Abstract
Purpose
Hemiarthroplasty (HA) is an established treatment for femoral neck fractures of the elderly. Several surgical approaches are currently used including dorsal and transgluteal. It is still unclear whether one approach may be advantageous. We compared early complication rates after dorsal and transgluteal approaches.
Methods
We retrospectively analysed a cohort including 704 consecutive patients who received HA for femoral neck fracture; 212 male and 492 female patients were included, and the mean age was 80.4 years (SD 9.8 years). In 487 patients a dorsal and in 217 a transgluteal approach was chosen. In all patients an Excia® stem with self-centring bipolar head manufactured by Aesculap (Tuttlingen, Germany) was used. We evaluated early postoperative complications including dislocation, infection, haematoma, seroma and perioperative fracture. Complication rates after dorsal and transgluteal approaches were calculated and compared by the chi-square test.
Results
After a dorsal approach 10.5 % [confidence interval (CI) 7.7–13.2 %] of the patients suffered one or more early complications. Following a transgluteal approach this proportion was 9.7 % (CI 5.7–13.6 %), which was not significantly different (p = 0.75). The predominant complication after a dorsal approach was dislocation (3.9 %; CI 2.2–5.6 %). The dislocation rate after a transgluteal approach was significantly lower (0.5 %; CI 0–1.4 %). Postoperative haematoma however was seen after a transgluteal approach in 5.5 % (CI 2.5–8.6 %), which was significantly more frequent than after a dorsal approach (1.2 %; CI 0.2–2.2 %). The frequency of the other types of complications did not significantly differ.
Conclusions
The rate of early surgical complications after dorsal and transgluteal approaches is not significantly different. However, the dorsal approach predisposed to dislocation, whereas the transgluteal approach predisposed to haematoma.
Introduction
Hemiarthroplasty (HA) is a common method for the treatment of displaced femoral neck fractures. Since octogenarians are predominantly affected [1], the outcome of this operative procedure is interesting especially in orthogeriatrics. Different operative techniques are described in the literature. However, some questions concerning benefits of different approaches, complication rates, fixation (cementless vs cemented), implant design (bipolar vs monopolar) and others are not completely resolved [1–4].
In particular, the different approaches and their respective advantages are still not resolved. Recently some less invasive modifications have been described and compared to the standard approaches such as Kocher-Langenbeck (dorsal), Bauer or Hardinge (lateral), Watson-Jones (anterolateral) and Smith-Peterson (anterior). All of them seem to have several advantages and every modification leads to different new problems [5–9].
Most studies comparing surgical approaches include only total hip arthroplasty (THA) and are not necessarily valid for HA. Following THA several studies showed a lower dislocation rate after the transgluteal approach compared to the dorsal approach [10–14]. Unfortunately most publications focus only on dislocation rate. This has to be regarded as a limitation, since all types of complications should be evaluated when investigating surgical techniques.
Other kinds of complications such as infection, haematoma, seroma and intraoperative fracture may also cause major problems to the patient and eventually lead to revision surgery.
The aim of this study is to perform a thorough evaluation of relevant early surgical complications in patients being treated with HA after femoral neck fracture, comparing the dorsal approach to the transgluteal approach. The results are needed in order to help orthopaedic surgeons to decide about the surgical approach when treating patients in orthogeriatrics, where studies about this topic are lacking.
Materials and methods
Study design
This study analyses a prospectively documented cohort including every patient treated with a hip HA at the Department of Trauma und Orthopaedic Surgery at the Klinikum Nürnberg Süd (KNS) between December 2006 and July 2011. Data were collected on 729 patients treated with HA. Any patient with femoral neck fracture was included. Exclusion criteria consisted of patients operated for hip osteoarthritis (n = 9), revision surgery (n = 13) or rare individual indications such as acetabular fracture or osteolysis (n = 3). Finally 704 patients remained in the study.
All patients received an Excia® femoral stem with self-centring bipolar head manufactured by B. Braun Aesculap (Tuttlingen, Germany). The stem was cemented in 673 cases (95.6 %), whereas 31 stems were cementless (4.4 %).
