Abstract
Objectives.
The objective of this study was to explore the associations between openness to experience and conscientiousness, two dimensions of the five-factor model of personality, and usual gait speed and gait speed decline.
Method.
Baseline analyses were conducted on 907 men and women aged 71–82 years participating in the Cognitive Vitality substudy of the Health, Aging, and Body Composition study. The longitudinal analytic sample consisted of 740 participants who had walking speed assessed 3 years later.
Results.
At baseline, gait speed averaged 1.2 m/s, and an average decline of 5% over the 3-year follow-up period was observed. Higher conscientiousness was associated with faster initial walking speed and less decline in walking speed over the study period, independent of sociodemographic characteristics. Lifestyle factors and disease status appear to play a role in the baseline but not the longitudinal association between conscientiousness and gait speed. Openness was not associated with either initial or decline in gait speed.
Discussion.
These findings extend the body of evidence suggesting a protective association between conscientiousness and physical function to performance-based assessment of gait speed. Future studies are needed to confirm these associations and to explore mechanisms that underlie the conscientiousness mobility connection in aging adults.
Keywords: Chronic conditions, Conscientiousness, Lifestyle factors, Openness to experience, Walking speed
Maintenance of mobility in old age is an important public health as well as individual concern. With increasing age, the ability to walk independently decreases progressively and in some individuals the extent of decline compromises the capacity to live independently. Theoretical models of the disablement process suggest that personality might play a role in the development and progression of disability related to mobility. A personality that predisposes to unhealthy behaviors or stress can lead to sedentary behavior and disease, which tend to accelerate the rate of decline in mobility that normally occurs with aging. Additionally, once pathology emerges, personality could exacerbate or reduce the functional impact through its effect on behavioral responses (Verbrugge & Jette, 1994).
Within the Big Five theoretical framework, which has received increasingly widespread recognition among personality researchers over the past decade, conscientiousness has emerged as an important personality correlate of health and self-reported physical functioning. More specifically, older individuals who are lower in conscientious (Chapman, Duberstein, & Lyness, 2007a; Goodwin & Friedman, 2006; Krueger, Wilson, Shah, Tang, & Bennett, 2006) have been shown to report worse physical function and an increased risk for mobility disability. Empirical evidence of biased reports of symptoms and illness by individuals with high conscientiousness (Feldman, Cohen, Doyle, Skoner, & Gwaltney, 1999) suggests that their perception of functional ability may also be altered. We believe that it is important to confirm these observations using performance-based indicators of physical function, such as walking speed. To date, most reports of an association with performance-based measures of function have focused on personality dimensions such as self-efficacy (Maly, Costigan, & Olney, 2005; Mendes de Leon, Seeman, Baker, Richardson, & Tinetti, 1996), optimism (Brenes, Rapp, Rejeski, & Miller, 2002), and vitality (Tiedemann, Sherrington, & Lord, 2005). Although these concepts tap into some dimensions of the Big Five (e.g., extraversion) and have been linked to conscientiousness (Marshall, Wortman, Vickers, Kusulas, & Hervig, 1994), whether personality dimensions assessed by validated personality instruments such as the NEO inventory are associated with performance-based measures of physical function and particularly functional decline has been less investigated. In previous work, we reported cross-sectional associations of the Big Five personality traits with walking speed (Tolea et al., 2010) and knee muscle strength (Tolea, Terracciano, Milaneschi, Metter, & Ferrucci, 2011) in a wide-age ranged population. However, we are unaware of any longitudinal study of personality and objectively measured decline in physical function, particularly among older populations.
Given the strong association between lifestyle, disease, and physical function, personality domains such as conscientiousness that have been shown to have strong associations with health behaviors (Bogg & Roberts, 2004) and chronic conditions (Chapman, Lyness, & Duberstein, 2007b) would be of particular interest to investigate. Individuals scoring high on conscientiousness tend to engage in health-promoting behaviors, such as physical activity (Rhodes & Smith, 2006) and avoid risky health-related behaviors such as smoking, excessive alcohol consumption, and illicit drug use (Bogg & Roberts 2004; Terracciano & Costa, 2004; Terracciano, Lockenhoff, Crum, et al., 2008). These health-promoting activities can help maintain health and good function and protect against functional decline. Although it is not clear whether openness to experience, the most debated and the least understood of the Big Five (Caspi, Roberts, & Shiner, 2005), is associated with health behaviors or disease, this Big Five personality dimension may prove to be an important, yet overlooked personality correlate of health. Recent evidence suggests that older persons high in openness to experience have lower risk of all-cause mortality (Iwasa et al., 2008; Masui, 2006). Arguably this advantage might stem from a predisposition toward curiosity and trying new activities, which in turn could foster development of greater functional capacity and better maintenance in old age.
