Abstract
Purpose
We performed this study to determine whether the use of imageless navigation reduces revision rates after total knee arthroplasty (TKA).
Methods
Data of 1,121 consecutive primary TKA with a follow-up of one to six years were retrospectively analysed. Following the conversion of the standard technique from conventional to navigated procedures, these data included the last 342 conventional and first 779 navigated procedures performed in our clinic. Demographic and perioperative covariates were recorded. All patients were asked by post to report instances of revisions.
Results
Data of 1,054 patients (94 %) were complete. Mean follow-up was 3.9 years for conventional and 2.4 years for navigated operations. Cumulative revision rate averaged 4.7 % for conventional and 2.3 % for navigated procedures. Cox’s proportional hazard model was used to assess the effect of covariates on survival, resulting in significantly lower revision rates for older patients (p < 0.001) and for the navigated technique (p = 0.012). The reduced revision rate for navigated operations was mainly caused by a significantly reduced rate of aseptic implant loosening (1.9 % vs. 0.1 %, p = 0.024).
Conclusions
Our study showed lower revision rates when computer navigation was used. However, due to the retrospective uncontrolled design, further prospective trials will be necessary to further evaluate this effect.
Introduction
Imageless computer navigation was introduced as a standard implantation technique for total knee arthroplasties (TKA) more than a decade ago. According to arthroplasty registers, 11 % of all TKAs in Western Australia, 2 % in the UK, 19 % in Norway, and 0.7 % in Sweden have been implanted using computer navigation. Those regional distinctions show that the debate as to whether navigation is a reasonable technique is still in progress. Advocates of the conventional, mechanical alignment technique argue the computer navigation techniques increase operation times [1], elevate costs [2], raise fracture risk [3, 4], and that as yet long term results are unavailable [5, 6]. By contrast, proponents of the navigated technique refer to meta-analyses, which prove better postoperative alignment [7–9]. Even if the outcome of TKA is multifactorial, it is generally assumed that restoring the patient’s normal mechanical axis is of paramount importance [10]. This assumption is mainly based on studies that have identified higher revision rates for alignment outliers [10–12]. As the reduced risk of alignment outliers has been proven for navigated operations, advocates of the navigated procedure expect lower revision rates [7, 13]. In summary, the cornerstone between arguments by proponents and critics of computer navigation is a potentially reduced revision rate, which might outbalance higher procedural costs. Surprisingly, very few studies have so far analysed revision rates after conventional and navigated TKA. Therefore, the aim of our study was to compare midterm revision rates after conventional and navigated TKA.
Material and methods
Data from 1,345 consecutive patients who underwent TKA in the authors’ clinic between January 2006 and December 2010 were retrospectively analysed (Fig. 1). Exclusion criteria were TKA revisions, implantation of primary hinged or condylar constrained prostheses and implants with an antiallergic ceramic coating. The study comprised 1,121 patients who met those criteria. For economic reasons, two different cemented implants were used during this period, although there were no different medical indications [Press-Fit Condylar (PFC) Sigma, DePuy, Leeds, UK; NexGen Highflex, Zimmer, Warsaw, IN, USA). Data collection was performed in December 2011, which allowed a minimum follow-up of one to six years. In this period, the standard technique for TKAs in our clinic switched from conventional mechanical instruments to the imageless navigated procedure. Therefore, the 1,121 TKAs include the last mechanically aligned (n = 342) and the first navigated (n = 779) procedures in our institution. In January 2006, all patients were operated upon using mechanical alignment guides. After our first navigated procedure in June 2006, only one set of navigation instruments was available until 2008. In that period, the choice of alignment procedure was influenced only by instrument availability: we planned the first operation per day as a navigated procedure and the second as a mechanically aligned procedure. Choice of alignment procedure has not been influenced by patient-specific criteria, such as leg deformity or concomitant diseases. Since 2008, a second set of navigation instruments were available, and the computer-navigated procedure became the standard. Mechanical instruments were used only if no sterile set of instruments for mechanical alignment was accessible.
