Abstract
Objectives.
To examine the association between openness to experience and conscientiousness and incident reported walking limitation.
Method.
The study population consisted of 786 men and women aged 71–81 years (M = 75 years, SD = 2.7) participating in the Health, Aging, and Body Composition—Cognitive Vitality Substudy.
Results.
Nearly 20% of participants (155/786) developed walking limitation during 6 years of follow-up. High openness was associated with a reduced risk of walking limitation (hazard ratio [HR] = 0.83, 95% confidence interval [CI] = 0.69–0.98), independent of sociodemographic factors, health conditions, and conscientiousness. This association was not mediated by lifestyle factors and was not substantially modified by other risk factors for functional disability. Conscientiousness was not associated with risk of walking limitation (HR = 0.91, 95% CI = 0.77–1.07).
Discussion.
Findings suggest that personality dimensions, specifically higher openness to experience, may contribute to functional resilience in late life.
Keywords: Conscientiousness, Functional limitations, Openness to experience, Personality
The ability to walk, a basic physical function and prerequisite for independent living, becomes compromised with increasing age. By age 80, one in two individuals reports difficulty in mobility tasks, such as walking a quarter of a mile (Ostchega, Harris, Hirsch, Parsons, & Kington, 2000). Typically defined as difficulty walking a moderate distance (e.g., one quarter to one half mile), walking limitation constitutes an early stage of the disablement process (Fried & Guralnik, 1997; Manty et al., 2007) and strongly predicts further declines in functioning (Rivera, Fried, Weiss, & Simonsick, 2008), morbidity (Gayman, Turner, & Cui, 2008; Rasch, Magder, Hochberg, Magaziner, & Altman, 2008), hospitalization (Rogers et al., 2008), institutionalization (Quadri, Tettamanti, Bernasconi, Trento & Loew, 2005), and mortality (Melzer, Lan, & Guralnik, 2003).
Development and progression of walking limitations in old age are complex processes in which lifestyle factors play a central role (Simonsick et al., 1993). Personality, which refers to relatively stable lifelong patterns of thinking, feeling, and behaving, could play an integral role in these processes by impacting health-related behaviors and interacting with other risk factors to accelerate or decelerate the progression from impairment to limitation to disability. Within the framework of the Big Five personality taxonomy, less favorable personality traits such as high neuroticism, low extraversion, and low conscientiousness have been associated with physical inactivity (McCann, 2005; Rhodes & Smith, 2006; Saklofske, Austin, Rohr, & Andrews, 2007), smoking and alcohol abuse (McCann, 2005; Munafo & Black, 2007; Terracciano & Costa, 2004; Terracciano, Lockenhoff, Crum, Bienvenu, & Costa, 2008), and unhealthy diets (Brummett, Siegler, Day, & Costa, 2008; O’Connor, Conner, Jones, McMillan, & Ferguson, 2009), which may explain the higher likelihood of limitations in mobility (Jang, Mortimer, Haley, & Graves, 2002) and activities of daily living (ADL; Chapman, Duberstein, & Lyness, 2007; Krueger, Wilson, Shah, Tang, & Bennett, 2006) among individuals with these traits. Though less consistent, there is evidence that less agreeable persons also tend to smoke (Terracciano & Costa, 2004; Terracciano et al., 2008). Openness to experience, probably the most debated and least understood of the Big Five (Caspi, Roberts, & Shiner, 2005), has recently emerged as a potentially significant personality correlate of health. Openness has been associated with better functional status, both self-rated (Duberstein et al., 2003) and performance-based (Suchy, Williams, Kraybill, Franchow, & Butner, 2010), as well as with a lower risk of all-cause mortality (Iwasa et al., 2008; Masui, 2006). Empirical evidence of a link between openness and healthy dietary practices (Brummett et al., 2008; Goldberg & Strycker, 2002) and lower body mass index (BMI; Brummett et al., 2006) suggests that lifestyle factors may help explain these health benefits. Furthermore, there is evidence that personality may interact with other risk factors such as age and chronic conditions (Jang, Haley, Mortimer, & Small, 2003) to influence likelihood of self-reported disability including walking disability.
However, whether personality plays a role in mitigating development of reported walking limitations in older adults is unknown. Evidence of an impact early in the disablement process could have important clinical implications as it may help identify salient characteristics of older individuals resistant to functional limitations. The current study was undertaken to explore whether specific dimensions of personality are associated with a reduced likelihood of developing incident walking limitations among relatively healthy older individuals. Additionally, we sought to assess the mediation and moderation of this association by lifestyle factors and other known risk factors, respectively.
METHOD
Study Population
The Health, Aging, and Body Composition (Health ABC) study is a prospective cohort study initiated in 1997 to investigate the associations of body composition, weight-related health conditions, and functional limitations in initially well-functioning White and Black men and women aged 70–79 years living in designated zip codes surrounding Pittsburgh, Pennsylvania and Memphis, Tennessee. Recruitment for the parent study lasted between March 1997 and July 1998. Besides age and geographic location, eligibility criteria included no reported difficulty walking a quarter of a mile, climbing 10 steps without resting or performing ADL, no life-threatening cancers, and no intention to leave the area for at least 3 years. All participants provided informed consent, and all protocols were approved by the Institutional Review Boards at the study sites.
