Abstract
Ultrasound studies are frequently requested for the work-up of patients with local elbow pain, which is generally caused by overuse syndromes, trauma, inflammatory diseases, or neuropathies. The technique used to examine this joint will vary to some extent depending on the precise location of the pain and other clinical findings. The aim of this article is to describe the standard technique used for elbow ultrasound, the normal anatomy of the joint, and the appearance on ultrasound of normal elbow anatomy and the alterations associated with some of the more common disorders affecting this joint.
Keywords: Elbow ultrasound, Elbow anatomy, Elbow injuries
Sommario
Lo studio ecografico del gomito è richiesto ed eseguito piuttosto frequentemente in pazienti con dolore localizzato, che riconosce come cause più frequenti sindromi da sovraccarico, traumi, malattie infiammatorie e neuropatie. Sebbene l'esame sia generalmente mirato alla sede del dolore, l'operatore deve essere in grado di eseguire un esame ecografico standard del gomito. Gli obiettivi dell'articolo consistono nel descrivere anatomia normale, anatomia ecografica del gomito e segni ecografici delle più comuni malattie di questa articolazione.
Introduction
Ultrasound (US) studies of the elbow are quite frequently requested by orthopedic surgeons and other physicians to obtain an accurate picture of paraarticular structures and to confirm the presence of articular disease. Standard radiographs are still the first-line approach to imaging diagnosis of these conditions: their advantages include panoramic views and the possibility to assess pathological changes involving the bones and joint. US allows low-cost, noninvasive, dynamic evaluation of paraarticular tendons and nerves as well as several joint ligaments. The most common indication for elbow US is chronic, local pain at the lateral or ulnar side of the joint. However, US can help clinicians in the assessment of a wide variety of disorders, including overuse syndromes (lateral epicondylitis, medial epicondylitis, triceps-tendon enthesopathy), traumatic changes (partial or total tendon ruptures, ligament tears, fractures, dislocation), inflammatory diseases (bursitis, arthritis), and neuropathies (ulnar or radial nerve entrapment neuropathies, nerve instability). It can also detect joint effusions (even those that are very small), synovial hypertrophy, and associated marginal joint erosions (Table 1). In selected cases of joint or bursal effusion, US can be used to guide needle placement during aspiration of synovial fluid for analysis and culture. US guidance is also useful for draining mucous cysts and administration of steroid injections. These procedures are usually more successful and less painful than those guided by palpation alone.
Table 1.
Elbow most common pathologies
| Overuse syndromes |
|
| Traumatic pathology |
|
| Inflammatory disorders |
|
| Entrapment neuropathy |
|
Basic normal anatomy
The elbow joint is composed of three communicating joints that share a common synovial membrane. The humero-ulnar joint is located between the trochlea of the humerus and the trochlear notch of the ulna. The humero-radial joint includes the capitulum of the humerus and the radial head, and the radio-ulnar joint is composed of the radial notch of the ulna and the radial head.
The synovial membrane of the elbow forms several synovial pouches, the most important of which are the anterior coronoid recess, the radial recess (located at the level of the radial neck), and the large posterior joint recess found within the olecranon fossa. The fibrous capsule is attached proximally to the medial epicondyle, the edge of the humerus above the coronoid, the radial and olecranon fossas, and the lateral epicondyle. Distally the capsule inserts into the edge of the ulnar coronoid process and annular ligament (anteriorly) and the margins of the coronoid process There are two major ligaments that stabilize the elbow joint in the coronal plane: the lateral collateral ligament, which maintains stability during varus stress, and the ulnar collateral ligament, which limits joint excursion during forced valgus stress. Synovial bursae are found within the periaarticular tissues. The olecranon bursa overlies the posterior aspect of the olecranon. It facilitates gliding of the skin over the joint during flexion and extension movements. The cubital bursa, located between the distal biceps tendon and the radial tuberosity, allows smooth tendon gliding during pronation/supination movements. The common tendon of the extensor muscles of the forearm attaches to the lateral epicondyle while the flexor muscles originate from a shorter tendon that inserts into the medial epitrochlea. The strong triceps tendon inserts into the posterior aspect of the olecranon process. At the anterior aspect of the elbow, the distal biceps brachii and brachialis tendons can be seen inserting into the radial tuberosity and the ulnar tuberosity, respectively. The humeral artery, the main vessel in the elbow region, runs through the anterior aspect of the joint, medial to the biceps tendon and lateral to the median nerve. The latter nerve passes beneath the lacertus fibrosus, an aponeurotic expansion of the biceps brachii tendon, between the two heads of the pronator teres muscles and then descends below the sublimis arcade of the flexor digitorum superficialis muscle. The ulnar nerve is located at the posteromedial aspect of the joint, where it runs inside an osteofibrous tunnel before passing between the humeral and ulnar heads of the flexor carpi ulnaris muscle. The third main nerve of the region, the radial nerve, is located at the anterolateral aspect of the joint. It divides into two terminal branches at the level of the distal humerus. The superficial sensory branch runs within the anterior portion of the joint close to the radial artery. The posterior motor branch (also known as the posterior interosseous nerve) runs posteriorly, passing between the superficial and deep portions of the supinator muscle. Injury can occur to the segment that passes below the fibrous arch formed by the proximal border of the superficial portion of the supinator muscle (arcade of Frohse).
