Abstract
Purpose
The aim of this study was to evaluate clinical outcomes and complications following minimally invasive plate osteosynthesis (MIPO) with the proximal humeral internal locking system (PHILOS) for treating proximal humeral shaft fracture through the deltopectoral approach.
Methods
Between November 2008 and March 2010, 74 patients with unilateral proximal humeral shaft fractures were treated using the MIPO technique with the PHILOS through the deltopectoral approach. Patients received an average follow-up of 16.9 (range, 12–24) months, and the final follow-up included anteroposterior and lateral imaging and recording of postoperative complications. The Constant–Murley shoulder score was used to evaluate function.
Results
No intraoperative complications occurred. Postoperative complications included subacromial impingement in four patients. There was no deep infection, neurovascular damage, breakage or implant loosening. All fractures united in an average time of 17.4 (15–25) weeks. In terms of function, the Constant–Murley score was 85.8 points on average (range, 67–100). The range of motion of the involved shoulder was satisfactory, and pain-free in 83.8 % of patients.
Conclusions
Using the MIPO technique with the PHILOS through the deltopectoral approach is a valid and safe method of treating proximal humeral shaft fractures.
Introduction
Proximal humeral shaft fractures are commonly seen in upper-limb injuries [1], and their incidence is rising as a result of an ageing society and increasing numbers of traffic accidents [2, 3]. Anatomical reduction, stable fixation and early mobilisation are prerequisites for full functional recovery of the involved shoulder following displaced proximal humeral shaft fractures.
According to previous reports, there are several methods to treat proximal humeral shaft fractures, each with different outcomes and associated complications. Traditionally, open reduction is used to achieve accurate alignment and avoid neurovascular damage. However, extensive soft-tissue dissection can result in iatrogenic damage to the radial nerve. Moreover, the risk of nonunion is increasing. Therefore, theoretically, minimally invasive percutaneous osteosynthesis (MIPO) should be beneficial to attain fracture union and prevent complications. Preliminary studies report that MIPO offers a valid option for treating proximal humeral shaft fractures [4].
The proximal humerus internal locking system (PHILOS; Synthes, Paoli, PA, USA) can provide angular stability and has been used for operative management of proximal humeral fractures for several years [5]. The system has the potential for enhanced stability of bone–plate structure that could allow early functional exercises. Additionally, it can be inserted using a MIPO approach without additional damage [6, 7]. This method requires less soft-tissue dissection and restricts fracture haematoma and damage to the blood supply to the bone fragments. Although there are numerous publications concerning the MIPO technique, few focus on proximal fractures of the humeral shaft.
Our retrospective study was designed to investigate clinical outcomes and associated complications of proximal humeral shaft fractures treated with the PHILOS using the minimally invasive deltopectoral approach. The study was approved by the Institutional Ethical Board.
Patients and methods
Between November 2008 and March 2010, we treated 92 patients with proximal humeral shaft fracture using the MIPO technique. Patients were included in this study if the diagnosis was acute and were treated with the PHILOS inserted through the deltopectoral approach in a minimally invasive manner. Indications for MIPO with the long PHILOS plate were fractures of the proximal third of the humeral shaft and shaft fractures that extended into the humeral head showing an angulation over 20° in the anteroposterior or lateral X-ray or an axial shortening of over three centimetres after closed reduction [4]. Those with follow-up under 12 months were excluded from the study. Patients with open injuries, pre-existing nerve injuries and polytrauma were also excluded. Consequently, there were 74 patients with detailed data for analysis (26 men, 48 women; age range 34–86 years, average 57.3 years). Forty-two cases were the result of accidental falls, and 32 were caused by traffic accidents. Sixty cases involved the dominant side. All fractures involved mainly the proximal and middle humeral shaft.
According to the Arbeitsgemeinshaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) criteria, four fractures were categorised as type A1, five as A2, 26 as B1, 14 as B2, five as B3, 12 as C1 and eight as C2. Thirty-two cases had confirmed primary osteoporosis. The average injury-to-surgery interval was 2.4 (range, one to five) days, and average follow-up was 16.9 (range, 12–24) months.
