Abstract
One of the documented benefits of neonatal circumcision is protection against invasive penile cancer. To date there have been a handful of published cases of invasive penile cancer in men circumcised as neonates. We report a case of a 73-year-old man, with a history of neonatal circumcision with no evidence of previous human papillomavirus exposure, who developed a buried penis secondary to obesity. He was diagnosed with Grade 2, pT3N0 squamous cell carcinoma of the penis. This report suggests that buried penis may pose a risk factor for the development of penile cancer despite the protective effects of neonatal circumcision. Thus periodic examination of a buried penis is warranted even in patients with no risk factors for penile cancer. A review of the literature is provided.
Introduction
Penile cancer usually affects males in the sixties and seventies. Risk factors for developing the disease include the presence of foreskin,1–3 phimosis,4–6 infection with HPV and the subsequent development of warts,7,8 poor penile hygiene and the irritating effects of smegma,9 chronic balanitis or trauma,10,11 prior treatment with psoralen and ultraviolet A photo chemotherapy (PUVA) for psoriasis,12 tobacco use of any kind,10,11,13 and high risk sexual behaviours with multiple sexual partners.10
Currently, there is a lack of literature addressing the topic of a buried penis and its risk for developing penile cancer. We report a case of invasive penile cancer in a male who underwent neonatal circumcision and then as an adult developed a buried penis secondary to aging and obesity. We propose that buried penis itself may pose a contributing risk to the development of penile cancer, despite the documented protective effects of neonatal circumcision.
On a global level, upwards of 30% of males are circumcised, making circumcision the most common surgical procedure in the world.14 On average, there are about 25 circumcisions being performed per minute worldwide.15 Most of these surgeries are performed for religious or cultural reasons and are therefore termed non-therapeutic. There are also therapeutic circumcisions in an attempt to treat an underlying pathologic process. A debate that continues to linger, and has for some time, is whether non-therapeutic circumcisions should be endorsed by health professionals. At the present time, the Canadian Pediatric Society and the American Academy of Pediatrics do not recommend routine circumcisions of newborns. Their stance stems from the fact that there are no valid medical indications for circumcision in neonates.16,17 Some of the documented benefits conferred by neonatal circumcision include decrease incidence of urinary tract infection (UTI) in the first year of life, decreased risk of HIV infection, deceased risk of human papillomavirus (HPV), and decreased incidence of invasive penile cancer.18,19 A long-standing misconception in medicine, dating back to the early 1930s, is that neonatal circumcision confers absolute protection against invasive penile cancer.20
Case
A 73-year-old man presented in urinary retention to the emergency room. After failed attempts at Foley catheter insertion, the patient underwent suprapubic cystotomy to decompress the bladder. Catheter insertion failed as the patient had a buried penis and a firm, indurated mass at the glans that extended to the shaft of the penis. This lesion caused a stricture just proximal to the urethral meatus making it difficult for catheter insertion. The patient described a remote smoking history and he was circumcised as a neonate. There was no history of HPV infection or high risk sexual behaviour. There was no history of trauma to the penis and the patient was not concerned about the lesion as he was not fully aware of it because of his buried penis. The patient had recurrent UTIs in the past year and described episodes of hematuria that had resolved prior to his presentation. The patient’s medical history was significant for type II diabetes mellitus, hypertension, dyslipidemia and basal cell carcinoma on the head and back treated with local excision and radiation.
On examination, the patient had a buried penis with an indurated lesion at the glans that extended to the shaft of the penis. There was no palpable lymphadenopathy, digital rectal examination and examination of the scrotum and testicles was unremarkable.
The patient went on to have a biopsy of the penile lesion under local anesthesia. The pathology came back as invasive moderately differentiated squamous cell carcinoma. Prior to surgery, he underwent computed tomography (CT) of the chest, abdomen and pelvis, which was unremarkable. A preoperative magnetic resonance imaging revealed a mass centred in the glans penis, involving distal ends of both corpora cavernosa and the corpus spongiosum – causing urethral obstruction (Fig. 1). Inguinal lymphadenopathy was not identified.
