day for men and greater than 50 milliliters for women.3 The average consumption of alcohol was 9.8 liters annually in 2005,4 contributing a net 2.3% to the overall health burden,5 trailing behind other modifiable risk factors of tobacco use, high blood pressure, cholesterol, body mass, and physical inactivity. The major avoidable consequences of both short- and long-term harmful alcohol consumption contribute to this burden in the forms of alcohol dependence, suicide and self-inflicted injuries, road traffic accidents, esophageal cancer, and breast cancer.5 Although the consumption of alcohol at moderate levels has also been linked to positive health benefits including the prevention of cardiovascular disease among mature-aged persons,6 the extent of such benefits remains controversial.6,7
Australia has a strong history of alcohol consumption control. This includes 3 main approaches to the issue. First, there is a reliance on regulation introduced over the past decades to restrict sales of alcohol to underage (younger than 18 years) persons, to license alcohol sales outlets, to allow police to conduct random alcohol breath testing of drivers of motor vehicles (legal limit of blood alcohol is 0.05 g/100 mL8) and to restrict multiple forms of advertising of alcohol. Second, taxation of alcoholic products has been adopted to reduce demand. Third, social marketing campaigns (print and visual media) have been used to alert and inform consumers of alcohol about the dangers of driving under the influence of alcohol and binge drinking especially among young adults.9 Together these measures have been used to establish a framework of successful measures to curb the avoidable harms of excessive alcohol consumption in the face of a culture of broad acceptance9 (e.g., random breath testing has been shown to be successful in preventing fatal crashes during certain hours10).
More recently, the National Preventative Health Taskforce in Australia has driven renewed interest in extending regulation and taxation to facilitate further reductions in harmful drinking behavior and reduce the negative health consequences of high-risk alcohol consumption.11 They identified the valuable role of regulation and taxation and recommended a number of measures to increase the preventive effort. This study is timely in that it quantifies the likely benefits of continued alcohol harm prevention on health, production (workforce and household), and leisure.
Modeling has been used in the past to quantify gains arising from general population health improvements12 following complete elimination of risk factor behaviors in Australia, including harmful drinking,13 tobacco smoking,13 and high body mass index (BMI; defined as weight in kilograms divided by the square of height in meters).14 There is, however, no information about the impact of realistic reductions in harmful drinking behaviors in the literature. The consequential impact of improved health on each of paid and unpaid production and leisure has similarly not been estimated.
The current prevalence of long-term harmful alcohol consumption is estimated to be 13% of Australian adults.15 We sought to quantify the potential economic outcomes that could be expected if a realistic reduction in alcohol consumption were achieved (measured in liters of alcohol consumed per capita each year), which is an important consideration in light of the current political and policy interest in Australia and elsewhere. This study was part of a project funded by VicHealth (the Victorian Health Promotion Foundation), completed in 2009, to evaluate the health, economic, and financial benefits of reductions in prevalence of 6 important risk factors (alcohol, physical inactivity, high BMI, tobacco smoking, inadequate consumption of fruit and vegetables, and intimate partner violence). To date, outcomes from the tobacco smoking, six risk factors combined, and physical activity components of the study have been published.16–18 The results of this study could readily be reexamined in other countries by adoption of similar methods, thereby adding to the economic arguments in support of public health prevention efforts.
METHODS
Selection of feasible target reductions in alcohol consumption per capita for Australia was the primary step in this analysis and was not an inconsequential task. We considered current consumption trends, likely future policies and their effectiveness, as well as the experience of other culturally and demographically similar countries. This formed an iterative process over several months, which included an extensive literature review, discussions with a study-specific advisory committee of subject experts, and a review of alcohol control and consumption levels in countries similar to Australia (outlined elsewhere).16 Because there was no agreement upon better guidance in the literature, we used an Arcadian mean to provide a valid prevalence target to model health and economic impact in Australia. The term Arcadian was introduced by Armstrong in his comparative study of age-standardized mortality rates in genetically similar countries in 1990.19 The Organization for Economic Co-operation and Development (OECD) reported that the average number of liters of alcohol consumed per capita each year (in persons aged older than 15 years) in 2005 was 6.4 in Norway, compared with 9.8 in Australia.4 A recent review also ranked Norway highest among OECD countries based on the strength and enforcement of their alcohol control policies.20 Norway was chosen by consensus over Sweden, Canada, and the United States to be the best comparator OECD country as it is a developed country that is culturally and demographically similar to Australia and has a history of government regulation and pricing policies aimed at reducing alcohol consumption.