Thus, the current research was undertaken to explore cross-sectional and longitudinal associations between the personality domains of conscientiousness and openness to experience and walking speed with the purpose of generating hypotheses particularly about the link between personality and physical functional decline and potential mediators in older adults. Walking speed in older adults reflects both habitual preference and health-related deficits or impairments, and it is possible that personality could be associated with both components. The cross-sectional analysis taps to some degree the habitual preference component and the longitudinal analysis, to the degree that it captures decline, addresses the impairment-related component. Investigating the relationship between personality characteristics, disease status, lifestyle factors, and mobility loss in old age may improve understanding of the mechanisms underlying functional decline and aid development of more effective preventive strategies for delaying mobility loss.
METHOD
Study Population
The study population consisted of participants in the Cognitive Vitality substudy within the Health, Aging, and Body Composition (Health ABC) Study, a longitudinal cohort study investigating the associations of body composition, weight-related health conditions, and development of functional limitations in older adults. Initially well-functioning Black and White men and women aged 70–79 years living in designated zip codes surrounding Pittsburgh, PA, and Memphis, TN, were recruited between March 1997 and July 1998. All participants provided informed consent, and all protocols were approved by the Institutional Review Boards at the study sites.
Of the 3,075 initial participants, 1,040 were selected at Year 3 (1999–2000) to participate in the Cognitive Vitality substudy, in which both conscientiousness and openness dimensions of personality were assessed. This subset was selected on the basis of performance on a test of cardiovascular fitness with the top 65 performers on an endurance walk test (Simonsick, Montgomery, Newman, Bauer, & Harris, 2001) in Year 2 (1998–1999) from each of eight groups defined by sex, race, and study site being invited to participate along with a random sample of 65 individuals drawn from the remaining members of each group. Substudy participants were slightly younger (74.9 vs. 75.6, p < .001), had more years of formal education (13.7 vs. 12.8, p < .001) and a lower body mass index (25.9 vs. 27.8, p < .001), but were similar in terms of their sex, race, and study site distribution. Of these, 907 had valid personality and walking speed data at the Year 3 study visit and constituted the analytic sample for the baseline analysis. The analytic sample for the longitudinal analysis consisted of 740 of the baseline participants for whom valid Year 6 (2002–2003) walking speed data were available.
Walking Speed
Walking speed was measured over a 20-m course as part of the core annual clinic visit. Participants were asked to walk at their usual pace for the full 20 m with timing beginning with the first footfall over the starting line and ending with the first foot across the finish line. Gait speed is expressed in meters per second (m/s).
Personality
The measures of openness and conscientiousness come from the NEO-Five-Factor Inventory (NEO-FFI; Costa & McCrae, 1989, 1992), a widely replicated model of personality (McCrae & Terracciano, 2005). The trait of openness to experience refers to the tendency to be imaginative, creative, emotionally, and artistically sensitive. The trait of conscientiousness refers to a tendency to be organized, strong-willed, persistent, reliable, and a follower of rules and ethical principles. In the Health ABC study, participants were asked to indicate their level of agreement (on a 5-item Likert scale ranging from strongly disagree to strongly agree) with 24 statements that comprise the openness and conscientiousness domains of personality. Total scores were calculated by summing scores for the 12 items representing each domain (after reversing negatively keyed items), resulting in two continuous variables with scores ranging from 0 to 48. Raw scores were converted to T-scores (mean = 50, standard deviation [SD] = 10) using the combined-sex norms for adults reported in the NEO-FFI manual (Costa & McCrae, 1992). The results present effects per 1 SD of these standardized scores. Internal consistency scores for openness and conscientiousness in this sample were alpha = .64 and .79, respectively.