Fig. 1.
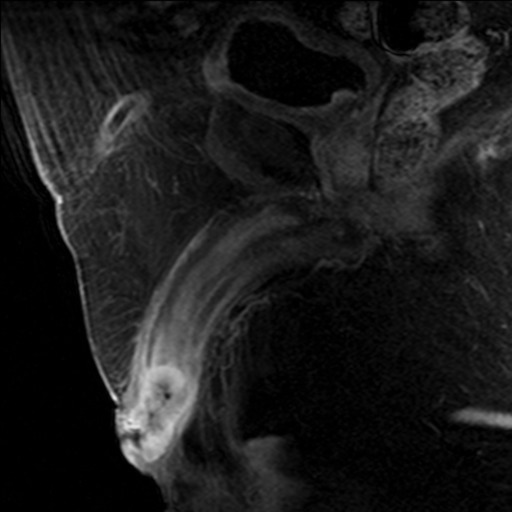
A preoperative magnetic resonance imaging showing a mass centred in the glans penis causing urethral obstruction.
The patient underwent radical penectomy and creation of a perineal urethrostomy. The final pathology revealed a Grade 2, pT3 squamous cell carcinoma of the penis with no evidence of lymphovascular or perineural invasion (Fig. 2). Immuno-histochemical staining for p16, a surrogate marker for HPV infection, was negative. As a result of the grade and stage of the penile cancer, this patient was at risk for harbouring disease in the inguinal lymph nodes.21 With no palpable lymphadenopathy, the established guidelines would dictate that the patient undergo a modified bilateral radical inguinal lymph node dissection. All lymph nodes assessed (n = 4) were negative for malignancy and therefore conversion to the standard inguinal lymph node dissection was not indicated. The patient continues with routine surveillance and has now been disease-free for more than 24 months.
Fig. 2.
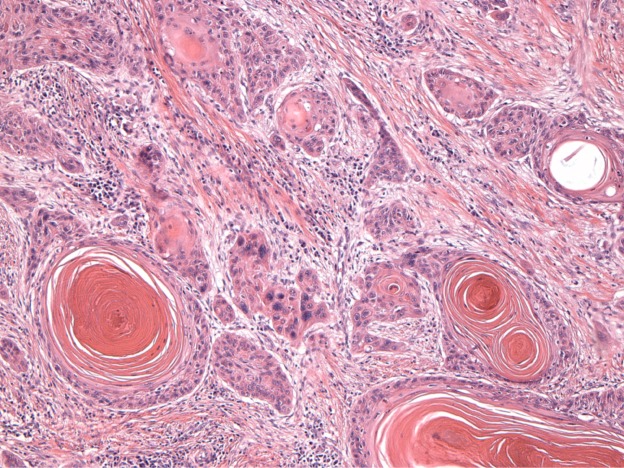
Infiltrating squamous cell carcinoma showing irregular pattern of malignant squamous cells, focally showing keratin pearls.
Discussion
Penile cancer, although a relatively rare disease in the Western world, is a disease with a high morbidity and mortality rates. The incidence of penile cancer varies among populations. These variations in incidence rates are related considerably to the practice of neonatal circumcision. For example, the lowest incidence of penile cancer is reported among Israeli Jews, at 0.1/100 000, where neonatal circumcision is universally practiced.22 Yet, neonatal circumcision does not confer absolute protection against the development of penile cancer. Our literature search (in PubMed with neonatal circumcision and penile cancer as keywords) found 16 published cases of penile cancer in men circumcised as neonates.2,23–34 Most recently, Saibishkumar and colleagues34 reported three separate cases of invasive penile cancer in men circumcised as neonates. A commonality among all these patients was their remote history of HPV infection, a factor thought to play a critical role in the development of invasive penile cancer. The specific subtypes of HPV that have been implicated in the development of in situ and invasive penile cancer include 16, 18, 31 and 33.35 Of these, HPV 16 is the most frequently detected subtype in primary carcinomas of the penis.35 We report, for the first time, a case of a circumcised man, with no history of HPV infection who developed invasive penile cancer in a buried penis.