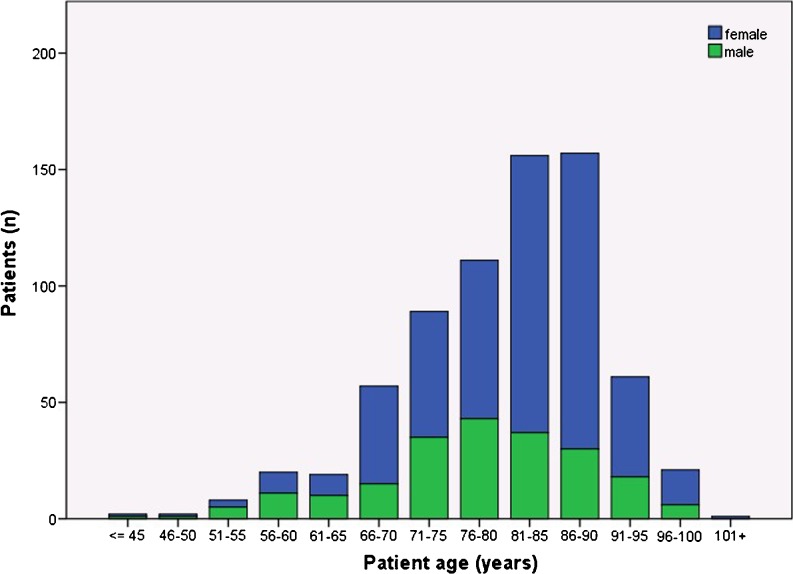
Our cohort consisted of 212 men and 492 women (30.1 vs 69.9 %). The mean age was 80.4 years (SD 9.8 years; range 41–103 years) reflecting the orthogeriatric character of this group (see Fig. 1).
Fig. 1.
Patient age and gender distribution. The majority of patients are octogenarians and women. The findings confirm that HA is typically performed in orthogeriatrics
Surgical technique and approaches
Both a dorsal and a transgluteal approach were used in our department, depending on the respective surgeon’s preference. The operations were performed by senior surgeons and by supervised residents. In total, the 704 hemiarthroplasties were performed by 49 surgeons. Regardless of the surgical approach all operations were performed under general anaesthesia with the patient positioned laterally. Single-shot cefuroxime was administered to each patient who was not allergic or under the treatment of antibiotics for another reason.
The dorsal approach was performed by a lateral incision over the greater trochanter with a slight dorsal curve cranially. The piriformis tendon was divided close to its attachment and reinserted later. The joint capsule was opened by a T-shaped incision and reconstructed by default.
The transgluteal approach was started by a straight lateral approach, dividing the M. gluteus medius longitudinally at a line dividing the width of the greater trochanter ventrodorsally by a ratio of 1:5. The vastogluteal continuity was preserved whenever possible. Joint capsule reconstruction was also part of the standard procedure.
Irrespective of the surgical approach the patients were mobilised as soon as possible, allowing for full weight-bearing. After a dorsal approach a polystyrene foam wedge was placed between and elastically attached to the patient’s legs while supine, preventing the affected hip from internal rotation.
Outcome parameters
The study focused on early surgical complications as primary outcome parameters. These included:
Arthroplasty dislocation, either occurring during inpatient treatment or causing readmission
Infection including any epifascial or subfascial wound infection needing medical or surgical intervention (e.g. administration of antibiotics, revision surgery)
Postoperative bleeding or haematoma needing revision surgery
Seroma needing surgical intervention including puncture or drainage
Fractures occurring intraoperatively or early postoperatively (e.g. shaft fragmentation, separation of greater trochanter)
Intraoperative and early postoperative mortality, defined as death during the operation or within the first 24 hours
Statistical analysis
Statistical analysis included both descriptive and inferential measures. Mean values and standard deviations were calculated for continuous variables, and frequency counts and percentages were obtained for the discrete variables. All confidence intervals (CI) are 95 % CI. The χ2 test was used for cross-tabulation analysis when all expected cell frequencies were five or greater; Fisher’s exact test was used otherwise. For continuous variables (patient age) the two-sample independent t test was used. All statistical analyses were performed with IBM SPSS Statistics Version 19.
