Abstract
Objective
In addition to increased risks for aneurysm-related death, previous studies have determined that all-cause mortality in abdominal aortic aneurysm (AAA) patients is excessive and equivalent to that associated with coronary heart disease (CHD). These studies largely preceded the current era of CHD risk factor management, however, and no recent study has examined contemporary mortality associated with early AAA disease (aneurysm diameter between 3 and 5 cm). As part of an ongoing natural history study of AAA, we report the mortality risk associated with presence of early disease.
Methods
Participants were recruited from three distinct health care systems in Northern California between 2006 and 2011. Aneurysm diameter, demographic information, co-morbidities, medication history, and plasma for biomarker analysis were collected at study entry. Survival status was determined at follow-up. Data were analyzed with t- or chi-square tests where appropriate. Freedom from death was calculated via Cox proportional hazards modeling; the relevance of individual predictors on mortality was determined by log-rank test.
Results
The study enrolled 645 AAA patients; age 76.4 +/− 8.0 years, aortic diameter 3.86+/− 0.7 cm. Participants were mostly male (88.8%) not current smokers (81.6%) and taking statins (76.7%). Mean follow-up was 2.1 +/− 1.0 years. Estimated 1- and 3-year survival was 98.2% and 90.9%, respectively. Factors independently associated with mortality included larger aneurysm size (HR 2.12, 95% CI 1.26 – 3.57 for diameter >4.0 cm) and diabetes (HR 2.24, 95% CI 1.12 – 4.47). After adjusting for patient-level factors, health care system independently predicted mortality.
Conclusion
Contemporary all-cause mortality for patients with early AAA disease is lower than that previously reported. Further research is warranted to determine important factors that contribute to imporved survival in early AAA disease.
INTRODUCTION
Abdominal aortic aneurysms (AAA) remain a significant health concern in industrialized countries, with an estimated prevalence of 5% of men and 1% of women over age 65. In the United States approximately 15,000 yearly deaths are attributable to ruptured AAA. In addition to aneurysm-related death and morbidity, prospective studies have shown that individuals with AAA greater than 3.0 cm in diameter have a two-fold increase in 5-year mortality compared with controls (65.1 vs. 32.8 deaths per 1000 person-years)1, 2. In a 10-year follow-up study AAAs continued to be associated with a higher risk of total mortality (hazard ratio 1.44, 95% confidence interval 1.25 to 1.66) and incident cardiovascular events (hazard ratio 1.52, 95% confidence interval 1.25 to 1.85)3. Current evidence suggests that increased mortality is secondary to increased cardiovascular events, and published guidelines consider AAA to be a coronary heart disease (CHD) equivalent4.
Death from rupture occurs in only a small percentage of those with AAA, and it is generally accepted that cardiovascular risk factor modification should be paramount in the overall management of these patients. No study has examined contemporary mortality with early AAA disease in the current era of CHD risk factor management. The goals of this study were to report the mortality associated with early disease, and to identify factors associated with decreased mortality.
METHODS
Participant Recruitment and Enrollment
Study recruitment and enrollment was conducted through the National Institutes of Health Specialized Center of Clinically Oriented Research (SCCOR) Program on AAA disease at Stanford University. The Stanford SCCOR was a prospective, longitudinal study of AAA disease conducted in the San Francisco Bay Area between 2006 and 2011. Participants were recruited from three participating health care systems: an academic medical center (Stanford University Medical Center), a government-sponsored medical center (Veterans Affairs Palo Alto Health Care System) and a private integrated medical system (Kaiser Permanente of Northern California). Inclusion criteria for study participation were 1) male or female patients with infra-renal abdominal aortic diameter greater than 3 cm and less than 5.5 cm in diameter at baseline and 2) age 50 or older. Potential participants were identified from medical record review, and permission was obtained from the participant’s primary care physician was obtained before initiating contact. Patients with known connective tissue disorders such as Ehlers-Danlos or Marfan’s syndrome(s) were excluded.
