Abstract
Malaria parasites have been suggested to alter the behavior of mosquito vectors to increase the likelihood of transmission. Some empirical evidence supports this hypothesis, yet the role of manipulation is ignored in most epidemiological models, and behavioral differences between infected and uninfected females are not considered in the development or implementation of control measures. We suggest that this disconnect exists because the link between behavioral alteration and actual transmission in the field has yet to be fully demonstrated or quantified. We review and discuss the current evidence for manipulation, explore its potential significance for malaria transmission and suggest ways to move this hypothesis forward from theory to potential application in malaria control.
Keywords: manipulation, Plasmodium, malaria, transmission, mosquito behavior, foraging
Manipulation by parasites
Transmission is a key determinant of parasite fitness. There are numerous examples of parasites altering the behavior of their host to increase the probability of transmission [1]. For example, ants infected with certain species of fungi ascend leaves at the appropriate moment prior to death to position themselves for prime dispersal of fungal spores [2]. Crab parasites castrate their crustacean hosts and manipulate them into caring for the parasite as they would their own offspring [3]. Normally terrestrial crickets leap into water allowing their hairworm parasite to complete its life cycle [4]. A variety of studies have shown that malaria parasites can alter mosquito feeding behavior. These results have been interpreted as adaptive manipulation of vector behavior by the malaria parasite to enhance transmission (the ‘manipulation hypothesis’). The majority of evidence for manipulation, however, comes from avian or rodent model systems rather than human malaria and focuses on isolated components of mosquito behavior. Accordingly, the implications for human malaria transmission are uncertain. Here we explore the evidence, evaluate what impacts manipulation might have on transmission, and propose further research that might allow for the incorporation of manipulation into understanding transmission dynamics and controlling disease.
Malaria and mosquitoes
It is not difficult to imagine that natural selection might favor a malaria parasite that could increase its own transmission. According to the manipulation hypothesis, malaria parasites decrease mosquito blood-feeding and other risky behaviors during the pre-infectious phase, thereby decreasing the risk of host death during parasite development (oocyst-stage). Parasites then increase vector feeding rate once they have become infectious (sporozoite-stage) (reviewed in [5]).
There is evidence that these behavioral changes occur. In laboratory studies, female mosquitoes infected with oocyst-stage malaria parasites were less persistent at blood feeding and less likely to resume feeding if interrupted [6-7]. Other studies reported that sporozoite-infected females probed more frequently than uninfected controls [6], [8–10] and were more persistent at attempts to obtain a blood meal [7] . In one study, sporozoite-infected females also took less blood per meal which in the field may lead these females to feed more than once within a gonotrophic cycle [6]. However, another studies found that infection status did not affect blood meal size [11] or probing duration [12].
Some field data are also consistent with infection-induced changes in mosquito behavior. For example, in human baited catches, infected and uninfected An. punctulatus were observed to take blood meals at different times of night [13]. Koella and others [14] found that sporozoite-infected An. gambiae females were more likely than uninfected females to take blood from multiple hosts in the same night and suffered higher feeding-associated mortality [15]. A clinical study in the Gambia reported instances in which children sharing rooms appeared to have received infectious bites from the same female on the same night [16]. Infected An. punctulatus females have been reported to exhibit different engorgement rates over a feeding period compared with uninfected females [17].
These examples suggest that manipulation might occur in the human malaria system, but determining how behavioral changes relate to human malaria transmission is difficult. For one thing, relevant data come from studies using various vector-parasite combinations. Several studies have measured the behavioral effect of the bird malaria parasite, P. gallinaceum, on Aedes aegypti, a mosquito that does not transmit human malaria parasites [6], [8] . Studies utilizing human-relevant vector species often test the effect of infection with rodent malaria [7], [9], [12],[18]. While such research is tantalizing, to our knowledge no studies have directly compared manipulation in model and human malaria systems, leaving the connection between them uncertain.
Furthermore, much of the behavioral data concerns the effect of Plasmodium infection on the ‘at-host’ feeding behavior of mosquitoes, generally using anesthetized hosts placed very close to mosquitoes [8], [10], [12]. ‘Bloodfeeding’ describes a suite of behaviors including detecting the host, alighting on it, probing, piercing, locating blood, ingesting it, and terminating the feed [19]. Each of these components represents an isolated stimulus response, with the output of one event becoming the input of the next [19]. The narrowly focused assays conducted to date make it difficult to characterize how infection affects this complex set of behaviors.
