Abstract
Purpose
The cementless Bicontact® total hip arthroplasty (THA) system (AESCULAP AG, Tuttlingen, Germany) was introduced in 1986/1987 and has been in successful clinical use in an unaltered form up to today. Although good long-term results with the Bicontact® stem have been published, it is questionable whether the implant provides the criteria for a state-of-the-art stem regarding proximal bone stock preservation. The purpose of the study was to monitor the periprosthetic bone mineral density (BMD) in a prospective two-year follow-up dual-energy X-ray absorptiometry (DEXA) study.
Methods
After power analysis, a consecutive series of 25 patients with unilateral Bicontact® stem implantation was examined clinically and underwent DEXA examinations. Scans of seven regions of interest were taken preoperatively and at one week, six months, and one and two years.
Results
One patient required stem revision due to a deep infection. The Harris Hip Score increased significantly by 44 points. The most significant bone loss was observed in the calcar region (R7) in the first six months (−19.2 %). It recovered in the following 18 months to −8.5 %. The BMD in the greater trochanter dropped significantly after six months and remained stable at this level. BMD exceeded baseline values in distal regions and even more in the lesser trochanter region after two years.
Conclusions
We conclude that the Bicontact® stem provides adequate proximal bone stock preservation. We observed some signs of stress shielding at the tip of the stem, which is inevitable to some degree in THA with cementless straight stems. However, in this prospective DEXA investigation, we showed that proximal off-loading does not occur after THA with the Bicontact® system. Thus, we believe that this stem is still a state-of-the-art implant.
Introduction
The cementless Bicontact® total hip arthroplasty system (AESCULAP AG, Tuttlingen, Germany) was introduced in 1986/1987 and has been in successful clinical use in an unaltered form up to today [1, 2]. Total hip arthroplasty (THA) is undergoing rapid development, with new implants constantly coming on the market. However, virtually every new stem comes up to the claim of “preserving bone“ by cementless proximal fixation and proximal load transfer to the bone. This can be assessed by direct acquisition of bone remodelling data via dual-energy X-ray absorptiometry (DEXA), which is the gold standard in evaluating redistribution of mechanical forces and femur remodelling around the THA implant [3]. Although good long-term results with the Bicontact® stem have been published [1, 2, 4], it is questionable whether the implant provides the criteria for a state-of-the-art stem regarding proximal bone stock preservation. The aim of our study was to monitor the periprosthetic bone mineral density (BMD) after implantation of the Bicontact® stem in a prospective two-year follow-up DEXA study.
Patients and methods
The investigation was performed in a subproject of the Collaborative Research Centre 599. The methods of this trial have already been published in this journal [5]. From July 2008 to November 2010, a consecutive series of 25 patients [nine (36 %) women and 16 (64 %) men] with unilateral Bicontact® stem implantation were analysed in this prospective study. The number of patients was calculated by a power analysis performed by our institute for biometry. Sample size assessment was performed using the program nQuery Advisor (STATCON, Witzenhausen, Germany) basing on the study of Sabo et al. [6]. This was required by our institute’s institutional review board committee to obtain approval for this study (Ethic Committee No. 4226). All patients gave written informed consent. Inclusion criteria were indication for unilateral implantation of the stem due to osteoarthritis of the hip and age 35–85 years. Patients with a body mass index (BMI) >35, with a history of previous surgery on the same hip, femoral fracture, metabolic bone disease, use of steroids or other drugs affecting bone metabolism, intraoperative cracks or severe osteoarthritis of the contralateral hip were excluded from the study. Patients who received THA of the contralateral hip during the study period or patients in whom an event leading to restricted weight bearing on the ipsi- or contralateral hip were subsequently excluded. Mean age was 68 (range 51–77) years, and mean preoperative BMI was 27.5 (range 20.0–35.0).
