Abstract
Wound closure requires deep understanding of wound physiology, anatomy, and the healing phase of the wound. The basic principles of wound closure, diabetes control, normal nutrition status, infection control, mechanical stress avoidance, and nursing care are all important elements in achieving healing of acute and chronic wounds. This goal is achievable only through the interdisciplinary approach to wound healing. A number of wound closure techniques are available to the plastic surgeon. This armamentarium includes a variety of techniques, from simple primary wound closure to more-sophisticated and -costly flap reconstructive techniques. This article summarizes the components of the reconstructive ladder for wound closure that are available to the reconstructive surgeon.
Keywords: Secondary intention, Primary closure, Skin grafts, Flaps, Tissue expansion, Wound healing, Wound closure
Various wound closure techniques are available to the reconstructive surgeon. Logic dictates that the closure choice should start with the simple approach, if applicable, while the surgeon bears in mind that in certain circumstances, more-sophisticated techniques are needed for a better outcome. The reconstructive ladder is the spectrum of closure options available for wounds, and in the mind of the reconstructive surgeon, closure should be achieved by the simplest effective technique.
Traumatic contaminated wounds should be debrided and irrigated, their foreign bodies removed, and hemostatsis obtained in preparation for closure. Other wounds, such as iatrogenic, which may result after cancer resection, are presumed clean.
To reduce the rate of dehiscence, scaring, skin necrosis, and infection, tension should be avoided at all costs when closing a wound.
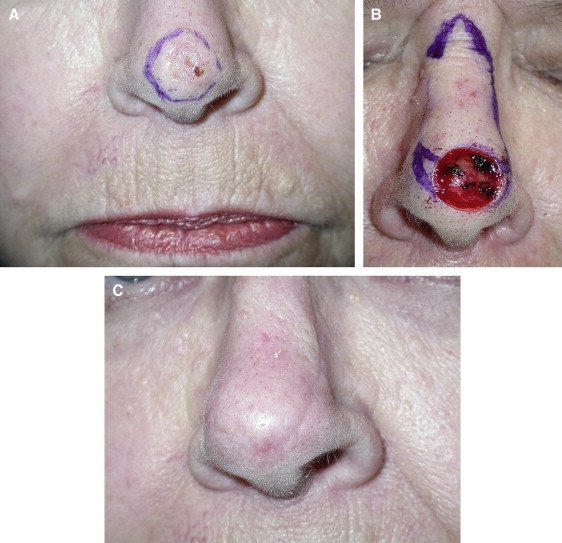
In small wounds the surgeon may choose to allow the wound to heal by secondary intention. This is done by keeping the wound clean and covered with topical antibiotic, if an infection is suspected, or hydrogel and dressing (Figure 1).1
Figure 1.
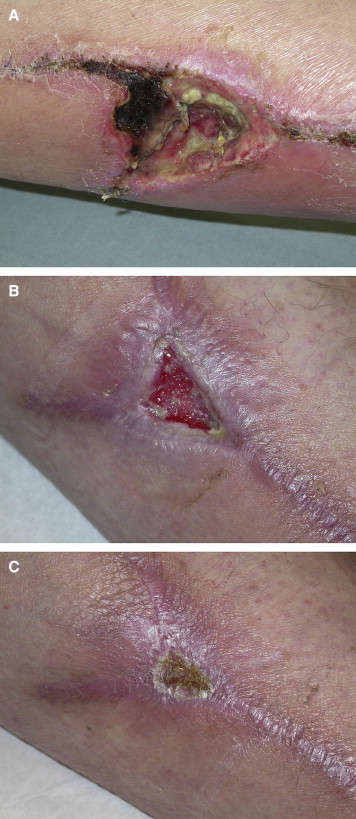
Healing Secondary Intention. A, Necrotic wound after attempted primary closure. B, Healing wound by secondary intention. C, Healed wound by secondary intention after 2 months.