US examination technique and normal US anatomy
The elbow joint is examined while the patient is seated with his/her arm resting on the examination table. The technique used depends to some extent on the location of the pain and other clinical findings. We will briefly describe a routine standard examination. A complete assessment of the elbow requires transverse and longitudinal images of all four aspects of the joint: posterior, medial, lateral, and anterior. The position of the patient's arm will obviously vary depending on the aspect being examined. The joint is studied in both the flexed and extended positions [1,2].
In the posterior aspect of the elbow, US reveals the superficial portion of the proximal triceps muscle and its distal tendon (including its insertion into the upper surface of the olecranon) (Fig. 1). On a deeper plane, the outline of the posterior humeral cortex and the olecranon process can be seen. The humerus presents a posterior fossa that houses the olecranon during elbow extension. This fossa contains the posterior synovial recess and the posterior fat pad (Fig. 2). Under normal conditions, no fluid is detectable within the recess. The synovial membrane cannot be visualized unless it is pathologically thickened. The olecranon bursa, which is located in the subcutaneous tissue, posterior to the olecranon, is visible on US only when it is distended by pathological effusions or when its wall is significantly thickened. Located at the posteromedial aspect of the joint, the ulnar nerve crosses the elbow region inside the cubital tunnel, which is stabilized by the Osborne ligament (Fig. 3a and b). Axial images are used to assess the location of the nerve inside the tunnel. The nerve is easy to identify thanks to its peculiar internal structure characterized by hypoechoic fascicles embedded within the hyperechoic connective tissue (epineurium and perineurium). More distal sonograms depict it running between the humeral and ulnar heads of the flexor carpi ulnaris muscle (Fig. 3c). Longitudinal US images reveal the nerve's typical fascicular appearance, but they are less informative. An essential part of the US examination is dynamic assessment of ulnar-nerve stability. Axial images are obtained over the nerve during intermittent elbow flexion and extension. Under normal conditions, neither subluxation nor anterior displacement of the nerve is seen, even when the elbow is fully flexed. In patients with anterior instability, the nerve shifts out of the tunnel (partially or completely) and into the subcutaneous soft tissues. This shift is accompanied by a snap, which can be felt by the patient as well as by the examiner. US assessment of the medial aspect of the elbow shows the proximal portion of the common flexor muscles and their attachment to the epitrochlea via a short, common tendon. In a deeper plane, the collateral ligament (which consists of three bands, anterior, posterior, and transverse, extending from medial epicondyle to the ulna) and the humero-ulnar joint can be seen (Fig. 4). On the lateral aspect of the joint, US reveals the epicondylar insertion of the common tendon of the extensor muscles, the humero-radial articulation, and the lateral collateral ligament (Fig. 5). The synovial membrane of the elbow, which forms the inner lining of the fibrous capsule, extends beneath the annular ligament around the proximal radius to form the