Implications for transmission
The reproductive rate of the malaria parasite (which provides a measure of transmission intensity) is captured in the Ross-MacDonald framework, R0=ma2bce-ps/pr [20], [21]. In this equation, ‘m’ is the ratio of vectors to humans, ‘a’ the mosquito biting frequency, ‘b’ the efficiency at which the parasite passes from mosquito to human, ‘c’ the efficiency that the parasite moves from human to mosquito, ‘p’ the daily survival of the vector, ‘s’ the extrinsic incubation period of the parasite, and ‘r’ the recovery rate of human hosts. Current evidence for manipulation indicates that the parasite might alter vector biting frequency (a) and the likelihood that a feeding attempt results in transmission (b), by increasing the feeding rate and altering the probing behavior of sporozoite-infected females. It might also alter daily survival (p) by decreasing feeding and reproductive stressors during parasite development prior to transmission.
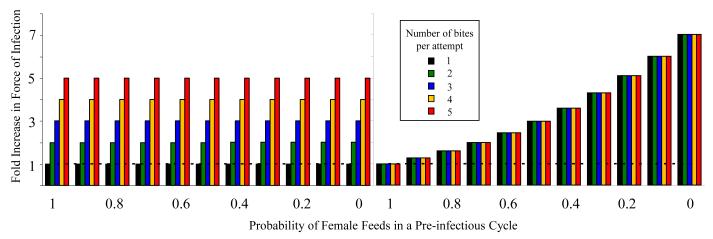
Quantifying these effects in a simple model (Box 1) reveals that relatively small behavioral changes can have substantial effects on transmission. The model’s predictions about quantitative increases in transmission are critically dependent on mortality schedules, particularly the mortality risks associated with feeding. Unfortunately, remarkably little is known about adult mortality in the field. Even so, our analysis suggests that, for plausible parameter values, parasite manipulation of vector behavior could increase the force of infection by 5-fold or more. To put that figure in perspective, a recent study found that high coverage with insecticide-treated nets reduced entomological inoculation rates (number of infectious bites per person per unit time) by a similar order of magnitude [22]. Another reported 7-fold increase in the number of infectious bites per person between transmission study sites and a fold increase in sites between dry and wet seasons[23]. Thus, behavioral alterations could be impacting malaria transmission ecology and overall disease dynamics as much as bed nets of major environmental variation.
Box 1. What would the impact of manipulation be on transmission intensity?
In order to model the relative effect of manipulation on force of infection we compared the number of predicted infectious bites per female (B) for mosquitoes that either express of do not express manipulation phenotypes. We calculated B for all groups using the equation;
where W is the probability that the female survives one cycle of resting, search and laying between feeding attempts, s is background mortality associated with time spent searching for blood hosts, f is background mortality associated the time spent with searching for an oviposition site, M is the probability an oocyst-positive female attempts to feed in each feeding cycle, A is the number of times a sporozoite-positive female attempts to bite per feeding cycle, n is the number of feeding cycles that the female experiences between taking an infected feed and becoming infectious (sporogony), k is the probability that the female survives a bite, incorporating both pre-and post-bite mortality, and λ is the combined incremental mortality associated with a single feed plus an attempt to lay.
Unmanipulated females feed once during each cycle (M=1) and attempt to bite one host per feeding cycle (A=1). Therefore, the ratio of force of infection for manipulated (B) to unmanipulated (B0) females would be:
Three days were assumed between blood meals [53] , 4 feeding cycles (12 days) from infectious bloodmeal to sporozoite-positivity[54], and females were assumed to attempt to bite no more than five different humans during a single feeding cycle.
The degree that mortality is associated with feeding events is unknown. Thus, we used two contrasting scenarios. For both we started with a commonly used assumption of 15% mortality per day [24], [55] to give 38.6% per feeding cycle, splitting feeding-associated mortality evenly between pre-and post-bite mortality. We assumed that this 38.6% mortality per feeding cycle was either almost completely associated with the feeding event (99.9%) or that this mortality was not at all associated with a feeding event (0.001%).
