Abstract
Purpose
Malposition of the acetabular cup is the most common cause of total hip arthroplasty (THA) dislocation. The position of a total hip implant is usually analysed on computed tomography (CT) scan. We aim to prove it is possible to measure, with good accuracy, the position of an acetabular cup using the low-dose irradiation (EOS) imaging.
Material and methods
We implanted an acetabular cup in a pelvic dry bone and measured cup anteversion and inclination with scanography. We performed 14 series of EOS acquisitions with different inclination, rotation and pelvic tilt, which were analysed by five observers. Two observers repeated angle measurements. We then calculated measurement inter- and intrareproducibility and accuracy.
Results
Using a confidence interval (CI) of 95 %, inter- and intra-observer reproducibility were ±1.6, and ±1.4°, respectively, for cup inclination; accuracy in comparison with CT was ±2.6°. Using a 95 % CI, inter- and intra-observer reproducibility for cup anteversion were ±2.5° and ±2.3°, respectively. Measurement accuracy compared with CT was ±3.9°.
Conclusion
EOS imaging system is superior to standard radiography in terms of measuring acetabular anteversion and inclination.
Introduction
Reconstructing a patient’s ideal biomechanical anatomy during implant placement in total hip arthroplasty (THA) is a major concern for orthopaedic surgeons. Implant position plays a major role in mechanical stability of the arthroplasty, and malpositioning of the acetabular component is the most common cause of THA dislocation [1–3]. Dislocation rates vary between 0.5 % and 10 % in large studies of primary THA implantations [4–8]. Every deviation of the acetabular cup from its ideal centre of rotation in the patient’s pelvic bone negatively influences endoprosthesis survival, implant wear and hip load [9, 10] and could limit range of motion (ROM) [11]. The use of computer navigation for acetabular cup positioning has proved to be reliable, and a prospective randomised study [12] shows better acetabular cup positioning with navigation than with the freehand technique using a minimally invasive anterior approach in the lateral position.
If inclination of the acetabular component could be measured on hip radiographies with a precision of around ±3° [13, 14], anteversion is measured with precision of around ±10°. Computed tomography (CT) is the gold standard for measuring acetabular component positioning in postoperative assessment [15] but is also commonly used for pre-operative planning in computer-assisted navigation [12]. Radiation exposure to patients is becoming a real health concern due to multiple CT examinations—a concern that must be considered. EOS imaging is a new system that reduces radiation exposure and allows image acquisition with the patient in a standing or sitting position [16–18]. Our study demonstrates that it is possible to measure inclination and anteversion of an acetabular cup implanted in a dry bone.
Material and method
We created an original device using a dry pelvic bone in which we implanted an RM Mathys® acetabular cup. (Fig. 1) That implant has a metallic ring that is easy to locate on a standard X-ray. We fixed the pelvis on a plexiglas support.
Fig. 1.

Dry pelvis bone with acetabular cup
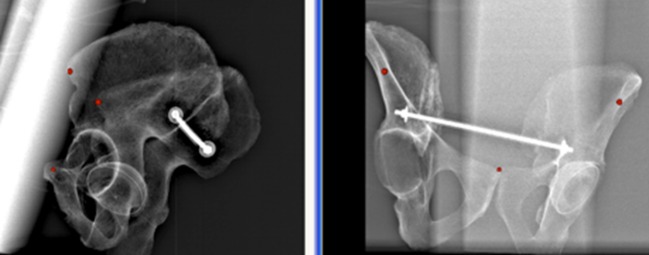
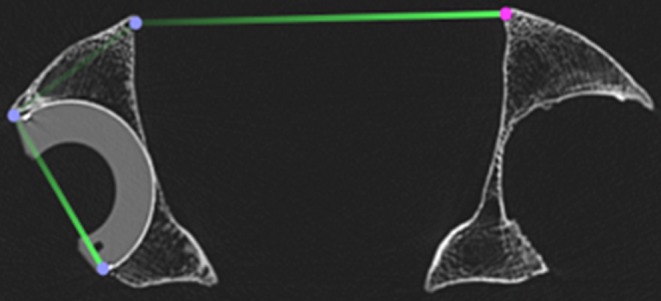
Measurement of the acetabular position with CT scan
We placed our device on the scanning table (Fig. 2) and performed a single CT scan and measured the acetabular cup reference position (Siemens Sensation 64-detector-row 0.75-mm thickness) according to the protocol described by Stem et al. [19]. Cup inclination was measured from a frontal reconstruction by obtaining the angle between a line drawn from the acetabular superior and inferior edges and a horizontal line between the ischial tuberosities (Fig. 3). Cup anteversion was measured on axial images at the centre of the cup. Acetabular anteversion was defined as the angle between the anterior and posterior edge of the cup and a reference line drawn perpendicular to a line between the posterior pelvic margines at the level of the sciatic notch (Fig. 4). All angular measurements were performed on the Siemens MagicView workstation. Two measurements of inclination and anteversion were made by the same radiologist, and the average of these two values was used.