radial recess. US of the anterior aspect of the elbow demonstrates the distal biceps tendon, which crosses the joint in a mediolateral direction to its insertion at the radial tuberosity. This tendon is quite thin and has no tendon sheath. Its proximal segment can be easily explored by US because it lies superficial to the brachialis muscle (Fig. 6). Its distal segment and its insertion can be difficult to visualize due to their deep location and anatomic complexity. High-quality US equipment is needed for reliable evaluation of these elements (Fig. 7). They are best imaged when the forearm is maintained in forced supination. The lacertus fibrosus (bicipital aponeurosis) is a flat aponeurosis that expands medially from the proximal tendon to insert into the deep fascia of the forearm. It is difficult to visualize on US. The anterior bundle containing the brachial artery and vein and the median nerve is much easier to evaluate. The nerve crosses the cubital fossa beneath the bicipital aponeurosis, running anteromedially to the brachialis muscle and medially to the biceps brachii muscle and tendon. Beneath the brachialis muscle, the anterior joint recess can be seen within the coronoid fossa. At the lateral aspect of the anterior elbow, US reveals the radial nerve lying between the brachioradialis and brachialis muscles (Fig. 8). More distal sonograms depict its distal branches: the superficial sensory branch, which continues distally passing beneath the brachioradialis muscle, and the deep motor branch (posterior interosseous nerve), which enters the posterior compartment of the forearm between the superficial and deep layers of the supinator muscle (Fig. 9). At this level, the nerve runs beneath the arcade of Frohse. The deep branch can be easily followed with sequential transverse (and also longitudinal) images (Fig. 10). However, its distal branches are hard to see due to their small caliber and the resolution limits of US.
Fig. 1.
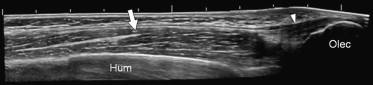
In the posterior aspect of the elbow, US depicts the superficial proximal triceps muscle (arrow), its distal tendon (arrow head) and the tendon's insertion into the upper surface of the olecranon.
Fig. 2.
On a deeper plane than that of the triceps tendon (full arrow head), US reveals the posterior fossa of the humerus, which houses the olecranon when the elbow is extended. This fossa contains the posterior synovial recess (blank arrow heads) and the posterior fat pad (star). Under normal conditions, the recess contains no visible fluid and the synovial membrane cannot be identified.
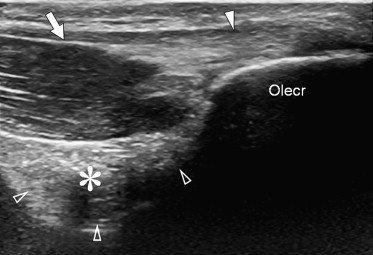
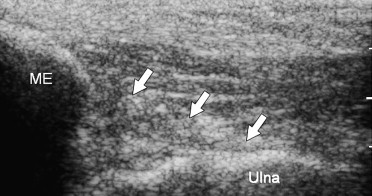
Fig. 3.
US shows the path of the ulnar nerve (black arrow) at the posteromedial aspect of the joint, both in longitudinal (a) and axial scans (b, c): the ulnar nerve crosses the elbow region inside the cubital tunnel (arrow heads) (a, b). Axial images are best for assessing the location of the nerve inside the tunnel (b). More distal sonograms depict it running between the humeral and ulnar heads of the flexor carpi ulnaris muscle (stars) (c). Longitudinal US images show the typical fascicular appearance of the nerve.
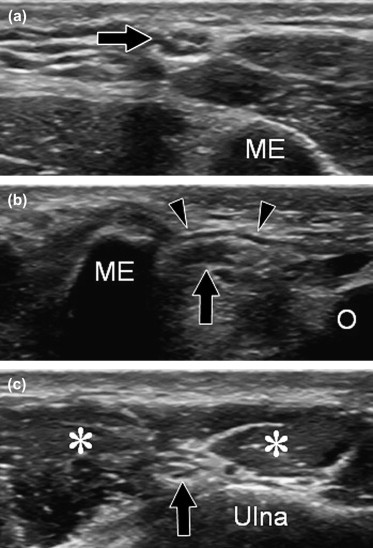
Fig. 4.

On a deeper plane, the ulnar collateral ligament (consisting of three bands) and extending from the medial epicondyle to the ulna) and the humero-ulnar joint can be seen.