Fig. 1.
Patient selection for the study
Operative procedure
A medial parapatellar approach to the joint was used; the tibia-first technique was always performed. In the conventional group, extramedullary tibial and intramedullary femoral alignment jigs were used, as provided by the manufacturer. In the navigated group, reference arrays were fixed on Schanz screws in the femur and tiba. Thereafter, tibial and femoral cutting blocks were adjusted using imageless computer navigation. In both groups, the balanced-gap technique was performed to determine rotation of the femoral component. Pulsed lavage and vacuum-mixed antibiotic bone cement was used in every patient. All patients received a cemented implant without patellar resurfacing. The following data were recorded from patients’ documents: age, gender, height and weight, arthritis aetiology(primary, secondary; rheumatic, post-traumatic), operation date and side, operative procedure duration, implant and alignment procedure (conventional vs. navigated) types. Thereafter, all patients were asked by post to report any instances of revisions of the affected knee joint. If a revision was affirmed, type of and reason for revision were requested. According to the Swedish Knee Register, revisions were defined as a new operation in the previously resurfaced knee during which one or more component is exchanged, removed, or added [14]. The reasons for revision were grouped into one of the following categories: loosening, instability, infection, limited range of motion, and fracture.
Statistical analysis
Data was tested for normality using the Kolmogorov–Smirnov test. As normality has not been proven, a Mann–Whitney-U test was used, and for nominal categories, the chi-squared test was calculated. To identify independent risk factors influencing revision rate, a Cox’s proportional hazard model was calculated. For further analyse, Kaplan–Meier estimators with 95 % confidence intervals (CI) were calculated using the log-rank test (Mantel Cox). The level of significance was set at p < 0.05. calculated using the SPSS Statistics 19 software (IBM, Somers, USA).
Results
Data were complete in 1,054 patients (94 %) and are shown in Table 1. Due to our study design, the average time between operation and our survey was longer for conventional than for navigated procedures (3.9 vs. 2.4 years). The two groups were comparable concerning age, side, body mass index (BMI), and rate of primary arthritis. In the mechanical group, slightly more women (73 % vs. 65 %) and post-traumatic patients (6 % vs. 4 %) but fewer patients with rheumatoid arthritis (6 % vs. 8 %) were detected. The percentage of implanted PFC prostheses was significantly higher in the navigated than in the mechanical group. In the conventional group, the percentage of operations performed by residents under supervision of a consultant was significantly higher than in the navigated group. The navigation procedure prolonged the operation by a mean of six minutes [navigated: 124 minutes, range 70–240, standard deviation (SD) 22; conventional: 118 minutes, range 60–215, SD 31; p = 0.002].
Table 1.
Patients’ demographic data
| Conventional | Navigated | Total | Level of significance | |
|---|---|---|---|---|
| Number (n) | 322 | 732 | 1,054 | -- |
| Years after operation | 3.9 (1–6; 1) | 2.4 (1–5; 1) | 2.8 (1–6; 1) | <0.001b |
| Age (years) | 69 (40–87;9) | 69 (34–96; 9) | 68 (34–96; 9) | 0.620b |
| % female | 228 (73 %) | 474 (65 %) | 702 (67 %) | 0.035a |
| % left | 164 (53 %) | 351 (48 %) | 515 (49 %) | 0.401a |
| BMI | 31 (20–49; 5) | 31 (18–54; 5) | 31 (18–54; 5) | 0.792b |