Confounders and Mediators
Sociodemographics included age in years, sex (0 = male; 1 = female), race (0 = white; 1 = black), number of years of formal education, and study site (0 = Pittsburgh; 1 = Memphis). Presence of cardiac disease (i.e., coronary heart disease, myocardial infarction, cardiovascular disease, and stroke), cancer, diabetes, and arthritis was ascertained at baseline. Baseline prevalence (Year 3) was determined by combining Year 1 prevalence with incidence (up to clinic visit 3 date) based on periodic questionnaires (annual contacts) and on Health ABC event data collected and documented from hospital records. A combination of self-report, medication use, testing (e.g., glucose tolerance testing), and hospital records was used to determine presence of disease. Cognitive status was measured at the study baseline using the Modified Mini-Mental State Examination. Scores range from 0 to 100, with higher scores indicating better cognitive function.
Three health risk factors, which may mediate the association between personality and walking speed, were also included. Body mass index was expressed as weight in kilograms (measured using a standard balance beam scale) divided by height in meters squared (measured in millimeters with a wall-mounted stadiometer). Smoking status was categorized as never smoker or former smoker who quit before age 50 and current smoker or recent quitter, and physical activity was estimated from a questionnaire covering frequency, duration, and intensity of walking and moderate and vigorous activity, time spent doing home-related activities, and number of flights of stairs climbed in a typical 7-day period. A four-level physical activity variable was created with the levels defined as follows: low = casual walking of fewer than 60 min per week and no intense activities; mild = casual walking exceeding 60 min per week and no intense activities; moderate = intense activities for fewer than 180 min per week; and high = intense activities exceeding 180 min per week. Brisk walking is considered an intense activity. This scale incorporates participation level in both exercise activity including brisk walking and casual walking activities. The four levels were constructed to distinguish persons who meet the federal guidelines for physical activity in healthy adults (Level 4 in our categorization) and those who are completely sedentary (Level 1). The two middle groups comprise those who do not exercise but engage in some casual walking (Level 2), as well as those who exercise but do not meet the federal recommendations (Level 3).
Data Analysis
Baseline associations between each personality dimension and usual walking speed were assessed using separate linear regression models adjusted for sociodemographic factors (Model 1). Potential mediation of the association between personality and walking speed by chronic conditions, cognitive status, and health risk factors was assessed for each factor by adding them separately and together to Model 1 and comparing the main effects with and without adjustment for these factors. Although not a formal test of mediation, given the a priori assumption of mediation by these factors, it may be considered as indicative of such effects. Finally, to ensure more precise estimates of the independent effects of openness and conscientiousness, each trait was assessed with adjustment for the other personality domain. Presence of cancer (Beta = .064, p = .713 for walking speed; Beta = −.004, p = .783 for decline in walking speed) and education (Beta = .003, p = .180 for decline in walking speed) were not associated with walking speed and/or walking speed decline and were therefore excluded from the models predicting these outcomes.
Longitudinal associations between personality and gait speed decline were assessed using linear regression models predicting the effect of personality on follow-up walking speed, while adjusting for baseline walking speed, sociodemographic factors, chronic conditions, and health risk factors, in a sequence similar to that used in the baseline analysis. To account for the possibility of sample selection bias, an indicator variable for substudy sample group (top 65 performers or selected at random) was included in cross-sectional and longitudinal analyses.
RESULTS
On average, participants were 75 years old (age range: 71–82 years), highly educated, overweight, and had a usual gait speed of 1.2 m/s (0.2 SD); see Table 1. Openness and conscientiousness scores fell within the range considered to be normal (45–54) (Costa & McCrae, 1992). The sample had equal numbers defined by sex, race, and study site. Arthritis was the most prevalent chronic condition, one in four study participants smoked or recently quit, and 40% reported low levels of physical activity. Usual walking speed declined on average 5% over the 3-year follow-up period.
Table 1.