We modeled economic and health gains on the basis of an absolute change in liters of national annual adult per capita alcohol consumption. We modeled 2 separate levels of realistic reduction targets: an ideal (equivalent to 3.4 L reduction annually per capita) representing what might be achieved based on current prevention knowledge in the medium or long term, and a progressive target reflecting a shorter-term goal set as half of the ideal reduction target (1.7 L per capita). We estimated the net difference in health status and economic costs between the current burden (assumed attributable to 9.8 L consumed4) and the avoidable burden at the targeted lower levels of alcohol consumption. Taking this population-based approach did lead to some reductions in the potential benefits of alcohol consumption, as well as the reductions in harm. By applying a general reduction in the average liters of alcohol consumed across the entire adult population of Australia, we estimated that some people who ordinarily consumed alcohol at moderate or low levels (most notably in older age groups) could become abstainers and would no longer experience the protective benefit of moderate alcohol consumption. Our health status results are hence the net change with consideration of both harm and benefit reductions.
We modeled the likely impact on paid and unpaid production and leisure resulting from the difference in health status (represented by fewer deaths and incident cases of alcohol-related disease) on the basis of differences in surveyed health-related behavior of persons who drank alcohol at long-term high-risk levels compared with persons who did not.
Data Sources
We based the estimate of the prevalence of long-term high-risk alcohol consumption (13%) on 2004–2005 National Health Survey (NHS) data. Respondents estimated their average daily consumption of alcohol during the week before the survey being completed, and high-risk drinking for men was defined as greater than 4 standard drinks per day and for women as greater than 2 standard drinks per day. We applied National Health and Medical Research Council guidelines to define the exposure category (long-term high-risk alcohol consumption) as being greater than 75 milliliters of alcohol consumed per day for men and greater than 50 milliliters of alcohol consumed per day for women.3 The nonexposed category (long-term low-risk alcohol consumption) was defined as 75 milliliters or less of alcohol consumed per day for men and 50 milliliters or less of alcohol consumed per day for women.
We obtained population-attributable risk fractions, health status estimates (incident cases of alcohol-related disease, deaths), and full disability adjusted life years (DALYs) by using the 2003 Australian Burden of Disease data files,5 which were made available to this study. We used the 2000–2001 Disease Costs and Impact Study21 Excel data files to estimate the change in health sector costs. We applied rates of disease and mortality estimates from 2003 to the 2008 population and health sector costs inflated to 2008 prices by using appropriate health price inflators.22
We obtained demographic data, employment status, and health-related actions of adults who consumed alcohol at levels associated with high risk and those who consumed alcohol at levels associated with low risk from the 2004–2005 NHS Confidentialised Unit Record Files (CURF), with the approval of the Australian Statistician, Australian Bureau of Statistics (ABS).15,23 These data are summarized in Table 1. We obtained household production and leisure time activities from the 2006 ABS Time Use Survey.24
TABLE 1—
Demographics of Persons Who Consume Alcohol at Levels Associated With High Risk Versus Low Risk by Gender and Workforce Status: Australia, 2004–2005
| Men |
Women |
|||
| High-Risk Alcohol Consumption | Low-Risk Alcohol Consumption | High-Risk Alcohol Consumption | Low-Risk Alcohol Consumption | |
| Age, y | ||||
| 15–64, no. (95% CI) | 548 967 (504 066, 593 867) | 5 159 965 (5 085 129, 5 234 801) | 215 942 (188 952, 242 931) | 5 412 604 (5 348 433, 5 476 774) |
| ≥ 65, no. (95% CI) | 42 640 (30 065, 55 216) | 1 009 718 (990 008, 1 029 427) | 25 977 (15 428, 36 525) | 1 182 647 (1 159 920, 1 205 374) |