Protocol and Data Collection
Study protocol for all participants in the SCCOR study included informed consent, extraction of medical history and drug information from medical records and completion of questionnaires regarding health history, and physical examination. Aortic diameter measurement was obtained via transabdominal ultrasound, and plasma and buffy coat was collected for biomarkers and genomic studies. Survival status and cause of death was determined by follow-up visits, phone calls, or review of medical records and through the Social Security Death Index. The protocol and consent forms were approved in advance by the Stanford University/VA Palo Alto Health Care System Institutional Review Board (IRB), the Kaiser Division of Research IRB and a NIH-appointed, SCCOR-specific Data Safety Monitoring Board.
Data Analysis
Descriptive statistics were calculated on baseline demographic data, co-morbidities, medication history, smoking variables and clinical labs, and are represented as means (SD) or percentages. Bivariate analysis was conducted on variables associated with survival using t- or chi-square tests where appropriate. Survival was estimated with life-table analysis. The association of individual variables with survival was determined by log-rank test. Cox proportional hazards models were then constructed with significant variables of interest to determine independent predictors of survival. Models were stratified by institution to adjust for unmeasured institutional variables that may have affected survival.
Reported survival of our cohort was compared with estimated survival based on US Population Vital Statistics5. Each patient’s predicted one-, two- and three-year survival was calculated using US Life Tables adjusted by age, gender, and ethnicity. Mean overall estimated survival of the cohort was then calculated with standard descriptive statistics. Data analysis was conducted using SPSS software version PASW Statistics 18 and SAS version 9.2 (Cary, N.C.). Statistical significance was determined at the level of p < .05.
RESULTS
A total of 634 patients with small AAA were enrolled in the study.. Mean participant age was 76.4 +/− 8.0 years. Mean aortic diameter was 3.86 +/− 0.6 cm. Mean body mass index (BMI) was 28.6 +/− 5.0, waist circumference was 39.8 +/− 5.1 inches. Co-morbidity is shown in TABLE 1. Hypercholesterolemia was noted in 86.0% of subjects; 77.0% were taking statin medications. Of those on statins, an LDL of less than 100 mg/dl was achieved in 80.5%. One fourth of patients had diabetes. Of those, 39.1% were diet-controlled, 56.3% were managed with oral hypoglycemic agents, and 5.6% with insulin. Mean hemoglobin A1c (HgA1c) for those with diabetes was 6.1 +/− 1.1 mg/dl.
Table 1.
Demographics
| Variable | Total (n=634) | PIMS (n=456) | AMC (n=85) | GSMC (n=93) | p-value |
|---|---|---|---|---|---|
| Age in years (mean, s.d.) | 76.4 (8.0) | 76.1 (7.9) | 77.1 (8.4) | 77.3 (7.8) | 0.27 |