Baseline Characteristics of Sample Participants
| Characteristic | Mean ± SD or % |
| Age in years | 75.2 + 2.7 |
| Female | 50.0 |
| Black | 48.0 |
| Education in years | 13.2 ± 3.1 |
| Memphis | 46.0 |
| Cancer | 18.9 |
| Cardiac conditions | 23.8 |
| Diabetes | 20.0 |
| Arthritis | 55.1 |
| Smoker | 25.8 |
| BMI | 26.9 ± 4.6 |
| High activity | 13.3 |
| Conscientiousness | 48.3 ± 9.4 |
| Openness | 46.1 ± 9.3 |
| Walking speed in m/s | 1.21 ± 0.22 |
Note. BMI = body mass index.
In baseline analyses (n = 907), conscientiousness was positively associated with walking speed (Table 2). Each SD higher conscientiousness was associated with 0.016 m/s faster gait speed, independent of age, sex, race, education, and study site (Model 1). Inclusion of diabetes reduced the association by 25% (p = .055) and that of physical activity by 19% (p = .033). Inclusion of all mediators reduced the association between conscientiousness and walking speed by half. Further controlling for sampling bias using the indicator variable for top performers or random participants did not significantly influence the results. Openness was not associated with walking speed and did not have an impact on the association between conscientiousness and walking speed when added to the fully adjusted model (Beta = .009, p = .170).
Table 2.
Associations Between Personality Traits and Baseline Usual Walking Speed
| Conscientiousness | Openness | |||
| No adjustment for sampling design | Adjustment for sampling design | |||
| Beta | % Change in effect sizea | Beta | Beta | |
| Model 1 includes: age, sex, race, education, and study site | .016*, b | .013* | .009 | |
| Model 1 + cardiac conditions | .014* | 12.5↓ | .012* | .008 |
| Model 1 + diabetes | .012 | 25.0↓ | .010 | .012 |
| Model 1 + arthritis | .017* | 6.3↑ | .014* | .009 |
| Model 1 + cognition | .015* | 6.3↓ | .013* | .006 |
| Model 1 + chronic conditions | .011 | 31.3↓ | .011 | .008 |
| Model 1 + smoking | .015* | 6.3↓ | .013* | .009 |
| Model 1 + BMI | .014* | 12.5↓ | .012* | .009 |
| Model 1 + physical activity | .013* | 18.8↓ | .011* | .005 |
| Model 1 + health risk factors | .011 | 31.3↓ | .010 | .004 |
| Model 1 + all chronic conditions + all health risk factors | .008 | 50.0↓ | .008 | .004 |
Note. BMI = body mass index.
Change calculated from Model 1.
Beta = .016 is interpreted as an increase in walking speed of 0.016 m/s for each unit of increase in conscientiousness; because no association exists between openness and walking speed, changes in effect size or adjustments for selection design were not reported for this personality trait.
*p < .05.
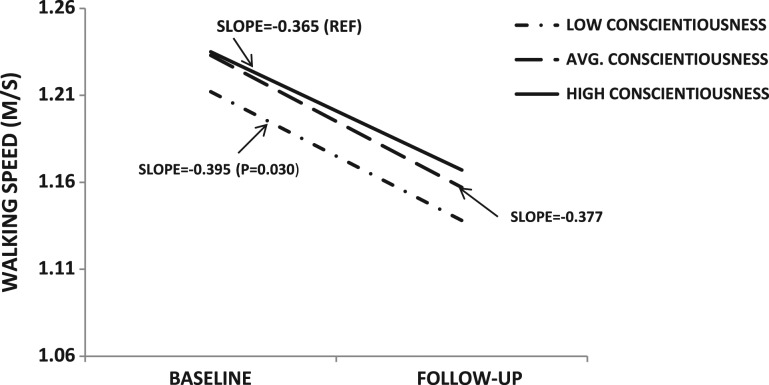
Similar to the baseline analysis, only conscientiousness was associated with decline in walking speed over the 3-year follow-up period, independent of baseline age, sex, race, study site, and walking speed (Table 3). For each SD increase in conscientiousness, the slope of decline increased by 0.011 m/s (Model 1). A graphical representation of the association between level of conscientiousness and decline in walking speed is presented in Figure 1. Compared with individuals with high conscientiousness (T-scores = 54), those with low conscientiousness (t scores < 45) declined by 0.030 m/s (p = .030), after adjustment for baseline walking speed and socio demographic factors. Neither the disease conditions nor the health risk factors had a significant impact on the association between conscientiousness and walking speed decline (Table 3). The association was not affected by inclusion of openness in the fully adjusted model (Beta = .010, p = .085) or by adjusting for participant selection.