| ≥ 15, mean (95% CI) | 42.6 (41.4, 43.8) | 45.3 (45.1, 45.5) | 43.5 (41.4, 45.6) | 46.1 (45.9, 46.3) |
| In labor force, aged ≥ 15 ya | ||||
| % (95% CI) | 82 (79, 85) | 75 (74, 76) | 69 (63, 75) | 58 (57, 59) |
| Days off work, mean (95% CI) | 0.32 (0.16, 0.48) | 0.31 (0.25, 0.37) | 0.37 (0.18, 0.55) | 0.30 (0.26, 0.35) |
| Not in labor force, aged 15–64 y | ||||
| % (95% CI) | 18 (16, 21) | 25 (24, 26) | 31 (25, 38) | 42 (41, 43) |
| Days of reduced activity, mean (95% CI) | 1.72 (0.75, 2.70) | 1.86 (1.53, 2.20) | 1.59 (0.65, 2.54) | 1.40 (1.24, 1.55) |
| Not in labor force, aged ≥ 65 y | ||||
| % (95% CI) | 7.2 (5.5, 9.5) | 16.4 (16.0, 16.7) | 10.7 (7.1, 15.9) | 17.9 (17.6, 18.3) |
| Days of reduced activity, mean (95% CI) | 0.89 (0.21, 1.57) | 1.22 (0.97, 1.47) | 1.64 (-0.62, 3.89) | 1.52 (1.32, 1.73) |
Note. CI = confidence interval. Mean days measured over a 2-week period.
Source. National Health Survey 2004–2005.15
Includes unemployed seeking work and those aged ≥ 65 years.
Data Analyses
We developed population simulation models in Excel 2003 (Microsoft Corp, Redmond, WA) to determine the potential lifetime benefits of a reduction in per capita alcohol consumption for the 2008 Australian adult cohort (aged ≥ 15 years). The time horizon for economic benefits was the remaining lifetime of the 2008 Australian population cohort and we applied a 3% discount rate for lifetime benefits.25 We varied the discount rate to 0%, 5%, and 7% in sensitivity analyses, which are not reported here, but are available from the authors. Each component of the economic benefits is outlined in the next section.
Workforce production gains model.
We estimated workforce production gains or losses reflecting differences in workforce participation and absenteeism rates associated with high-risk and low-risk alcohol consumption, combined with changes in population health status following a per capita reduction in liters of alcohol consumed. The workforce production gains model follows a theoretical cohort of Australians (aged 15–65 years), accruing the production gains or losses of the expected health benefits of a per capita reduction in alcohol consumption during working years until retirement. We used 2 techniques to measure and value production gains and losses: the friction cost approach (FCA) and, as a separate sensitivity analysis, the human capital approach (HCA). The FCA assumes a disabled or deceased worker will be replaced within 3 to 12 months whereas the HCA assumes the worker will not be replaced, and hence assigns a larger value to a worker leaving the workforce permanently through death or disability. This important difference to how workforce production is valued is still the matter of some controversy in the economics literature.26,27
Household production and leisure time model.
We defined household production as the hours of time spent performing nonpaid household duties such as cooking, shopping, cleaning, child care, and maintenance. We estimated the value of these duties by using the “replacement cost method,” adapted from the accounting discipline, assuming the services would be purchased at current commercial rates when a person in the household was ill. Leisure time comprised social and community interaction together with recreation and leisure activities. We estimated the value of changes in leisure time by using an “opportunity cost” conventional method applying one third of average weekly earnings for men and women for 2008.28
Health sector cost estimation.
To estimate health sector costs, we calculated the portion of total 2008 Australian health sector costs attributable to disease and injury associated with high-risk alcohol consumption, applying the 2000–2001 Disease Costs and Impact Study disease and injury classification system,21 by using population attributable fractions.5 We did not attempt to model lifetime health expenditure costs from these data, because they consisted of expenditure on both incident and prevalent cases of disease and injury. Instead, we maintained a conservative approach assuming annual health sector costs attributed to the diseases associated with long-term high-risk alcohol consumption would approximate the lifetime costs of treating incident cases of disease.
Uncertainty analysis.