Under either scenario, manipulation can have a substantial impact on the force of infection. Under our assumptions, changes in the number of bites per feeding attempt in the sporozoite stage can increase the relative force of infection (number of infectious bites per female) by as much as 500%, while oocyst-stage manipulation could increase force of infection by as much as 700%. In a scenario assuming heavy feeding-associated mortality, even just a 10% decrease in the probability of a female feeding during the pre-infectious stage results in a 27% increase in relative force of infection.
The actual pattern of mortality in the field is likely to be intermediate between our two extreme mortality scenarios, with changes in relative force of infection resulting from effects on both non-feeding and feeding-related mortality. The impact of manipulation on transmission can, however, still be considerable. For example, if we split the mortality evenly between feeding events and daily mortality then the increase in force of infection can still be over 400%. Such estimates, tentative as they are, show that manipulation could be of substantial epidemiological significance.
Manipulation-induced behavioral changes would also affect understanding of how current control tools such as Insecticide Treated Nets (ITNs) actually work. At present, infected and uninfected mosquitoes are presumed to behave in identical ways, feeding every 2-3 days across their lifetime [24–27]. This repeat feeding means mosquitoes have multiple chances of contacting a lethal ITN before they become infectious, which is why even moderate coverage of ITNs can theoretically lead to reduced transmission intensity [28]. However, if manipulation reduces this exposure risk, higher coverage of ITNs could be required to achieve a given level of control (and by extension, manipulation could make eradication that much harder).
Research priorities to resolve the issues
Various lines of research would enable better characterization of the putative manipulation phenotype, a critical step in assessing its effect on transmission (Box 1). Not least, the current evidence for manipulation needs to be greatly improved before we can understand the impact of parasite-induced behavior change on disease epidemiology.
Expanded range of behavioral assays
There is evidence from both the laboratory and the field for the manipulation hypothesis. However, laboratory experiments have been conducted almost exclusively on model species and field experiments (justifiably) do not control for confounding variables, such as female mosquito age. Bringing a natural system into the laboratory, conducting controlled experiments, and then confirming results in the field would greatly strengthen the current evidence.
Most of the laboratory work on the feeding behaviors of malaria-infected mosquitoes has occurred over a distance of less than 36 cm [6–10], [12]. While these studies have revealed differences in behavior, it is not clear how relevant these differences are in the context of natural host seeking over distances of many meters. Expanding behavioral assays to include greater distances and the entire sequence of searching and feeding behaviors, would allow for better assessment of how manipulation might actually impact transmission. Such assays have already been used to study host-seeking in uninfected mosquitoes [29], [30][31].
Natural combinations of relevant hosts and parasites
The evidence for behavioral manipulation comes from several vector parasite combinations, but none conducted simultaneously, making it difficult to know whether systems differ or if results lack repeatability. For example, one study found stage-specific changes in the feeding behavior of An. stephensi infected with P. yoelii [7], while another found no effect when the same vector species was infected with P. berghei [12]. It is not clear if these differences are due to species combination, intensity of infection [32], experimental conditions, or had truly disparate outcomes. Extending assays to human parasites and relevant malaria vectors is a key next step in investigating manipulation. Including natural and artificial vector-parasite pairings in the same experiments would enable us to determine which systems, if any, provide robust models for human malaria.
Exploring effects beyond the flying syringe
While the number of infectious bloodmeals a mosquito takes has the most direct link to parasite transmission, other aspects of mosquito biology highly relevant to malaria epidemiology [33] might also be altered by the parasite. Malaria parasites impact mosquito fecundity [18], [34–38], but we know of no studies investigating whether there are additional effects on, for example, the length of gonotrophic cycle. If Plasmodium infection changes the duration and number of gonotrophic cycles, transmission dynamics could be altered through the frequency of blood feeding and any associated mortality
Malaria infection could also alter mosquito dispersal, an important component of transmission dynamics [39]. There is some evidence that P. cynomolgi [40] and P. yoelii [41] infection reduces the flight performance of An. stephensi. We know of no data on the flight capacity of mosquitoes infected with human malaria parasites. More broadly, do malaria parasites affect decisions vectors make about which hosts to feed on? Several studies have reported that infected vertebrate hosts are most attractive during transmissible stages of infection [42-43]. In addition to effecting choices mosquitoes make within vertebrate host species, malaria parasites could also affect decisions on feeding between species. The degree of anthrophily is a key determinant of malaria epidemiology. Again we know of no relevant data but it is an intriguing possibility that malaria infection might alter host preference; an effect that might be particularly important for the vectorial capacity of mosquito species which tend to be naturally more zoophilic.