Of the 3075 initial participants, 1040 were invited at Year 3 (1999–2000) to participate in the Cognitive Vitality substudy, in which both conscientiousness and openness to experience dimensions of personality were assessed. These target participants were selected on the basis of their performance on an endurance walk test from the preceding visit (Year 2: 1998–1999; Simonsick, Montgomery, Newman, Bauer, & Harris, 2001). To assure sufficient numbers of robust participants, the top 65 performers (Simonsick et al., 2001) from eight groups defined by sex, race, and study site and a random sample of 65 individuals from the remaining participants in each group were invited to participate. Of these, 907 had a clinic visit in Year 3, were eligible and agreed to participate, and also had valid personality data. We further excluded 121 who reported walking limitation at baseline for a final analytic cohort of 786 participants who were followed up from Year 3 to Year 9 (2005–2006).
Outcome Variable: Persistent Walking Limitation
The occurrence of walking limitation was ascertained every 6 months during annual clinical visits and interim 6-month telephone interviews. Persistent walking limitation was defined as two consecutive reports of any difficulty walking one quarter of a mile (0.4 km) because of health or a physical problem. Defining walking limitation as difficulty at two consecutive assessments has the potential to select more participants with chronic walking limitation, providing an outcome that is thought to be a more reliable indicator of clinically relevant change in functional status than an indicator based on one assessment only (Koster et al., 2007). Additional information on reason for missing study contact and proxy information for participants who died was considered when incidence of mobility limitation was adjudicated (Koster et al., 2008). Time to incident walking limitation was calculated as the number of days from the baseline interview (Year 3) to the first interview when difficulty was reported either by participants or by their proxy.
Explanatory Variable: Personality
Participants in the Cognitive Vitality Substudy were asked to indicate their level of agreement (on a five-item Likert scale ranging from strongly disagree to strongly agree) with 24 statements that comprise the openness and conscientiousness domains of personality, as measured by the NEO Five Factor Inventory (FFI; Costa & McCrae, 1992). The trait of openness to experience refers to the tendency to be imaginative, creative, and emotionally and artistically sensitive. The trait of conscientiousness refers to a tendency to be organized, strong-willed, persistent, and reliable and to follow rules and ethical principles. Total scores were calculated by summing scores for the 12 items representing each domain (after reversing negatively keyed items), resulting in two continuous variables with scores ranging from 0 to 48. Raw scores were converted to T-scores (M = 50, SD = 10) using the combined-sex norms for adults reported in the NEO-FFI Manual (Costa & McCrae, 1992). Relationships are presented as effects associated with one standard deviation of these standardized scores. Internal consistency for openness and conscientiousness in this sample was good (α = .64 and .79, respectively).
Confounders: Sociodemographic and Health Measures
Sociodemographic characteristics included age, sex, race, years of formal education, and study site. Depressed mood was assessed with a 10-item version of the Center for Epidemiological Studies Depression Scale (Andresen, Malmgren, Carter, & Patrick, 1994), with a score of 10 or greater used to indicate high level of depressive symptomatology. Comorbidity was defined as presence of at least one of the following medical conditions: any cancer, coronary heart disease, myocardial infarction, cardiovascular disease, stroke, diabetes, or arthritis. Disease status was determined by combining prevalent disease variables from Health ABC Year 1 with incident disease variables up to the Year 3 clinic visit (the Cognitive Vitality substudy baseline) based on semiannual contacts and event data collected and documented from hospital records. Except for event data, all other disease variables used a combination of self-report, medication use, and/or objective tests (e.g., glucose tolerance testing).
Mediators: Health-Related Behaviors
Three health-related factors that could potentially mediate the association between personality and development of walking limitation were also examined. NEO Personality Inventory traits have been shown to predict change in BMI over time (Brummett et al., 2006). On the other hand, a BMI more than 30 may put one at increased risk of having mobility limitation as compared with a BMI of less than 25 (Wannamethee, Ebrahim, Papacosta, & Shaper, 2005). We therefore investigated whether BMI, which was derived from measured weight and height and calculated as kg/m2, explains the association between personality and incident walking limitation. Smoking has been previously reported to explain in part the effect of personality traits on physical health (Mroczek, Spiro, & Turiano 2009) and was included in our analysis as a potential mediator of the associations of interest. We categorized smoking status as never smoker or former smoker who quit before age 50 and current smoker or former smoker who quit after age 50. Similarly, it is well known that sedentary lifestyle is associated with increased risk of mobility limitation. Moreover, personality correlates of physical activity have been identified (Rhodes & Smith, 2006), suggesting that physical activity may also mediate the personality and walking limitation association. We estimated physical activity level from questionnaire items covering frequency, duration, and intensity of walking and vigorous activity in a typical 7-day period. A four-level physical activity variable was created with the following levels: low = casual walking of less than 60 min per week and no intense activities; mild = casual walking exceeding 60 min per week and no intense activities; moderate = intense activities for less than 180 min per week; and high = intense activities exceeding 180 min per week. Brisk walking was considered an intense activity. The four levels were constructed to distinguish persons who meet the federal guidelines for physical activity in healthy adults (Level 4 in our categorization) and those who are completely sedentary (Level 1). The two middle groups comprise those who do not exercise but engage in some casual walking (Level 2) as well as those who exercise but do not meet the federal recommendations (Level 3).