We undertook multivariable probabilistic uncertainty analyses by using @RISK software version 4.5 (Palisade Corp, New York, NY) for Excel 2007. We generated estimates of mean, median, and 95% uncertainty interval for each of the economic and financial outcome measures from a minimum 4000 iterations by using data from the known surveyed distribution of input variables to the modeling. Further details are available in the full study report29 and the previous publications arising from this study16-18 on tobacco smoking.
RESULTS
Demographic data and days of reduced activity attributable to ill health are provided in Table 1 for persons who consumed alcohol at levels associated with high risk, compared with persons who consumed alcohol at levels associated with low risk in the 2008 adult Australian population, by gender, age group, and workforce status. Men and women who consumed alcohol at levels associated with high risk were significantly younger and more likely to be employed than were persons who consumed alcohol at levels associated with low risk. The high-risk consumers also took more days off work, but the difference was not statistically significant. Among persons who were retired or not in the workforce, the mean days of reduced activity because of ill health varied according to gender, but the differences were again not significant. Women who consumed alcohol at levels associated with high risk, on average, had slightly more days of reduced activity than did women who consumed alcohol at levels associated with low risk. By contrast, men who consumed alcohol at levels associated with high risk, on average, had fewer days of reduced activity than did men who consumed alcohol at levels associated with low risk.
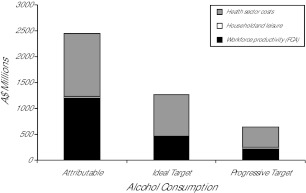
We found that if the liters of alcohol consumed per capita each year could be reduced to the ideal target, over time, potential opportunity cost savings of A$ 789 million to the health sector, A$ 427 million in workforce production (FCA), and A$ 21 million in home-based production could be achieved. This is because the 282 000 new cases of disease related to alcohol consumption at levels associated with high risk could be reduced by 98 000 (35%), the 1000 annual deaths attributed to alcohol consumption at levels associated with high risk could be reduced by 380 (38%), and the 61 000 DALYs attributable to this risk factor could be reduced by 21 000 (34%). The largest component of the total potential opportunity cost savings modeled would occur in the health sector, followed by workforce and household or leisure, respectively, when we used the FCA (Figure 1).
FIGURE 1—
Total potential opportunity cost savings from reductions in high-risk alcohol consumption: Australia, 2008.
If the liters of alcohol consumed per capita could be reduced from 9.8 to only 8.1 (the progressive target) half the potential opportunity cost savings of A$ 395 million to the health sector, A$ 220 million in workforce production (FCA), and A$ 11 million in home-based production could be gained over time from the reduction by 49 000 in annual new cases of disease related to alcohol consumption at levels associated with high risk, the reduction in deaths attributed to alcohol consumption at levels associated with high risk by 190, and the reduction in DALYs by 11 000.
We estimated losses, rather than gains, for additional early retirements (ideal target: 1400 persons; progressive target: 700 persons) because people who consumed alcohol at levels associated with high risk participated in the workforce at higher rates than the comparator group. Similarly, losses of leisure time (ideal target: 28 000 days; progressive target: 14 000 days) could occur if alcohol consumption reduction targets were achieved because persons consuming alcohol at levels associated with high risk reported having fewer lost days of leisure attributable to ill health than the comparator group.
A sensitivity analysis using the HCA indicated a loss in workforce production (ideal: A$ 1.54 billion; progressive: A$ 777 million) could be expected because of the relatively high value (compared with FCA) placed on younger workers leaving the workforce through alcohol-related death or disability, combined with the high workforce participation rates of young workers and the higher proportion of younger persons reporting the consumption of alcohol at levels associated with high risk. Further details of the sensitivity analyses are provided in the full study report.29
Tables 2 and 3 present the full economic benefits modeled including 95% uncertainty intervals for the point estimates in health status for each of the ideal and progressive alcohol consumption targets.