| Caucasian Race | 81.9 | 81.4 | 82.4 | 83.9 | 0.84 |
| Male gender | 88.8 | 87.1 | 87.1 | 98.9 | 0.004 |
| Body Mass Index (mean, s.d.) | 28.6 (5.0) | 28.7 (5.0) | 27.9 (5.0) | 29.4 (4.7) | 0.007 |
| Baseline AAA Diameter in cm (mean, s.d.) | 3.86 (0.62) | 3.84 (0.6) | 3.88 (0.6) | 3.91 (0.6) | 0.53 |
| Medical History | |||||
| Family History of AAA | 14.2 | 12.6 | 14.1 | 22.6 | 0.04 |
| Coronary Artery Disease | 43.6 | 43.5 | 36.5 | 50.5 | 0.17 |
| Cardiomyopathy | 6.2 | 6.8 | 1.2 | 7.6 | 0.12 |
| Pulmonary Disease | 41.0 | 40.6 | 43.5 | 40.2 | 0.87 |
| Peripheral Arterial Disease | 24.6 | 26.2 | 10.6 | 29.7 | 0.004 |
| Diabetes | 26.1 | 23.9 | 21.2 | 40.9 | 0.002 |
| Dyslipidemia | 86.0 | 86.7 | 71.8 | 95.8 | <0.0001 |
| Hypertension | 82.8 | 83.8 | 72.9 | 87.1 | 0.03 |
| Medications | |||||
| Statins | 77.0 | 77.4 | 63.5 | 87.1 | 0.001 |
| ACE Inhibitor or ARB | 53.3 | 51.3 | 56.5 | 60.2 | 0.24 |
| Beta Blockers | 56.3 | 59..9 | 45.9 | 48.4 | 0.02 |
| Insulin use among diabetics | 5.6 | 2.8 | 5.6 | 13.2 | .06 |
| Smoking | |||||
| Current Smoker | 18.4 | 17.8 | 16.7 | 22.6 | 0.50 |
| Ever Smoker | 84.1 | 84.8 | 74.2 | 89.3 | 0.02 |
| Laboratory Values | |||||
| LDL | 92.4 (31.8) | 92.8 (32.0) | 97.4 (35.4) | 85.6 (26.1) | 0.05 |
| HgA1C (those with diabetes) | 6.8 (1.5) | 6.9 (1.7) | 6.5 (0.6) | 6.6 (0.7) | 0.61 |
Numbers are percentages unless otherwise noted. PIMS: private integrated medical system, AMC: academic medical center; GSMC: government-sponsored medical center; ARB: angiotensin receptor blocker; LDL: low density lipoprotein; HgA1C: hemoglobin A1C; s.d.: standard deviation
Of the entire cohort, 59.8% had an aortic diameter between 3.0 cm – 3.99 cm inclusive. A majority of participants were men (88.8%). Subjects with ≥ 4.0 cm aneurysms were more likely to carry concomitant diagnoses of cardiomyopathy (9.5% vs.4.3%, p=0.01), coronary artery disease (48.6% vs. 40.7%, p=0.05), and were more commonly on statin medication (79.5% vs. 74.9%, p=0.03). Demographics were similar across participating institutions, though VA participants were more likely to have diabetes, dyslipidemia, or a family history of AAA (TABLE 1).
Mean follow-up was 25.2 +/− 12 months (range 1 – 51 months). During follow-up 51 (8.0%) patients underwent AAA repair for clinical indications. Death occurred in 35 subjects during the study period. Cardiovascular disease was the cause of death in 37%, other disease was the cause in 43%, and the cause in 20% was unknown (TABLE 2). Mean AAA diameter of those with unknown cause of death was no different than for those with a known cause of death (3.8 cm vs. 4.2 cm, p=0.2). Two AAA-related deaths occurred, both after repair.
Table 2.
Causes of Death
| Cause | Deaths, (%) N=35 |
|---|---|
| Cancer | 9 (26) |
| Cardiovascular | 13 (37) |
| Acute Myocardial Infarction | 3 |
| AAA | 2 |
| Ischemic Heart Disease | 4 |