Data Analysis
Differences in baseline characteristics between participants who developed and did not develop persistent walking limitation were compared using t test statistics for continuous variables and λ2 tests for categorical variables. Kaplan–Meier survival function plots were obtained, and Cox proportional hazards regression models were fit to study the individual association between personality traits and time to development of walking limitation. The proportionality assumption was assessed by testing interactions of each variable in the models with time (log transformed). The proportional hazards assumptions were not violated. Participants surviving without developing persistent walking limitation were censored at their last study visit. Persons who died without evidence of persistent walking limitation were censored at their time of death. Those lost to follow-up were censored at their last interview. The association between personality and incident walking limitations was first assessed without adjustment (Model 1), then adjusted for baseline age, sex, education, race, study site, presence of comorbidities, and depressive symptoms (Model 2). An additional model testing the association of each personality trait with time to incident walking limitation after adjusting for other personality traits in addition to the covariates was also run (Model 3). To investigate the mediating effect of BMI, smoking status, and physical activity level on the association between personality and incident walking limitation, we added these three factors as covariates into the fully adjusted model. Additionally, potential moderators of the personality—incident walking limitation association were assessed by introducing in the model appropriate interaction terms (Personality × Factor). Results are presented as hazard ratios (HRs) with 95% confidence intervals (CIs). Because we found no interaction between personality and sex (p = .469 for openness; p = .531 for conscientiousness), analyses were conducted on men and women together. Statistical significance was considered at a p level of less than .05. All analyses were conducted using SAS 9.2 Statistical Package (SAS Institute, Inc., Cary, North Carolina, USA).
RESULTS
Participants, who took on average 3.5 years (across the entire sample) to develop walking limitation (SD = 0.9 years; range = 0.3–4.3 years) were equally distributed by sex and were on average aged 75 years (SD = 2.7), highly educated (M = 13.4 years of formal education), and mildly overweight (BMI = 26.4). They also exhibited average scores on openness and conscientiousness. A majority had at least one of the seven chronic conditions, one in six engaging in intense physical activities at least 3 hr per week, and about 10% had a high level of depressive symptoms.
Baseline characteristics for the entire sample and by incident walking limitation status are presented in Table 1. Approximately 20% (155/786) developed walking limitation during the study follow-up. Compared with participants who remained free of walking limitation, incident cases were less educated, more likely to be Black, had more depressive symptoms, and were more likely to report comorbidity. They also had higher BMI, were less likely to report high levels of physical activity, and had lower scores on openness.
Table 1.
Participant Characteristics at Study Baseline by Incident Walking Limitation in Women and Men
| Characteristic | All (n = 786) | No walking limitation (n = 631) | Walking limitation (n = 155) | p Valuea |
| Age, years, M (SD) | 75.1 (2.7) | 75.0 (2.7) | 75.3 (2.8) | .212 |
| Female, % | 49.1 | 48.3 | 52.3 | .382 |
| Education, years (SD) | 13.4 (3.1) | 13.5 (3.0) | 12.8 (3.0) | .006 |
| Black, % | 45.6 | 41.7 | 61.3 | <.001 |
| Study site, % Memphis | 47.2 | 47.9 | 44.5 | .455 |
| High depressive symptoms, % | 9.0 | 7.3 | 15.5 | .001 |
| Chronic conditions, % | 73 | 71 | 82 | .00 |
| BMI (kg/m2), M (SD) | 26.4 (4.3) | 26.2 (4.1) | 28.1 (5.0) | <.001 |
| Smokers, % | 24.0 | 22.6 | 29.7 | .065 |
| High physical activity, % | 15.0 | 16.9 | 7.1 | <.001 |
| Openness, M (SD) | 46.5 (9.4) | 47.0 (9.5) | 44.6 (8.9) | .006 |
| Conscientiousness, M (SD) | 48.8 (9.4) | 48.9 (9.4) | 47.9 (9.3) | .240 |
Notes. BMI = body mass index; CESD = Center for Epidemiological Studies Depression Scale.
From tests of comparison of means (t test) or proportions (λ2).