Primary Closure
After the operative site has been prepped and anesthetized, the wound edges are approximated and closed with sutures. Traumatic wounds are debrided, and the edges of the wound are trimmed and closed. When dealing with skin cancer, after the completion of the excision, the defect is closed respecting the same principals (Figure 2). To minimize tension on closure and cancel dead space, buried dermal sutures are placed. Sutures at skin level are removed early, a measure facilitated by a secure dermal closure with absorbable sutures. To maintain skin apposition, the sutures are removed, and Steri-Strips are applied. In general, facial sutures are removed in 3 to 7 days; scalp, 7 to 10 days; and lower extremity and trunk, 10 to 14 days. The suture line is placed in a natural skin wrinkle line if possible to camouflage the closure line.2
Figure 2.
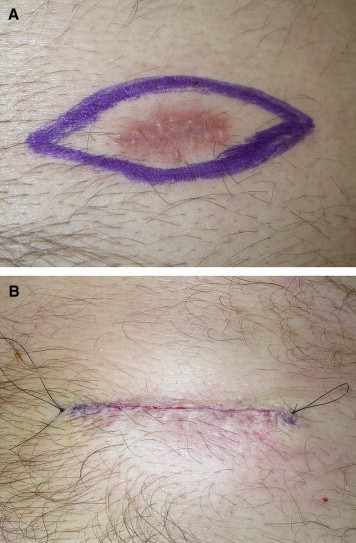
Primary Closure. A, Preoperative marking for basal cell carcinoma excision. B, Postoperative view after excision and primary closure of resulting wound.
Skin Grafts
When primary closure is not possible because of an exceedingly large defect, a skin graft is available to cover the wound. Smaller wounds, especially on the face, should be closed with a full-thickness skin graft. This contains epithelium and a full thickness of dermis. The donor site is closed primarily. Preauricular and postauricular skin and supraclavicular, inguinal, and antecubital skin are all examples of donor sites (Figure 3). A full-thickness skin graft contracts less, and because it isn't as readily available in large quantities, it is reserved for relatively small defects, such as some on the as face and hands, to provide better functional results. Grafts in general are placed over the prepared wound bed and secured with a bolster dressing for 5 to 7 days to ensure contact with the recipient bed. Split-thickness skin grafts are reserved for large wounds and contain epithelium and variable amounts of dermis. The donor site heals spontaneously by epithelialization. Thigh, buttocks, and trunk are all examples of donor sites (Figure 4).3–5
Figure 3.
Full-Thickness Skin Graft. A, Preoperative view of left infraorbital defect after basal cell carcinoma excision. B, 6 month Postoperative view after full thickness skin graft harvested from left supraclavicular area.
Figure 4.

Split-Thickness Skin Graft. A, Preoperative view of left shoulder fibrohistiocytoma. B, Postoperative view at 1 week, after excision and split thickness skin graft harvested from left thigh. C, Postoperative view at 1 month. D, Postoperative view at 1 year.
Flaps
Flaps are tissue transferred from its bed to an adjacent area while retaining its vascular attachment. Arterial-venous vessels remain in their native bed in a pedicled flap or are anastomosed by microvascular technique in free flap.
Types of flaps include skin flaps, muscle flaps, musculocutaneous flaps, fascial flaps, fasciocutaneous flaps, and osteocutaneous.
Skin flaps may also be classified as local or distant. Local flaps include transposition flaps, interpolation flaps, and advancement flaps (V-Y or rectangular). A rotation flap is a semicircular flap of skin and subcutaneous tissue that is rotated about a pivot point into the defect (Figure 5).
Figure 5.
Local Flaps. A, Preoperative view of stage IV sacral pressure wound. B, Postoperative view of right gluteal fasciocutaneous rotational flap closure.
A transposition flap, such as a rhomboid flap, is elevated and transposed into an adjacent defect. The donor site is closed primarily or skin grafted. An advancement flap is raised and advanced into the defect in a straight line (Figure 6). The degree of advancement depends on the amount of stretching of the skin. A rectangular flap and a V-Y advancement flap are examples of these types of flaps.2
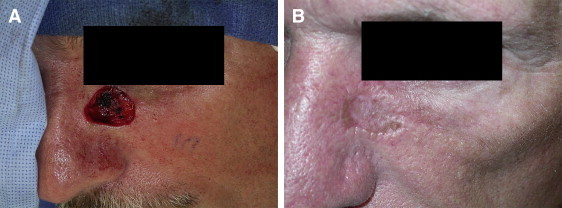
Figure 6.