TABLE 2—
Health Status and Economic Outcomes of a Reduction in Liters of Alcohol Consumed per Capita: Australia, 2008
| High-Risk Alcohol Consumption, Health Status and Economic Outcomes | Ideal Target Reduction, Mean in 1000s (95% CI) | Progressive Target Reduction, Mean in 1000s (95% CI) |
| Per annum | ||
| DALYs | 21 | 11 |
| Incidence of disease | 98 | 49 |
| Mortality | 0.38 | 0.19 |
| Lifetime | ||
| Leisure, days | –28 (–2906, 2778) | –14 (–1453, 1389) |
| Absenteeism, days | 5002 | 2501 |
| Days out of home-based production role | 54 (–1252, 1341) | 27 (–626, 670) |
| Early retirement, persons | –1 | –1 |
Note. CI = confidence interval; DALYs = disability adjusted life years. Incidence of disease and mortality calculated for all age groups. Leisure and home-based production calculated for persons aged 15+ years. Absenteeism and early retirement calculated for persons aged 15–64 years. Negative numbers indicate the possibility of losses resulting from achieving the target, rather than gains.
TABLE 3—
Financial Outcomes of a Reduction in Liters of Alcohol Consumed Per Capita: Australia, 2008
| High-Risk Alcohol Consumption, Financial Outcomes | Ideal Target Reduction (A$ Million), Mean (95% CI) | Progressive Target Reduction (A$ Million), Mean (95% CI) |
| Health sector costs | 789 | 395 |
| Production costs HCA | –1541 (–4060,1123) | –777 (–2046,566) |
| Production costs FCA | 427 (–381, 1609) | 220 (–189, 846) |
| Recruitment and training costs | 30 | 15 |
| Leisure-based production | –12 (–813,779) | –6 (–406,389) |
| Home-based production | 21 (–495, 532) | 11 (–247, 266) |
| Total production HCA | –1532 (–4418,1398) | –772 (–2190,690) |
| Total production FCA | 435 (–1142, 2115) | 224 (–556, 1076) |
Note. CI = confidence interval; FCA = friction cost approach (preferred conservative estimate); HCA = human capital approach. These financial outcomes are opportunity cost estimates and not immediately realizable cash savings. The total opportunity cost savings are the sum of the health sector offsets and the combined workforce, household, and leisure-production effects. The mean estimates can be added together in this way, but not the uncertainty intervals, as both the components and the total are run as independent simulations. Recruitment and training costs are included in production gains or losses when we used the FCA but not counted when we used the HCA. No probabilistic uncertainty analysis was conducted for health sector offsets. Taxation is treated as a transfer payment and should not be added to production effects or health sector offsets. Health sector, leisure, and home-based production estimates are based on persons aged ≥ 15 years. Production gains (losses) and taxation effects are based on persons aged 15–64 years. Values are net present value using a 3% discount rate. Negative numbers indicate the possibility of losses resulting from achieving the target, rather than gains.
DISCUSSION
We assessed the potential benefits to health status, health sector costs, workforce paid production, home-based unpaid production, and leisure, following a reduction in the average liters of alcohol consumed (rather than total abstinence) among Australian adults. We selected the target level of reduction following an examination of actual achievements made by an equivalent country, therefore, considered feasible in Australia. The results show that gains can be significant and potentially larger than gains through targeted reductions (selected and modeled in a similar process) in smoking prevalence.16 Our findings provide important new information, especially for policymaking, regarding the value of investment in health promotion initiatives from a broader societal perspective.
If Australia were able to achieve a national reduction in adult alcohol consumption from an average 9.8 liters to 6.4 liters (an absolute reduction of 3.4 L) per capita per year, the largest component of the total potential opportunity cost savings modeled would occur in the health sector, followed by workforce and household production, respectively, using the more realistic FCA. We estimated a reduction in new cases of disease, decline in days absent from work, and an increase in days of home-based production.
Methodological issues surround the assessment of workforce production. Losses in workforce production using human capital occur because participation rates of young men (aged 15–24 years) and most women who consume alcohol at high-risk levels were greater than those of persons reporting low-risk alcohol consumption. To reduce levels of alcohol consumption could thus lead to a reduction in workforce participation. The FCA, on the other hand, remained positive because it captures only a portion of a year’s income under such circumstances and does not weight the behavior of the younger age groups as heavily. The decision to model net benefits (benefits gained–benefits lost) may have also contributed to negative findings associated with the potential loss of health benefits, particularly in the elderly moderate drinkers, among whom alcohol consumption is reduced at a population level.