Associations between openness and conscientiousness and risk of developing incident persistent walking limitation are presented in Table 2. A significant association was observed for the domain of openness only. When no other factors are considered, for each standard deviation increases in openness score, the risk of incident walking limitation was 21% lower. Although slightly, the association of openness remained even after sociodemographic and health-related factors were adjusted for in the analysis. This association was independent of conscientiousness score. In contrast, the domain of conscientiousness was not associated with incident walking limitation (see Tables 1 and 2).
Table 2.
Hazard Ratios Associated With One Standard Deviation Increase in Openness and Conscientiousness Score on the Risk of Developing Incident Walking Limitation in Women and Men Older Than 4.5 Years
| Personality trait | Model 1 | Model 2 | Model 3 |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Openness | 0.788 (0.671–0.925) | 0.829 (0.695–0.989) | 0.825 (0.692–0.984) |
| Conscientiousness | 0.904 (0.774–1.057) | 0.917 (0.782–1.075) | 0.908 (0.774–1.065) |
Note . Model 1: openness and conscientiousness tested separately and without adjustment. Model 2: openness and conscientiousness tested separately with adjustment for age, sex, race, education, site, chronic conditions, and high depressive symptomatology. Model 3: includes both personality traits and Model 2 adjustment factors. CI = confidence interval; HR = hazard ratio.
Because only openness showed a protective association with developing walking limitation, mediation analyses were conducted for this domain alone. Smoking status, BMI, and physical activity were added one at a time to the fully adjusted model displayed in Table 2. As shown in Table 3, adding smoking status and BMI to the model did not markedly impact the association between openness and the risk of incident walking limitation. Although the addition of physical activity to the model reduced the openness–walking limitation association to nonsignificance, the effect size was only slightly reduced and thus does not definitely indicate physical activity as a mediator.
Table 3.
Hazard Ratios Associated With One Standard Deviation Increase in Personality Score on the Risk of Incident Walking Limitation as Affected by Smoking, BMI, and Physical Activity
| Association of openness with incident walking limitation | HR | 95% CI |
| Adjusted for covariates | 0.825 | 0.692–0.984 |
| Adjusted for covariates and smoking | 0.837 | 0.702–0.998 |
| Adjusted for covariates and BMI | 0.824 | 0.689–0.986 |
| Adjusted for covariates and physical activity | 0.842 | 0.705–1.006 |
Note. Covariates were age, sex, race, study site, comorbidities, depressive symptoms, and conscientiousness. BMI = body mass index; CI = confidence interval; HR = hazard ratio.
We found no evidence of an interaction between personality and age, presence of chronic conditions, other covariates, or potential mediators. No moderation effects were found for either of the sociodemographic, health-related, or behavioral factors investigated (data not shown).
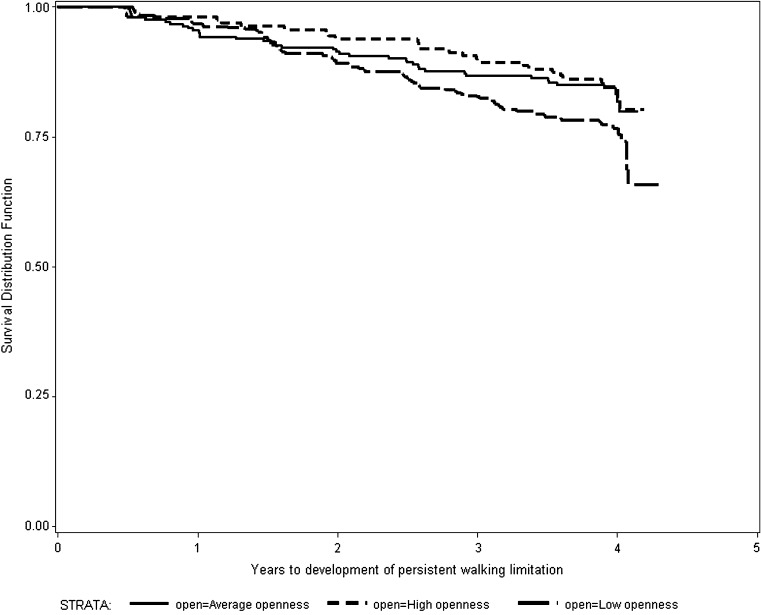
Figure 1 illustrates the association between openness and risk of incident walking limitation over the 6 years of follow-up. For ease of presentation and to be consistent with other reports (Weiss & Costa, 2005), the domain of openness was categorized as low (<45), average (45–54), or high (≥54). Protection from developing mobility limitation with respect to openness appears to operate in a dose–response manner with the risk decreasing with increasing openness level (HR = 0.68, 95% CI = 0.46–0.98 for average vs. low; HR = 0.63, 95% CI = 0.41–0.98 for high vs. low; and HR = 0.94, 95% CI = 0.57–1.53 for high vs. average).
Figure 1.
Proportion not developing walking limitation according to openness level and years to incident limitation.
DISCUSSION
This study examined the association of openness and conscientiousness on incident reported walking limitation among well-functioning older adults with consideration of potential mediators and moderators of this association. Higher openness to experience, but not conscientiousness, appears protective of developing walking limitation independent of age, sex, race, prevalent comorbid conditions, and lifestyle factors, such as smoking and BMI. Participation in vigorous physical activity including brisk walking may partially explain the protective association of openness.