In all patients, the Bicontact® straight stem (Figs. 1 and 2) and the Plasmacup SC press-fit acetabular component or the SC-Screwcup (both BBraun, Aesculap, Tuttlingen, Germany) were implanted by four experienced senior surgeons over the lateral transgluteal Bauer’s approach with the patient in the supine position. Cementless implants are made of a titanium forged alloy (Ti6Al4V). The stem has a proximal microporous pure titanium Plasmapore coating. A flat, rectangular stem shape, lateral fixation fins and a dorsal antirotation wing give the stem primary stability and proximal force transmission exclusively in the intertrochanteric region. Distal pressfit is expressively not intended with this design [7] (Fig. 2). Before Implantation, the prosthetic bed is prepared by a divided so-called osteoprofiler system. With the distally serrated A osteoprofiler, the medullary space is opened and smoothed in ascending order of size. The shoulder of the osteoprofiler compresses the intertrochanteric cancellous bone. The B osteoprofiler is then used to cut a precise bed in the previously compressed bone to accept the implant. Indications for this implant are primary and secondary osteoarthritis of the hip and avascular necrosis of the femoral head. The implant can be used for severe deformities and in some revision cases. These cases were not included in the study.
Fig. 1.

The cementless Bicontact® stem is tapered, with a rough proximal hydroxyapatite coating and a smooth distal portion
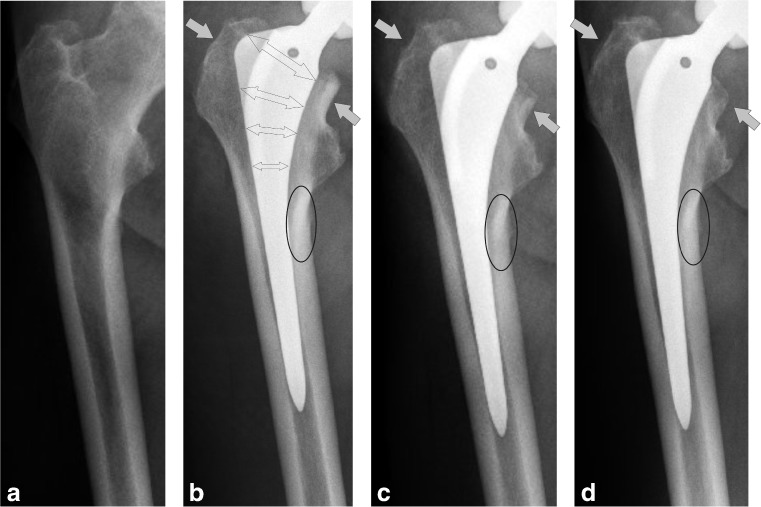
Fig. 2.
Anteroposterior preoperative (a) and postoperative (b, c, d) radiographs of a right femur over the course of 2 years after implantation of the Biconatct® stem. The region of intertrochanteric force transmission is marked with double arrows. Note the slight decrease in bone density in the proximal calcar and the greater trochanter (grey arrows). A slight bone density increase can be observed in the lesser trochanter region
Preoperatively and one week, six months and one and two years after implantation, the patients were examined clinically [Harris Hip Score (HHS)] and underwent DEXA examinations. BMD, g/cm2 data was collected one week after surgery and served as baseline value for the following DEXA examinations. All patients were fully weight bearing postoperatively. DEXA scans were performed using a HOLOGIC Discovery A S/N 80600 device (Hologic Inc., Waltham, MA, USA). BMD of the operated hip was measured using the metal-removal hip-scanning mode in seven conventional Gruen zones [8] (Fig. 3). Each patient’s individual regions of interest (ROI) were saved on the Hologic system and were used for all subsequent measurements to reduce bias. The images were analysed using dedicated Windows analysis software (version 11.2). The patients were placed in the supine position with the affected leg in 20° internal rotation. The foot was secured in the Hologic foot positioning device in order to obtain reproducible rotation in all patients to limit measurement errors, as it has been demonstrated that rotation influences BMD measurement [9–11]. DEXA precision was assessed on all patients, and all underwent sequential DEXA examinations of the contralateral unoperated hip and the proximal femur—taken preoperatively and one week later. Additional quality controls were done every morning for the DEXA equipment according to the manufacturer’s guidelines to verify the stability of the system. We did not identify any shift or drift during the entire study period; the device was therefore characterised as stable. The same observer analysed all DEXA examinations. According to our routine clinical follow-up, radiographs were taken preoperatively, intraoperatively and one week, three months and one year postoperatively. All radiographs were reviewed by a single observer regarding more than three millimetres subsidence, osteolysis and bone resorption.