| Primary arthritis (n) | 285 (89 %) | 646 (88 %) | 931 (88 %) | 0.994a |
| Rheumatism (n) | 20 (6 %) | 58 (8 %) | 78 (7 %) | 0.390a |
| Post-traumatic (n) | 19 (6 %) | 26 (4 %) | 45 (4 %) | 0.026a |
| Implant Nexgen (n) | 96 (30 %) | 57 (8 %) | 153 (15 %) | <0.001a |
| Implantat PFC (n) | 226 (70 %) | 675 (92 %) | 901 (85 %) | <0.001a |
| Consultant surgeon (n) | 233 (72 %) | 605 (82 %) | 838 (80 %) | <0.001a |
BMI body mass index, PFC press-fit condylar
aChi-squared test, bMann–Whitney U test
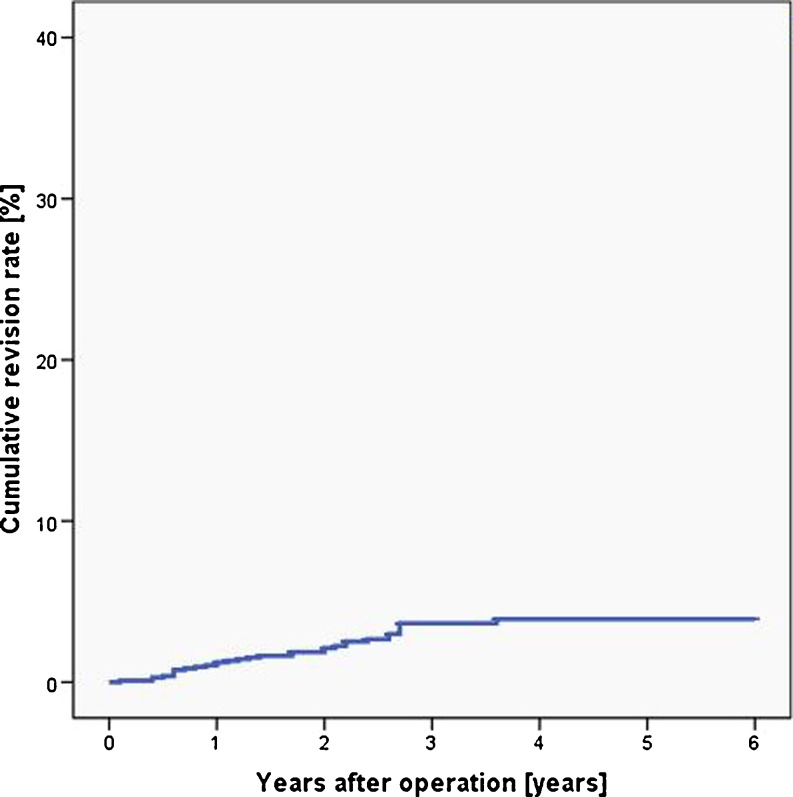
In our study population, 32 revisions (cumulative revision rate 3 %, Fig. 2) were detected. Of those 32, 15 occurred in the conventional group (cumulative revision rate 4.7 %)and 17 in the navigated group (cumulative revision rate 2.3 %).
Fig. 2.
Cumulative revision rate for all patients (blue line)
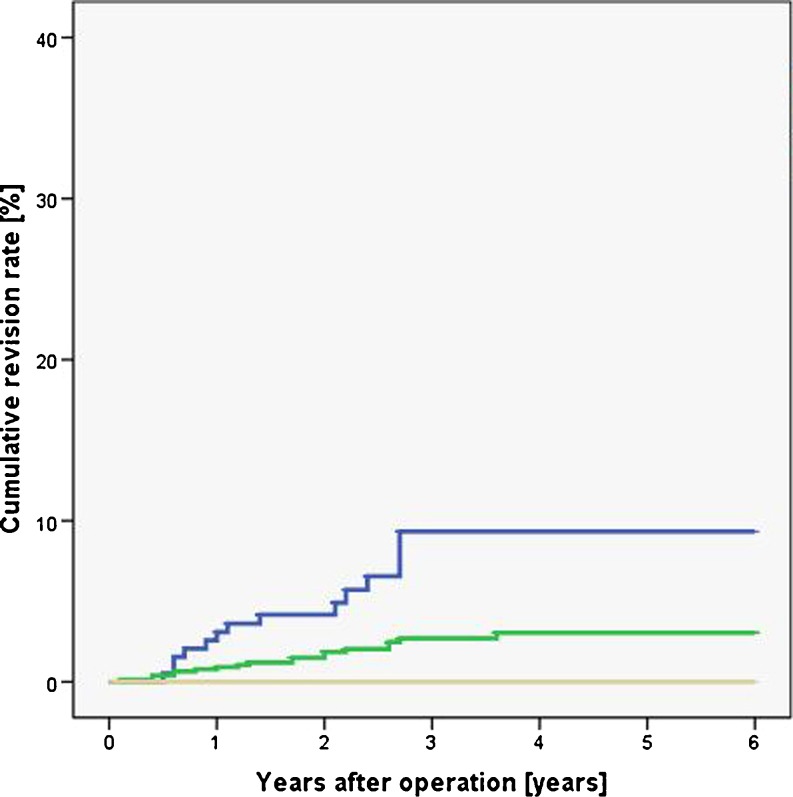
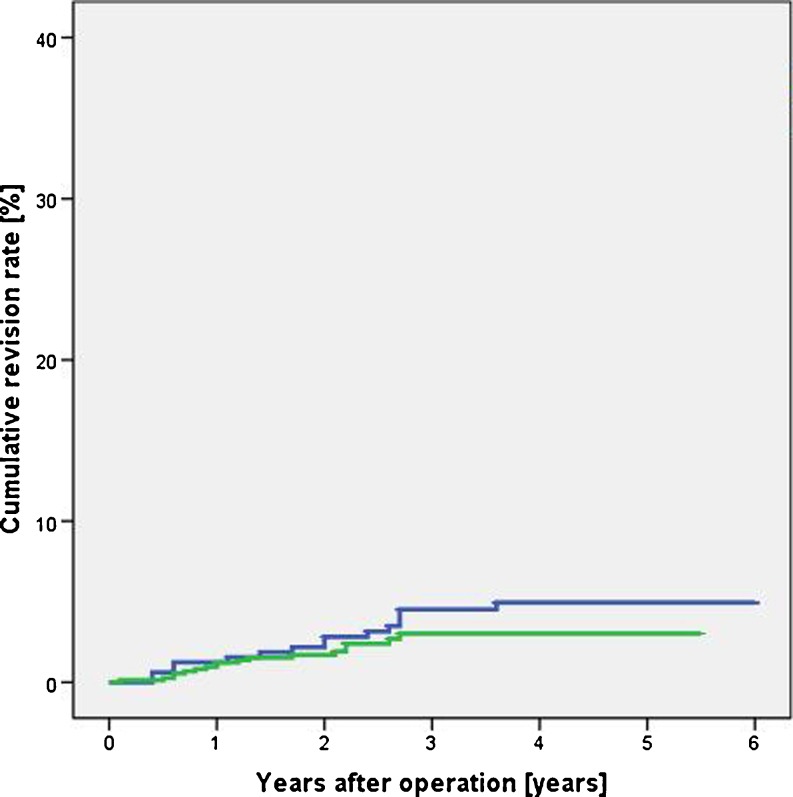
Further statistical analysis using a Cox proportional hazard model was undertaken to identify independent risk factors influencing revision rate. All demographic and operative factors were included in the Cox model: age, type of alignment (conventional vs. navigated), gender, implant (Nexgen vs. PFC), post-traumatic arthritis, rheumatism, BMI, side and level of surgeon’s expertise (consultant vs. resident). The results are shown in Table 2: the only factors, which influenced the revision rate independently, were patients’ age and the alignment procedure. Based on those results, a Kaplan Meier analysis was performed for the factors patients’ age and alignment procedure. Figure 3 shows significantly higher revision rates for younger patients, and Fig. 4 shows the lower revision rates for navigated procedures in comparison with conventional prostheses.
Table 2.