Table 3.
Associations Between Personality Traits and Decline in Usual Walking Speed
| Conscientiousness | Openness | ||
| No adjustment for sampling design | Adjustment for sampling design | ||
| Slope | Slope | Slope | |
| Model 1 includes: age, sex, race, study site, and baseline walking speed | 0.011*a | 0.011* | 0.008 |
| Model 1 + cardiac conditions | 0.012* | 0.011* | 0.008 |
| Model 1 + diabetes | 0.011* | 0.011* | 0.005 |
| Model 1 + arthritis | 0.011* | 0.010 | 0.007 |
| Model 1 + cognition | 0.011* | 0.011* | 0.006 |
| Model 1 + all chronic conditions | 0.010 | 0.010 | 0.003 |
| Model 1 + smoking | 0.011* | 0.010 | 0.008 |
| Model 1 + BMI | 0.011* | 0.010 | 0.008 |
| Model 1 + physical activity | 0.011* | 0.010* | 0.006 |
| Model 1 + all health risk factors | 0.010 | 0.010 | 0.006 |
| Model 1 + all chronic conditions + all health risk factors | 0.009 | 0.009 | 0.007 |
Note. BMI = body mass index.
The rate of decline goes up by 0.011 m/s with each unit increase in conscientiousness, indicating lower decline with higher conscientiousness. Education was not significantly associated with decline in walking speed, so was not included in Model 1. Because no association exists between openness and walking speed decline, adjustments for sampling design were not reported for this personality trait.
*p < .05.
Figure 1.
Change in walking speed by level of conscientiousness.
DISCUSSION
In relatively healthy and generally well-functioning persons in their 70s, higher levels of conscientiousness were associated with a faster usual gait speed and less steep decline independent of sociodemographic factors. Both diabetes and physical activity partially explained the baseline association but not the association with mobility decline. Openness showed no cross-sectional or longitudinal association with gait speed.
Conscientiousness is regarded as one of the most significant personality determinants of health. Empirical evidence suggests that besides having a reduced risk of mortality (Iwasa et al., 2008; Taylor et al., 2009; Terracciano, Lockenhoff, Zonderman, et al., 2008; Weiss & Costa, 2005; Wilson, Mendes de Leon, Bienias, Evans, & Bennett, 2004), older adults who score higher on conscientiousness show fewer self-reported functional limitations. For example, in a sample of primary care older patients, for each 1 SD increase in conscientiousness, the likelihood of being free from instrumental activities of daily living impairment was increased by a factor of 0.071 (p = .01), above and beyond medical burden (Chapman et al., 2007a). A reduction of 3% in the risk of incident disability as measured by ADL limitations for each 1-unit increase in conscientiousness was reported among older individuals, even after chronic conditions and depressive symptoms were taken into account (Krueger et al., 2006). The findings of the current study add to the body of evidence supporting a protective effect of conscientiousness on functional status among older persons. Not only do high conscientious older individuals report better function but they also show better performance and reduced decline on performance-based measures of mobility. Moreover, effect sizes appear to be similar regardless of the nature of measurement used.
The significant reduction in the association between conscientiousness and gait speed after accounting for prevalent diabetes and physical activity level indicates that these factors may play a role in the link between personality trait and mobility. Compared with their counterparts, higher conscientious older individuals are more likely to engage in physical activities, which in turn may lead to faster walking speed. We have previously reported that physical activity level partially mediated the association between personality and knee muscle strength, another performance-based measure of functionality (Tolea et al., 2011). The current study provides further support for a mediating effect of health behavior and physical activity level in particular. Also, reports of lower conscientiousness among individuals with diabetes (Goodwin, & Friedman, 2006), a risk factor for poor physical function (Sayer et al., 2005), are in line with our results of potential mediation by chronic conditions and diabetes in particular. However, given the informal mediation testing that was employed in our study, these factors should be tested using more formal techniques in future research. However, consistent with other reports, we found little evidence of mediation of the association between conscientiousness and walking speed decline by lifestyle behaviors. In a sample of 2,359 relatively healthy and highly educated participants in the Baltimore Longitudinal Study of Aging (meanage 50.1 [16.9 SD]), the protective association between conscientiousness and mortality was largely unexplained by smoking and obesity (Terracciano, Lockenhoff, Zonderman, et al., 2008b).
