Abstract
Purpose
The objective of this study was to evaluate the morphological characteristics of Schatzker type IV tibial plateau fractures.
Methods
A retrospective analysis of radiographic and computed tomographic data of tibial plateau Schatzker type IV fractures from January 2010 to December 2011 was conducted in a level 1 trauma centre. The medial fracture angle (MFA), surface area percentage (SAP), and medial fracture height (MFH) were measured on CT images using the Picture Archiving and Communication System.
Results
Based on the location of fracture and the MFA, 75 cases of Schatzker type IV fracture were divided into three subtypes: anteromedial fracture (seven cases, 9.3 %), total medial plateau fracture (36 cases, 48 %), and posteromedial fracture (32 cases, 42.7 %). The anteromedial fracture was located on the anterior part of the medial plateau, the average MFA was positive 47.5°, the SAP was 38.3 % and the MFH was 41.6 mm. The total medial plateau fracture usually involved the entire medial plateau, the mean value of MFA was 81.2°, the SAP was 53.9 % and the MFH was 64.0 mm. The posteromedial fracture was located on the posterior part of the medial plateau, the MFA was negative 42.5°, the SAP was 32.4 % and the MFH was 44.8 mm.
Conclusion
The direction and location of Schatzker type IV fractures are highly variable. Proper operative approach and fixation method should be selected based on the morphological characteristics of individual medial plateau fractures.
Introduction
Schatzker classification is the most common system of classifying tibial plateau fractures in clinical practice. Based on location, morphology, and treatment, fractures are divided into six general types. Type IV fractures are fractures that occur in the medial plateau. They account for 10–30 % of all tibial plateau fractures [1–3]. In most textbooks, the fracture lines of type IV fracture are described lying in sagittal plane, and medial buttress plating is widely recommended [4].
Compared with plain radiographs, CT scans can provide detailed information on intra-articular fractures. With the widespread use of CT, it was found that in some type IV cases, especially in the posteromedial shearing fractures, the fracture line may appear on the coronal plane [5, 6]. In clinical practice, medial buttress plating for these fractures often has a high rate of fixation failure. The posteromedial fragment is difficult to stabilize though a standard medial approach [7–9]. Failure of primary fixation often results in secondary varus deformity, an unstable knee, and deterioration in the long-term results [10].
Thorough understanding of the fracture morphology can help orthopedic surgeons better understand the mechanism of injury and to plan appropriate surgical procedures. In the present study, CT images from patients with Schatzker IV fractures were analysed retrospectively to clarify the morphologic characteristics of these fractures.
Patients and methods
The retrospective study was conducted at a level 1 trauma center. Eighty-seven patients with Schatzker type IV tibial plateau fractures from January 2010 to December 2011 were retrieved from the orthopedic trauma database in our institution. Fracture types in this database were verified by senior surgeons at the time of post-operation. Exclusion criteria were age under 18 years, previous knee surgery and/or existing knee deformity. Additional, patients without adequate imaging documentation (incomplete X-ray or CT images) were excluded.
Finally, 75 (86.2 %) fractures were finally identified during the study period. Of these, 47 were male and 28 were female, with an average of 35 years (range, 17–67 years). The injury mechanisms were traffic accident in 51 cases, fall from a height in 17 cases, and simply fall injury in seven cases.
Radiographic measurements
The images were evaluated on clinical Picture Archiving and Communication (PACS) System workstations by one orthopedic trauma resident surgeon and one radiologist specializing in musculoskeletal radiology. The morphologic characteristics of the medial plateau fracture was described using the measurement parameters proposed by Bare [5] and Higgins [6]. All measurements were reviewed simultaneously by the two observers and agreement was reached by consensus.