Surgical technique
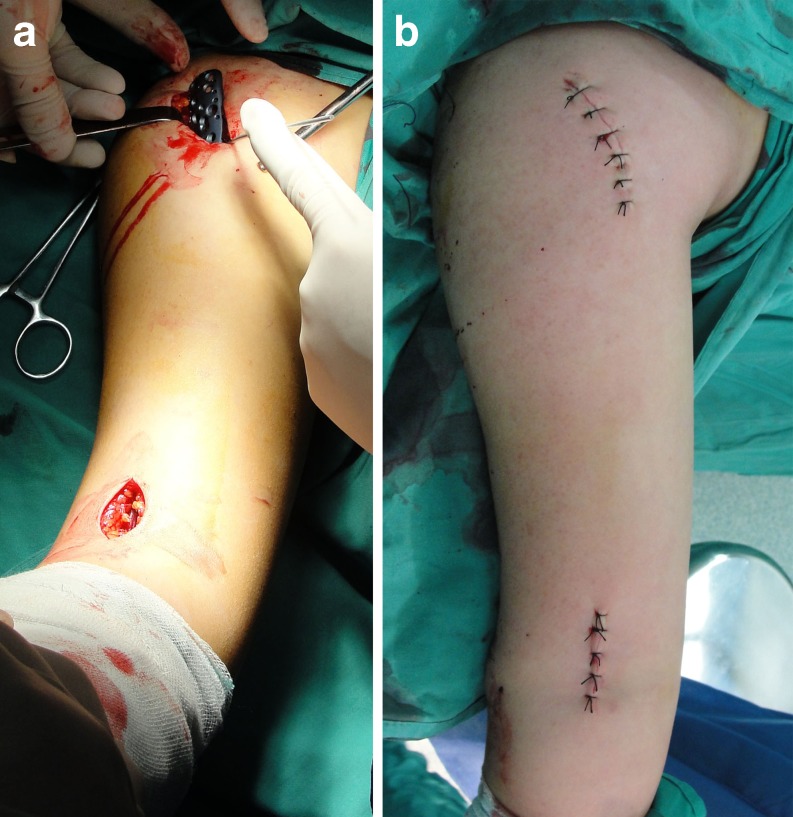
Under general anaesthesia, the patient was put in a beach-chair position under C-arm control. Proximally, a five centimetre incision was made at the deltopectoral groove to expose the anterolateral side of the greater tuberosity of the humerus. The other five centimetre incision was made over the lateral side of the distal humeral shaft. The brachialis muscle was split by blunt dissection along the lateral side of the biceps brachii. It should be noted that the musculocutaneous nerve was lying on the lateral brachialis muscle. It is generally considered that eight centimetres above the lateral epicondyle is the landmark where the radial nerve pierces the lateral intermuscular septum and winds along the lateral border of the humerus. Generally, the nerve was not exposed, and the lateral retraction was performed gently. To develop a submuscular tunnel, the muscle was split bluntly when the epiperiosteal level was reached. The proximal fragment was positioned to maintain abduction and internal rotation. Then, the distal fragment was manoeuvred to obtain satisfactory alignment. The PHILOS was inserted proximal to distal. The proximal end of the plate was fixed temporarily at the anterolateral side of the greater tuberosity using a Kirschner wire, and the distal end was fixed with a screw. The location and alignment of the plate–humerus construction was confirmed using both the anteroposterior and lateral views under the C-arm machine. The proximal end was fixed with four or five 3.5-mm locking screws and the distal part with two or three 3.5-mm locking screws. Plate–humerus construction alignment was again checked radiographically. The wound was sutured layer by layer (Fig. 1), and postoperatively, the patient was allowed to perform free, active shoulder movements without any additional external stabilisation device.
Fig. 1.
Minimally invasive deltopectoral approach for plating proximal humeral shaft fractures. The proximal humeral internal locking system (PHILOS) was inserted proximal to distal. Proximal fragments were stabilised temporarily using a Kirschner wire (a). General view of the approach is shown after closure (b)
Follow-up
These patients agreed postoperatively to regular follow-ups at one, three, six and 12 months. Radiological imaging was used to determine bone–plate position and fracture union progress. Functional outcome was evaluated according to the Constant–Murley shoulder assessment [8], the scoring system of which comprises four parts: pain, power, activities of daily living and range of movement.
Results
General
Operative time was 86 minutes on average (range, 45–150 min). Fluoroscopy time was an average of 70 seconds (range, 30–180 seconds). There were no intraoperative complications. All fractures united at an average of 17.4 (range, 15–25) weeks (Fig. 2). Hardware was removed in four patients due to lateral impingement and in 42 for social and personal reasons.
Fig. 2.
Proximal humeral shaft fractures treated with the proximal humeral internal locking system (PHILOS) through the minimally invasive deltopectoral approach. Anteroposterior view of a proximal humeral shaft fracture categorised as type 12-B1.1 (a). Anteroposterior imaging was used after the fracture was plated with the PHILOS (b). Fracture union was achieved radiographically 15 weeks after the operation (c)
Function
The Constant–Murley score was assessed by two surgeons, with mean points for statistical analysis. In terms of movement, median range was 142° flexion (range, 90–180°); 45° extension (range, 30–50°); 45° internal rotation (range, 30–70°); 60° external rotation (range, 45–85°); 140° abduction (range, 110–180°). Regarding pain, 62 patients had none and 11 reported mild and one reported moderate pain. The average Constant–Murley score was 85.8 (range, 67–100) points.