Taken together, these findings suggest that the mechanisms linking conscientiousness to gait speed and mobility decline are likely complex. Whether disease status and health risk behavior represent significant components of these processes needs further study. Other factors should be considered as well. For example, individuals with high conscientiousness scores are more likely than those with lower scores to have greater feelings of efficacy as well as higher levels of health goals while being more disciplined and deliberate in following them with the likely direct result of better physical performance as measured in the present study. It is also possible that other factors such as better adherence to a medication regimen (Christensen & Smith, 1995; Dobbels et al., 2005), more common among individuals with higher conscientiousness could also play a role. These and other hypotheses should be investigated in future studies.
One explanation for the absence of an association for openness may relate to the older age of the population and the saliency of health conditions in impacting mobility. Studies that found an association between openness and physical function included younger persons on average (Duberstein et al., 2003; Tolea et al., 2010) or reported an association among individuals with physical illness (Goodwin & Friedman, 2006). In contrast, in the current sample, the age ranged from 72 to 81 years at baseline and consisted of relatively healthy individuals. Another explanation could be related to internal consistency. Cronbach’s alpha for the openness domain was lower than that reported in the NEO-PI-R manual (Costa & McCrae, 1992), suggesting a relatively poor correlation between items in the domain, which could potentially explain the null effect. Whether lower internal consistency is specific to older populations such as represented by the current sample should be investigated in future studies. Lastly, the relationship of openness to experience to physical function may be restricted to self-perceived difficulties (Duberstein et al., 2003) rather than performance.
Findings should be interpreted with consideration of potential limitations of this study. First, the study population consisted of well-functioning older individuals, who do not accurately represent the general elderly population. Longitudinal studies of personality and mobility decline in nationally representative populations of older individuals are needed. Second, we investigated the association of the domain levels of just two personality dimensions—openness and conscientiousness—with walking speed decline as these were the only personality traits measured in the Health ABC study. It is possible that other personality traits such as neuroticism, extraversion, and agreeableness and/or specific facets of these traits could also be related to mobility decline. Third, it is possible that variables not included in this study may explain the conscientiousness—walking speed association. For example, both conscientiousness and gait speed could be linked to genetic or other biological factors. Fourth, as mentioned above, the relatively poor internal consistency for the domain of openness might have limited our ability to observe an association with this personality trait. On the positive side, our investigation had the advantage of a relatively large sample size and a longitudinal design.
In conclusion, findings highlight the relationship of conscientiousness with gait speed and decline in gait speed with potential implications for the disablement process. Conscientious healthy older individuals tend to walk faster and to show less decline in gait speed, above the effect of sociodemographic characteristics. More research is needed to clarify the role of disease status and health behaviors as well as other pathways to better understand the robust and consistent beneficial association of conscientiousness with health and physical function in particular. From a five-factor model perspective, neuroticism, extraversion, and agreeableness should also be studied in relation to mobility decline in future longitudinal studies. Understanding what specific components of the domain of conscientiousness confer benefit can provide further insight into the mechanisms involved in the process of mobility decline in old age. A better understanding of these mechanisms may help inform medical and behavioral interventions to prevent decline and delay the development of mobility disability, which could be more efficient if tailored to individual’s personality characteristics. In this context, simpler and easier to complete exercise regimens would increase adherence of low conscientious individuals (Chapman et al., 2007b). The relative stability of personality traits after the age of 30 (Terracciano, Costa, & McCrae, 2006) suggests that these strategies could be implemented earlier in life when prevention of mobility decline is likely to be more effective.
FUNDING
This work was supported (in part) by the Intramural Research Program of the National Institutes of Health, National Institute on Aging (NIA). The Health ABC Study is funded by NIA contracts N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106. H.N.A. was partly supported by one of these contracts. P.T.C. receives royalties from the NEO-PI-R.