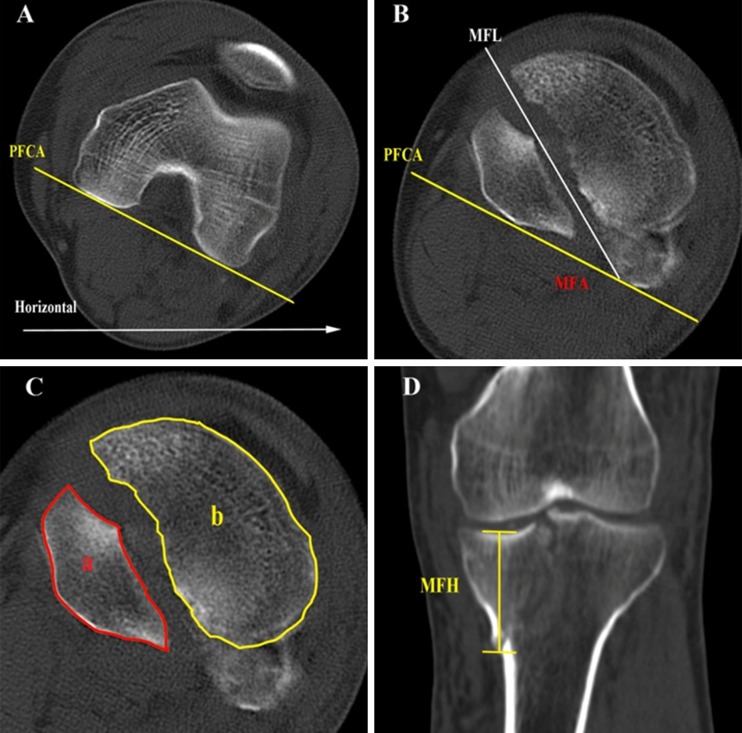
Axial angle of fracture
In the transverse view, the posterior femoral condylar axis (PFCA), the line connecting the posterior aspects of the femoral condyles, acted as a neutral axis for the coronal plane (Fig. 1a). Major fracture angle (MFA) was determined by measuring the angle between the PFCA and the major fracture line of the plateau (Fig. 1b). To distinguish fracture direction, the MFA was considered positive if internally rotated relative to the PFCA and negative if externally rotated relative to the PFCA (cf. Fig. 4).
Fig. 1.
a The posterior femoral condylar axis (PFCA) was used as the reference line to determine the angle of lower extremity rotation relative to horizontal plane. b The major fracture angle (MFA) was determined by measuring the angle between PFCA and main fracture line. c The surface area (SA) was determined by calculating the percent of Areaa/(Areaa+Areab). d The MFH was determined by measuring the joint line to the most distal extent of the medial fragment
Fig. 4.
Posteromedial fracture. The fracture is located on the posterior of tibial plateau, and its fracture line is from anteromedial to posterolateral
Surface area
In the transverse view, the area of the medial of fragment and the remaining cross-sectional area of the plateau were measured on the same section that the fibular head first appeared. Then, surface area percentage (SAP) was determined by calculating the medial fragment area to the entire plateau area (Fig. 1c).
Medial fragment height
Utilizing the coronal or sagittal CT reformation, the medial fragment height (MFH) was obtained by measuring the joint line to the most distal extent of the medial fragment (Fig. 1d). If CT reformations were not available, the MFH was determined by calculating the number of scan slices containing the fragment and multiplying by the slice thickness.
Statistical analysis
All statistical analyses were performed using SPSS software (version 17.0). Data were subjected to Kolmogorov-Smirnov test and one-way analysis of variance (ANOVA). A P <0.05 was considered statistically significant.