Fig. 2.

Computed tomography scan of the experimental device
Fig. 3.
Measurement of acetabular cup inclination
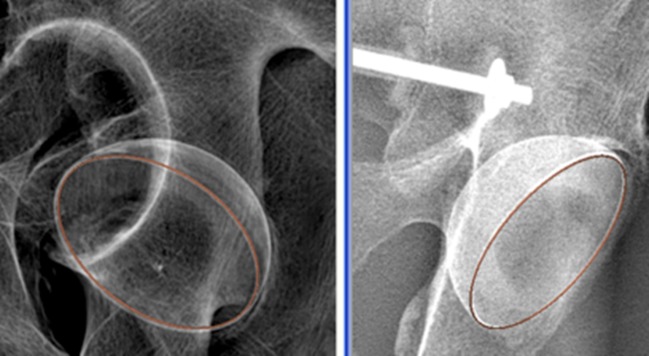
Fig. 4.
Measurement of acetabular cup anteversion
Measurement of acetabular position with EOS imaging
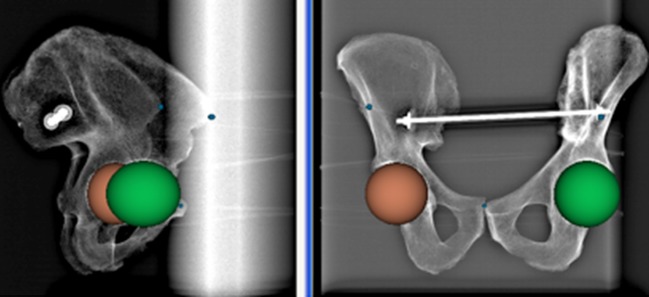
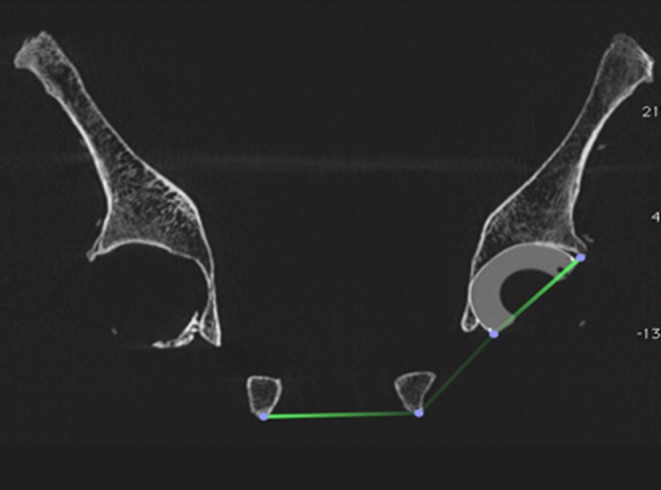
The EOS Imaging device uses two high-energy particle detectors that enable X-ray imaging to be performed at lower radiation dose to the patient and allows images to be captured with the patient in the upright or sitting position (Fig. 5). The system achieves anteroposterior and lateral pelvic acquisition at the same time. We performed 14 acquisitions using our device by varying its position in rotation (+8°, 0°, −8°), pelvic tilt (45°, 0°, −45°) and inclination (70°, 0°, −70°) via the plexiglas support. We defined a reference plane with 3D objects manually placed on anterosuperior iliac spines right and left and the pubic symphysis on anteroposterior and lateral views (Fig. 6). We placed right and left markers on the anatomical locations on frontal and lateral views at the same time on two different windows in order to prevent misplacement of the virtual markers. A 3D view of the virtual objects allows their placement to be checked. Two spheres were manually placed to locate the position of the right and left acetabulum (Fig. 7). A ring, known as the EOS ring, is adjusted on the metallic ring of the acetabular cup (Fig. 8) on anteroposterior and lateral EOS images. The software calculates placement of the EOS ring in the reference plane and measures acetabular cup position. Each observer independently placed the 3D markers and spheres with the sterEOS software.