Results
A total of 487 hemiarthroplasties were performed using a dorsal approach, whereas in 217 cases a transgluteal approach was used. There were no relevant differences between these groups regarding age, sex, indications, implant fixation (cemented vs cementless) or the implant sizes used. Of all patients, 10.2 % were affected by one or more early complications (CI 8.0–12.5 %).
The predominant complications were infection (2.7 %, CI 1.5–3.9 %), dislocation (2.8 %, CI 1.6–4.1 %), haematoma (2.6 %, CI 1.4–3.7 %), seroma (1.6 %, CI 0.6–2.5 %) and perioperative fracture (0.6 %, CI 0.0–1.1 %). Intraoperative or early postoperative death was a very rare event (0.6 %, CI 0.0–1.1 %).
Overall complication rates after dorsal and transgluteal approaches
After a dorsal approach 10.5 % (CI 7.7–13.2 %) of all patients suffered from one or more early complications. For the transgluteal approach this proportion was 9.7 % (CI 5.7–13.6 %), which did not significantly differ on χ2 test (p = 0.75).
Arthroplasty dislocation
The predominant complication after a dorsal approach was dislocation (3.9 %). The risk of dislocation was 3.4 % (CI 1.5–5.4 %) higher after a dorsal approach than after a transgluteal approach. For dislocation the odds ratio calculated was 8.8, indicating that the risk of dislocation in hemiarthroplasties implanted via a dorsal approach may be more than eightfold increased compared to those being implanted transgluteally.
Postoperative bleeding and haematoma
Postoperative haematoma occurred most frequently (5.5 %) after a transgluteal approach. After the transgluteal approach the risk for haematoma was increased by 4.3 % (CI 1.1–7.5 %) compared to the dorsal approach. The odds ratio for postoperative haematoma was 4.7, meaning that bleeding after a transgluteal approach may be about five times more likely to occur.
Infection and other complications
Regardless of the surgical approach, infection was the second most frequent complication. Other complications such as seroma and perioperative fracture were very rare. For these complications no difference between the surgical approaches could be detected (see Table 1). Intraoperative death occurred in four nonagenarians of the dorsal approach group (0.8 ± 0.8 %), but was not observed in the transgluteal approach group. This difference is not significant on Fisher’s exact test (p = 0.32).
Table 1.
Demographic and early complication data
| Dorsal approach group | Transgluteal approach group | p value | |
|---|---|---|---|
| No. of hips | 487 | 217 | |
| Age (years) | 80.4 ± 0.9 | 80.3 ± 1.3 | 0.84 (NS) |
| Sex (M/F) | 145/342 | 67/150 | |
| Lateral (high offset) shaft (%) | 2.7 ± 1.5 | 4.1 ± 2.7 | 0.30 (NS) |
| Complications | |||
| Dislocation (%) | 3.9 ± 1.7 | 0.5 ± 0.9 | 0.01 |
| Infection (%) | 2.5 ± 1.4 | 3.2 ± 2.4 | 0.57 (NS) |
| Haematoma (%) | 1.2 ± 1.0 | 5.5 ± 3.1 | 0.001 |
| Seroma (%) | 1.8 ± 1.2 | 0.9 ± 1.3 | 0.36 (NS) |
| Perioperative fracture (%) | 0.6 ± 0.7 | 0.5 ± 0.9 | 0.80 (NS) |
Discussion
The significance of early surgical complications in orthogeriatrics
To our knowledge this is the first study which takes all early complications into account when evaluating possible advantages of different surgical approaches for HA. In a large cohort we could not find a significant difference of overall complications. This study also focused on older patients after intracapsular hip fractures. These patients are at increased risk for a variety of complications, which might be divided into surgical and medical. The latter are directly associated with increased mortality and include general infections such as urinary tract infection and pneumonia, thrombosis and embolism, and delirium [15, 16]. However, these medical complications seem to be induced by immobility to a considerable extent [17, 18]. Immobility again is a consequence of early surgical complications that either directly interfere with movements (fracture, dislocation) or indirectly prevent mobilisation by necessitating further operations (infections, haematoma). This chain of cause and effect explains why early surgical complications are associated with the outcome, which is also consistent with findings in the literature [19]. Since elderly patients are even more prone to medical complications [20], any surgical complication may easily trigger further problems. Moreover, early surgical complications can be influenced most directly by the operative technique. This is why this study focused on this aspect, comparing early surgical complications after dorsal and transgluteal approaches.
