Abstract
Traditionally, wound closure sutures have in common the need to tie knots with the inherent risk of extrusion, palpability, microinfarcts, breakage, and slippage. Bidirectional barbed sutures have barbs arrayed in a helical fashion in opposing directions on either side of an unbarbed midsegment. This suture is inserted at the midpoint of a wound and pulled through till resistance is encountered from the opposing barbs; each half of the suture is then advanced to the lateral ends of the wound. This design provides a method of evenly distributing tension along the incision line, a faster suture placement and closure time with no need to tie knots, and the possibility of improved cosmesis. Bidirectional barbed sutures, which are available in both absorbable and nonabsorbable forms, can be used for simple closures, multilayered closures, and closure of high-tension wounds in a variety of surgical settings.
Keywords: Bidirectional barbed sutures, Wound closure
Introduction
Fundamentally, little has changed over many decades with regard to the method of approximating tissues that have been separated as a result of trauma or separated surgically (for excision of lesions of the skin and/or for access to deeper structures). For several centuries, wounds were sutured through rudimentary but effective methods. Cardinal events that have occurred in the history of sutures include (1) the ability to sterilize catgut; (2) the development of various polymers that were used for construction of the suture material; (3) the development of absorbable and nonabsorbable suture materials; (4) recognition of the value of monofilament and braided sutures and the relative indications for each; and (5) the ability to swedge needles directly on the end of the suture, eliminating the need to thread the suture through the eye of the needle. More recently, alternate methods of approximating wounds have also been developed, including staples, adhesives, and clips.
One important feature of conventional sutures is that they require the tying of knots to secure the closure. Complications of knot tying are well recognized. Knot tying requires time and training. Knots may break and slip. Knots may extrude. Infection related to knots is frequently seen when braided sutures are used. Wound tension with traditional sutures when the tension is not uniformly distributed throughout the length of the closure can result in tissue ischemia and unfavorable scarring. Excessive tension can also result in reduced wound strength, inflammation, and dehiscence.1 Excessive tension occurs at the individual suture loops, providing an opportunity for focal ischemia. Pressure-induced ischemia and necrosis predispose the wound to infection and are the principal factors leading to wound dehiscence.2
It follows that a suture that does not require the tying of knots would offer significant advantages, avoiding all of the possible complications described above. To this end, various suture modifications (eg, sutures with cones, sutures with large anchor knots) have been studied.3,4 However, it was the development of barbed sutures that proved to be a particularly important evolutionary step in providing a technology that would avoid the need to tie knots. Early designs that used unidirectional barbs were abandoned because a single knot was still required at one end to secure the suture. This problem was solved with the advent of the bidirectional barbed suture. The bidirectional technology was first adopted by plastic surgeons for use in various minimally invasive percutaneous rejuvenation procedures to lift ptotic tissues, including the brow, midface, and neck.3,4 While these sutures continue to be used by plastic surgeons for tissue suspension in open aesthetic procedures with extensive dissection, they are rarely used in closed procedures primarily because of the limited longevity of results and a consequent failure to meet patients' expectations. In recent years, it has become apparent that the unique features of the self-anchoring bidirectional barbed suture are particularly well suited for the purposes of wound closure in a number of different surgical applications. The advantages of this design for tissue approximation include no need for an assistant's hand to follow the suture placement, more rapid deployment of the sutures, even distribution of tension along the incision line, and the possibility of improved cosmesis.
In 2007, absorbable and nonabsorbable bidirectional barbed sutures (Quill SRS, Angiotech Pharmaceuticals, Vancouver, British Columbia, Canada) received US Food and Drug Administration clearance for use in approximating soft tissues (Figure 1). Extensive preclinical testing by Gregory Ruff, M.D. and colleagues has ensured that the tensile strength of these materials provides sustained soft tissue approximation and that the absorption curve is compatible with the time that is required to allow collagen deposition, ensuring the integrity of the soft tissue approximation.5 Barb morphology influences holding and tensile strength. It follows that the deeper the barb is cut, the lower the tensile strength. A novel helical design in the placement of the barbs supports the concept of better tissue adherence to the barbs. Gradients of tension and compression are created by using a bidirectional barbed suture (Figure 2).5 In addition, using smaller diameter needles results in better adherence of the soft tissue to the barbs because a wider channel is not produced by a larger diameter needle. Animal studies to investigate closure of dermal and abdominal wall (ie, deep fascial) tissues confirmed that knotless barbed sutures provide the same in vivo wound security as do conventional sutures that are 1 size smaller.6 The suggestion was made by the author that cosmesis may be improved by eliminating knots that could serve as a source for a foreign body reaction. This issue may be of particular relevance to knots placed in the subcutaneous layers, where foreign body reactions are more commonly in evidence.