Buried penis, also referred to as hidden penis, inconspicuous penis and/or concealed penis, is a condition in which the penile shaft is invisible below the surface of the pre-pubic skin and/or scrotum. Such anatomy gives the impression of a short phallus, even though corporeal length is normal and palpable under the overlying skin and subcutaneous tissue.36 In adults, buried penis can result from aging, obesity, complications from an overly aggressive circumcision and, in rare cases, a missed congenital buried penis.37,38 In the case of the patient presented, it appears that his buried penis was a combination of aging and obesity.38 The patient had no complications throughout puberty and in early adulthood related to the circumcision; in the last two decades, however, he had difficulty seeing his penis.
The psychological consequences related to a buried penis are well-documented and include distortion of body image, locker room syndrome and functional hindrance of sexual activity perhaps leading to decreased sex drive. Physical consequences related to this condition include painful erection, difficulty with voiding, chronic balanitis and difficulty in maintaining penile hygiene.37,39 Although there is no direct link between a buried penis and penile cancer, chronic balanitis and difficulty in maintaining penile hygiene (two consequences of a buried penis) are also identified as risk factors for penile cancer.9–11
Conclusion
Our case suggests that the development of a buried penis later in life, despite the neonatal circumcision, may pose a risk factor for the development of penile cancer through such mechanisms as balanitis and poor penile hygiene, both of which are thought to be a sequelae of buried penis and are risk factors for squamous cell cancer of the penis.28–30 With the current global obesity epidemic,40,41 there will undoubtedly be more patients who present with a buried penis as a result of increasing abdominal girth. Whether they are circumcised or not, proper inspection of the penis in these patients by primary care physicians and specialists will become increasingly important.
Footnotes
Competing interests: None declared.
This paper has been peer-reviewed.
References
- 1.Wolbarst AL. Circumcision and penile cancer. Lancet. 1932;1:150–3. doi: 10.1016/S0140-6736(01)24346-3. [DOI] [Google Scholar]
- 2.Dean Al., Jr Epithelioma of the penis. J Urol. 1935;33:252–83. [Google Scholar]
- 3.Schoen EJ. The relationship between circumcision and cancer of the penis. CA Cancer J Clin. 1991;41:306–9. doi: 10.3322/canjclin.41.5.306. [DOI] [PubMed] [Google Scholar]
- 4.Daling JR, Madeleine MM, Johnson LG, et al. Penile cancer: importance of circumcision, human papillomavirus and smoking in situ and invasive disease. Int J Cancer. 2005;116:606–16. doi: 10.1002/ijc.21009. [DOI] [PubMed] [Google Scholar]
- 5.Dillner J, von Krogh G, Horenblas S, et al. Etiology of squamous cell carcinoma of the penis. Scand J Urol Nephrol. 2000;34:189–93. doi: 10.1080/00365590050509913. [DOI] [PubMed] [Google Scholar]
- 6.Maden C, Sherman KJ, Beckmann AM, et al. History of circumcision, medical conditions, and sexual activity and risk of penile cancer. J Natl Cancer Inst. 1993;85:19–24. doi: 10.1093/jnci/85.1.19. [DOI] [PubMed] [Google Scholar]