References
- Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. doi:10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Brenes GA, Rapp SR, Rejeski WJ, Miller ME. Do optimism and pessimism predict physical functioning? Journal of Behavioral Medicine. 2002;25:219–231. doi: 10.1023/a:1015376510466. [DOI] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. doi:10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Chapman B, Duberstein P, Lyness JM. Personality traits, education, and health-related quality of life among older adult primary care patients. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2007a;62:343–352. doi: 10.1093/geronb/62.6.p343. doi:10.1093/geronb/62.6.P343. [DOI] [PubMed] [Google Scholar]
- Chapman BP, Lyness JM, Duberstein P. Personality and medical illness burden among older adults in primary care. Psychosomatic Medicine. 2007b;69:277–282. doi: 10.1097/PSY.0b013e3180313975. doi:10.1097/PSY.0b013e3180313975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen AJ, Smith TW. Personality and patient adherence: Correlates of the five-factor model in renal dialysis. Journal of Behavioral Medicine. 1995;18:305–313. doi: 10.1007/BF01857875. doi:10.1007/BF01857875. [DOI] [PubMed] [Google Scholar]
- Costa PTJ, McCrae RR. The NEO-PI/NEO-FFI manual supplement. Odessa, FL: Psychological Assessment Resources; 1989. [Google Scholar]
- Costa PTJ, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Dobbels F, Vanhaecke J, Desmyttere A, Dupont L, Nevens F, De Geest S. Prevalence and correlates of self-reported pretransplant nonadherence with medication in heart, liver, and lung transplant candidates. Transplantation. 2005;79:1588–1595. doi: 10.1097/01.tp.0000158430.06507.87. doi:10.1097/01.TP.0000158430.06507.87. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Sorensen S, Lyness JM, King DA, Conwell Y, Seidlitz L, Caine ED. Personality is associated with perceived health and functional status in older primary care patients. Psychology and Aging. 2003;18:25–37. doi: 10.1037/0882-7974.18.1.25. doi:10.1037/0882-7974.18.1.25. [DOI] [PubMed] [Google Scholar]
- Feldman PJ, Cohen S, Doyle WJ, Skoner DP, Gwaltney JM., Jr The impact of personality on the reporting of unfounded symptoms and illness. Journal of Personality and Social Psychology. 1999;77:370–378. doi: 10.1037//0022-3514.77.2.370. doi:10.1037//0022-3514.77.2.370. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Friedman HS. Health status and the five-factor personality traits in a nationally representative sample. Journal of Health Psychology. 2006;11:643–654. doi: 10.1177/1359105306066610. doi:10.1177/1359105306066610. [DOI] [PubMed] [Google Scholar]
- Iwasa H, Masui Y, Gondo Y, Inagaki H, Kawaai C, Suzuki T. Personality and all-cause mortality among older adults dwelling in a Japanese community: A five-year population-based prospective cohort study. The American Journal of Geriatric Psychiatry. 2008;16:399–405. doi: 10.1097/JGP.0b013e3181662ac9. doi:10.1097/JGP.0b013e3181662ac9. [DOI] [PubMed] [Google Scholar]
- Krueger KR, Wilson RS, Shah RC, Tang Y, Bennett DA. Personality and incident disability in older persons. Age and Ageing. 2006;35:428–433. doi: 10.1093/ageing/afl028. doi:10.1093/ageing/afl028. [DOI] [PubMed] [Google Scholar]
- Maly MR, Costigan PA, Olney SJ. Contribution of psychosocial and mechanical variables to physical performance measures in knee osteoarthritis. Physical Therapy. 2005;85:1318–1328. [PubMed] [Google Scholar]
- Marshall GN, Wortman CB, Vickers RR, Jr, Kusulas JW, Hervig LK. The five-factor model of personality as a frame-work for personality-health research. Journal of Personality and Social Psychology. 1994;67:278–286. doi: 10.1037//0022-3514.67.2.278. [DOI] [PubMed] [Google Scholar]
- Masui Y. Do personality characteristics predict longevity? Age. 2006;28:353–361. doi: 10.1007/s11357-006-9024-6. doi:10.1007/s11357-006-9024-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae RR, Terracciano A. Universal features of personality traits from the observer's perspective: Data from 50 cultures. Journal of Personality and Social Psychology. 2005;88:547–561. doi: 10.1037/0022-3514.88.3.547. doi:10.1037/0022-3514.88.3.547. [DOI] [PubMed] [Google Scholar]