There are some limitations to this study. First, we assumed a causal pathway between levels of alcohol consumed, health effects, and workforce behaviors. In the absence of longitudinal cohort studies, these assumptions remain untested. Cross-sectional survey data issues have contributed to some of the counterintuitive negative estimates reported. The NHS data showed that both men and women who consumed alcohol at levels associated with high risk reported significantly higher workforce participation rates. In addition, among retired and nonworking men, fewer days of reduced activity among those who consume alcohol at levels associated with high risk compared with men reporting alcohol consumption at levels associated with low risk was reported. It is not clear from the survey data whether alcohol-related ill health may have preceded or followed the current level of alcohol consumed by these older men.
The number of people reporting “high-risk” alcohol consumption on the NHS is small and volatile with wide confidence intervals, making modeled estimates unstable and more difficult to interpret. It is possible that misreporting on the NHS of the quantity of alcohol consumed on a long-term basis has influenced reported findings. We did not control for other risk factors or socioeconomic status because we were unable to undertake further subgroup analysis. Most people surveyed had more than 1 risk factor, and there is likely to be a complex relationship among these risk factors that will affect health and the economic outcomes modeled in the current study.
Our estimates are “opportunity cost savings” because the benefits will only be achieved by the adoption of effective interventions that will have implementation costs attached. It was outside the scope of the current study to include, as an offset, the cost of interventions needed to achieve the reduction targets. The recently released Assessing Cost Effectiveness Prevention report, which presents the evaluation of a range of potential preventive interventions to reduce alcohol consumption, confirmed the beneficial health effects of activities including increasing taxes, banning advertising, raising the minimum legal drinking age, and greater licensing controls. These were identified as cost-effective options and even cost-saving in some circumstances,30 but the authors of that study noted that there is a lack of political will to adopt tighter regulation given the current Australian culture.
Time lags to the realization of health benefits have also not been incorporated. Although improvements in some conditions are experienced reasonably soon after a decrease in alcohol consumption, reductions in the risk of cancers, for example, would occur more slowly. Financial savings are therefore not immediately realizable, but rather should be regarded as indicative estimates of resources used in current practice that could be available in the future for other purposes.
Our estimates are likely to be conservative. They are based on reduced incident cases of disease associated with high-risk alcohol consumption in 2008 and the associated lifetime costs or benefits based on these fewer incident cases. Prevalent cases of alcohol-related disease are also likely to benefit from reduction in consumption of alcohol, but we did not include the benefits accruing to those prevalent cases because of limitations in project scope and resourcing.
It is difficult to compare our findings with Australian and international literature. Cost estimates associated with alcohol misuse in Australia reported by Collins and Lapsley13 were generally higher than those reported in the current study. For example, net productivity costs of A$ 3.5 billion estimated by Collins and Lapsley were almost 3 times greater than the total workforce production of A$ 1.2 billion (FCA) estimated in the current study. However Collins and Lapsley’s estimates were based on past and present drug abuse by comparing a counterfactual scenario in which no alcohol misuse occurred to the present population.
A recent international review by Rehm et al.31 identified 4 studies that estimated the economic cost of excessive alcohol consumption in high-income countries (France,32 Scotland,33 Canada,34 United States35), which they deemed to be comparable methodologically. These were all prevalence-based cost-of-illness studies, which included a broader range of direct and indirect cost categories than the current study, and relied on the HCA (and, in 1 instance, willingness-to-pay method) to estimate productivity costs. Applying the findings from these studies, Rehm et al. identified the greatest cost contributors to excessive alcohol consumption to be productivity loss (72.1%), followed by direct health care costs (12.8%) and other direct costs (11.6%). By modeling a target reduction of per capita consumption of alcohol, taking an incident case approach to health sector costs reduction, and utilizing the more conservative FCA, we found in the current study the largest potential opportunity cost savings to be in the health care sector followed by the workforce and household sectors.