Figure 1.

Bidirectional Barbed Suture Reprinted with permission from Angiotech Pharmaceuticals, Inc.
Figure 2.
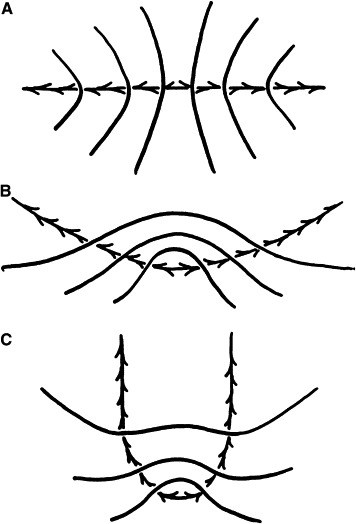
A, Linear compression at the point where the barbs change direction. B, Arcuate placement imparts a mound by adding a vertical vector to the horizontal vector. C, U-shaped deployment results in the forces on the barbs being opposed by the bend in the U (rather than the opposing barbs). Reprinted with permission from Elsevier Inc.
The one clinical study that has been conducted to date with the bidirectional barbed suture was a prospective, randomized controlled noninferiority study intended for submission to the U.S. Food and Drug Administration.2 A comparison with conventional 3-0 polydioxanone sutures was conducted in 188 evaluable subjects undergoing dermal closure of the Pfannenstiel incision during nonemergent cesarean delivery. In this context, the bidirectional barbed size 0 polydioxanone suture proved to be noninferior to the conventional suture in terms of cosmesis, closure time, and safety outcomes. No other clinical study data with this product have been published. The methodology that follows, summarizing the various wound closure techniques and applications for bidirectional barbed sutures, is based on the personal experience of the author and that of a handful of other surgeons who have published their experiences with this novel product. Illustrations to support the text were downloaded with permission from the manufacturer's Web site for health care professionals.
Methodology
General Description
The bidirectional suture has barbs that are aligned in a helical pattern and proceed in opposite directions from a small central nonbarbed segment. A needle is attached at each end of the suture. The suture is available in both absorbable (polydioxanone; a polyglycolide-poly-e-caprolactone copolymer) and nonabsorbable (polypropylene; nylon) formats and in various lengths with various needle sizes. When the suture is inserted in the center of the wound and begins its journey to the lateral end of the wound, each sequential suture placement produces an engagement of the barbs, equally distributing the tension along the entire length of the closure. The suture self-locks as soon as it is advanced past the nonbarbed segment. After the wound is completely closed, the needle can be returned in a J-loop fashion or allowed to exit the skin about 1 cm to 2 cm lateral to the wound edge, where it is cut off flush, while the skin is pushed inward so that the end disappears below the dermis. It is important to note that a third hand is not required as the suture is self-anchoring.
On first use, the surgeon may inadvertently exert excessive tension when advancing the suture and create bunching of the tissue. Should this occur, the midsegment can be cut and the suture halves can readily be removed and the barbs disengaged by pulling gently on the lateral ends. As with all surgical procedures, placement of the barbed suture is a learned technique. The skill of exerting adequate tension while avoiding undue stress is one that is gained relatively quickly—in this author's experience, within1 or 2 attempts.
Wound Closure Techniques
-
1.
Simple wound closure: When only the full thickness of the skin and subcutaneous fat is to be approximated, an absorbable bidirectional suture can be passed from the center of the wound to each end, exiting about 1 cm from the wound edge. The suture is cut flush with the skin at each end (Figure 3).7
-
2.
Multilayered wound closure: This includes the full thickness of the skin, subcutaneous fat, and superficial fascia, with or without the deep fat. These layers are closed in a manner similar to that described under “simple would closure,” with the addition of a second bidirectional suture for the deep layer. At each end of the deep layer closure, a J-loop ensures good wound approximation (Figure 4).7
-
3.