Local Flaps. A, Preoperative view nasal tip basal cell carcinoma. B, Intraoperative view after basal cell carcinoma excision and dorsal nasal flap design. C, Final result after wound reconstruction with an advancement dorsal nasal flap.
Distant/Rotational flaps with direct transfer are performed by the flap being raised based on a pedicle, which brings blood supply, and being placed to cover the defect. Local vessels grow into the flap, which no longer depends on its pedicle, by inserting the flap into the defect (Figure 7). The groin flap for the reconstruction of hand defects and the forehead for the reconstruction of nasal defects are examples of this kind of flap.2
Figure 7.
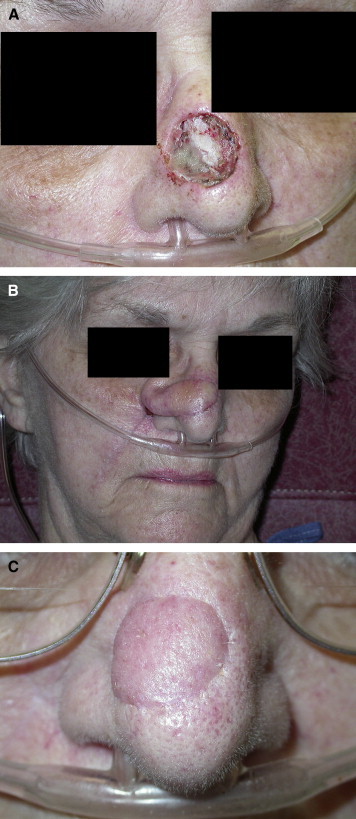
Distant/Regional Flaps. A, Right nasal side wall Mohs defect after squamous cell carcinoma excision. B, First stage reconstruction using right nasal labial fold pedicle flap. C, Final result after second stage reconstruction including division and inset of flap.
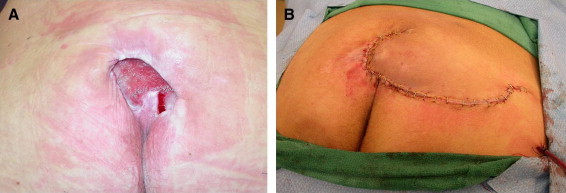
Tissue Expansion
Skin responds to mechanical stress when it is applied. During pregnancy the lower abdominal skin responds rapidly to expansion. By expanding local skin surrounding the defect, wound coverage is provided with tissue that carries similar color and texture without compromising the donor area. The tissue expander is placed adjacent to the future defect when a congenital birth mark or burn scar is excised. When the target column is reached, the device is removed, and the skin is advanced in the wedge for coverage.3,6 The device is placed under the muscle and skin when a breast is reconstructed after mastectomy. When the target volume is reached, the expander is removed and replaced with a permanent saline implant (Figure 8).2
Figure 8.
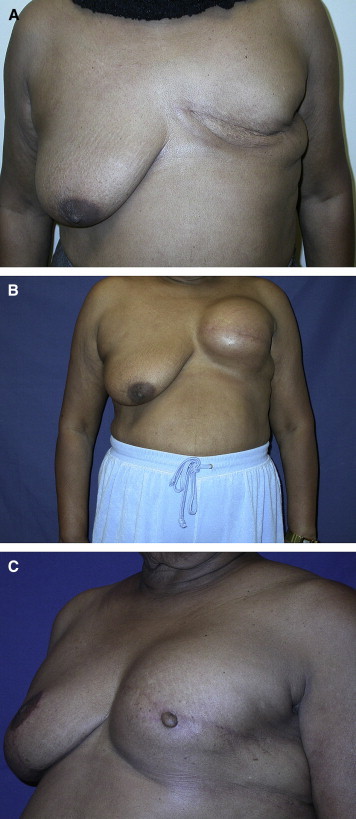
Tissue Expander. A, Preoperative view after left breast mastectomy. B, Postoperative view of left breast reconstruction with tissue expander. C, Final result after left breast tissue expander exchange with saline implants, left nipple reconstruction and right breast mastopexy to achieve symmetry.
Free Tissue Transfer and Microsurgery
A free flap contains a mass of tissue, with its vascular pedicle, that is transferred surgically from its native body location to a distant defect recipient site where vessel continuity is restored by microvascular anastomosis. This free flap is indicated when a large defect is seen with or without bone, vessel, or nerve exposure in an area where local pedicle flaps are unavailable or too small to cover a large defect (Figure 9).2,7
Figure 9.