Fig. 3.
The Bicontact® stem with seven regions of interest
Student’s t test was used to test the hypothesis of a difference between the means of the HHS at different measurement time points. The Shapiro-Wilk tests showed no normal distribution for DEXA measurements; the Wilcoxon signed-ranks test was used to statistically compare the density changes. A p value < 0.05 was considered significant. Data analysis was performed using SPSS (11.05 SPSS Inc. Chicago, IL, USA).
Results
After 12 months follow-up, five patients were excluded from the study. In two patients, the contralateral hip became symptomatic, two patients refused to continue the study, and one patient needed two-staged stem revision due to a deep infection. No infection, loosening, or periprosthetic fracture occurred in the remaining patients. HHS increased significantly (p < 0.001) from 48 points [standard deviation (SD) 12] preoperatively to 92 points (SD 9) at the latest follow-up. There were no signs of radiographic subsidence or radiolucent lines in any of the stems. In two patients, periarticular ossification occurred (Brooker I). Spot welds, pedestal formations, cortical hypertrophy and neocortex formation were not found.
One week after surgery, a significant increase in BMD was observed on the operated side in the greater trochanter region (R1) (p = 0.001) and in the area below (R2) (p = 0.005). Under the tip of the stem (R4), BMD decreased. Only minimal changes were seen in the distal medial area (R3), the lesser trochanter region (R6) and the proximal calcar area (R7). Due to the small number of cases, women and men were evaluated together. Table 1 shows mean BMD of the ROIs 1–7 during the two year follow-up. The most significant bone loss was observed in R7 (calcar region) in the first six months (−19.2 %). It recovered in the following 18 months to −8.5 %. BMD in the greater trochanter (R1) dropped significantly after six months and remained stable at this level (Fig. 4). It is remarkable that BMD significantly exceeded baseline values in the distal medial region (R3) and below the tip of the implant (R4) and even in the lesser trochanter region (R6) after two years (Fig. 4). No significant correlation of BMD with stem size or resection height was found in any region.
Table 1.
Mean bone mineral density (BMD) (g/cm2) of the seven regions of interest during the 2-year follow-up after implantation of the Bicontact® stem
| ROI | 1 week preoperatively | SD | 1 week postoperatively (baseline value) | SD | 6 months postoperatively | SD | 1 year postoperatively | SD | 2 years postoperatively | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.73 | 0.18 | 0.85* | 0.15 | 0.76** | 0.16 | 0.75** | 0.17 | 0.74** | 0.16 |
| 2 | 1.14 | 0.24 | 1.59* | 0.29 | 1.44** | 0.20 | 1.51 | 0.27 | 1.49 | 0.24 |
| 3 | 1.76 | 0.24 | 1.78 | 0.24 | 1.68** | 0.20 | 1.67 | 0.23 | 1.77 | 0.24 |
| 4 | 1.86 | 0.24 | 1.80* | 0.25 | 1.85 | 0.28 | 1.85 | 0.25 | 1.91** | 0.30 |
| 5 | 1.83 | 0.25 | 1.88 | 0.21 | 1.85 | 0.23 | 1.82 | 0.22 | 1.79** | 0.18 |
| 6 | 1.41 | 0.26 | 1.41 | 0.23 | 1.39** | 0.22 | 1.47 | 0.22 | 1.47 | 0.26 |
| 7 | 1.04 | 0.32 | 1.08 | 0.28 | 0.90** | 0.29 | 1.03 | 0.30 | 0.99 | 0.37 |
ROI Regions of interest 1–7 , SD Standard deviation
*Significant change to preoperative value (Wilcoxon signed-ranks test, p < 0.05)
**Significant change to baseline value 1 week after surgery (Wilcoxon signed-ranks test, p < 0.05)
Fig. 4.