Wounds with excessive tension: When there is excessive tension, closure in 2 directions effectively distributes the tension by first passing a straight needle with one-half of the barbed suture and traversing the wound that has been divided into equal segments. The other half goes in the opposite direction. The standard wound closure continues in the direction of the wound at right angles to the first suture placement (Figure 5).7
Figure 3.
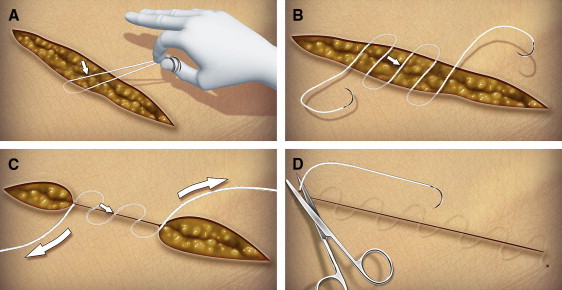
Simple Wound Closure With Bidirectional Barbed Suture. A, Start by taking one end of the suture and pulling it through until the transition zone has reached the tissue. Estimation of the center of the device can be aided by taking a single bite of tissue, then aligning the 2 needles until both ends of the suture are of roughly equal lengths. B, Taking one arm of the suture, complete at least 2 loose arcs through the tissue, then take a few tissue bites with the other arm of the device. C, Once at least 2 arcs per side have been deployed, each of the strands can be grasped and the tissue approximated to the desired tension. Continue the bites sinusoidally until the end of the wound is reached. D, Take the last bite 2 cm beyond the end of the wound, exiting through the skin. Repeat the technique on the opposite side. Push down on the tissue and cut the device and needle flush with the skin. Reprinted with permission from the manufacturer.
Figure 4.
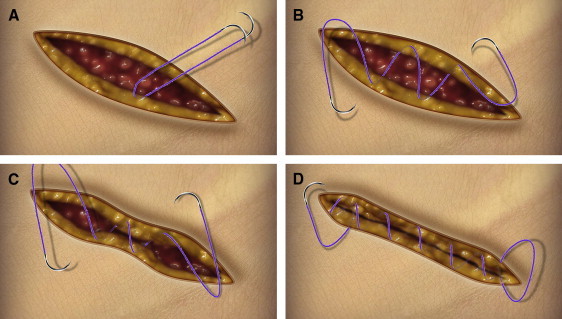
Deep Multilayered Wound Closure With Bidirectional Barbed Suture. A, Start at the midpoint. Using a helical suturing technique, pass the first needle through the tissue until the midpoint is reached. The midpoint can be approximated by roughly aligning the needles together as illustrated. Do not pass the first needle beyond the midpoint. B, Take at least 1 more pass with the first needle, followed by at least 2 loose passes with the second needle. C, Once each needle has been loosely passed at least twice, approximate the wound by pulling on both ends of the suture. Based on surgeon experience and the particular configuration used, some surgeons may find it unnecessary to loosely pass both needles twice before approximating the wound. D, Continue closing the deep layer with each needle, securing the ends by employing a backstitch within the wound margin. When approximation is complete, simply cut off the excess; there is no need to tie knots. Reprinted with permission from the manufacturer.
Figure 5.
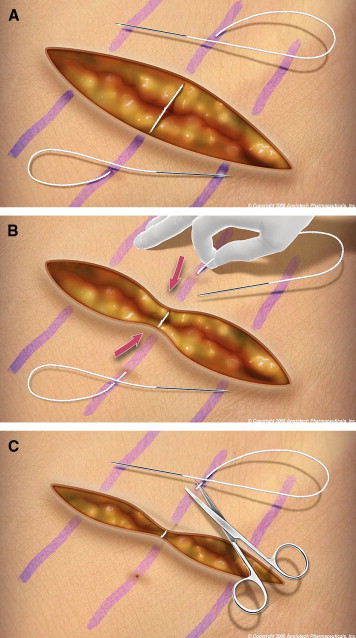
High-Tension Closure With Bidirectional Barbed Suture. A, Mark the vector lines of the suture at 5-cm intervals. Insert the needle from either side of the wound through the full thickness of the wound, exiting the skin at least 3 cm from the border of the wound. B, Hold tension on the device and ratchet the wound edges close together. C, Repeat the procedure until the wound is an optimal size. Close the wound in layers as shown in Figure 4, discarding the ends of the suture and the attached needles. Reprinted with permission from the manufacturer
Surgical Applications
There are several applications for these bidirectional barbed sutures.