Conclusions
A greater understanding of the magnitude and distribution of avoidable economic costs associated with a reduction in liters of national annual alcohol consumption has been achieved. Overall opportunity cost savings are largest in the health sector, followed by gains in workforce and household production, and arise from the reduction in annual new cases of alcohol-related disease, deaths, and DALYs. The decision to apply reduction targets using an Arcadian mean enabled more realistic estimates in the Australian context and enables comparisons to the benefits of other risk factor reductions such as tobacco smoking, which have been assessed with a similar methodology. A suitable next step would be a consideration of cost-effective interventions and attention to stakeholder concerns to facilitate a reduction in excessive alcohol consumption. This methodology could be adopted in other countries to provide economic argument supportive of the prevention debate regarding alcohol consumption, where needed.
Acknowledgments
Deakin University and the National Stroke Research Institute received funding from the Victorian Health Promotion Foundation (VicHealth) to undertake this study following a competitive tender process.
Members of the advisory committee for the study are thanked for the time and expertise they contributed, which included staff from the Victoria Department of Treasury and Finance, the Victorian Department of Health, the Centre for Alcohol Social Research, Faculty of Business and Economics (Monash University), various health promotion experts from VicHealth, and external experts from Deakin University and the University of Wollongong. Theo Vos, PhD, MSc, (University of Queensland) is acknowledged for providing access to the relevant 2003 Australian Burden of Disease study files and his ongoing advice.
Human Participation Protection
Because preexisting data sources were used, no protocol approval was needed for this study.
References
- 1.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–2233 [DOI] [PubMed] [Google Scholar]
- 2.Balakrishnan R, Allender S, Scarborough P, Webster P, Rayner M. The burden of alcohol-related ill health in the United Kingdom. J Public Health (Oxf). 2009;31(3):366–373 [DOI] [PubMed] [Google Scholar]
- 3. Australian Alcohol Guidelines: Health Risks and Benefits. Canberra, Australia: National Health and Medical Research Council; 2001.
- 4. OECD Health Data. Paris, France: Organization for Economic Cooperation and Development; 2008. Available at: http://www.oecd.org/document/16/0, 3343, en_2649_34631_2085200_1_1_1_1,00.html. Accessed July 9, 2008.
- 5.Begg S, Vos T, Barker B, Stevenson C, Stanley L, Lopez AD. The Burden of Disease and Injury in Australia 2003. Vol PHE 82. Canberra, Australia: Australian Institute of Health and Welfare; 2007:337 [Google Scholar]
- 6.Jackson R, Broad J, Connor J, Wells S. Alcohol and ischaemic heart disease: probably no free lunch. Lancet. 2005;366(9501):1911–1912 [DOI] [PubMed] [Google Scholar]
- 7.Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W. Moderate alcohol use and reduced mortality risk: systematic error in prospective studies. Ann Epidemiol. 2007;17(5, suppl):S16–S23 [DOI] [PubMed] [Google Scholar]
- 8.Australian Drug Foundation Blood alcohol concentration. 2011. Available at: http://www.druginfo.adf.org.au/topics/bac. Accessed January 31, 2011
- 9.Ministerial Council on Drug Strategy National Alcohol Strategy 2006–2011. Canberra, Australia: Commonwealth of Australia; 2006 [Google Scholar]
- 10.Drummond A, Sullivan G, Cavallo A. An Evaluation of the Random Breath Testing Initiative in Victoria 1989–1990. Quasi-experimental Time Series Approach. Melbourne, Australia: Monash University Accident Research Centre; 1992 [Google Scholar]
- 11.Australia: The Healthiest Country by 2020. National Preventative Health Strategy—The Roadmap for Action. Canberra, Australia: National Preventative Health Taskforce; 2009 [Google Scholar]
- 12.Bhattacharya J, Lakdawalla DN. The labor market value of health improvements. Forum Health Econ Policy. 2006;9(2 [Biomedical Research and the Economy]):article 2 [Google Scholar]
- 13.Collins DJ, Lapsley HM. The costs of tobacco, alcohol and illicit drug abuse to Australian Society in 2004/05. Canberra, Australia: Department of Health and Ageing; 2008. Monograph series no. 64 [Google Scholar]
- 14. The Growing Cost of Obesity in 2008: Three Years On. Melbourne, Australia: Access Economics ;2008. Report prepared for Diabetes Australia.