| Stroke | 3 |
| Other cardiovascular | 1 |
| Other | 6 (17) |
| Unknown | 7 (20) |
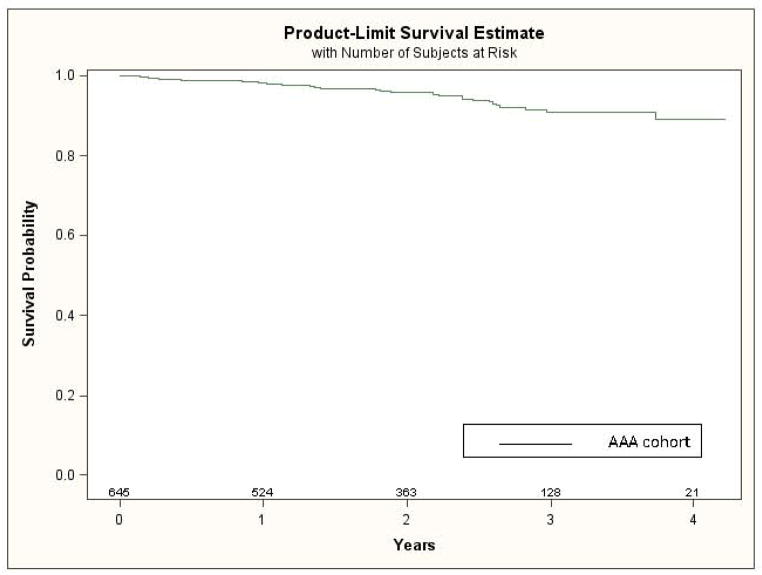
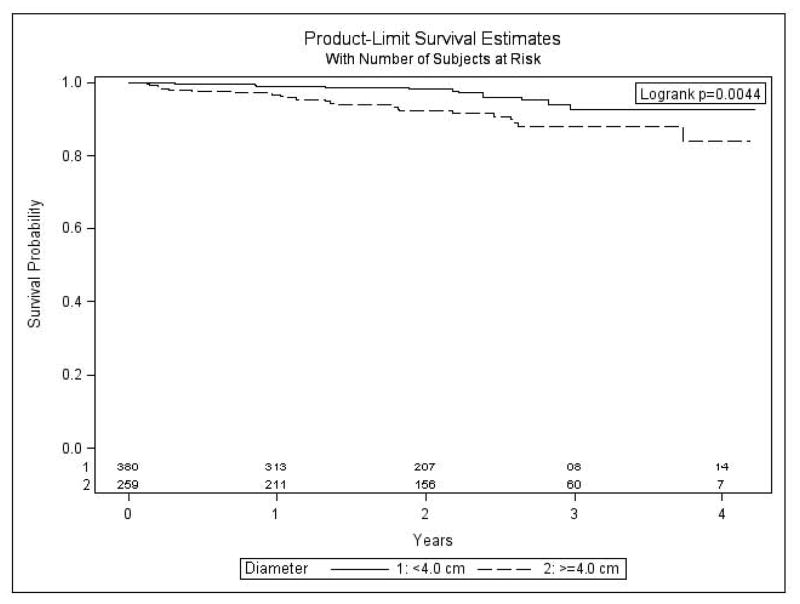
Survival by life-table analysis is shown in figure 1 and summarized in table 3. Overall estimated 1-year survival was 98.2% and estimated 3-year survival was 90.9%. Based on US Life Table analysis, the estimated 1-year and 3-year survival of our cohort was 93.8% and 81.5% respectively. Patients with aneurysms 3.0 – 3.9 cm had improved survival compared with AAA ≥ 4.0 cm (figure 2, p=0.004). Estimated 3-year survival for AAA <4.0 cm was 92.7%, while that for AAA ≥ 4.0 cm was 88.0% (table 4). Improved survival was also associated with absence of diabetes (p=0.005, log rank test), with estimated 3-year survival for those with and without diabetes of 83.0% and 93.7% respectively (table3). Institutional differences in overall all-cause mortality also were present (p=0.01, log rank test). Of note, survival was not affected by age (p=0.10), gender (p=0.47), coronary heart disease (p=0.14), COPD (p=0.72), cardiomyopathy (p=0.07), dyslipidemia (p=0.27), statin use (p=0.81), hypertension (p=0.53), hypertension management (p=0.77), or smoking status (p=0.66) (log rank test).
Figure 1. Overall estimated survival.
Number at risk includes those alive who were not lost to follow-up.
Table 3.
Survival Comparison
| Time period | Observed Cohort* (95% CI) | Estimate of Cohort† (95% CI) |
|---|---|---|
| 1-year | 98.2% (96.8% – 99.0%) | 93.8% (93.5% – 94.1%) |
| 2-year | 95.8% (93.7% – 97.2%) | 87.6% (87.0% – 88.2%) |
| 3-year | 90.9% (87.0% – 93.7%) | 81.5% (80.6% – 82.4%) |
Kaplan-Meier Method
Estimate based on 2006 National Vital Statistics and adjusted for age, sex, and ethnicity
CI: confidence interval
Figure 2. Survival by aneurysm size.
Number at risk includes those alive who were not lost to follow-up.
Table 4.
Predictors of survival
| Variable* (n) | Total deaths | Estimated 1-year survival | Estimated 3-year survival | Unadjusted HR (95% CI) | Adjusted HR† |
|---|---|---|---|---|---|
| Aneurysm size | |||||
| AAA < 4.0 cm (386) | 23 | 90.1% | 92.7% | 1.0 (referent) | |
| AAA ≥ 4.0 cm (248) | 12 | 96.8% | 88.0% | 2.66 (1.32 – 5.35) | 2.12 (1.26 – 3.57) |
| Diabetes (162) | 16 | 96.8% | 83.0% | 2.34 (1.19 – 4.60) | 2.24 (1.12 – 4.47) |
PIMS: private integrated medical system, AMC: academic medical center; GSMC: government-sponsored medical center
stratified by institution; adjusted for age, AAA diameter, diabetes
Aneurysm diameter and diabetes remained Independent predictors of mortality by Cox regression analysis, and are summarized in table 4. After adjusting for institution and age, the relative hazard of death for those with AAA ≥ 4.0 cm was 2.12 (95% CI 1.26 – 3.57) compared with those with AAA < 4.0 cm. Adjusted hazard of death for those with diabetes was 2.24 (95% CI 1.12 – 4.47) compared with non-diabetics.