- 7.Heideman DA, Waterboer T, Pawlita M, et al. Human papillomavirus-16. Is the predominant type etiologically involved in penile squamous cell carcinoma. J Clin Oncol. 2007;25:4550–6. doi: 10.1200/JCO.2007.12.3182. [DOI] [PubMed] [Google Scholar]
- 8.McCance DJ, Kalache A, Ashdown K, et al. Human papillomavirus types 16 and 18 in carcinomas of the penis from Brazil. Int J Cancer. 1986;37:55–9. doi: 10.1002/ijc.2910370110. [DOI] [PubMed] [Google Scholar]
- 9.Kalcev B. Circumcision and personal hygiene in school boys. Med Officer. 1964;112:171–3. [Google Scholar]
- 10.Hellberg D, Valentin J, Eklund T, et al. Penile cancer: is there an epidemiological role for smoking and sexual behaviour. Br Med J Clin Res Ed. 1987;295:1306–8. doi: 10.1136/bmj.295.6609.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tseng HF, Morgenstern H, Mack T, et al. Risk factors for penile cancer: results of a population-based case-control study in Los Angeles county. Cancer Causes Control. 2001;12:267–77. doi: 10.1023/A:1011266405062. [DOI] [PubMed] [Google Scholar]
- 12.Gross G, Pfister H. Role of human papillomavirus in penile cancer, penile intraepithelial squamous cell neoplasias and in genital warts. Med Microbiol Immunol. 2004;193:35–44. doi: 10.1007/s00430-003-0181-2. [DOI] [PubMed] [Google Scholar]
- 13.Harish K, Ravi R. The role of tobacco in penile carcinoma. Br J Urol. 1995;75:375–7. doi: 10.1111/j.1464-410X.1995.tb07352.x. [DOI] [PubMed] [Google Scholar]
- 14.Moses S, Bailey RC, Ronald AR. Male circumcision: assessment of health benefits and risks. Sex Transm Inf. 1998;74:368–73. doi: 10.1136/sti.74.5.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond T. A preliminary poll of men circumcised in infancy or childhood. BJU Int. 1999;83:85–92. doi: 10.1046/j.1464-410x.1999.0830s1085.x. [DOI] [PubMed] [Google Scholar]
- 16.American Academy of Paediatrics Task Force on Circumcision Circumcision policy statement. Paediatrics. 1999;103:686–93. doi: 10.1542/peds.103.3.686. [DOI] [PubMed] [Google Scholar]
- 17.Andrews W, McMillan D, Ohlsson A, et al. Clinical Practice Guidelines: Neonatal Circumcision Revisited. Can Med Assoc J. 1996;154:769–80. [Google Scholar]
- 18.Alanis MC, Lucidi RS. Neonatal circumcision: A review of the world’s oldest and most controversial operation. Obstet Gynecol Surv. 2004;59:379–95. doi: 10.1097/00006254-200405000-00026. [DOI] [PubMed] [Google Scholar]
- 19.Morris BJ. Why circumcision is a biomedical imperative for the 21st century. Bioessays. 2007;29:1147–58. doi: 10.1002/bies.20654. [DOI] [PubMed] [Google Scholar]
- 20.Cold CJ, Storms MR, Van Howe RS. Carcinoma in situ of the penis in a 76-year-old circumcised man. J Fam Pract. 1997;44:407–10. [PubMed] [Google Scholar]
- 21.Ficarra V, Zattoni F, Artinai W, et al. Nomogram predictive of pathological inguinal lymph node involvement in patients with squamous cell carcinoma of the penis. J Urol. 2006;175:1700–5. doi: 10.1016/S0022-5347(05)01003-7. [DOI] [PubMed] [Google Scholar]
- 22.Curado MP, Edwards B, Shin HR, et al., editors. Cancer incidence in five continents. IX. Lyon: IARC Scientific Publications; 2007. No. 160. [Google Scholar]