- 15.National Health Survey 2004–05. Canberra, Australia: Australian Bureau of Statistics; 2006. Vol Cat. No. 4364.0 [Google Scholar]
- 16.Magnus A, Cadilhac D, Sheppard L, Cumming TB, Pearce D, Carter R. The economic gains of realistic smoking cessation targets for Australia. Am J Public Health. 2011(2);101:321–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cadilhac DA, Magnus A, Sheppard L, Cumming TB, Pearce DC, Carter R. The societal benefits of reducing six behavioural risk factors: An economic modelling study from Australia. BMC Public Health. 2011;11:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cadilhac DA, Cumming TB, Sheppard L, Pearce DC, Carter R, Magnus A. The economic benefits of reducing physical inactivity: An Australian example. Int J Behav Nutr Phys Act. 2011;8:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Armstrong B. Morbidity and mortality in Australia: how much is preventable? : McNeil JJ, King RWF, Jennings GL, Powles J, A Textbook of Preventive Medicine. Melbourne, Australia: Edward Arnold; 1990. [Google Scholar]
- 20.Brand DA, Saisana M, Rynn LA, Pennoni F, Lowenfels AB. Comparative analysis of alcohol control policies in 30 countries. PLoS Med. 2007;4(4):e151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Health System Expenditure on Disease and Injury in Australia, 2000–01. Canberra, Australia: Australian Institute of Health and Welfare; 2004. Vol AIHW cat. no. HWE 26 [Google Scholar]
- 22.Public Health Expenditure in Australia, 2006–07. Canberra, Australian Capital Territory, Australia: Australian Institute of Health and Welfare; 2008 [Google Scholar]
- 23.National Health Survey (2004–05) Basic and expanded CURF data. Findings based on use of ABS CURF data, CD-ROM and RADL. Canberra, Australia: Australian Bureau of Statistics; 2006 [Google Scholar]
- 24.How Australians Use Their Time, 2006. Canberra, Australia: Australian Bureau of Statistics; 2008. Vol cat. no. 4153.0 [Google Scholar]
- 25.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996 [Google Scholar]
- 26.Koopmanschap MA, Rutten FF. A practical guide for calculating indirect costs of disease. Pharmacoeconomics. 1996;10(5):460–466 [DOI] [PubMed] [Google Scholar]
- 27.Liljas B. How to calculate indirect costs in economic evaluations. Pharmacoeconomics. 1998;13(1 pt 1):1–7 [DOI] [PubMed] [Google Scholar]
- 28.Jacobs P, Fassbender K. The measurement of indirect costs in the health economics evaluation literature: a review. Int J Technol Assess Health Care. 1998;14(4):799–808 [DOI] [PubMed] [Google Scholar]
- 29.Cadilhac D, Magnus A, Cumming T, Sheppard L, Pearce D, Carter R. The Economic Benefits of Reducing Disease Risk Factors. Melbourne, Australia: Deakin Health Economics Group, Deakin University and National Stroke Research Institute; 2009 [Google Scholar]
- 30.Vos T, Carter R, Barendregt Jet al. Assessing Cost-Effectiveness in Prevention (ACE-Prevention): Final Report. Melbourne, Australia: University of Queensland, Brisbane, and Deakin University; 2010 [Google Scholar]
- 31.Rehm J, Taylor B, Patra J, Gmel G. Avoidable burden of disease: conceptual and methodological issues in substance abuse epidemiology. Int J Methods Psychiatr Res. 2006; 15(4):181–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fenoglio P, Parel V, Kopp P. The social cost of alcohol, tobacco and illicit drugs in France, 1997. Eur Addict Res. 2003;9(1):18–28 [DOI] [PubMed] [Google Scholar]
- 33.Varney SJ, Guest JF. The annual societal cost of alcohol misuse in Scotland. Pharmacoeconomics. 2002;20(13):891–907 [DOI] [PubMed] [Google Scholar]
- 34.Rehm J, Gnam W, Popova Set al. The costs of alcohol, illegal drugs, and tobacco in Canada, 2002 (report). J Stud Alcohol Drugs. 2007;68(6):886–895 [DOI] [PubMed] [Google Scholar]
- 35.Harwood H. Updating Estimates of the Economic Costs of Alcohol Abuse in the United States: Estimates, Update Methods, and Data. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2000 [Google Scholar]