Fig. 5.
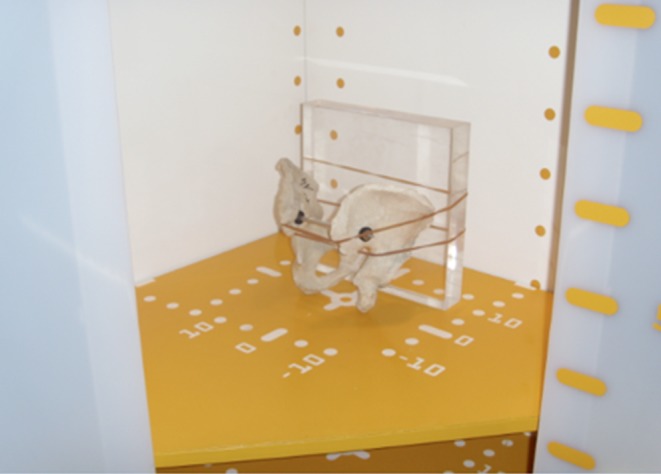
Experimental device in the electro-optical system (EOS) cabin
Fig. 6.
Three-dimensional objects define Lewinnek plane inclination
Fig. 7.
Two spheres show right and left acetabulum
Fig. 8.
A ring is used to measure acetabular cup inclination and anteversion
Intra- and interobserver reproducibility
Inclination and anteversion angle measurements were performed by five observers on 14 acquisitions. Two observers repeated angle measurements. Intra- and interreproducibility were calculated using the Norme française-International Organization for Standardization 5725-2 (NF-ISO 5725-2) standard [20]. We used a one-way random-effects model of analysis of variance (ANOVA) and calculated inter- and intra-observer reproducibility with a 95 % confidence interval (CI). We calculated measurement accuracy using CT-scan values as actual values.
Results
With CT scan acquisition measurements, acetabular cup inclination was 45° and anteversion was 30°. With the EOS imaging system acetabular cup inclination and intra- and inter-observer reproducibility were 1.4° and 1.6° with a 95 % CI, amplitude was 3.9° (42.6–46.5°) and accuracy in comparison with CT scan 2.6°. For anteversion, intra- and interobserver reproducibility were 2.3° and 2.5° with a 95 % CI, amplitude was 6.6° (28.1–34.7°) and accuracy in comparison with CT scan 3.9°.
Discussion
We conducted a feasibility study to demonstrate it is possible to use EOS imaging to measure acetabular implant position. The software sterEOS used to measure acetabular implant inclination and anteversion required basic notions in anatomy. Measurement repeatability and reproducibility are <3° with a 95 % CI. Kalteis et al. [15] demonstrated that X-ray and CT scan have approximately 3° and 2° accuracy, respectively, for measuring acetabular cup inclination. EOS imaging showed an accuracy of 2.6°; this new method is then competitive with X-ray and CT scan, with reduced radiation dose to the patient. Ackland et al. [21] demonstrate that a simple anteroposterior X-ray does not allow recognition of acetabular cup ante- or retroversion. Extrapelvic X-ray is therefore useful for analyzing opening or closing of the ellipse to determine implant ante- or retroversion. Measurement accuracy with X-ray and CT scan are 9.2° and 2.9°. Using EOS imaging we found accuracy of 3.9°, indicating EOS is less accurate than CT scan for measuring anteversion but superior to X-rays.