Fig. 5.
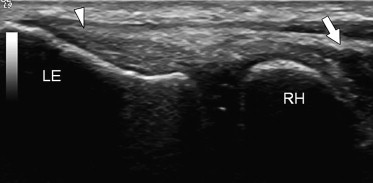
In the lateral part of the elbow, US reveals the common tendon of the extensor muscles at their insertion into the epicondyle (arrow head), the humero-radial articulation, and lateral collateral ligament.
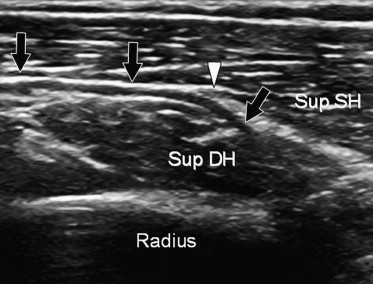
Fig. 6.
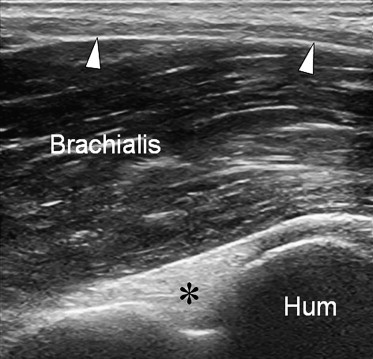
US of the anterior aspect of the elbow demonstrates the distal biceps tendon, which crosses the joint in a mediolateral direction and inserts into the radial tuberosity. Its proximal segment (arrow heads) is superficial to the brachialis muscle and can therefore be easily explored.
Fig. 7.
The distal portion of the biceps tendon and its insertion can be difficult to evaluate due to their deep location and local anatomic complexity.
Fig. 8.
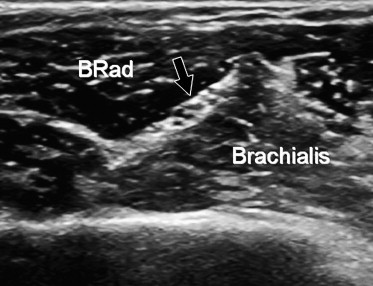
At the lateral aspect of the anterior elbow, US depicts the radial nerve (arrow) lying between the brachioradialis and brachialis muscles.
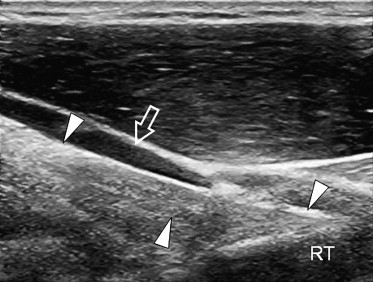
Fig. 9.
Distal sonograms reveal the distal branches of the radial nerve: the superficial sensory branch and the posterior interosseous nerve (arrows).
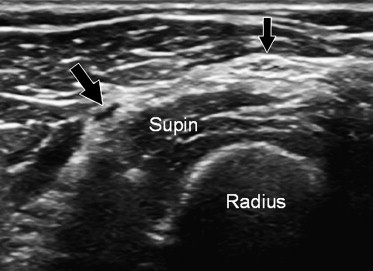
Fig. 10.
The deep branch of the radial nerve (arrows) can also be easily followed on longitudinal images. Here it enters the posterior compartment of the forearm between the superficial and deep layers of the supinator muscle.
Pathology
Tendon-overuse syndromes
Tendon-overuse syndromes (lateral epicondylitis, medial epicondylitis, triceps enthesopathy) (Figs. 11–13) can be caused by aging, microtrauma, or vascular compromise. They are frequent in athletes as well as in patients with sedentary lifestyles. Lateral epicondylitis (Fig. 11) is the most frequent and medial epicondylitis (Fig. 12) is less common. Triceps enthesopathy (Fig. 13) is described by many authors as very rare, but our experience indicates that it is relatively frequent. In all these syndromes, the most common symptom is localized pain and reduced function [3]. They are caused by noninflammatory, degenerative, angiofibroblastic changes in the tendon, which displays focal areas of myxoid and hyalin degeneration, angiofibroblastic proliferation, fibrosis, and calcifications on histological examination [4,5]. There is no evidence of inflammatory cells in either the acute or chronic stage [6].