-
1.
Emergency room applications: The ability to close multiple wound layers with a running barbed suture can significantly decrease the time required for closure, most notably in the case of deeper and larger wounds.
-
2.
General and thoracic applications: Laparotomy and thoracotomy incisions can be closed efficiently and securely with the use of barbed sutures. In fact, cadaver work has demonstrated that it is virtually impossible to pull apart the posterior rectus sheath after repair with the bidirectional barbed sutures. The attachment of the soft tissue to the barbs and the equal distribution of tension along the incision line are effective in providing a strong resistance to wound separation.
-
3.
Urologic applications: There has been an impressive increase in the number of robotic prostatectomies that have been performed. The strength of barbed sutures in performing vesicourethral anastomosis with the goal of a watertight seal and resistance to disruptive forces has been studied, and the benefits of the barbed sutures have been validated.8 When the security of the vesicourethral anastomosis was tested by cutting every fourth loop of the 12-loop closure, there was no discernable change in the security of the bidirectional barbed closure, whereas there was complete disruption of closure performed with a standard running suture.8 In addition, an in vivo and in vitro study of urinary tract reconstruction in the porcine model found that self-anchoring sutures (barbed suture configuration) provide the same secure tissue approximation as standard tied sutures do. The authors also concluded that the self-anchoring system eliminates the need for knot tying and provides a watertight anastomosis.9
-
4.
Orthopedic and hand applications: The ability to avoid knot tying through an arthroscope has obvious advantages, including faster tying and no need to manipulate complex instruments. An ex vivo study using the barbed suture for tenorrhaphy showed that a 6-core barbed suture repair showed markedly increased tensile strength compared with a 4-core cruciate control.10
-
5.
Obstetrical and gynecologic open and laparoscopic applications: The ability to quickly and effectively repair cesarean section (ie, the Pfannenstiel incision)2 and laparotomy incisions and the clear advantage of suturing through a laparoscope with a material that does not require the tying of knots are important benefits of barbed suture technology. Closing the vaginal cuff during total laparoscopic hysterectomy is facilitated with the use of barbed sutures.11 And, in their case series of 5 laparoscopic myomectomies, Greenberg and Einarsson noted that the barbed suture was particularly advantageous in reapproximating the myometrium.11 In contrast to what was seen when a traditional closure was performed with standard sutures, as expected, no knot tying was required. In addition and of particular interest, once the bidirectional barbed suture had passed through, the tissue remained approximated without recoil and without any need for further tension to be applied. It is anticipated that this benefit, first reported in a gynecologic procedure, will prove to be widely applicable to a range of laparoscopic surgeries.
-
6.
Plastic and reconstructive applications: There have been numerous applications in the plastic surgery literature, including facial cosmetic surgery,12 breast surgery, and body contouring. The speed of placement and the avoidance of knots or a purse-string effect (face and breast) are obvious advantages. In a recently completed preliminary investigation of closures of 3 basic aesthetic procedures, this author and colleagues found evidence of a significant reduction in time to closure with a bidirectional barbed suture technique compared with a traditional suture technique. Each procedure (abdominoplasty, brachioplasty, mastopexy) required closure of 3 layers: the superficial fascia/deep tissue, deep dermis, and superficial dermis. With traditional wound closure techniques, separate sutures were required for each of the 3 layers. With bidirectional barbed sutures, the 3 layers were closed with 2 running sutures. The closures were performed by a junior plastic surgery resident, a senior plastic surgery resident, and a senior plastic surgery professor; each surgeon served as his own control. In each case, regardless of the level of training, overall closure times were reduced by approximately 50% when bidirectional barbed sutures were used (Figure 6). While these data appear promising, they are based on a small sample, and therefore caution is warranted in their interpretation.
-
7.
Hair restoration applications: Bidirectional barbed sutures have also been reported to be of value for the closure of the hair restoration graft donor site at the occipital scalp.13,14 Using a layered closure technique, first of the occipitalis fascia, followed by the subcuticular layer, surgeons markedly reduced closure times compared with their experience with traditional closures. Donor strips up to 26 cm in length have been successfully closed with this technique.