Dorsal vs transgluteal approach: from the frying pan into the fire
We found no significant difference in overall complication rates comparing dorsal and transgluteal approaches (10.5 vs 9.7 %; p = 0.75). This overall complication rate seems to be high for hip arthroplasty in general. For HA in particular however these findings are consistent with the literature [21, 22], indicating a need to further optimise femoral neck fracture treatment in geriatric trauma patients.
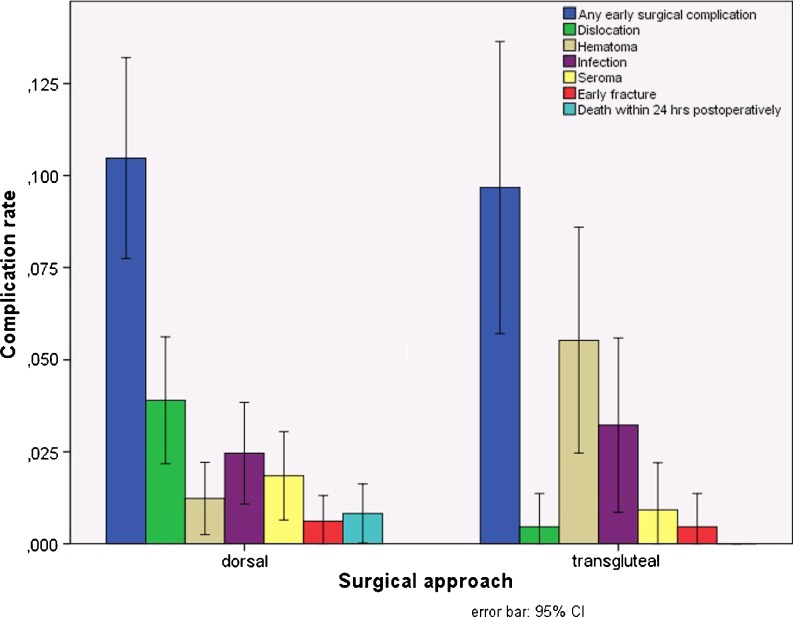
Remarkably, the patterns of early surgical complications were not equally distributed in the two groups (see Fig. 2). This was particularly true for the complications of dislocation and haematoma. Consistent with the literature [10–12, 23] we found that the risk for dislocation was reduced by 3.4 % after a transgluteal approach (3.9 vs 0.5 %). This advantage however was offset by an increase of 4.3 % in risk for haematoma needing operative intervention (1.2 vs 5.5 %).
Fig. 2.
Early surgical complications after dorsal and transgluteal approaches. The rate of patients having complications is similar after dorsal and transgluteal approaches. However, dislocation rates are higher after a dorsal approach, whereas relevant haematoma is more likely to occur after a transgluteal approach
Both types of complications may be influenced by surgical technique. Dislocation rates may be influenced by joint capsule reconstruction [10] and implant positioning [13]. Increased dislocation rates have also been found in patients after prolonged operative time [14]. The risk for haematoma on the other hand may be reduced by atraumatic soft tissue handling and meticulous bleeding control, which however may prolong operative time.
All in all neither the dorsal nor the transgluteal approach seem to offer a clear advantage regarding early surgical complications. Although there is evidence showing a significant decrease in quality of life after hip arthroplasty [24] there are actually no studies on the effects of postoperative haematoma in the elderly. Thus a recommendation for a certain surgical approach still remains an expert opinion based on a subjective judgement on the severity of several complications. Further studies concerning long-term differences of possible complications after HA such as late-onset infections, loosening and late dislocation should be conducted.