Fig. 11.
In lateral epicondylitis, US demonstrates focal hypoechoic areas within the tendon, which are associated with loss of the normal internal fibrillar pattern (arrows). Hyperechoic areas, either related to fibrosis or calcifications, can also be detected.
Fig. 12.

In medial epicondylitis, the pathologic features are the same as those of lateral epicondylitis: focal hypoechoic areas within the tendon, which are associated with loss of the normal internal fibrillar pattern (arrows).
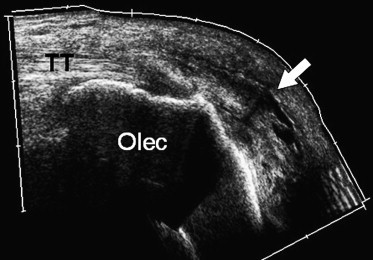
Fig. 13.
In triceps tendon enthesopathy, US shows focal hypoechoic areas within the tendon with loss of the normal internal fibrillar pattern. Hyperechoic areas reflect fibrosis or calcification at the tendon's insertion into the olecranon (arrows).
The US findings are essentially the same in all overuse syndromes: hypoechoic foci within the affected tendon (Fig. 11) are associated with loss of the normal internal fibrillar pattern. Hyperechoic areas can also be seen and are related to either fibrosis or calcification (Figs. 11–13). The tendon is frequently thickened, and there is often evidence of enthesopathy manifested by bone irregularity and small, focal calcifications [7]. Exclusion of joint effusion is a fundamental step: it rules out most intraarticular disorders and supports the diagnosis of periarticular involvement. US can be used to differentiate lateral epicondylitis from posterior interosseous nerve entrapment, chondromalacia, and osteochondritis dissecans of the humeral condyle. Medial epicondylitis can be distinguished from medial epicondyle osteophytosis or medial collateral ligament tears [8].
Traumatic pathology
The most frequent traumatic lesions of the elbow are partial or complete ruptures of tendons (Fig. 14) or ligaments (Fig. 15), cortical avulsions, fractures (Fig. 16), and dislocations.
Fig. 14.
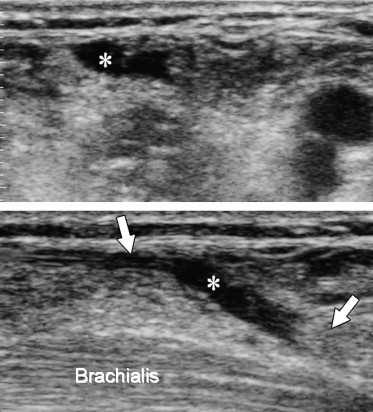
In complete tendon ruptures, US demonstrates the site of the rupture (stars), the retracted tendon stumps (arrows), and the fluid collection lying between them.
Fig. 15.
In chronic ligament disorders, US shows thickening of the ligament and hyperechoic areas corresponding to local calcifications (arrows).
Fig. 16.

US shows fragmentation and roughening of the cortical bone with avulsion of fragments (arrows) that may not be evident on plain radiographs.
Tears involving the common extensor and flexor tendons are generally seen after repeated intratendinous steroid injections for local treatment of overuse syndromes. The most frequent tendon ruptures are those involving the distal biceps brachii tendon; triceps tendon tears are less common. Total or partial ruptures of the distal biceps tendon are rarer than those of the long head of the biceps tendon at the shoulder. They generally occur in middle-aged subjects as a result of violent traction on the tendon while the elbow is flexed. In complete ruptures the clinical examination reveals swelling of the antecubital fossa related to the retracted muscle and local edema. If the lacertus fibrosus is not torn, retraction of the proximal stump may be less evident [9,10]. Clinical findings in cases of partial rupture are definitely less remarkable and specific. They are generally limited to local pain with no significant swelling. US features of complete ruptures include the absence of the tendon in the expected location and the presence of a fluid collection in the gap left by retraction of the proximal tendon stump. The stumps of the acutely ruptured tendon are surrounded by variable amounts of fluid. In the presence of subacute or chronic lesions, there may be an irregular, hypoechoic halo representing granulation tissue and fibrosis. The US findings in cases of incomplete rupture are intratendinous hypoechogenicity and tendon thinning or thickening [11]. Intrasubstance triceps ruptures are relatively rare, while tendon avulsions from the olecranon are more frequent. They occur as a result of forced extension of a flexed elbow, which can occur during a fall. The physical examination reveals a soft-tissue depression near the olecranon, and impossibility to extend the joint. The clinical diagnosis is confirmed by US demonstration of the avulsed cortical fragment, which appears as an hyperechoic fragment retracted proximally by the tendon.