Mean bone mineral density (BMD) changes of the seven regions calculated from the relative changes for each patient after 6 months (a), 1 year (b) and 2 years (c) of follow-up. The immediate postoperative value is set as baseline reference
Discussion
The successful era of THA was initiated and established by the cemented fixation technique introduced by Charnley in the 1960s [12]. Over the following 20 years, numerous different successful cemented THA systems followed. The cemented straight stem by Müller in the 1970s [13] built the conceptional preconditions for the success of the cementless systems of the following decades. However, the first concept of cementless THA, by Judet in the 1970s [14], failed in the long term. One decade later, the principle of diaphyseal cementless stem fixation was introduced in Austria by Zweymüller [15], in Italy by Spotorno [16] and in Germany by Weller [17]. In Zweymüller stems, stress shielding is a common finding. This stem, however, yields good clinical results as well. All these stems have been in successful clinical use in unaltered form up to now and were imitated by numerous manufacturers [18].
Today, much is said and published about hip resurfacing and short-stem systems in THA. However, there is common consensus that there are good indications for straight stems and the long-term value of short stems, and resurfacing still has to be evaluated. The numbers from our centre (584 Bicontact® stems implanted in 2011) and data from the joint replacement registries [19, 20] demonstrate the need for straight stems. On the one hand, patients undergoing THA are becoming younger; on the other hand, the number of THA with conventional stems will increase in an ageing population. As a trend, we see an increase in elderly patients undergoing THA with a straight stem as well younger patients with severe deformities where a short-stem implantation is impossible. Thus, our aim was to investigate whether the cementless Bicontact® straight stem used in our department in its unaltered form for 20 years provides criteria for a state-of-the art stem regarding proximal bone stock preservation. This can be determined by DEXA, which is the most reliable tool for evaluating bone remodelling after THA using different stem designs [21, 22].
Although the first postoperative scan taken one week after index surgery is the most important measurement for obtaining comparable baseline values [23, 24], we conducted an additional scan preoperatively to gather data regarding direct postoperative changes due to femoral preparation. The BMD increase in the greater trochanter (R1) and in in the region below one week after surgery can be ascribed to compressed cancellous bone. This is an important issue, as the bed for the dorsal antirotation fin is cut into the compressed bone for rotational stability (Fig. 2). Further scans were taken six months and one and two years after index surgery to obtain data from the most active period of bone remodelling [25, 26]. Although many factors are known to influence periprosthetic BMD [3], stem design and fixation are the most important [27]. In agreement with previous studies, we observed a strong decrease in BMD for almost all regions. This can be ascribed to blood-flow disruption due to femoral canal preparation three to six months after surgery [28]. The major BMD decreases in the greater trochanter (R1) and the calcar (R7) are typical for straight stems [3, 21, 23, 25, 27, 29–32]. They occur mostly due to stress shielding in the very proximal portion of the calcar due to the vast proximal cross section of the implant [28, 31]. However, it has to be noted that some load bearing seems to take place at the calcar, as BMD recovered in R7 during the study period. Except for the greater trochanter, BMD recovery is more or less pronounced in every region. This was previously described for the Bicontact® stem and other straight stems [6, 23, 31]. In particular, the calcar region (R7) showed the strongest recovery (Fig. 4). Although long-term results of short stems are unclear, it can be assumed that a concentrated load distribution on the medial portion of the femur might be an important factor for long-term implant survival in short-stemmed THA [5, 21, 33, 34]. This has not yet been reported for conventional proximal porous-coated straight stems and might suggest a relatively physiological load bearing. However, it has to be stated that in most uncemented metaphyseal coated stems some degree of buttressing occurs at the lower border of the coated surface. To some extend, this could account for the BMD increase in the lesser trochanter region. In this study, we noted a BMD increase at the tip of the implant. This can possibly be attributed to a stress-shielding phenomenon but not to a bony integration of the distal part of the implant, as the BMD would not increase in R6 if the implant would buttress distally, which can sometimes be found after THA with other conventional straight stems [6, 35–37]. A recent DEXA study by Ten Broeke et al. [38] compared two metaphyseal coated stems and observed only a small BMD increase in R4 after two years. However, BMD increase was only up to 3 % in R6 and a strong BMD decrease was seen in R7, indicating less load distribution to the calcar. The regions in their study were related to the implant, not to anatomical landmarks on the femur. We believe that this could be another explanation for their BMD results in R7 and R6 in their study, because more cortical bone was included in the measurement, and cancellous bone tends to remodel more extensively than does cortical bone [39]. It has to be noted that further comparisons to the study of Ten Broeke et al. is not reasonable due to the fundamental differences in size and position of the assessed regions.