- Mendes de Leon CF, Seeman TE, Baker DI, Richardson ED, Tinetti ME. Self-efficacy, physical decline, and change in functioning in community-living elders: A prospective study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1996;51:S183–190. doi: 10.1093/geronb/51b.4.s183. doi:10.1093/geronb/51B.4.S183. [DOI] [PubMed] [Google Scholar]
- Rhodes RE, Smith NE. Personality correlates of physical activity: A review and meta-analysis. British Journal of Sports Medicine. 2006;40:958–965. doi: 10.1136/bjsm.2006.028860. doi:10.1136/bjsm.2006.028860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayer AA, Dennison EM, Syddall HE, Gilbody HJ, Phillips DI, Cooper C. Type 2 diabetes, muscle strength, and impaired physical function: The tip of the iceberg? Diabetes Care. 2005;28:2541–2542. doi: 10.2337/diacare.28.10.2541. doi:10.2337/diacare.28.10.2541. [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Montgomery PS, Newman AB, Bauer DC, Harris T. Measuring fitness in healthy older adults: The Health ABC Long Distance Corridor Walk. Journal of the American Geriatrics Society. 2001;49:1544–1548. doi: 10.1046/j.1532-5415.2001.4911247.x. doi:10.1046/j.1532-5415.2001.4911247.x. [DOI] [PubMed] [Google Scholar]
- Taylor MD, Whiteman MC, Fowkes GR, Lee AJ, Allerhand M, Deary IJ. Five Factor Model personality traits and all-cause mortality in the Edinburgh Artery Study cohort. Psychosomatic Medicine. 2009;71:631–641. doi: 10.1097/PSY.0b013e3181a65298. doi:10.1097/PSY.0b013e3181a65298. [DOI] [PubMed] [Google Scholar]
- Terracciano A, Costa PT., Jr Smoking and the five-factor model of personality. Addiction. 2004;99:472–481. doi: 10.1111/j.1360-0443.2004.00687.x. doi:10.1111/j.1360-0443.2004.00687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Lockenhoff CE, Crum RM, Bienvenu OJ, Costa PT., Jr Five-factor model personality profiles of drug users. BMC Psychiatry. 2008;8:22. doi: 10.1186/1471-244X-8-22. doi:10.1186/1471-244X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Lockenhoff CE, Zonderman AB, Ferrucci L, Costa PT., Jr Personality predictors of longevity: Activity, emotional stability, and conscientiousness. Psychosomatic Medicine. 2008;70:621–627. doi: 10.1097/PSY.0b013e31817b9371. doi:10.1097/PSY.0b013e31817b9371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiedemann A, Sherrington C, Lord SR. Physiological and psychological predictors of walking speed in older community-dwelling people. Gerontology. 2005;51:390–395. doi: 10.1159/000088703. doi:10.1159/000088703. [DOI] [PubMed] [Google Scholar]
- Tolea MI, Costa PT, Terracciano A, Griswold M, Simonsick EM, Najjar SS, Ferrucci L. Sex-specific correlates of walking speed in a wide age-ranged population. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2010;65:174–184. doi: 10.1093/geronb/gbp130. doi:10.1093/geronb/gbp130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolea MI, Terracciano A, Milaneschi Y, Metter EJ, Ferrucci L. Personality typology in relation to muscle strength. International Journal of Behavioral Medicine. 2011 doi: 10.1007/s12529-011-9166-5. Advance online publication. doi:10.1007/s12529-011-9166-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. doi:10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Weiss A, Costa PT., Jr Domain and facet personality predictors of all-cause mortality among Medicare patients aged 65 to 100. Psychosomatic Medicine. 2005;67:724–733. doi: 10.1097/01.psy.0000181272.58103.18. doi:10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes de Leon CF, Bienias JL, Evans DA, Bennett DA. Personality and mortality in old age. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2004;59:110–116. doi: 10.1093/geronb/59.3.p110. doi:10.1093/geronb/59.3.P110. [DOI] [PubMed] [Google Scholar]