Finding a mechanism
Across the many host-parasite systems where there is indisputable evidence of manipulation, the mechanisms by which parasites alter host behavior are not well understood [44]. The mosquito-malaria system is no exception. One possibility is that infection interferes with the mosquito’s ability to imbibe blood. The activity of apyrase, a key enzyme involved in feeding efficiency, has been shown to be reduced in sporozite-infected females[8]. This reduced activity was associated with fine lesions in the salivary glands. Infection also affects the expression of salivary proteins [45].
Malaria parasites might also manipulate the satiation threshold, so that infected females take smaller and more frequent blood meals [6]. The head proteome of sporozoite-infected females differs from uninfected females [46]. Hairworms that manipulate the behavior of crickets have been found to produce molecules that may act directly on the cricket central nervous system and proteomic changes can be detected in cricket hosts during manipulation [47], [48]. Similar studies looking at the mechanisms by which human malaria parasites manipulate their vectors could identify interesting new targets for control.
Concluding remarks
Several studies suggest that malaria parasites manipulate mosquito behavior to facilitate transmission, but the nature and extent of the phenomenon remains unclear. Without transmission data, it is formally possible that these behavioral alterations could be side-effects of infection that do not increase transmission. Changes in mosquito behavior following parasite invasion could be a pathological consequence of infection, or a manifestation of the mosquito immune response to infection, or an interaction between the two [49]. Even if behavioral differences are not the direct result of manipulation, they are still relevant to our understanding of transmission ecology. ITNs are central to contemporary malaria control [50], and their efficacy depends on the patterns of mosquito feeding behavior and the resultant mortality [51]. If malaria alters feeding behavior, then infected mosquitoes might interact with ITNs differently. Understanding whether these differences exist and if they do, the mechanisms that underlie them, could allow us to use this powerful control tool even more effectively. Moreover, if infected mosquitoes do behave differently, it might be possible to develop novel control tools to exploit this altered behavior. If oocyst-infected females are less likely to blood-feed, for example, then strategies which target sugar feeding [52], or resting sites might lead to larger than expected benefits in terms of malaria control. More speculatively, determining the molecular and physiological mechanisms responsible for changes in mosquito behavior could lead to novel genetic, chemical or semio-chemical control strategies to target infected mosquitoes, possibly even ‘manipulating the manipulation’. After more than 100 years since it was confirmed that mosquitoes transmit malaria, it simply should not be an open question whether human parasites manipulate the behavior of their mosquito hosts.
Figure 1. The effect of manipulation on transmission.
The effect of increased number of bites per attempt (different colored bars) and the probability that a female feeds in a pre-infectious cycle (x-axis) on the force of malaria infection. For the left panel, daily mortality is assumed to be the most important source of mortality; in the right panel, mortality is assumed to be almost entirely feeding-associated. The dashed line indicates force of infection for unmanipulated females that always feed during the pre-infectious cycle and bite one person per feeding attempt. These two mortality extremes illustrate the interactions between mortality distribution and manipulation phenotypes. When mortality is evenly distributed through the feeding cycle and not associated with the feeding event, the biggest increase in force of infection comes from the number of bites per attempt (the differences between different colored bars). When mortality is attributed to feeding, the biggest increases in relative force of infection are mediated by the decreased mortality experienced by females in the oocyst-stage.