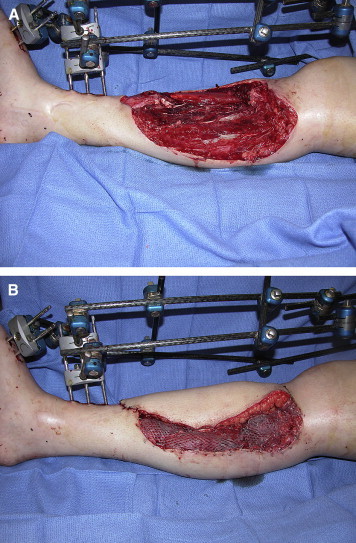
Free Flap. A, Preoperative view of high-impact accident with comminuted tibial and fibular bone fracture and significant soft tissue loss (Gustillo IIIB; courtesy of Jessie Taylor, MD, University of Cincinnati, Plastic Surgery). B, Postoperative view of anterolateral thigh free tissue transfer to cover defect (courtesy of Jessie Taylor, MD, University of Cincinnati, Plastic Surgery).
Postoperative Surgical Considerations
Immobilization of a wound site while a skin graft is taking is crucial for adherence and neovascularization. Sliding or direct pressure can cause separation of a graft from its vascular bed. This separation can be complicated by seroma, hematoma, fibrin, or purulent secondary effects. There are many methods of immobilization: splinting, restricted motion, bolster dressing, negative pressure therapy dressing and pinning, or external fixation. A sterilized wound bed and antibiotics may be needed to prevent skin graft loss from infection.
Suture selection is important. The time needed for collagen deposition must be considered. Suture or staple removal is dependent on the particular wound site. Sites of dependency and pressure-bearing areas need at least 6 weeks of wound closure to reach 60% tensile before any stress to the incision line is attempted. At 3 weeks tensile strength is approximately 30%, which is enough for suture or staple removal for major trunk and upper extremity reconstructions. On the face and neck and areas where aesthetic appearance of a scar is a factor, sutures may be removed in 5 to 7 days if layered dermal closure was performed.
Flap or skin graft failure proceeds through an orderly series of events. Cardinal signs of flap failure include the following:
swelling (hyperpermability)
erythema (hyperemia)
cyanosis (venous congestion)
epidermolysis (partial-thickness necrosis)
demarcation necrosis (full-thickness necrosis)
wound separation (loss of vascularity and fibrin/collagen attachments)
Conclusion
Successful wound closure requires deep understanding of wound physiology, anatomy, and healing phases of wounds. Applying these principles will minimize complications and lead to better results. Diabetes control, nutrition status, infection control, mechanical stress, and good nursing are all relevant when dealing with acute and chronic wounds.
References
- 1.Cohen I.K., Digelmann R.F., Cindbald W.I. Wound Healing: Biochemical and Clinical Aspects. Saunders; Philadelphia, PA: 1992. [Google Scholar]
- 2.Grabb and Smith's Plastic Surgery. 5th ed. Lippicott Raven, Aston, Bessley, Thornton, 1997. 13–25.
- 3.Herndon D.N., editor. Total Burn Care. Saunders Co; Philadelphia, PA: 1996. [Google Scholar]
- 4.Smahel J. The healing process in skin grafts. Clin Plast Surg. 1977;4:409–424. [PubMed] [Google Scholar]
- 5.Grabb W.C. Basic techniques of plastic surgery. In: Grabb W.C., Smith J.W., editors. Plastic Surgery. 3rd ed. Little, Brown; Boston, MA: 1979. pp. 1–30. [Google Scholar]
- 6.Argenta L.C., Marks M.W., Pasyk K.A. Advances in tissue expansion. Clin Plast Surg. 1985;12:159–171. [PubMed] [Google Scholar]
- 7.Kroll S.S., Schusterman M.A., Reece G.P. Choice of flap and incidence of free flap success. Plast Reconst Surg. 1996;98(3):450–463. doi: 10.1097/00006534-199609000-00015. [DOI] [PubMed] [Google Scholar]