DISCUSSION
Our study is the first prospective U.S. study in the era of cardiovascular risk management to report all-cause mortality for patients with small AAA. We have shown that patients with small AAA can achieve comparable survival to the population at large, a finding that challenges earlier studies showing that patients with small AAA have up to a 73% increased risk of all-cause mortality compared with those without AAA2. Our cohort was similar to others with respect to diabetes, coronary artery disease, peripheral arterial disease, and hypertension1, 2. This comparison suggests that comprehensive cardiovascular risk management may be a key reason behind this favorable survival.
A number of factors may have contributed to our findings. Compared with prior research1, a much lower proportion of participants in our study (18.4%) were current smokers. California also has one of the lowest rates of adult cigarette smokers in the nation. Active smoking has been linked to an increase in both aneurysm rupture and all-cause mortality6–8. Although a history of smoking was present in the majority of participants, it appeared to have little influence on mortality. Smoking cessation has been shown to decrease all cause mortality compared with active smoking, although risk continues to be higher than for those who never smoked6.
Another possible contributor to survival was the high rate of statin use. Over three-fourths of patients were on statin medication, with most having achieved target LDL levels. LDL levels in our study (mean 92mg/dl) were lower than those of previous studies (mean 124 mg/dl – 130 mg/dl) 2, 3. Additionally, 76% of our cohort had reached a target of 70 mg/dl. Although we were unable to show an effect of statins on mortality, it is likely our study was underpowered to identify such an association. The effect of statins on mortality prevention has been investigated for patients with AAA, with a recent meta-analysis confirming a significant survival benefit9. Statins have not been shown, however, to decrease the need for AAA repair10, and data regarding aneurysm growth rates has been conflicting11–13, supporting the concept of systemic over local benefit in regard to AAA pathogenesis.
In our series, larger aneurysm diameters independently predicted an increased mortality risk. These findings are consistent with those of Brady and others, who suggested that AAA diameter may be a marker of progressive cardiovascular disease unrelated to traditional cardiovascular risk factors, and instead mediate mortality through other pathways14. Potential mediators have included any of a number of circulating pro-inflammatory molecules produced within the aneurysm itself, the vascular system at large, or the liver (e.g. proteolytic enzymes, chemokines, cytokines, or interleukins)15.
Even with improved survival, differences were present between referral institutions. Possible patient-level factors for this finding include differences in the severity of co-existing medical conditions, unmeasured co-morbidity, or societal factors (socioeconomic status, education) between groups. Additionally, institutional features may have also contributed to differences in survival, such as access to cardiovascular care, efficacy in screening for non-cardiovascular disease (i.e. colon cancer, prostate cancer, and tuberculosis), diabetic care management programs, and integration of health care services. Since these variables were not collected we can not speculate on the relative impact of these or other factors on survival; however, our findings suggests that a study comparing the impact on survival of differences in health care delivery systems is warranted.
The main limitations of this study are incomplete information regarding the cause of death in many of the subjects. In the absence of complete autopsy data on all participants, estimates regarding AAA-related mortality are prone to error. However, as very few aneurysms rupture at the small diameters prevalent in our trial, our findings remain relevant. Additionally, as our cohort represents a population having access to medical care who not offered participation without primary care physician approval, it is not necessarily representative of the overall population; participants in our study may have had better opportunity for general and preventative health care. These limitations do not detract from the principal finding of our study, that in the current era of cardiovascular risk management and with access to medical care the overall mortality of patients with small AAA was very low and below historical precedent.