Openness to experience has recently emerged as an important correlate of health outcomes. For example, higher scores on openness have been associated with slower disease progression (Ironson, O’Cleirigh, Weiss, Schneiderman, & Costa, 2008) and a reduced risk of mortality (Iwasa et al., 2008). However, reports on an association between openness and functional status are limited. In a recent study investigating the effect of personality on both self-reported and performance-based instrumental activities of daily living difficulties (Suchy et al., 2010), actual difficulties were associated with lower openness to experience in community-dwelling older adults. In another cross-sectional study, openness was also associated with perceived mobility and ADL disability in older primary care patients (Duberstein et al., 2003). The current study extends findings of a positive effect of openness to protection against development of walking limitation in generally healthy community-dwelling older adults.
In spite of the growing evidence of its health benefits, the mechanisms explaining the association between openness and health outcomes are still largely unknown. One such pathway could be represented by health behaviors. Higher openness to experience in older adults may reflect a lifetime of health-enhancing behaviors (Brummett et al., 2008; de Bruijn, Kremers, van Mechelen, & Brug, 2005; McCann, 2005; Smith & Spiro, 2002), which in turn may protect against development of mobility limitations. However, in the current study, we did not find compelling support for this hypothesis. Although higher openness was associated with higher level of physical activity, its effect on incident walking limitation was only slightly reduced by taking into account one’s physical activity level indicating that other factors may play a more significant role in explaining its protective effect.
Another potential mechanism for the association between openness and physical health may involve stress regulation. In a recent study of undergraduate students, greater stress resilience was found among highly open students, who demonstrated a combination of increased parasymphathetic response, lesser sympathetic reactivity, as well as modest increases in positive affect (Williams, Rau, Cribbet, & Gunn, 2009). These beneficial responses could in turn offer protection against onset of disability (Rai et al., 2011; Ullrich, Turner, Ciol, & Berger, 2005). It could therefore be argued that greater vulnerability to adverse effects of stress associated to lower openness may over time lead to a higher likelihood of mobility limitations. Moreover, a link between high openness and better executive functioning among older adults has been reported (Williams, Suchy, & Kraybill, 2010). Executive functioning in turn has been found to be an important determinant of functional status (Grigsby, Kaye, Baxter, Shetterly, & Hamman, 1998). Therefore, openness to experience could be associated with “cognitive reserve” with potential protective effects against cognitive decline (Williams et al., 2010) and with further beneficial effects on physical functioning (DeYoung, Peterson, & Higgins, 2005; Duchek, Balota, Storandt, & Larsen, 2007). Other psychological factors such as mastery, motivation, purposefulness, and/or emotional suppression (Duberstein et al., 2003) have been suggested as potential mediators. Future studies should investigate whether these factors help elucidate the association of openness with self-reported preservation of physical function.
The International Classification of Functioning, Disability, and Health model of disability proposes that personality interacts with health conditions (aging is included in this category) to affect disability development and progression. Previous cross-sectional studies have found evidence of interactions of neuroticism (Duberstein et al., 2003; Jang et al., 2003) and extraversion (Duberstein et al., 2003), with age and chronic conditions in predicting reports of poor functional status. We found no evidence of an age interaction with openness or conscientiousness with age, chronic conditions or other risk behavioral factors, and incident mobility limitation. The absence of an age interaction with openness and function is consistent with Duberstein and colleagues’ (2003) work, who suggested that with increasing age affective processes (associated with traits like neuroticism and extraversion) are more important for subjective health than behavioral processes (associated with openness and conscientiousness).
We found no support for the hypothesis that higher conscientiousness protects against mobility limitation, which contrasts with Krueger and colleagues who reported that older individuals having high conscientiousness had a lower risk of developing disability (Krueger et al., 2006). These differential findings may be explained in part by sample differences. Krueger and colleagues studied Catholic clergy members, a more homogenous group in terms of lifestyle and socioeconomic status than the Cognitive Vitality Substudy population, which may have enhanced the ability to identify an association between conscientiousness and disability. Alternatively, reports of self-care difficulties may be more sensitive to conscientiousness than reports of walking capacity alone.
The primary limitation of this study concerns the abbreviated assessment of personality. Only the short forms of just two personality domains—openness and conscientiousness—were ascertained, thus restricting the ability to more thoroughly investigate the relationship between personality and maintenance of walking ability in late life. Thus, it is possible that other dimensions or facets of personality have more robust associations with functional resiliency or that the relationship between openness and walking limitation may be explained by associated personality features. The mediation analyses were also limited to the behavioral factors assessed, which did not cover all possible mechanisms. Last, given that the potential for reciprocal associations between personality and physical functional status across time and that the time-to-event analysis usually implies a clear precedence of exposure (i.e., personality) to outcome (i.e., development of mobility limitation), our findings should be interpreted with caution.