Figure 6.
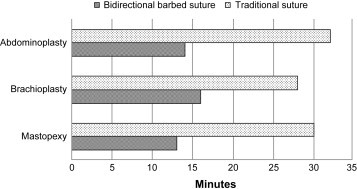
Mean Time to Closure With Bidirectional Barbed Suture and Traditional Suture Techniques. Each procedure required closure of 3 layers: the superficial fascia/deep tissue, deep dermis, and superficial dermis. Closures were performed by a junior plastic surgery resident, a senior plastic surgery resident, and a senior plastic surgery professor, each serving as his own control.
Complications and Contraindications
Complications that have been reported with use of bidirectional barbed sutures include extrusion and, in rare cases, infection. Cases of extrusion have been observed when sutures, size 2.0 or greater, have been placed too close to the superficial dermis. As a result, it is recommended that smaller sutures be used for this type of closure. No cases of infection related to use of any of the nylon, polypropylene, or absorbable polyglycolide-poly-e-caprolactone copolymer formulations of the suture have been reported to the manufacturer. The complaints of infections that have been received relate to the absorbable polydioxanone formulation. To date, the confirmed infection rate based on reported complaints is 0.05%, which falls well within the range of published infection rates for surgical site infections.15-17 Given that complaints of infection with this product have occurred most commonly in cases in which a larger caliber suture has been used and when the suture has been placed too superficially, an alternative absorbable formulation (the polyglycolide-poly-e-caprolactone copolymer formulation) was developed and is available as an option to be used in appropriate cases for the closure of superficial layers. In any case, should a bidirectional barbed suture become infected, it can readily be removed without damaging the tissue. The suture should be cut at the unbarbed midsegment. In this way, tension from the opposing barbs is released. Either 1 or both suture halves can then be removed by pulling gently from the lateral ends. Sutures that have been inadvertently placed with excess tension can be removed in a similar fashion.
The absorbable formulations of the bidirectional barbed sutures are contraindicated in closures where prolonged approximation of tissue under stress is required; in addition, they are not to be used for fixation of nonabsorbable prosthetic devices. Both polypropylene and nylon nonabsorbable formulations are contraindicated for surface closures through the epidermis. Of the 2 nonabsorbable formulations, the nylon sutures are also contraindicated for use where permanent retention of tensile strength is required since gradual loss of tensile strength has been observed in vivo over prolonged periods. Adverse effects that have been associated with this product include wound dehiscence and failure to provide adequate support for the wound closure. Complete contraindications, warnings, precautions, and adverse reactions are listed in the product instructions for use.
Cost Considerations
As a novel technology, the bidirectional barbed suture is more expensive than is traditional suture material. However, at least in the case of a simple closure, it is intuitive that, since a single suture can be used and no knot tying is required, less material would be needed than if a traditional suturing technique was used. In addition, in this author's experience with plastic surgery applications, there are also considerable time savings associated with the bidirectional barbed suture—in the range of 50% for the closure itself, with a savings in overall operative time of between 25% and 30%. No doubt, these savings in time will have cost implications. To date, no direct cost comparisons have been published. It is anticipated that economic evaluations of this technology will begin to appear in the literature within the next year.
Summary
The introduction of the bidirectional barbed suture has resulted in a paradigm shift in how wounds may be closed. Eliminating knot tying, speeding the placement of the sutures, eliminating the need for an assistant's hand to follow the suture placement, enhancing the equal distribution of tension, and creating the possibility of improved scar cosmesis are compelling validations of this emerging technology, which arguably may be the most important recent advancement in suture technology, with clear benefits to the patient and to the surgeon.
Footnotes
Conflict of interest and financial disclosure statement: The author is a paid consultant to Angiotech Pharmaceuticals, Inc., the manufacturer of Quill SRS, and receives a monthly stipend.
References
- 1.Leung JC. Barbed suture technology: Recent advances. Medical Textiles 2004, Advances in Biomedical Textiles and Healthcare Products, Conference Proceedings, Pittsburgh, Pennsylvania. IFAI Expo 2004, October 26-27, 2004, p. 62–80.