Chronic ligament disorders are more frequent than acute tears. They are mainly related to repetitive microtrauma in athletes or professional activities characterized by varus or valgus overuse. The collateral ligament of the ulna, a primary stabilizer during valgus stress, is most frequently involved [11]. Lateral collateral ligament rupture is less frequent. Histological studies demonstrate microrupture, local hemorrhagic foci, ligament loosening, and partial rupture. Later, calcification and foci of ossification can be noted [12]. US shows thickening of the ligament and hyperechoic areas corresponding to local calcifications. Most avulsion injuries of the elbow region involve the medial epicondyle and are caused by trauma with excessive tension over the medial capsulo-ligamentous structures, such as that associated with falls onto an outstretched hand with the elbow in full extension. Medial epicondylar avulsion is also frequently seen with posterolateral dislocation of the elbow. In valgus stress, the medial joint space is temporarily opened, and at times the avulsed fragment is trapped within the joint [13]. In acute avulsions, US reveals local soft-tissue swelling and separation of the medial epicondyle. Fragmentation and roughening of the medial epicondyle can be found in chronic lesions [14].
Standard radiographs are indisputably the first-line imaging technique for identifying elbow fractures in a patient with acute joint trauma [13], but US can be a help when an undisplaced fracture line fails to show up on plain radiographs. In this context, US may show an intraarticular effusion suggesting the presence of a fracture extending all the way to the surface of the joint. It can also detect direct evidence of the fracture, such as cortical bone irregularity or interruption of the hyperechoic line corresponding to the bone cortex.
Inflammatory disorders
As described earlier [1], the normal paraarticular bursae of the elbow region are not visible on US because of their thin walls and the absence of significant internal fluid, but acute (Fig. 17) and chronic bursitis can both be easily detected by US. It allows clear visualization of the internal structure of the inflamed bursa, and it can also be helpful in choosing the correct treatment. Most cases of bursitis in this region involve the olecranon and cubital bursae. The former appears as a subcutaneous lump posterior to the olecranon and can be easily diagnosed clinically. The clinical diagnosis of cubital bursitis is more difficult due to the deep location of this bursa and it is frequently misdiagnosed as biceps tendinitis. US shows thickening of the bursal wall associated with an intralesional, anechoic effusion that will be more or less pronounced depending on the cause of the inflammation (microtraumatic events, infections, rheumatoid arthritis, gout).
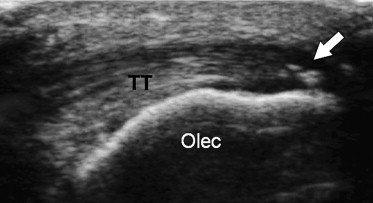
Fig. 17.
Bursitis of the elbow usually involves the olecranon bursa: US demonstrates thickening of the bursal wall with an effusion (arrow) that varies from hypo-anechoic to anechoic, depending on the cause of the inflammation.
An intraarticular effusion (Fig. 18a and b) can have a wide variety of causes, including trauma, joint inflammation, degenerative changes, and infections. On US, the effusion appears as a hypoechoic or anechoic area that fills the anterior and posterior recess and is associated with displacement of the fat pad. The annular radial recess can be also assessed for possible effusions with US. Whenever an effusion is found at US, the joint must be carefully inspected for loose bodies resulting from osteochondromatosis, osteochondral fractures, and osteochondritis dissecans, all of which are frequent in the elbow.
Fig. 18.