- 23.Marshall VF. Typical carcinoma of the penis in a male circumcised in infancy. Cancer. 1953;6:1044–5. doi: 10.1002/1097-0142(195309)6:5<1044::AID-CNCR2820060526>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 24.Reitman PH. An unusual case of penile carcinoma. J Urol. 1953;69:547–9. doi: 10.1016/S0022-5347(17)68110-2. [DOI] [PubMed] [Google Scholar]
- 25.Paquin AJ, Jr, Pearce JM. Carcinoma of the penis in a man circumcised in infancy. J Urol. 1955;74:626–7. doi: 10.1016/S0022-5347(17)67329-4. [DOI] [PubMed] [Google Scholar]
- 26.Amelar RD. Carcinoma of the penis due to trauma occurring in the male patient circumcised at birth. J Urol. 1956;75:728–9. doi: 10.1016/S0022-5347(17)66872-1. [DOI] [PubMed] [Google Scholar]
- 27.Ledlie RC, Smithers DW. Carcinoma of the penis in a man circumcised in infancy. J Urol. 1956;76:756–7. doi: 10.1016/S0022-5347(17)66762-4. [DOI] [PubMed] [Google Scholar]
- 28.Kaufman JJ, Sternberg TH. Carcinoma of the penis in a circumcised man. J Urol. 1963;90:449–450. doi: 10.1016/S0022-5347(17)64435-5. [DOI] [PubMed] [Google Scholar]
- 29.Melmed EP, Pyne JR. Carcinoma of the penis in a Jew circumcised in infancy. Br J Surg. 1967;54:729–731. doi: 10.1002/bjs.1800540818. [DOI] [PubMed] [Google Scholar]
- 30.Leiter E, LefkovitIs AM. Circumcision and penile carcinoma. N Y State J Med. 1975;75:1520–1522. [PubMed] [Google Scholar]
- 31.Boczko S, Freed S. Penile carcinoma in circumcised males. N Y State J Med. 1979;79:1903–1904. [PubMed] [Google Scholar]
- 32.Rogus BJ. Squamous cell carcinoma in a young circumcised man. J Urol. 1987;138:861–862. doi: 10.1016/s0022-5347(17)43402-1. [DOI] [PubMed] [Google Scholar]
- 33.Kanik AB, Lee J, Wax F, et al. Penile verrucous carcinoma in a 37 year old circumcised man. J Am Acad Dermatol. 1997;37:329–331. doi: 10.1016/S0190-9622(97)80384-2. [DOI] [PubMed] [Google Scholar]
- 34.Saibishkumar EP, Crook J, Sweet J. Neonatal circumcision and invasive squamous cell carcinoma of the penis: a report of 3 cases and a review of the literature. CUAJ. 2008;2:39–42. doi: 10.5489/cuaj.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wiener JS, Walther PJ. The association of oncogenic human papillo-maviruses with urologic malignancy. Surg Oncol Clin North Am. 1995;4:257–76. [PubMed] [Google Scholar]
- 36.Lim DJ, Barraza MA, Stevens PS. Correction of retractile concealed penis. J Urol. 1995;153:1668. doi: 10.1016/S0022-5347(01)67500-1. [DOI] [PubMed] [Google Scholar]
- 37.Alter GJ, Ehrlich RM. A new technique for correction of the hidden penis in children and adults. J Urol. 1999;161:455–9. doi: 10.1016/S0022-5347(01)61922-0. [DOI] [PubMed] [Google Scholar]
- 38.Casale AJ, Beck SD, Cain MP, et al. Concealed penis in childhood: A spectrum of etiology and treatment. J Urol. 1999;162:1165–8. doi: 10.1016/S0022-5347(01)68114-X. [DOI] [PubMed] [Google Scholar]
- 39.Donatucci CF, Ritter EF. Management of the buried penis in adults. J Urol. 1998;159:420–4. doi: 10.1016/S0022-5347(01)63939-9. [DOI] [PubMed] [Google Scholar]
- 40.Desapriya EBR. Obesity epidemic. Lancet. 2004;364:1488. doi: 10.1016/S0140-6736(04)17270-X. [DOI] [PubMed] [Google Scholar]
- 41.Wald N, Willett W. Reversing the obesity epidemic. Lancet. 2004;364:140. doi: 10.1016/S0140-6736(04)16623-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