In conclusion, we found evidence for a protective association of openness to experience against incident walking limitation in initially well-functioning community-resident persons in their seventies, beyond contributions of age, sex, race, education, and health-related factors. These findings provide further evidence for the notion that openness to experience, an often overlooked personality dimension, may be an important health determinant. The lower risk of mobility limitations in open older adults is consistent with their reported reduced risk of mortality (Iwasa et al., 2008. Future research should focus on identifying contributions of specific aspects of openness.
FUNDING
The Health ABC Study is funded by N ational Institute on Aging (NIA) Contracts N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106. H.N. Ayonayon was partly supported by one of these contracts. This research was supported (in part) by the Intramural Research Program of the National Institutes of Health , NIA. P. T. Costa receives royalties from the NEO-PI-R.
CONFLICT OF INTEREST
The sponsor had no role in any of the following: design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation and review of the manuscript.
Acknowledgments
All authors approved the submitted manuscript and have participated sufficiently in the research report to take public responsibility. M. I. Tolea, E. M. Simonsick, and L. Ferrucci were involved in conception and design of the study; all the other authors critically revised the manuscript for important intellectual content. M. I. Tolea performed statistical analysis. E. M. Simonsick provided supervision of the research project.
References
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Brummett BH, Babyak MA, Williams RB, Barefoot JC, Costa PT, Siegler IC. NEO personality domains and gender predict levels and trends in body mass index over 14 years during midlife. Journal of Research in Personality. 2006;40:222–236. doi:10.1016/j.jrp.2004.12.002. [Google Scholar]
- Brummett BH, Siegler IC, Day RS, Costa PT. Personality as a predictor of dietary quality in spouses during midlife. Behavioral Medicine. 2008;34:5–10. doi: 10.3200/BMED.34.1.5-10. doi:10.3200/BMED.34.1.5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. doi:10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Chapman B, Duberstein P, Lyness JM. Personality traits, education, and health-related quality of life among older adult primary care patients. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2007;62:343–352. doi: 10.1093/geronb/62.6.p343. doi:10.1093/geronb/62.6.P343. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- de Bruijn GJ, Kremers SP, van Mechelen W, Brug J. Is personality related to fruit and vegetable intake and physical activity in adolescents? Health Education Research. 2005;20:635–644. doi: 10.1093/her/cyh025. doi:10.1093/her/cyh025. [DOI] [PubMed] [Google Scholar]
- DeYoung CG, Peterson JB, Higgins DM. Sources of openness/intellect: Cognitive and neuropsychological correlates of the fifth factor of personality. Journal of Personality. 2005;73:825–858. doi: 10.1111/j.1467-6494.2005.00330.x. doi:10.1111/j.1467-6494.2005.00330.x. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Sorensen S, Lyness JM, King DA, Conwell Y, Seidlitz L, Caine ED. Personality is associated with perceived health and functional status in older primary care patients. Psychology and Aging. 2003;18:25–37. doi: 10.1037/0882-7974.18.1.25. doi:10.1037/0882-7974.18.1.25. [DOI] [PubMed] [Google Scholar]
- Duchek JM, Balota DA, Storandt M, Larsen R. The power of personality in discriminating between healthy aging and early-stage Alzheimer's disease. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2007;62:353–361. doi: 10.1093/geronb/62.6.p353. doi:http://dx.doi.org/10.1093%2Fgeronb%2F62.6.P353. [DOI] [PubMed] [Google Scholar]
- Fried LP, Guralnik JM. Disability in older adults: Evidence regarding significance, etiology, and risk. Journal of the American Geriatrics Society. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- Gayman MD, Turner RJ, Cui M. Physical limitations and depressive symptoms: Exploring the nature of the association. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2008;63:219–228. doi: 10.1093/geronb/63.4.s219. doi:10.1093/geronb/63.4.S219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg LR, Strycker LA. Personality traits and eating habits: The assessment of food preferences in a large community sample. Personality and Individual Differences. 2002;32:49–65. doi:10.1016/S0191-8869(01)00005-8. [Google Scholar]
- Grigsby J, Kaye K, Baxter J, Shetterly SM, Hamman RF. Executive cognitive abilities and functional status among community-dwelling older persons in the San Luis Valley Health and Aging Study. Journal of the American Geriatrics Society. 1998;46:590–596. doi: 10.1111/j.1532-5415.1998.tb01075.x. [DOI] [PubMed] [Google Scholar]