Conclusions
Early surgical complications after HA may be the origin of cascades leading to general complications and increased mortality. This is why their prevention is especially important in orthogeriatrics.
We compared early surgical complications after dorsal and transgluteal approaches. No significant difference in overall complication rate was found (10.5 vs 9.7 %). However, the rates of the types of complications examined varied significantly: the dislocation rate was higher after a dorsal approach (3.9 vs 0.5 %). On the other hand the rate for haematoma was less (1.2 vs 5.5 %). The rates for infection, seroma and perioperative fracture did not differ significantly.
Thus a decision in favour of one surgical approach cannot be based on evidence on early surgical complication rates alone. More outcome parameters should be included together with studies on the severity of the various kinds of complications.
Acknowledgments
The authors would like to thank Mrs. Marion Wendlik, who took care of collecting the patient records and participated in maintaining the data files.
Footnotes
Roland Biber and Matthias Brem contributed equally to this work.
Contributor Information
Roland Biber, Email: biber@klinikum-nuernberg.de.
Matthias Brem, Email: Matthias.brem@klinikum-nuernberg.de.
Katrin Singler, Email: katrin.singler@aging.med.uni-erlangen.de.
Manfred Moellers, Email: Manfred.moellers@klinikum-nuernberg.de.
Cornel Sieber, Email: sieber@klinikum-nuernberg.de.
Hermann Josef Bail, Email: hermann-josef.bail@klinikum-nuernberg.de.
References
- 1.Leonardsson O, Garellick G, Kärrholm J, Åkesson K, Rogmark C (2012) Changes in implant choice and surgical technique for hemiarthroplasty. 21,346 procedures from the Swedish Hip Arthroplasty Register 2005–2009. Acta Orthop 83:7–13. doi:10.3109/17453674.2011.64104 [DOI] [PMC free article] [PubMed]
- 2.Luo X, He S, Li Z, Huang D. Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg. 2012;132:455–463. doi: 10.1007/s00402-011-1436-9. [DOI] [PubMed] [Google Scholar]
- 3.Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010;6:CD001706. doi: 10.1002/14651858.CD001706.pub4. [DOI] [PubMed] [Google Scholar]
- 4.Deangelis JP, Ademi A, Staff I, Lewis CG. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-up. J Orthop Trauma. 2012;26:135–140. doi: 10.1097/BOT.0b013e318238b7a5. [DOI] [PubMed] [Google Scholar]
- 5.Bauer R, Kerschbaumer F, Poisel S, Oberthaler W. The transgluteal approach to the hip joint. Arch Orthop Trauma Surg. 1979;95:47–49. doi: 10.1007/BF00379169. [DOI] [PubMed] [Google Scholar]
- 6.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64:17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 7.Sendtner E, Borowiak K, Schuster T, Woerner M, Grifka J, Renkawitz T. Tackling the learning curve: comparison between the anterior, minimally invasive (Micro-hip®) and the lateral, transgluteal (Bauer) approach for primary total hip replacement. Arch Orthop Trauma Surg. 2011;131:597–602. doi: 10.1007/s00402-010-1174-4. [DOI] [PubMed] [Google Scholar]
- 8.Pospischill M, Kranzl A, Attwenger B, Knahr K. Minimally invasive compared with traditional transgluteal approach for total hip arthroplasty: a comparative gait analysis. J Bone Joint Surg Am. 2010;92:328–337. doi: 10.2106/JBJS.H.01086. [DOI] [PubMed] [Google Scholar]
- 9.Lafosse JM, Chiron P, Tricoire JL, Giordano G, Molinier F, Puget F. Prospective and comparative study of minimally invasive posterior approach versus standard posterior approach in total hip replacement. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:228–237. doi: 10.1016/S0035-1040(07)90244-5. [DOI] [PubMed] [Google Scholar]