Results of the Cox proportional hazard model. Factors individually influencing revision rate are shown in bold
| Factors | Level of significance | 95 % confidence Interval |
|---|---|---|
| Age | < 0.001 | 0.096–0.466 |
| Alignment procedure | 0.012 | 0.146–0.801 |
| Gender | 0.093 | 0.899–4.669 |
| Posttraumatic arthritis | 0.499 | 0.287–12.481 |
| Side | 0.546 | 0.324–1.704 |
| Body mass index | 0.608 | 0.931–1.039 |
| Surgeon expertise | 0.862 | 0.475–2.452 |
| Rheumatism | 0.872 | 0.247–4.691 |
| Implant | 0.982 | 0.310–2.794 |
Fig. 3.
Cumulative revision rates for patients younger than 60 years (blue line), from 61 to 80 years (green line), and older than 80 years (grey line). Higher revision rates were identified in younger patients
Fig. 4.
Navigated alignment procedure (green line) reduced the cumulative revision rate in comparison with conventionally aligned prostheses (blue line)
Statistical analyses was performed to determine why conventionally aligned prostheses required more frequent revision. Kaplan–Meier estimators were calculated for the five subcategories of revision causes, and results are shown in Table 3. Computer navigation resulted in a significantly reduced rate of aseptic component loosening, and whereas instability was reduced by 47 %, it missed the level of significance. The type of alignment procedure had no effect on infection, fracture, or revision due to a limited range of motion.
Table 3.
Numbers of revisions and cumulative revision rates are shown for revision subcategories
| Conventional | Navigation | Level of significance | |||
|---|---|---|---|---|---|
| CRR (%) | Number | CRR (%) | Number | Log rank test (Mantel Cox) | |
| Aseptic loosening | 1.9 | 6 | 0.1 | 1 | 0.024 |
| Instability | 1.9 | 6 | 1 | 7 | 0.439 |
| Fracture | 0 | 0 | 0.1 | 1 | 0.451 |
| Limited range of motion | 0.6 | 2 | 0.7 | 5 | 0.662 |
| Infection | 0.3 | 1 | 0.4 | 3 | 0.795 |
Discussion
Meta-analyses clearly show that navigation provides a higher degree of accuracy in TKA [7–9]. However, the hypothesis that navigation decreases revision rate by providing better alignment, persists [15]. To date, few publications report midterm results of navigated versus conventional TKAs: most focus on postoperative function, involve less than 100 patients [16, 17], and provide no revision rates. Other studies report revision rates of navigated TKAs: Hernández-Vaquero et al. assessed 100 patients with a follow-up of eight years and detected similar revision rates between conventional and navigated techniques [18]. Harvie et al. evaluated 71 patients and found no revisions after five years [19], Pang et al. 140 patients and no revisions after two years [20], and Ishida 54 patients and one revision in each group after five years [21]. Lüring et al. performed a matched-pair analysis of 100 patients and detected no revision after five to seven years [22]. In a recently published study, Hoffart et al. compared five year results after 97 conventional and 98 navigated TKAs [23]. They detected one revision in each group, but follow-up was complete in only 62 % of patients. Besides those single-unit studies, Gothesen et al. presented data from the Norwegian Arthroplasty Register [6] after assessing 1,465 navigated and 8,214 conventional TKAs, with a mean follow-up of 1.4 years in the navigated and 1.8 years in the conventional group. Their statistical analysis found higher revisions rates for the navigated procedure (cumulative revisions rate at two years: navigated 3.6 %; conventional 2.1 %). Conversely, our study detected lower revisions rates for navigated operations (cumulative revision rate at two years: navigated 1.6 %, conventional 2.8 %). For a detailed analysis of these conflicting results, we assessed the reasons for revision. In our study, the decreased revision rate for navigated operations was due to a significantly lower rate of aseptic implant loosening and a reduced rate of joint instability. Similarly, Gothesen et al. found more revisions due to misalignment and femoral loosening for conventional procedures. However, this effect was outweighed by higher revision rates following the navigated technique due to tibial loosening and infection. We found no difference in infection rates between alignment techniques. At this time we can only speculate about reasons for these different results. Both studies used consecutive operations for analysis and no controlled or randomised groups. Our study assessed TKAs at a single institution, whereas Gothesen et al.’s was a multicentre study [6]. It is important to note that the authors found a higher revision rate for the navigated technique with implantation of the LCS Mobile-Bearing Total Knee System, which represented about 570 of the 1,465 procedures. They found no elevation in revision rate for other implants for which the same navigation device was used. They postulated that there might be brand-specific problems when matching computer navigation systems and prostheses brands. In our study equal revision rates were found for both implant brands. Another important difference is the implant fixation method. Gothesen et al. found revision rate of 20 % in uncemented femoral and 5–10 % in uncemented tibial components, whereas cemented prosthesis were used in all our patients. It is noteworthy that the higher revisions rate for navigated procedures found in the Norwegian Arthroplasty Register study is inconsistent not only with our study but with all the above-cited studies.