Acknowledgements
This work was supported by a NIH-NIAID ICEMR award (#U19AI089676).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Moore J. Parasites and the behavior of animals. Oxford University Press; 2002. [Google Scholar]
- 2.Evans HC. Entomogenous fungi in tropical forest ecosystems: an appraisal. Ecol. Entomol. 1982;7:47–60. [Google Scholar]
- 3.Rasmussen E. Behaviour of sacculinized shore crabs (Carcinus maenas Pennant) Nature. 1959;183:479–480. [Google Scholar]
- 4.Thomas F, et al. Do hairworms (Nematomorpha) manipulate the water seeking behaviour of their terrestrial hosts? J. Evolution. Biol. 2002;15:356–361. [Google Scholar]
- 5.Schwartz A, Koella JC. Trade-offs, conflicts of interest, and manipulation in Plasmodium-mosquito interactions. Trends Parasitol. 2001;17:189–194. doi: 10.1016/s1471-4922(00)01945-0. [DOI] [PubMed] [Google Scholar]
- 6.Koella JC, et al. Stage-specific manipulation of a mosquito’s host-seeking behavior by the malaria parasite Plasmodium gallinaceum. Behav. Ecol. 2002;13:816–820. [Google Scholar]
- 7.Anderson RA, et al. The effect of Plasmodium yoelii nigeriensis infection on the feeding persistence of Anopheles stephensi Liston throughout the sporogonic cycle. Proc. Roy. Soc. B. 1999;266:1729–1733. doi: 10.1098/rspb.1999.0839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rossignol PA, et al. Increased intradermal probing time in sporozoite-infected mosquitoes. Am. J. Trop. Med. Hyg. 1984;33:17–20. doi: 10.4269/ajtmh.1984.33.17. [DOI] [PubMed] [Google Scholar]
- 9.Ponnudurai T, et al. Feeding behaviour and sporozoite ejection by infected Anopheles stephensi. T. Roy. Soc. Trop. Med. Hyg. 1991;85:175–180. doi: 10.1016/0035-9203(91)90012-n. [DOI] [PubMed] [Google Scholar]
- 10.Wekesa JW, et al. Effect of Plasmodium falciparum on blood feeding behavior of naturally infected Anopheles mosquitoes in western Kenya. Am. J. Trop. Med. Hyg. 1992;47:484–488. doi: 10.4269/ajtmh.1992.47.484. [DOI] [PubMed] [Google Scholar]
- 11.Hogg JC, Hurd H. Malaria-induced reduction of fecundity during the first gonotrophic cycle of Anopheles stephensi mosquitoes. Med. Vet. Ent. 1995;9:176–180. doi: 10.1111/j.1365-2915.1995.tb00175.x. [DOI] [PubMed] [Google Scholar]
- 12.Li X, et al. Probing behaviour and sporozoite delivery by Anopheles stephensi infected with Plasmodium berghei. Med. Vet. Ent. 1992;6:57–61. doi: 10.1111/j.1365-2915.1992.tb00036.x. [DOI] [PubMed] [Google Scholar]
- 13.Bockarie MJ, Dagoro H. Are insecticide-treated bednets more protective against Plasmodium falciparum than Plasmodium vivax-infected mosquitoes? Malaria J. 2006;5:15. doi: 10.1186/1475-2875-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koella JC, et al. The malaria parasite, Plasmodium falciparum, increases the frequency of multiple feeding of its mosquito vector, Anopheles gambiae. Proc. Roy. Soc. B. 1998;265:763–768. doi: 10.1098/rspb.1998.0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson RA, et al. Plasmodium falciparum sporozoites increase feeding-associated mortality of their mosquito hosts Anopheles gambiae sl. Parasitology. 2000;120:329–333. doi: 10.1017/s0031182099005570. [DOI] [PubMed] [Google Scholar]
- 16.Lindsay SW, et al. Malaria in a peri-urban area of The Gambia. Ann. Trop. Med. Parasitol. 1990;84:553–562. doi: 10.1080/00034983.1990.11812510. [DOI] [PubMed] [Google Scholar]
- 17.Koella JC, et al. Malaria parasites enhance blood-feeding of their naturally infected vector Anopheles punctulatus. Parasitology. 1996;113:105–110. doi: 10.1017/s0031182000066348. [DOI] [PubMed] [Google Scholar]
- 18.Ferguson HM, et al. The influence of malaria parasite genetic diversity and anaemia on mosquito feeding and fecundity. Parasitology. 2003;127:9–19. doi: 10.1017/s0031182003003287. [DOI] [PubMed] [Google Scholar]