Complications
No deep-wound infections, nerve or vascular injuries were observed. Four patients had subacromial impingement three months later. There was no implant loosening or breakage. Alignment was satisfactory in both anteroposterior and lateral views.
Discussion
There are few reports concerning clinical outcomes and associated complications following the MIPO technique for treating proximal humeral shaft fractures. Brunner and associates published preliminary results of MIPO for proximal humeral shaft fractures with the PHILOS using the delta-split approach and concluded that MIPO was effective for such fractures, and that lower rates of wound infection and shorter hospital stay could be achieved [4]. In our study, with an average postoperative follow-up of 16.9 months, we found MIPO to be safe and valid for proximal humeral shaft fractures. Satisfactory outcomes were achieved, including fracture union, lower incidence of complications and optimal restoration of shoulder function demonstrated by the Constant–Murley score.
Conservative treatment continues to be the most commonly accepted management for humerus shaft fractures. Although external stabilisation is simple and cheap, it is not easy to reduce the abducted fragment of the proximal fracture [9, 10]. Absolute and relative indications for surgical treatment of proximal humeral shaft fractures have been documented in textbooks. These include polytrauma, open fractures, bilateral fractures and floating elbow. Traditional open reduction and internal fixation often requires an extensive soft-tissue dissection, which may damage the vascular supply to the humeral head. Moreover, other less invasive methods, such as percutaneous pinning, require advanced skills and good bone quality, minimal fracture comminution and a cooperative patient [11]. Minimally invasive surgical techniques in diaphyseal fractures of long bones have shown advantages over the open conventional techniques, especially when they preserve the biological milieu of the fracture focus, allowing a better environment for consolidation with fewer complications, such as infection and nonunion [6, 12]. These techniques have not been very popular in the proximal humeral fracture because of its anatomical complexity and the fear of damaging vital structures.
The deltopectoral approach is regarded as the standard for proximal humeral shaft fractures [13] as it provides adequate exposure for internal fixation. Concern about using the approach centres on potential damage to the radial nerve. In our study, the radial nerve was covered by lateral musculature and not routinely exposed. There was no radial nerve neurapraxia in these patients. Distally, the radial nerve is not at risk when the plate is placed on the anterior aspect of the humerus; however, slight supination is recommended [6]. For the delta-split approach, the implant is placed on the anterior face of the humerus; therefore, exposure of the radial nerve is unavoidable. The radial nerve should be handled cautiously during the procedure and protected simply by using gentle retraction if it is directly visualised. Lau et al. reported three cases of radial nerve neurapraxia from a total of 17 patients treated with MIPO for proximal humeral fractures [14]. They suggest that this problem was very likely because of the traction to the nerve during fixation of the plate distally.
Damage to the axillary nerve is very rare with the deltopectoral approach. However, by contrast, it is seen commonly when the delta-split approach is employed, when there are concerns regarding injury to the axillary nerve with subsequent dysfunction of the anterior deltoid [15, 16]. Although in a recent study injury to the axillary nerve was not observed, the axillary nerve is in danger according to previous studies [17]. The plate is inserted through a tunnel created proximal to distal along the lateral surface of the humerus and beneath the axillary nerve. The nerve is raised off the humerus with a finger as the plate is slid beneath it. The axillary nerve should be identified and examined intraoperatively thereafter. It has been indicated that early range of shoulder and elbow motion is possible after MIPO for humeral shaft fractures [18]. Brunner and associates found that MIPO with the PHILOS through the delta-split approach offered a valid option for proximal humeral shaft fractures, with lower rates of radial neuropathy [4].
The PHILOS plate has proven to be a valid implant for fractures extending into the proximal humeral shaft [19]. This recommendation is supported by recent findings of Lau et al. who treated 17 patients with proximal humerus fractures using a metaphyseal locking compression plate, which was put on the lateral side of the humerus [14]. Using this implant, they achieved stable fixation of the proximal fragment, even in osteoporotic bone, with three to four 3.5-mm locking screws.
In our study comprising 74 patients, all fractures united with an average union time of 17.4 weeks. No implant-related complications were observed during an average follow-up of 16.9 months. No neurovascular damage was observed. The full range of shoulder and elbow motion was achieved in the majority of patients. There were four cases with subacromial impingement, which was confirmed by symptoms and radiographic examinations. Restricted motion disappeared when the implant was removed following fracture union.