- 2.Murtha A.P., Kaplan A.L., Paglia M.J., Mills B.B., Feldstein M.L., Ruff G.L. Evaluation of a novel technique for wound closure using a barbed suture. Plast Reconstr Surg. 2006;117:1769–1780. doi: 10.1097/01.prs.0000209971.08264.b0. [DOI] [PubMed] [Google Scholar]
- 3.Matarasso A., Pfeifer T.M. The use of modified sutures in plastic surgery. Plast Reconstr Surg. 2008;122:652–658. doi: 10.1097/PRS.0b013e3181773982. [DOI] [PubMed] [Google Scholar]
- 4.Villa M.T., White L.E., Alam M., Yoo S.S., Walton R.L. Barbed sutures: A review of the literature. Plast Reconstr Surg. 2008;121:102e–108e. doi: 10.1097/01.prs.0000299452.24743.65. [DOI] [PubMed] [Google Scholar]
- 5.Ruff G. Technique and uses for absorbable barbed sutures. Aesthetic Surg J. 2006;26:620–628. doi: 10.1016/j.asj.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Rodeheaver GT, Pin˜eros-Fernandez A, Salopek LS, Rodeheaver PA, Leung JC, Ruff GL, Batchelor SD. Barbed sutures for wound closure: In vivo wound security, tissue compatibility and cosmesis measurements. Society for Biomaterials 30th Annual Meeting, April 27–30, 2005, Memphis Cook Convention Center, Memphis, TN, USA. Joel D. Baumgardner, program chair. Meeting Transactions. Transaction 229, p. 232.
- 7.Paul M.D., Avelar R. 2nd ed. Angiotech Pharmaceuticals; Vancouver, BC, Canada: 2008. Quill™ SRS. Techniques and Procedures. A Novel Approach to Soft Tissue Approximation. [Google Scholar]
- 8.Moran M.E., Marsh C., Perrotti M. Bidirectional-barbed sutured knotless running anastomosis v classic van Velthoven in a model system. J Endourology. 2007;21:1175–1178. doi: 10.1089/end.2007.9913. [DOI] [PubMed] [Google Scholar]
- 9.Weld K.J., Ames C.D., Hruby G., Humphrey P.A., Landman J. Evaluation of a novel knotless self-anchoring suture material for urinary tract reconstruction. Urology. 2006;67:1133–1137. doi: 10.1016/j.urology.2005.12.022. [DOI] [PubMed] [Google Scholar]
- 10.Parikh P: Barbed suture tenorrhaphy: An ex-vivo biomechanical analysis. Abstract available at http://www.aaps1921.org/abstracts/2008/7.cgi. Accessed March 4, 2009. [DOI] [PubMed]
- 11.Greenberg J.A., Einarsson J.I. The use of bidirectional barbed suture in laparoscopic myomectomy and total laparoscopic hysterectomy. J Minim Invas Gynecol. 2008;15:621–623. doi: 10.1016/j.jmig.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Paul M.D. Barbed sutures for aesthetic facial plastic surgery: Indications and techniques. Clin Plastic Surg. 2008;35:451–461. doi: 10.1016/j.cps.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Recasens J. Knotless, layered, single-suture skin and scalp closure. Cosmetic Dermatol. 2008;21:236–237. [Google Scholar]
- 14.Pak J.P., Rassman W.R., Gazoni P., Zeballos A. Management of the occipital scalp tension wound in hair transplant surgery with the Quill suture. Hair Transplant Forum International. 2008;July/Aug:149–150. [Google Scholar]
- 15.Gaynes R.P., Culver D.H., Horan T.C. Surgical site infection (SSI) rates in the United States, 1992-1998: The National Nosocomial Infections Surveillance System Basic SSI Risk Index. Clin Infect Dis. 2001;33(Suppl 2):S69–S77. doi: 10.1086/321860. [DOI] [PubMed] [Google Scholar]
- 16.NNIS System National Nosocomial Infections Surveillance (NNIS) System report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32:470–485. doi: 10.1016/S0196655304005425. [DOI] [PubMed] [Google Scholar]
- 17.Edwards J.R., Peterson K.D., Andrus M.L. National Healthcare Safety Network (NHSN) report, data summary for 2006 through 2007, issued November 2008. Am J Infect Control. 2008;36:609–626. doi: 10.1016/j.ajic.2008.08.001. [DOI] [PubMed] [Google Scholar]