- Ironson GH, O’Cleirigh C, Weiss A, Schneiderman N, Costa PT., Jr Personality and HIV disease progression: Role of NEO-PI-R openness, extraversion, and profiles of engagement. Psychosomatic Medicine. 2008;70:245–253. doi: 10.1097/PSY.0b013e31816422fc. doi:10.1097/PSY.0b013e31816422fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwasa H, Masui Y, Gondo Y, Inagaki H, Kawaai C, Suzuki T. Personality and all-cause mortality among older adults dwelling in a Japanese community: A five-year population-based prospective cohort study. American Journal of Geriatric Psychiatry. 2008;16:399–405. doi: 10.1097/JGP.0b013e3181662ac9. doi:10.1097/JGP.0b013e3181662ac9. [DOI] [PubMed] [Google Scholar]
- Jang Y, Haley WE, Mortimer JA, Small BJ. Moderating effects of psychosocial attributes on the association between risk factors and disability in later life. Aging & Mental Health. 2003;7:163–170. doi: 10.1080/1360786031000101111. doi:10.1080/1360786031000101111. [DOI] [PubMed] [Google Scholar]
- Jang Y, Mortimer JA, Haley WE, Graves AB. The role of neuroticism in the association between performance-based and self-reported measures of mobility. Journal of Aging and Health. 2002;14:495–508. doi: 10.1177/089826402237180. doi:10.1177/089826402237180. [DOI] [PubMed] [Google Scholar]
- Koster A, Patel KV, Visser M, van Eijk JT, Kanaya AM, de Rekeneire N, Harris TB. Joint effects of adiposity and physical activity on incident mobility limitation in older adults. Journal of the American Geriatrics Society. 2008;56:636–643. doi: 10.1111/j.1532-5415.2007.01632.x. doi:10.1111/j.1532-5415.2007.01632.x. [DOI] [PubMed] [Google Scholar]
- Koster A, Penninx BW, Newman AB, Visser M, van Gool CH, Harris TB, Kritchevsky SB. Lifestyle factors and incident mobility limitation in obese and non-obese older adults. Obesity (Silver Spring) 2007;15:3122–3132. doi: 10.1038/oby.2007.372. doi:10.1038/oby.2007.372. [DOI] [PubMed] [Google Scholar]
- Krueger KR, Wilson RS, Shah RC, Tang Y, Bennett DA. Personality and incident disability in older persons. Age and Ageing. 2006;35:428–433. doi: 10.1093/ageing/afl028. doi:10.1093/ageing/afl028. [DOI] [PubMed] [Google Scholar]
- Manty M, Heinonen A, Leinonen R, Tormakangas T, Sakari-Rantala R, Hirvensalo M, Rantanen T. Construct and predictive validity of a self-reported measure of preclinical mobility limitation. Archives of Physical Medicine and Rehabilitation. 2007;88:1108–1113. doi: 10.1016/j.apmr.2007.06.016. doi:10.1016/j.apmr.2007.06.016. [DOI] [PubMed] [Google Scholar]
- Masui Y. Do personality characteristics predict longevity? Age. 2006;28:353–361. doi: 10.1007/s11357-006-9024-6. doi:10.1007/s11357-006-9024-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann SJ. Longevity, big five personality factors, and health behaviors: Presidents from Washington to Nixon. Journal of Psychology. 2005;139:273–286. doi: 10.3200/JRLP.139.3.273-288. doi:10.3200/JRLP.139.3.273-288. [DOI] [PubMed] [Google Scholar]
- Melzer D, Lan TY, Guralnik JM. The predictive validity for mortality of the index of mobility-related limitation–results from the EPESE study. Age and Ageing. 2003;32:619–625. doi: 10.1093/ageing/afg107. doi:10.1093/ageing/afg107. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A, Turiano N. Do Health Behaviors Explain the Effect of Neuroticism on Mortality? Longitudinal Findings from the VA Normative Aging Study. Journal of Research in Personality. 2009;43:653–659. doi: 10.1016/j.jrp.2009.03.016. doi:10.1016/j.jrp.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafo MR, Black S. Personality and smoking status: A longitudinal analysis. Nicotine & Tobacco Research. 2007;9:397–404. doi: 10.1080/14622200701188869. doi:10.1080/14622200701188869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor DB, Conner M, Jones F, McMillan B, Ferguson E. Exploring the benefits of conscientiousness: An investigation of the role of daily stressors and health behaviors. Annals of Behavioral Medicine. 2009;37:184–196. doi: 10.1007/s12160-009-9087-6. doi:10.1007/s12160-009-9087-6. [DOI] [PubMed] [Google Scholar]
- Ostchega Y, Harris TB, Hirsch R, Parsons VL, Kington R. The prevalence of functional limitations and disability in older persons in the US: Data from the National Health and Nutrition Examination Survey III. Journal of the American Geriatrics Society. 2000;48:1132–1135. doi: 10.1111/j.1532-5415.2000.tb04791.x. [DOI] [PubMed] [Google Scholar]
- Quadri P, Tettamanti M, Bernasconi S, Trento F, Loew F. Lower limb function as predictor of falls and loss of mobility with social repercussions one year after discharge among elderly inpatients. Aging Clinical and Experimental Research. 2005;17:82–89. doi: 10.1007/BF03324578. [DOI] [PubMed] [Google Scholar]