In summary, our study has shown that with contemporary management of cardiovascular risk factors the mortality of patients with small AAA approximates that of the general population. Patients with AAA should be advised to stop smoking, and statin medications should be considered. Despite this overall improvement, mortality rates for may vary between different health care systems within the same region, suggesting that institutional factors may also contribute to survival in early AAA disease.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Forsdahl SH, Solberg S, Singh K, Jacobsen BK. Abdominal aortic aneurysms, or a relatively large diameter of non-aneurysmal aortas, increase total and cardiovascular mortality: the Tromso study. Int J Epidemiol. 2010;39(1):225–32. doi: 10.1093/ije/dyp320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Newman AB, Arnold AM, Burke GL, O’Leary DH, Manolio TA. Cardiovascular disease and mortality in older adults with small abdominal aortic aneurysms detected by ultrasonography: the cardiovascular health study. Ann Intern Med. 2001;134(3):182–90. doi: 10.7326/0003-4819-134-3-200102060-00008. [DOI] [PubMed] [Google Scholar]
- 3.Freiberg MS, Arnold AM, Newman AB, Edwards MS, Kraemer KL, Kuller LH. Abdominal aortic aneurysms, increasing infrarenal aortic diameter, and risk of total mortality and incident cardiovascular disease events: 10-year follow-up data from the Cardiovascular Health Study. Circulation. 2008;117(8):1010–7. doi: 10.1161/CIRCULATIONAHA.107.720219. [DOI] [PubMed] [Google Scholar]
- 4.Smith SC, Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113(19):2363–72. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- 5.Arias E United States Life Tables. National Vital Statistics Reports 2010. 2006. pp. 1–40. [PubMed] [Google Scholar]
- 6.Woloshin S, Schwartz LM, Welch HG. The risk of death by age, sex, and smoking status in the United States: putting health risks in context. J Natl Cancer Inst. 2008;100(12):845–53. doi: 10.1093/jnci/djn124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogot E, Murray JL. Smoking and causes of death among U.S. veterans: 16 years of observation. Public Health Rep. 1980;95(3):213–22. [PMC free article] [PubMed] [Google Scholar]
- 8.Brown LC, Powell JT. Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. UK Small Aneurysm Trial Participants. Ann Surg. 1999;230(3):289–96. doi: 10.1097/00000658-199909000-00002. discussion 96–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Twine CP, Williams IM. Systematic review and meta-analysis of the effects of statin therapy on abdominal aortic aneurysms. Br J Surg. 2010 doi: 10.1002/bjs.7343. [DOI] [PubMed] [Google Scholar]
- 10.Randomized trial of the effects of cholesterol-lowering with simvastatin on peripheral vascular and other major vascular outcomes in 20,536 people with peripheral arterial disease and other high-risk conditions. J Vasc Surg. 2007;45(4):645–54. doi: 10.1016/j.jvs.2006.12.054. discussion 53–4. [DOI] [PubMed] [Google Scholar]
- 11.Ferguson CD, Clancy P, Bourke B, Walker PJ, Dear A, Buckenham T, et al. Association of statin prescription with small abdominal aortic aneurysm progression. Am Heart J. 2010;159(2):307–13. doi: 10.1016/j.ahj.2009.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sweeting MJ, Thompson SG, Brown LC, Greenhalgh RM, Powell JT. Use of angiotensin converting enzyme inhibitors is associated with increased growth rate of abdominal aortic aneurysms. J Vasc Surg. 2010;52(1):1–4. doi: 10.1016/j.jvs.2010.02.264. [DOI] [PubMed] [Google Scholar]
- 13.Thompson AR, Cooper JA, Ashton HA, Hafez H. Growth rates of small abdominal aortic aneurysms correlate with clinical events. Br J Surg. 2010;97(1):37–44. doi: 10.1002/bjs.6779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brady AR, Fowkes FG, Thompson SG, Powell JT. Aortic aneurysm diameter and risk of cardiovascular mortality. Arterioscler Thromb Vasc Biol. 2001;21(7):1203–7. doi: 10.1161/hq0701.091999. [DOI] [PubMed] [Google Scholar]
- 15.Tedesco MM, Dalman RL. Arterial Aneurysms. In: Cronenwett JL, Johnston KW, editors. Rutherford’s Vascular Surgery. 7. Elsevier; 2010. [Google Scholar]