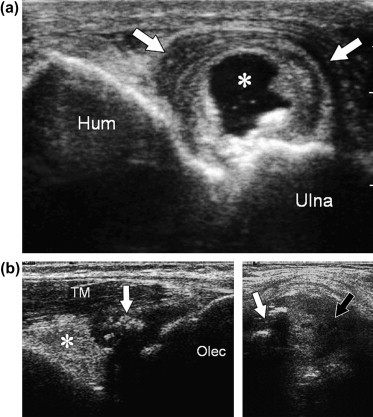
Intraarticular effusions appear as anechoic (a, star) or hypo-anechoic (b, white arrow) areas filling the anterior and posterior recesses and displacing the fat pad (b, star).
Neuropathy
The most frequent neuropathy in the elbow is caused by ulnar-nerve entrapment inside the cubital tunnel (Fig. 19). Symptoms such as numbness or tingling in the hand or fingertips and a tendency to drop objects may be the initial signs of significant abnormalities [11]. Many patients complain of paresthesia radiating from the medial aspect of the elbow to the fourth and fifth fingers. US can identify the site of constriction and the proximal swelling of the nerve, which is characterized by internal hypoechogenicity and loss of the normal fascicular appearance [15]. In every patient presenting with ulnar tunnel syndrome, nerve instability must be carefully ruled out (Fig. 20). Dynamic US scans can reveal subluxation of the ulnar nerve when the elbow is flexed even when the nerve returns to its proper place in the sulcus during joint extension.
Fig. 19.
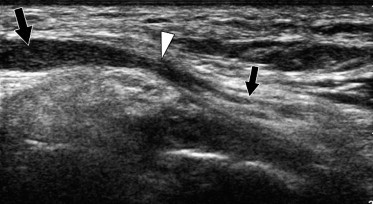
In cubital tunnel entrapment neuropathy, US shows the site of constriction (small black arrow) and proximal swelling of the nerve (large black arrow), which is characterized by internal hypoechogenicity and loss of the normal fascicular pattern (white arrow head).
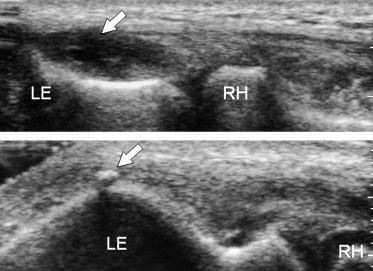
Fig. 20.
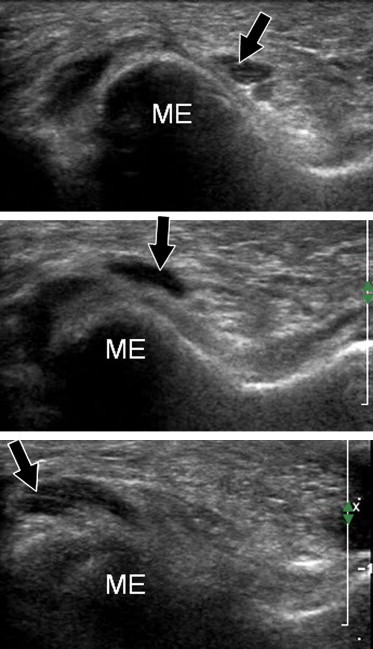
In patients with ulnar tunnel syndrome, dynamic US can reveal ulnar-nerve subluxation (black arrow) during elbow flexion. The nerve returns to its normal position in the sulcus when the joint is extended.
Compression of the posterior interosseous nerve inside the radial tunnel is usually caused by thickening of the arcade of Frohse or the presence of synovial cysts or ganglia in the radial recess [7]. Patients present with local pain, signs of radial nerve palsy, and inability to extend the wrist. Simple neurolysis of the posterior interosseous nerve with resection of the fibrous bands compressing it is generally followed by complete recovery of motor function. As in other compressive forms of neuropathy, this entrapment disorder is associated with US evidence of nerve-fiber swelling and increases in the caliber of the nerve.
Conclusions
US is an efficient diagnostic imaging tool for evaluation of the articular and paraarticular structures of the elbow. It can identify degenerative changes associated with tendon-overuse syndromes, and it plays a major role in assessing traumatic damage to tendons and/or ligaments. It is also a useful adjunct to plain radiography in the diagnosis of nondisplaced fractures. US has a major role in detection of inflammatory changes and paraarticular bursitis in the elbow. Entrapment neuropathies are also easily diagnosed using US, which can pinpoint the site of nerve compression and document the morphologic changes it provokes in the nerve.