One aspect of our study focused on navigation-specific complications: some studies reported increased fracture rates after screw fixation[3, 4]; other authors suspected higher infection rates due to prolonged operative times [24]. A similar correlation has been published for hip replacements [25]. However, we detected only one femoral fracture in our navigation group and similar low infection rates in both groups. Gothesen et al.’s study from the Norwegian Arthroplasty Register [6] reported higher infection rates for navigated procedures, whereas in their meta-analysis, Cheng et al. found similar infection and fractures rates for navigated and conventional procedures [24]. In summary, we did not find higher revision rates for navigated procedures.
Our study has strengths and limitations: To our knowledge, the number of navigated procedures in our study is higher than in previous reports. Furthermore the follow-up rate of 94 % appears to be adequate. However, we performed a retrospective study of consecutive operations, and our study population therefore comprised differing factors such as age, prosthesis type, and the cause of arthritis. Certainly, this complicates data interpretation. To exclude significant impacts of those factors, a multivariate statistical analysis was performed that assessed all these factors, and the reduced revision rate for navigated procedures was still proven. Also, the number of patients in our study groups was substantially different due to conversion from the conventional to the navigated procedure. Therefore, the last 342 conventional TKAs were included as a control group for all navigated procedures performed in our clinic. The absence of control groups could lead to patient selection for navigated procedures. However, there was no specific patient selection for either procedure.
In conclusion, our study showed reduced TKA revision rates using the imageless computer navigation technique as a result of lower rates of aseptic implant loosening and instability and no elevation of complications. However, due to the uncontrolled design of the study, prospective, randomised, long-term studies are necessary to confirm lower revision rates after computer navigated TKA.
Acknowledgments
Conflict of interest
None
References
- 1.Bonutti PM, Dethmers DA, McGrath MS, Ulrich SD, Mont MA. Navigation did not improve the precision of minimally invasive knee arthroplasty. Clin Orthop Relat Res. 2008;466(11):2730–2735. doi: 10.1007/s11999-008-0359-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Callaghan JJ, Liu SS, Warth LC. Computer-assisted surgery: a wine before its time: in the affirmative. J Arthroplasty. 2006;21(4 Suppl 1):27–28. doi: 10.1016/j.arth.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Bonutti PM, Dethmers D, Ulrich SD, Seyler TM, Mont MA. Computer navigation-assisted versus minimally invasive TKA: benefits and drawbacks. Clin Orthop Relat Res. 2008;466(11):2756–2762. doi: 10.1007/s11999-008-0429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoke D, Jafari SM, Orozco F, Ong A. Tibial shaft stress fractures resulting from placement of navigation tracker pins. J Arthroplasty. 2011;26(3):504–508. doi: 10.1016/j.arth.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Berend ME (2009) Computer-assisted TKA: greater precision, doubtful clinical efficacy: affirms. Orthopedics 32 (9):orthosupersite-24 [DOI] [PubMed]
- 6.Gothesen O, Espehaug B, Havelin L, Petursson G, Furnes O. Short-term outcome of 1,465 computer-navigated primary total knee replacements 2005–2008. Acta Orthop. 2011;82(3):293–300. doi: 10.3109/17453674.2011.575743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bathis H, Shafizadeh S, Paffrath T, Simanski C, Grifka J, Luring C. Are computer assisted total knee replacements more accurately placed? A meta-analysis of comparative studies. Orthopade. 2006;35(10):1056–1065. doi: 10.1007/s00132-006-1001-3. [DOI] [PubMed] [Google Scholar]