- 19.Friend WG, Smith JJB. Factors affecting feeding by bloodsucking insects. Annu. Rev. Entomol. 1977;22:309–331. doi: 10.1146/annurev.en.22.010177.001521. [DOI] [PubMed] [Google Scholar]
- 20.Smith DL, et al. Ross, MacDonald, and a theory for the dynamics and control of mosquito-transmitted pathogens. PLos Path. 2012;8:e1002588. doi: 10.1371/journal.ppat.1002588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Macdonald G, et al. The Epidemiology and Control of Malaria. Oxford University Press; 1957. [Google Scholar]
- 22.Russell TL, et al. Impact of promoting longer-lasting insecticide treatment of bed nets upon malaria transmission in rural Tanzanian setting with pre-existing high coverage of untreated nets. Malar. J. 2010;9:187. doi: 10.1186/1475-2875-9-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burkot TR, et al. Human malaria transmission studies in the Anopheles punctulatus complex in Papua New Guinea: sporozoite rates, inoculation rates, and sporozoite densities. Am. J. Trop. Med. Hyg. 1988;39:135–144. doi: 10.4269/ajtmh.1988.39.135. [DOI] [PubMed] [Google Scholar]
- 24.Killeen GF, et al. A simplified model for predicting malaria entomologic inoculation rates based on entomologic and parasitologic parameters relevant to control. Am. J. Trop. Med. Hyg. 2000;62:535–544. doi: 10.4269/ajtmh.2000.62.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saul AJ, et al. A cyclical feeding model for pathogen transmission and its application to determine vectorial capacity from vector infection rates. J Appl. Ecol. 1990:123–133. [Google Scholar]
- 26.Smith D, McKenzie FE. Statics and dynamics of malaria infection in Anopheles mosquitoes. Malaria J. 2004;3:13. doi: 10.1186/1475-2875-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sandip M, et al. Mathematical models of malaria-a review. Malaria J. 2011;10:202. doi: 10.1186/1475-2875-10-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koella JC, et al. Towards evolution-proof malaria control with insecticides. Evol. Appl. 2009;2:469–480. doi: 10.1111/j.1752-4571.2009.00072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Verhulst NO, et al. Differential attraction of malaria mosquitoes to volatile blends produced by human skin bacteria. PloS One. 2010;5:e15829. doi: 10.1371/journal.pone.0015829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Verhulst NO, et al. Structural design affects entry response of mosquitoes in olfactometers. Proc. Neth. Entomol. Soc. 2008;19:129–136. [Google Scholar]
- 31.Takken W. The role of olfaction in host-seeking of mosquitoes: a review. Int. J. Trop. Insect. Sci. 1991;12:287–295. [Google Scholar]
- 32.Billingsley PF, et al. Relationship between prevalence and intensity of Plasmodium falciparum infection in natural populations of Anopheles mosquitoes. Am. J. Trop. Med. Hyg. 1994;51:260–270. doi: 10.4269/ajtmh.1994.51.260. [DOI] [PubMed] [Google Scholar]
- 33.Ferguson HM, et al. Ecology: a prerequisite for malaria elimination and eradication. PLoS medicine. 2010;7:e1000303. doi: 10.1371/journal.pmed.1000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hacker CS, Kilama WL. The relationship between Plasmodium gallinaceum density and the fecundity of Aedes aegypti. J. Invertebr. Pathol. 1974;23:101–105. doi: 10.1016/0022-2011(74)90079-2. [DOI] [PubMed] [Google Scholar]
- 35.Freier JE, Friedman S. Effect of host infection with Plasmodium gallinaceum on the reproductive capacity of Aedes aegypti. J. Invertebr. Pathol. 1976;28:161–166. doi: 10.1016/0022-2011(76)90117-8. [DOI] [PubMed] [Google Scholar]
- 36.Hogg JC, Hurd H. The effects of natural Plasmodium falciparum infection on the fecundity and mortality of Anopheles gambiae s.l. in north east Tanzania. Parasitology. 1997;114:325–331. doi: 10.1017/s0031182096008542. [DOI] [PubMed] [Google Scholar]
- 37.Jahan N, Hurd H. Effect of Plasmodium yoelii nigeriensis (Haemosporidia: Plasmodiidae) on Anopheles stephensi (Diptera: Culicidae) vitellogenesis. J. Med. Ent. 1998;35:956–961. doi: 10.1093/jmedent/35.6.956. [DOI] [PubMed] [Google Scholar]