Acknowledgments
The authors are very grateful to the Sonographic Sector of General Electric Italia for providing the scanner used to obtain images of normal anatomy during the 2006 Euroson Congress in Bologna, Italy.
References
- 1.Gruber G., Gruber G.M., Weiss C. Ultrasound examination technique of the elbow and wrist joints. Orthopade. 2002;31:262–267. doi: 10.1007/s00132-001-0249-x. [DOI] [PubMed] [Google Scholar]
- 2.Martinoli C., Bianchi S., Giovagnorio F. Ultrasound of the elbow. Skeletal Radiol. 2001;30:605–614. doi: 10.1007/s002560100410. [DOI] [PubMed] [Google Scholar]
- 3.Connell D., Burke F., Coombes P. Sonographic examination of lateral epicondylitis. AJR Am J Roentgenol. 2001;176:777–782. doi: 10.2214/ajr.176.3.1760777. [DOI] [PubMed] [Google Scholar]
- 4.Galliani I., Burattini S., Mariani A.R. Morpho-functional changes in human tendon tissue. Eur J Histochem. 2002;46:3–12. doi: 10.4081/1649. [DOI] [PubMed] [Google Scholar]
- 5.Nirschl R.P., Ashman E.S. Tennis elbow tendinosis (epicondylitis) Instr Course Lect. 2004;53:587–598. [PubMed] [Google Scholar]
- 6.Ashe M.C., McCauley T., Khan K.M. Tendinopathies in the upper extremity: a paradigm shift. J Hand Ther. 2004;17:329–334. doi: 10.1197/j.jht.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Levin D., Nazarian L.N., Miller T.T. Epicondylitis. Radiology. 2005;237:230–234. doi: 10.1148/radiol.2371040784. [DOI] [PubMed] [Google Scholar]
- 8.Martinoli C., Bianchi S., Zamorani M.P. Ultrasound of the elbow. Eur J Ultrasound. 2001;14:21–27. doi: 10.1016/s0929-8266(01)00142-2. [DOI] [PubMed] [Google Scholar]
- 9.Chew M.L., Giuffrè B. Disorders of the distal brachii biceps tendon. Radiographics. 2005;25:1227–1237. doi: 10.1148/rg.255045160. [DOI] [PubMed] [Google Scholar]
- 10.Belli P., Costantini M., Mirk P., Leone A., Pastore G., Marano P. Sonographic diagnosis of distal biceps tendon rupture: a prospective study of 25 cases. J Ultrasound Med. 2001;20:587–595. doi: 10.7863/jum.2001.20.6.587. [DOI] [PubMed] [Google Scholar]
- 11.Lyle Cain E., Jr., Dugas J.R., Wolf R.S. Elbow injuries in throwing athletes. Am J Sports Med. 2003;31:621–635. doi: 10.1177/03635465030310042601. [DOI] [PubMed] [Google Scholar]
- 12.Jarvinen M., Jozsa L., Kannus P. Histopathological findings in chronic tendon disorders. Scand J Med Sci Sports. 1997;7:86–95. doi: 10.1111/j.1600-0838.1997.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 13.Stevens M.A., El-Khoury G.Y., Khatol M.H. Imaging features of avulsion injuries. Radiographics. 1999;19:655–672. doi: 10.1148/radiographics.19.3.g99ma05655. [DOI] [PubMed] [Google Scholar]
- 14.Kessler T., Winkler H., Weiss C. Ultrasound diagnosis of elbow joint in fracture of the head of the radius. Orthopade. 2002;31:268–270. doi: 10.1007/s00132-001-0250-4. [DOI] [PubMed] [Google Scholar]
- 15.Okamoto M., Abe M., Shirai H. Diagnostic ultrasonography of the ulnar nerve in cubital tunnel syndrome. J Hand Surg (Br) 2000;25:499–502. doi: 10.1054/jhsb.1999.0350. [DOI] [PubMed] [Google Scholar]