Some critical points must be discussed. We can only present a relatively small sample size. However, to obtain approval for this study, the number of patients had to be calculated. Although some authors suggest that bone remodelling after THA is complete within the first postoperative year [25, 26, 40], it is unlikely that bone remodelling reaches equilibrium after only a short follow-up period when seen from a theoretical point of view.
We can conclude that the Bicontact® stem provides adequate proximal bone stock preservation. To our knowledge, some degree of stress shielding is inevitable in THA with cementless straight stems. We observed little signs of stress shielding at the tip of the stem. However, in this prospective DEXA investigation, we showed that proximal off-loading does not occur after THA with the Bicontact® system. Thus, we believe that this stem is still a state-of-the-art implant.
Acknowledgements
The study was undertaken in the subproject D6 of the Collaborative Research Center 599 “Sustainable degradable and permanent implants out of metallic and ceramic materials”. The authors thank the German Research foundation (DFG) for the financial support.
The authors declare that they have no conflict of interest.
References
- 1.Ochs U, Eingartner C, Volkmann R, et al. Prospective long-term follow-up of the cementless bicontact hip stem with plasmapore coating. Z Orthop Unfall. 2007;145(Suppl 1):S3–S8. doi: 10.1055/s-2007-965652. [DOI] [PubMed] [Google Scholar]
- 2.Eingartner C, Heigele T, Dieter J, et al. Long-term results with the BiCONTACT system–aspects to investigate and to learn from. Int Orthop. 2003;27(Suppl 1):S11–S15. [PubMed] [Google Scholar]
- 3.Brodner W, Bitzan P, Lomoschitz F, et al. Changes in bone mineral density in the proximal femur after cementless total hip arthroplasty. A five-year longitudinal study. J Bone Joint Surg Br. 2004;86:20–26. [PubMed] [Google Scholar]
- 4.Swamy G, Pace A, Quah C, Howard P. The Bicontact cementless primary total hip arthroplasty: long-term results. Int Orthop. 2012;36:915–920. doi: 10.1007/s00264-010-1123-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lerch M, Haar-Tran A, Windhagen H, et al. Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop. 2012;36:533–538. doi: 10.1007/s00264-011-1361-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabo D, Reiter A, Simank HG, et al. Periprosthetic mineralization around cementless total hip endoprosthesis: longitudinal study and cross-sectional study on titanium threaded acetabular cup and cementless Spotorno stem with DEXA. Calcif Tissue Int. 1998;62:177–182. doi: 10.1007/s002239900413. [DOI] [PubMed] [Google Scholar]
- 7.Stukenborg-Colsman CM, Haar-Tran A, Windhagen H, et al. Bone remodelling around a cementless straight THA stem: a prospective dual-energy X-Ray absorptiometry study. Hip Int. 2012;39:2544–2558. doi: 10.5301/HIP.2012.9227. [DOI] [PubMed] [Google Scholar]
- 8.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27 [PubMed]
- 9.Cohen B, Rushton N. Accuracy of DEXA measurement of bone mineral density after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:479–483. [PubMed] [Google Scholar]
- 10.Martini F, Lebherz C, Mayer F, et al. Precision of the measurements of periprosthetic bone mineral density in hips with a custom-made femoral stem. J Bone Joint Surg Br. 2000;82:1065–1071. doi: 10.1302/0301-620X.82B7.9791. [DOI] [PubMed] [Google Scholar]