- 10.Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res. 2006;447:34–38. doi: 10.1097/01.blo.0000218746.84494.df. [DOI] [PubMed] [Google Scholar]
- 11.Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. doi: 10.1097/01.blo.0000218752.22613.78. [DOI] [PubMed] [Google Scholar]
- 12.Bush JB, Wilson MR. Dislocation after hip hemiarthroplasty: anterior versus posterior capsular approach. Orthopedics. 2007;30:138–144. doi: 10.3928/01477447-20070201-05. [DOI] [PubMed] [Google Scholar]
- 13.Enocson A, Lapidus G, Törnkvist H, Tidermark J, Lapidus LJ. Direction of hip arthroplasty dislocation in patients with femoral neck fractures. Int Orthop. 2010;34:641–647. doi: 10.1007/s00264-009-0943-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madanat R, Mäkinen TJ, Ovaska MT, Soiva M, Vahlberg T, Haapala J (2012) Dislocation of hip hemiarthroplasty following posterolateral surgical approach: a nested case-control study. Int Orthop 36:935–940. doi:10.1007/s00264-011-1353-0 [DOI] [PMC free article] [PubMed]
- 15.Siracuse JJ, Odell DD, Gondek SP, Odom SR, Kasper EM, Hauser CJ, Moorman DW. Health care and socioeconomic impact of falls in the elderly. Am J Surg. 2012;203:335–338. doi: 10.1016/j.amjsurg.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Rathier MO, Baker WL. A review of recent clinical trials and guidelines on the prevention and management of delirium in hospitalized older patients. Hosp Pract (Minneap) 2011;39:96–106. doi: 10.3810/hp.2011.10.928. [DOI] [PubMed] [Google Scholar]
- 17.Flaherty JH, Little MO. Matching the environment to patients with delirium: lessons learned from the delirium room, a restraint-free environment for older hospitalized adults with delirium. J Am Geriatr Soc. 2011;59(Suppl 2):S295–S300. doi: 10.1111/j.1532-5415.2011.03678.x. [DOI] [PubMed] [Google Scholar]
- 18.Meguro K, Yamagauchi S, Doi C, Nakamura T, Sekizawa K, Sasaki H. Prevention of respiratory infections in elderly bed-bound nursing home patients. Tohoku J Exp Med. 1992;167:135–142. doi: 10.1620/tjem.167.135. [DOI] [PubMed] [Google Scholar]
- 19.Pedersen SJ, Borgbjerg FM, Schousboe B, Pedersen BD, Jørgensen HL, Duus BR, Lauritzen JB, et al. A comprehensive hip fracture program reduces complication rates and mortality. J Am Geriatr Soc. 2008;56:1831–1838. doi: 10.1111/j.1532-5415.2008.01945.x. [DOI] [PubMed] [Google Scholar]
- 20.Jameson SS, Khan SK, Baker P, James P, Gray A, Reed MR, Deehan DJ. A national analysis of complications following hemiarthroplasty for hip fracture in older patients. QJM. 2012;105:455–460. doi: 10.1093/qjmed/hcs004. [DOI] [PubMed] [Google Scholar]
- 21.Ames JB, Lurie JD, Tomek IM, Zhou W, Koval KJ. Does surgeon volume for total hip arthroplasty affect outcomes after hemiarthroplasty for femoral neck fracture? Am J Orthop. 2010;39:E84–E89. [PubMed] [Google Scholar]
- 22.Schliemann B, Seybold D, Gessmann J, Fehmer T, Schildhauer TA, Muhr G. Bipolar hemiarthroplasty in femoral neck fractures–impact of duration of surgery, time of day and the surgeon’s experience on the complication rate. Z Orthop Unfall. 2009;147:689–693. doi: 10.1055/s-0029-1186204. [DOI] [PubMed] [Google Scholar]
- 23.Enocson A, Tidermark J, Tornkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop. 2008;79:211–217. doi: 10.1080/17453670710014996. [DOI] [PubMed] [Google Scholar]
- 24.Enocson A, Pettersson H, Ponzer S, Törnkvist H, Dalén N, Tidermark J. Quality of life after dislocation of hip arthroplasty: a prospective cohort study on 319 patients with femoral neck fractures with a one-year follow-up. Qual Life Res. 2009;18:1177–1184. doi: 10.1007/s11136-009-9531-x. [DOI] [PubMed] [Google Scholar]