EOS imaging represents a major advantage in terms of reduced patient irradiation. One EOS acquisition is approximately 0.1 mSv, whereas an analysis of a THA with X-rays requires three images (anteroposterior, lateral, pelvic), corresponding to 2 mSv, and a pelvic CT scan is between 3 and 5 mSv. EOS imaging therefore divides irradiation by ten to 100 times. It also allows imaging with the patient in standing and sitting positions. Lazennec et al. [22] demonstrated that measuring anatomic acetabular anteversion on a plain CT scan is biased in the THA population. EOS captures patient images in their upright and weight-bearing and sitting positions, and a recent report [23] shows that analysis of a THA in standing and sitting positions may help determine possible cases of implant impingement, instability or abnormal wear.
The software sterEOS creates 3D images from two unique frontal and lateral low radiation dose images: we used a method based on positioning figures on both frontal and lateral images to obtain measurement of the 3D position of the acetabular cup in the pelvis. Recent publications [24, 25] show that EOS reconstruction is a useful and reliable technique for assessing lower-limb and spine deformities in 3D, and new tools are under development to analyse hip and pelvic concerns. Measurement in Lewinnek and horizontal planes can be made easily and allow analysis of the patient’s pelvis positioning and biomechanical behaviour of hip implants in the upright and weight-bearing position. A second method to measure femoral stem positioning and neck anteversion is being developed at this very moment. Three-dimensional surface reconstruction of the acetabular cup and the native acetabulum does not seem challenging for the software developer and would be interesting to explore for use in surgical planning.
We studied the position of an acetabular cup on dry bone and demonstrated measurement feasibility, but our study has important limits: Firstly, the EOS ring adjusted on the metallic ring of the acetabular implant was easy to place because of our implant, which is highly favourable due to its radiolucent design. Nonetheless, the large majority of acetabular implants are metal backed. We tried to adjust the EOS ring on metal-backed implants; it worked, and we began a comparison study of reproducibility with different acetabular components. Secondly, we studied the acetabular component of a hip arthroplasty without the femoral implant, a condition that barely simulates the real clinical world; we therefore tried our method on patients with THA, but the EOS ring was not adjusted on the acetabular implant.
We attempted to measure the position of variable acetabular cups in routine follow-up of THA using EOS imaging instead of standard X-rays. The new system worked well, and there was no particular difficulty caused by the femoral implant or digestive gases. We did not evaluate intra- and interobserver reproducibility, and we were unable to compare measurements between standard and EOS X-rays for ethical reasons.
Conclusion
Measuring acetabular cup positioning is feasible using EOS imaging, which provides good accuracy and is superior to standard radiography in terms of measuring acetabular anteversion. Further studies are needed to validate and demonstrate its usefulness in clinical application.