- 11.Mortimer ES, Rosenthall L, Paterson I, Bobyn JD (1996) Effect of rotation on periprosthetic bone mineral measurements in a hip phantom. Clin Orthop Relat Res 324:269–274 [DOI] [PubMed]
- 12.Wroblewski BM, Siney PD, Fleming PA. Charnley low-frictional torque arthroplasty: follow-up for 30 to 40 years. J Bone Joint Surg Br. 2009;91:447–450. doi: 10.1302/0301-620X.91B4.21933. [DOI] [PubMed] [Google Scholar]
- 13.Muller ME (1992) Lessons of 30 years of total hip arthroplasty. Clin Orthop Relat Res 274:12–21 [PubMed]
- 14.Bettin D, Greitemann B, Polster J, Schulte-Eistrup S. Long term results of uncemented Judet hip endoprostheses. Int Orthop. 1995;19:144–150. doi: 10.1007/BF00181859. [DOI] [PubMed] [Google Scholar]
- 15.Zweymuller K, Semlitsch M. Concept and material properties of a cementless hip prosthesis system with Al2O3 ceramic ball heads and wrought Ti-6Al-4 V stems. Arch Orthop Trauma Surg. 1982;100:229–236. doi: 10.1007/BF00381662. [DOI] [PubMed] [Google Scholar]
- 16.Spotorno L, Schenk RK, Dietschi C, et al. Personal experiences with uncemented prostheses. Orthopade. 1987;16:225–238. [PubMed] [Google Scholar]
- 17.Weller S. The bicontact hip arthroplasty system. Z Orthop Unfall. 2007;145(Suppl 1):S1–S2. doi: 10.1055/s-2007-965651. [DOI] [PubMed] [Google Scholar]
- 18.Effenberger H, Imhof M, Witzel U, Rehart S. Cementless stems of the hip. Current status. Orthopade. 2005;34:477–500. doi: 10.1007/s00132-005-0800-2. [DOI] [PubMed] [Google Scholar]
- 19.Australian Orthopaedic Association National Joint Replacement Registry (2012) Annual Report. Adelaide: AOA; 2011. http://www.dmac.adelaide.edu.au/aoanjrr/documents/AnnualReports2011/AnnualReport_2011_WebVersion.pdf
- 20.National Joint Registry for England and Wales (2011) 8th Annual Report. http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/NJR%208th%20Annual%20Report%202011.pdf
- 21.Albanese CV, Rendine M, Palma F, et al. Bone remodelling in THA: A comparative DXA scan study between conventional implants and a new stemless femoral component. A preliminary report. Hip Int. 2006;16(Suppl 3):9–15. doi: 10.1177/112070000601603S03. [DOI] [PubMed] [Google Scholar]
- 22.Panisello JJ, Herrero L, Herrera A, et al. Bone remodelling after total hip arthroplasty using an uncemented anatomic femoral stem: a three-year prospective study using bone densitometry. J Orthop Surg (Hong Kong) 2006;14:32–37. doi: 10.1177/230949900601400108. [DOI] [PubMed] [Google Scholar]
- 23.Aldinger PR, Sabo D, Pritsch M, et al. Pattern of periprosthetic bone remodeling around stable uncemented tapered hip stems: a prospective 84-month follow-up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int. 2003;73:115–121. doi: 10.1007/s00223-002-2036-z. [DOI] [PubMed] [Google Scholar]
- 24.Kobayashi S, Saito N, Horiuchi H, et al. Poor bone quality or hip structure as risk factors affecting survival of total-hip arthroplasty. Lancet. 2000;355:1499–1504. doi: 10.1016/S0140-6736(00)02164-4. [DOI] [PubMed] [Google Scholar]
- 25.Bobyn JD, Mortimer ES, Glassman AH, et al. (1992) Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop Relat Res 274:79–96 [PubMed]
- 26.Munting E, Smitz P, Van SN, et al. Effect of a stemless femoral implant for total hip arthroplasty on the bone mineral density of the proximal femur. A prospective longitudinal study. J Arthroplasty. 1997;12:373–379. doi: 10.1016/S0883-5403(97)90192-3. [DOI] [PubMed] [Google Scholar]