- 38.Gray EM, Bradley TJ. Malarial infection in Aedes aegypti: effects on feeding, fecundity and metabolic rate. Parasitology. 2006;132:169–176. doi: 10.1017/S0031182005008966. [DOI] [PubMed] [Google Scholar]
- 39.Depinay JMO, et al. A simulation model of African Anopheles ecology and population dynamics for the analysis of malaria transmission. Malaria J. 2004;3:29. doi: 10.1186/1475-2875-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schiefer BA, et al. Ward RA, Eldridge BF. Plasmodium cynomolgi: effects of malaria infection on laboratory flight performance of Anopheles stephensi mosquitoes. Exp.Parasitol. 1977;41:397–404. doi: 10.1016/0014-4894(77)90111-4. [DOI] [PubMed] [Google Scholar]
- 41.Rowland M, Boersma E. Changes in the spontaneous flight activity of the mosquito Anopheles stephensi by parasitization with the rodent malaria Plasmodium yoelii. Parasitology. 1998;97:221–227. doi: 10.1017/s003118200005842x. [DOI] [PubMed] [Google Scholar]
- 42.Lacroix R, et al. Malaria infection increases attractiveness of humans to mosquitoes. PLos Biology. 2005;3:e298. doi: 10.1371/journal.pbio.0030298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ferguson HM, Read AF. Mosquito appetite for blood is stimulated by Plasmodium chabaudi infections in themselves and their vertebrate hosts. Malaria J. 2004;3:12. doi: 10.1186/1475-2875-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Poulin R. Parasite Manipulation of Host Behavior: An Update and Frequently Asked Questions. Adv. Stud. Behav. 2010;41:151–186. [Google Scholar]
- 45.Shandilya S, et al. Plasmodium infection-induced changes in salivary gland proteins of the malaria vector Anopheles stephensi (Diptera: Culicidae) Jpn. J. Infect. Dis. 1999;52:214–216. [PubMed] [Google Scholar]
- 46.Lefevre T, et al. Malaria Plasmodium agent induces alteration in the head proteome of their Anopheles mosquito host. Proteomics. 2007;7:1908–1915. doi: 10.1002/pmic.200601021. [DOI] [PubMed] [Google Scholar]
- 47.Biron DG, et al. Behavioural manipulation in a grasshopper harbouring hairworm: a proteomics approach. Proc. Roy. Soc. B. 2005;272:2117–2126. doi: 10.1098/rspb.2005.3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Biron DG, et al. ‘Suicide’of crickets harbouring hairworms: a proteomics investigation. Insect Mol. Biol. 2006;15:731–742. doi: 10.1111/j.1365-2583.2006.00671.x. [DOI] [PubMed] [Google Scholar]
- 49.Koella JC. Malaria as a manipulator. Behav. Process. 2005;68:271–273. doi: 10.1016/j.beproc.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 50.World Health Organization World Malaria Report 2011. 2011 ( http://www.who.int/malaria/world_malaria_report_2011)
- 51.Le Menach A, et al. An elaborated feeding cycle model for reductions in vectorial capacity of night-biting mosquitoes by insecticide-treated nets. Malaria J. 2007;6:10. doi: 10.1186/1475-2875-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Müller GC, et al. Successful field trial of attractive toxic sugar bait (ATSB) plant spraying methods against malaria vectors in the Anopheles gambiae complex in Mali, West Africa. Malaria J. 2010;9:210. doi: 10.1186/1475-2875-9-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Afrane YA, et al. Effects of microclimatic changes caused by land use and land cover on duration of gonotrophic cycles of Anopheles gambiae (Diptera:Culicidae) in western Kenyan highlands. J. Med Entomol. 2005;42:974–980. doi: 10.1093/jmedent/42.6.974. [DOI] [PubMed] [Google Scholar]
- 54.World Health Organization . Manual of practical entomology in malaria. Offset Publications; 1975. [Google Scholar]
- 55.Kiszewski A, et al. A global index representing the stability of malaria transmission. Am. Trop. Med. Hyg. 2004;70:486–498. [PubMed] [Google Scholar]