- 8.Brin YS, Nikolaou VS, Joseph L, Zukor DJ, Antoniou J. Imageless computer assisted versus conventional total knee replacement. A Bayesian meta-analysis of 23 comparative studies. Int Orthop. 2011;35(3):331–339. doi: 10.1007/s00264-010-1008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu Y, Wang M, Liu Y, Fu Q (2011) Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. [epub ahead of print; doi:10.1007/s00167-011-1695-6] [DOI] [PubMed]
- 10.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 Suppl):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 11.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 12.Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 13.Mullaji A, Shetty GM (2009) Computer-assisted TKA: greater precision, doubtful clinical efficacy: opposes. Orthopedics 32 (9):orthosupersite-25 [DOI] [PubMed]
- 14.No authors listed (2011) The Swedish Knee Arthroplasty Register—Annual Report 2011 Part II
- 15.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the 15-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92(12):2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 16.Khan MM, Khan MW, Al-Harbi HH, Weening BS, Zalzal PK. Assessing short-term functional outcomes and knee alignment of computer-assisted navigated total knee arthroplasty. J Arthroplasty. 2012;27(2):271–277. doi: 10.1016/j.arth.2011.04.038. [DOI] [PubMed] [Google Scholar]
- 17.Lutzner J, Gunther KP, Kirschner S. Functional outcome after computer-assisted versus conventional total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1339–1344. doi: 10.1007/s00167-010-1153-x. [DOI] [PubMed] [Google Scholar]
- 18.Hernandez-Vaquero D, Suarez-Vazquez A, Iglesias-Fernandez S. Can computer assistance improve the clinical and functional scores in total knee arthroplasty? Clin Orthop Relat Res. 2011;469(12):3436–3442. doi: 10.1007/s11999-011-2044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harvie P, Sloan K, Beaver RJ (2011) Computer Navigation vs Conventional Total Knee Arthroplasty 5-year Functional Results of a Prospective Randomized Trial. J Arthroplasty. [epub ahead of print; doi:10.1016/j.arth.2011.08.009] [DOI] [PubMed]
- 20.Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN (2011) Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc [epub ahead of print; doi: 10.1007/s00167-011-1483-3] [DOI] [PubMed]
- 21.Ishida K, Matsumoto T, Tsumura N, Kubo S, Kitagawa A, Chin T, Iguchi T, Kurosaka M, Kuroda R. Mid-term outcomes of computer-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1107–1112. doi: 10.1007/s00167-010-1361-4. [DOI] [PubMed] [Google Scholar]
- 22.Luring C, Kauper M, Bathis H, Perlick L, Beckmann J, Grifka J, Tingart M, Rath B. A 5 to 7 year follow-up comparing computer-assisted vs freehand TKR with regard to clinical parameters. Int Orthop. 2012;36(3):553–558. doi: 10.1007/s00264-011-1297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffart HE, Langenstein E, Vasak N (2012) A prospective study comparing the functional outcome of computer-assisted and conventional total knee replacement. J Bone Joint Surg Br 94(2):194–199 [DOI] [PubMed]
- 24.Cheng T, Pan XY, Mao X, Zhang GY, Zhang XL (2011) Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee. [epub ahead of print; doi:10.1016/j.knee.2011.10.001] [DOI] [PubMed]
- 25.Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010;468(1):52–56. doi: 10.1007/s11999-009-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]