- Rai K, Kosidou K, Lundberg M, Araya R, Lewis G, Magnusson C. Psychological distress and risk of long-term disability: Population-based longitudinal study. Journal of Epidemiology and Community Health. 2011 doi: 10.1136/jech.2010.119644. Advance online publication. doi:10.1136/jech.2010.119644. [DOI] [PubMed] [Google Scholar]
- Rasch EK, Magder L, Hochberg MC, Magaziner J, Altman BM. Health of community-dwelling adults with mobility limitations in the United States: Incidence of secondary health conditions. Part II. Archives of Physical Medicine and Rehabilitation. 2008;89:219–230. doi: 10.1016/j.apmr.2007.08.159. doi:10.1016/j.apmr.2007.08.159. [DOI] [PubMed] [Google Scholar]
- Rhodes RE, Smith NE. Personality correlates of physical activity: A review and meta-analysis. British Journal of Sports Medicine. 2006;40:958–965. doi: 10.1136/bjsm.2006.028860. doi:10.1136/bjsm.2006.028860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera JA, Fried LP, Weiss CO, Simonsick EM. At the tipping point: Predicting severe mobility difficulty in vulnerable older women. Journal of the American Geriatrics Society. 2008;56:1417–1423. doi: 10.1111/j.1532-5415.2008.01819.x. doi:10.1111/j.1532-5415.2008.01819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers MA, Fries BE, Kaufman SR, Mody L, McMahon LF, Jr, Saint S. Mobility and other predictors of hospitalization for urinary tract infection: A retrospective cohort study. BMC Geriatrics. 2008;8:31. doi: 10.1186/1471-2318-8-31. doi:10.1186/1471-2318-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saklofske DH, Austin EJ, Rohr BA, Andrews JJ. Personality, emotional intelligence and exercise. Journal of Health Psychology. 2007;12:937–948. doi: 10.1177/1359105307082458. doi:10.1177/1359105307082458. [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Lafferty ME, Phillips CL, Mendes de Leon CF, Kasl SV, Seeman TE, Lemke JH. Risk due to inactivity in physically capable older adults. American Journal of Public Health. 1993;83:1443–1450. doi: 10.2105/ajph.83.10.1443. doi:10.2105/AJPH.83.10.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonsick EM, Montgomery PS, Newman AB, Bauer DC, Harris T. Measuring fitness in healthy older adults: The Health ABC Long Distance Corridor Walk. Journal of American Geriatrics Society. 2001;49:1544–1548. doi: 10.1046/j.1532-5415.2001.4911247.x. doi:10.1046/j.1532-5415.2001.4911247.x. [DOI] [PubMed] [Google Scholar]
- Smith TW, Spiro A., III Personality, health, and aging: Prolegomenon for the next generation. Journal of Research in Personality. 2002;36:363–394. doi:10.1016/S0092-6566(02)00014-4. [Google Scholar]
- Suchy Y, Williams PG, Kraybill ML, Franchow E, Butner J. Instrumental activities of daily living among community-dwelling older adults: Personality associations with self-report, performance, and awareness of functional difficulties. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2010;65:542–550. doi: 10.1093/geronb/gbq037. doi:10.1093/geronb/gbq037. [DOI] [PubMed] [Google Scholar]
- Terracciano A, Costa PT., Jr Smoking and the five-factor model of personality. Addiction. 2004;99:472–481. doi: 10.1111/j.1360-0443.2004.00687.x. doi:10.1111/j.1360-0443.2004.00687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Lockenhoff CE, Crum RM, Bienvenu OJ, Costa PT., Jr Five-factor model personality profiles of drug users. BMC Psychiatry. 2008;8:22. doi: 10.1186/1471-244X-8-22. doi:10.1186/1471-244X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich PM, Turner JA, Ciol M, Berger R. Stress is associated with subsequent pain and disability among men with nonbacterial prostatis/pelvic pain. Annals of Behavioral Medicine. 2005;30:112–118. doi: 10.1207/s15324796abm3002_3. doi:10.1207/s15324796abm3002_3. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Ebrahim S, Papacosta O, Shaper AG. From a postal questionnaire of older men, healthy lifestyle factors reduced the onset of and may have increased recovery from mobility limitation. Journal of Clinical Epidemiology. 2005;58:831–840. doi: 10.1016/j.jclinepi.2005.01.007. doi:10.1016/j.jclinepi.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Weiss A, Costa PT., Jr Domain and facet personality predictors of all-cause mortality among Medicare patients aged 65 to 100. Psychosomatic Medicine. 2005;67:724–733. doi: 10.1097/01.psy.0000181272.58103.18. doi:10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- Williams PG, Rau HK, Cribbet MR, Gunn HE. Openness to experience and stress regulation. Journal of Research in Personality. 2009;43:777–784. doi:10.1016/j.jrp.2009.06.003. [Google Scholar]
- Williams PG, Suchy Y, Kraybill ML. Five-factor model personality traits and executive functioning among older adults. Journal of Research in Personality. 2010;44:485–491. doi:10.1016/j.jrp.2010.06.002. [Google Scholar]