Acknowledgments
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
References
- 1.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87(6):762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 2.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–220. [PubMed] [Google Scholar]
- 3.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 4.Palan J, Beard DJ, Murray DW, Andrew JG, Nolan J. Which approach for total hip arthroplasty: anterolateral or posterior? Clin Orthop Relat Res. 2009;467(2):473–477. doi: 10.1007/s11999-008-0560-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blom AW, Rogers M, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Dislocation following total hip replacement: the Avon Orthopaedic Centre experience. Ann R Coll Surg Engl. 2008;90(8):658–662. doi: 10.1308/003588408X318156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conroy JL, Whitehouse SL, Graves SE, Pratt NL, Ryan P, Crawford RW. Risk factors for revision for early dislocation in total hip arthroplasty. J Arthroplasty. 2008;23(6):867–872. doi: 10.1016/j.arth.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Sierra RJ, Schleck CD, Cabanela ME. Dislocation of bipolar hemiarthroplasty: rate, contributing factors, and outcome. Clin Orthop Relat Res. 2006;442:230–238. doi: 10.1097/01.blo.0000183741.96610.c3. [DOI] [PubMed] [Google Scholar]
- 8.Berry DJ, Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87(11):2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 9.Bicanic G, Delimar D, Delimar M, Pecina M. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop. 2009;33(2):397–402. doi: 10.1007/s00264-008-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schutte H, Jr LAJ, Bannar SM, Livermore JT, Ilstrup D, Morrey BF. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty. 1998;13(6):621–626. doi: 10.1016/S0883-5403(98)80003-X. [DOI] [PubMed] [Google Scholar]
- 11.D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW., Jr The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82(3):315–321. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Sendtner E, Schuster T, Wörner M, Kalteis T, Grifka J, Renkawitz T. Accuracy of acetabular cup placement in computer-assisted, minimally-invasive THR in a lateral decubitus position. Int Orthop. 2011;35(6):809–815. doi: 10.1007/s00264-010-1042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19(3):387–390. doi: 10.1016/j.arth.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 14.Pradhan R. Planar anteversion of the acetabular cup as determined from plain anteroposterior radiographs. J Bone Joint Surg Br. 1999;81(3):431–435. doi: 10.1302/0301-620X.81B3.9067. [DOI] [PubMed] [Google Scholar]
- 15.Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup—accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58(2):294–300. doi: 10.1016/j.ejrad.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Dubousset J, Charpak G, Skalli W, Kalifa G, Lazennec JY. EOS stereo-radiography system: whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose. Rev Chir Orthop Reparatrice Appar Mot. 2007;93(6 Suppl):141–143. doi: 10.1016/S0035-1040(07)92729-4. [DOI] [PubMed] [Google Scholar]
- 17.Dubousset J, Charpak G, Dorion I, Skalli W, Lavaste F, Deguise J, Kalifa G, Ferey S. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med. 2005;189(2):287–297. [PubMed] [Google Scholar]
- 18.Kalifa G, Charpak Y, Maccia C, Fery-Lemonnier E, Bloch J, Boussard JM, Attal M, Dubousset J, Adamsbaum C. Evaluation of a new low-dose digital x-ray device : first dosimetric and clinical results in children. Pediatr Radiol. 1998;28(7):557–561. doi: 10.1007/s002470050413. [DOI] [PubMed] [Google Scholar]
- 19.Stem ES, O’Connor MI, Kransdorf MJ, Crook J. Computed tomography analysis of acetabular anteversion and abduction. Skeletal Radiol. 2006;35(6):385–389. doi: 10.1007/s00256-006-0086-4. [DOI] [PubMed] [Google Scholar]
- 20.NF-ISO-5725-2 (1994) Application de la statisique – exactitude (justesse et fidélité) des résultats et méthodes de mesure – Partie 2 : méthode de base pour la détermination de la répétabilité et de la reproductibilité d’une méthode de mesure normalisée
- 21.Ackland MK, Bourne WB, Uhtoff HK. Anteversion of the acetabular cup. Measurement of angle after total hip replacement. J Bone Joint Surg. 1986;68(3):409–413. doi: 10.1302/0301-620X.68B3.3733807. [DOI] [PubMed] [Google Scholar]
- 22.Lazennec JY, Boyer P, Gorin M, Catonné Y, Rousseau MA. Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res. 2011;469(4):1103–1109. doi: 10.1007/s11999-010-1732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lazennec JY, Charlot N, Gorin M, Roger B, Arafati N, Bissery A, Saillant G. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat. 2004;26(2):136–144. doi: 10.1007/s00276-003-0195-x. [DOI] [PubMed] [Google Scholar]
- 24.Than P, Szuper K, Somoskeöy S, Warta V, Illés T. Geometrical values of the normal and arthritic hip and knee detected with the EOS imaging system. Int Orthop. 2012;36(6):1291–1297. doi: 10.1007/s00264-011-1403-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Illés T, Somoskeöy S. The EOS™ imaging system and its uses in daily orthopaedic practice. Int Orthop. 2012;36(7):1325–1331. doi: 10.1007/s00264-012-1512-y. [DOI] [PMC free article] [PubMed] [Google Scholar]