To our knowledge, this is the first time that the MIPO technique with the PHILOS for proximal humeral shaft fractures in an adequate number of patients with follow-up has been reported. Although the MIPO plating technique is beneficial for proximal humeral shaft fractures, skilled and state-of-the-art patient management is necessary. The learning curve of MIPO plating for proximal humeral shaft fractures is unknown; however, mastery of the traditional technique of open reduction and internal fixation is essential in case the MIPO technique fails. In summary, the MIPO technique with the PHILOS through the deltopectoral approach is valid and safe for proximal humeral shaft fractures. However, controlled studies between MIPO through the deltopectoral and the delta-split approaches should be undertaken.
Acknowledgments
Conflict of interest statement
The authors declare that they have no conflict of interest.
References
- 1.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 2.Rees J, Hicks J, Ribbans W. Assessment and management of three-and four-part proximal humeral fractures. Clin Orthop Relat Res. 1998;353:18–29. doi: 10.1097/00003086-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Kannus P, Palvanen M, Niemi S, Paakkari J, Järvinen M, Vuori I. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970–1998 and alarming projections for the new millennium. Acta Orthop Scand. 2000;71:465–470. doi: 10.1080/000164700317381144. [DOI] [PubMed] [Google Scholar]
- 4.Brunner A, Thormann S, Babst R. Minimally invasive percutaneous plating of proximal humeral shaft fractures with the proximal humerus internal locking system (PHILOS) J Shoulder Elbow Surg. 2011;21:1056–1063. doi: 10.1016/j.jse.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 5.Koukakis A, Apostolou CD, Taneja T, Korres DS, Amini A. Fixation of proximal humerus fractures using the PHILOS plate: early experience. Clin Orthop Relat Res. 2006;442:115–120. doi: 10.1097/01.blo.0000194678.87258.6e. [DOI] [PubMed] [Google Scholar]
- 6.Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005;36:530–538. doi: 10.1016/j.injury.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 7.Helmy N, Hintermann B. New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res. 2006;442:100–108. doi: 10.1097/01.blo.0000194674.56764.c0. [DOI] [PubMed] [Google Scholar]
- 8.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 9.Hanson B, Neidenbach P, Boer P, Stengel D. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg. 2009;18:612–621. doi: 10.1016/j.jse.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 10.Monga P, Verma R, Sharma VK. Closed reduction and external fixation for displaced proximal humeral fractures. J Orthop Surg (Hong Kong) 2009;17:142–145. doi: 10.1177/230949900901700203. [DOI] [PubMed] [Google Scholar]
- 11.Herscovici D, Jr, Saunders DT, Johnson MP, Sanders R, DiPasquale T. Percutaneous fixation of proximal humeral fractures. Clin Orthop Relat Res. 2000;375:97–104. doi: 10.1097/00003086-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Ji F, Tong D, Tang H, Cai X, Zhang Q, Li J, Wang Q. Minimally invasive percutaneous plate osteosynthesis (MIPPO) technique applied in the treatment of humeral shaft distal fractures through a lateral approach. Int Orthop. 2009;33:543–547. doi: 10.1007/s00264-008-0522-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zlotow DA, Catalano LW, Barron OA, Glickel SZ. Surgical exposures of the humerus. J Am Acad Orthop Surg. 2006;14:754–765. doi: 10.5435/00124635-200612000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Lau TW, Leung F, Chan CF, Chow SP. Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop. 2007;31:657–664. doi: 10.1007/s00264-006-0242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gardner MJ, Griffith MH, Dines JS, Briggs SM, Weiland AJ, Lorich DG. The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res. 2005;434:123–129. doi: 10.1097/01.blo.0000152872.95806.09. [DOI] [PubMed] [Google Scholar]
- 16.Laflamme GY, Rouleau DM, Berry GK, et al. Percutaneous humeral plating of fractures of the proximal humerus: results of a prospective multicenter clinical trial. J Orthop Trauma. 2008;22:153–158. doi: 10.1097/BOT.0b013e3181694f7d. [DOI] [PubMed] [Google Scholar]
- 17.Rancan M, Dietrich M, Lamdark T, Can U, Platz A. Minimal invasive long PHILOS®-plate osteosynthesis in metadiaphyseal fractures of the proximal humerus. Injury. 2010;41:1277–1283. doi: 10.1016/j.injury.2010.07.235. [DOI] [PubMed] [Google Scholar]
- 18.Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010;24:212–216. doi: 10.1097/BOT.0b013e3181c2fe49. [DOI] [PubMed] [Google Scholar]
- 19.Schwarz N, Windisch M, Mayr B. Minimally invasive anterior plate osteosynthesis in humeral shaft fractures. Eur J Trauma Emerg Surg. 2009;35:271–276. doi: 10.1007/s00068-008-8047-3. [DOI] [PubMed] [Google Scholar]