- 27.Rahmy AI, Gosens T, Blake GM, et al. Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthetic bone loss. Osteoporos Int. 2004;15:281–289. doi: 10.1007/s00198-003-1546-5. [DOI] [PubMed] [Google Scholar]
- 28.Katano H. Periprosthetic Bone Mineral Density in Bicontact SD Stem. Five to Ten Years Follwo-up. In: Weller S, Braun A, Eingartner C, Maurer F, Weise K, Winter E, Volkmann R, editors. The Bicontact hip arthroplasty system 1987–2007. Georg Thieme Verlag: Tübingen; 2007. pp. 63–69. [Google Scholar]
- 29.Boden HS, Skoldenberg OG, Salemyr MO, et al. Continuous bone loss around a tapered uncemented femoral stem: a long-term evaluation with DEXA. Acta Orthop. 2006;77:877–885. doi: 10.1080/17453670610013169. [DOI] [PubMed] [Google Scholar]
- 30.Korovessis P, Droutsas P, Piperos G, et al. Course of bone mineral content changes around cementless Zweymueller total hip arthroplasty. A 4-year follow-up study. Arch Orthop Trauma Surg. 1997;116:60–65. doi: 10.1007/BF00434103. [DOI] [PubMed] [Google Scholar]
- 31.Roth A, Richartz G, Sander K, et al. Periprosthetic bone loss after total hip endoprosthesis. Dependence on the type of prosthesis and preoperative bone configuration. Orthopade. 2005;34:334–344. doi: 10.1007/s00132-005-0773-1. [DOI] [PubMed] [Google Scholar]
- 32.Skoldenberg OG, Boden HS, Salemyr MO, et al. Periprosthetic proximal bone loss after uncemented hip arthroplasty is related to stem size: DXA measurements in 138 patients followed for 2–7 years. Acta Orthop. 2006;77:386–392. doi: 10.1080/17453670610046307. [DOI] [PubMed] [Google Scholar]
- 33.Albanese CV, Santori FS, Pavan L, et al. Periprosthetic DXA after total hip arthroplasty with short vs. ultra-short custom-made femoral stems: 37 patients followed for 3 years. Acta Orthop. 2009;80:291–297. doi: 10.3109/17453670903074467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Falez F, Casella F, Panegrossi G, et al. Perspectives on metaphyseal conservative stems. J Orthop Traumatol. 2008;9:49–54. doi: 10.1007/s10195-008-0105-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Braun A, Papp J, Reiter A. The periprosthetic bone remodelling process–signs of vital bone reaction. Int Orthop. 2003;27(Suppl 1):S7–S10. [PubMed] [Google Scholar]
- 36.Reiter A, Gellrich JC, Bachmann J, Braun A. Changes of periprosthetic bone mineral density in cementless bicontact stem implantation; influence of different parameters–a prospective 4-year follow-up. Z Orthop Ihre Grenzgeb. 2003;141:283–288. doi: 10.1055/s-2003-40171. [DOI] [PubMed] [Google Scholar]
- 37.Sano K, Ito K, Yamamoto K. Changes of bone mineral density after cementless total hip arthroplasty with two different stems. Int Orthop. 2008;32:167–172. doi: 10.1007/s00264-006-0298-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Broeke RH, Hendrickx RP, Leffers P, et al. Randomised trial comparing bone remodelling around two uncemented stems using modified Gruen zones. Hip Int. 2012;22:41–49. doi: 10.5301/HIP.2012.9103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin RB. The effects of geometric feedback in the development of osteoporosis. J Biomech. 1972;5:447–455. doi: 10.1016/0021-9290(72)90003-6. [DOI] [PubMed] [Google Scholar]
- 40.Nishii T, Sugano N, Masuhara K, et al. (1997) Longitudinal evaluation of time related bone remodeling after cementless total hip arthroplasty. Clin Orthop Relat Res 339:121–131 [DOI] [PubMed]