Results
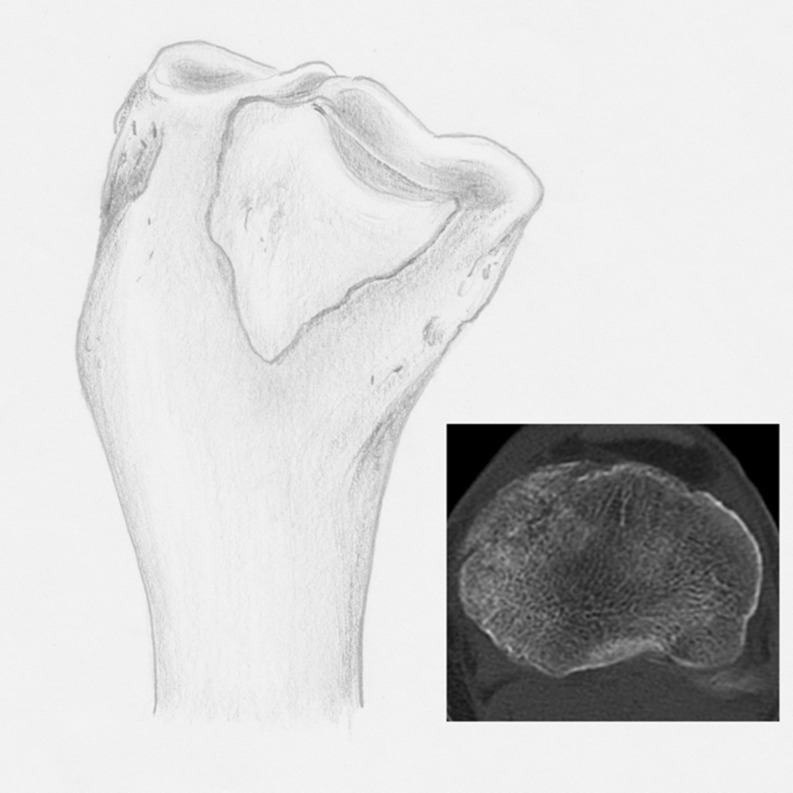
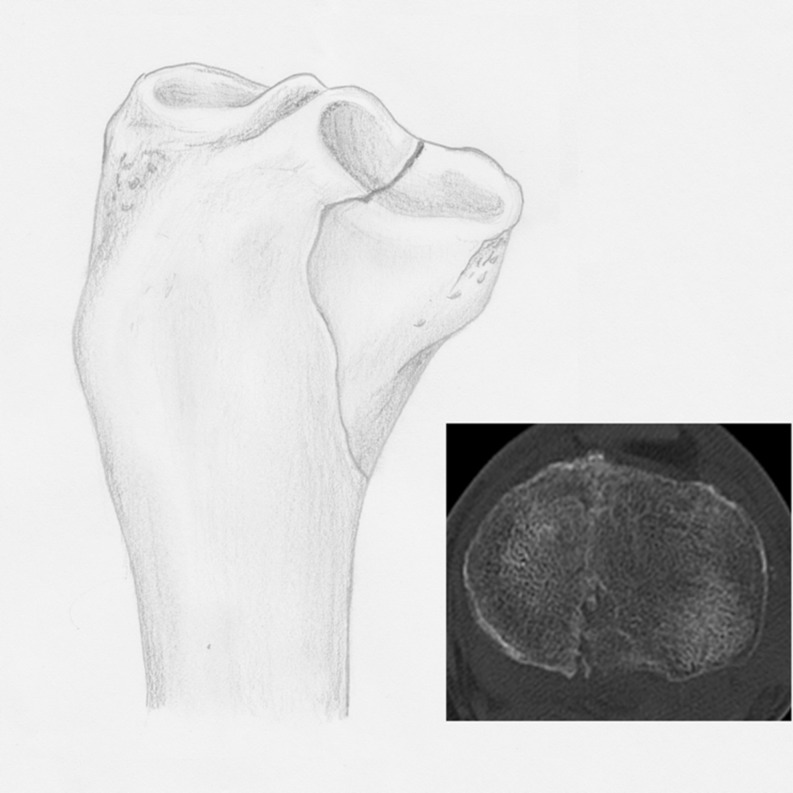
On the basis of fracture location and the MFA, Schatzker type IV fractures were further categorized into three subtypes: anteromedial fracture, total medial plateau fracture, and posteromedial fracture. The fragment of the anteromedial fracture is mainly located on the anterior part of the medial plateau, the MFA is positive, and its fracture line is from anterolateral to posteromedial (Fig. 2). In the total medial plateau fractures, the fracture almost involved the entire medial plateau, the MFA is close to 90°, and the fracture line is usually from anterior to posterior (Fig. 3). The posteromedial fracture is located on the posterior part of the medial plateau, the MFA is negative, and the fracture line is in an anteromedial to posterolateral direction (Fig. 4).
Fig. 2.
Anteromedial fracture. The fracture is located anterior of the tibial plateau, and its fracture line is from anterolateral to posteromedial
Fig. 3.
Total medial fracture. The fracture is involving the entire medial plateau and its fracture line is usually from anterior to posterior
According to this classification system, among the 75 cases, there were seven anteromedial fractures, 36 total medial plateau fractures and 32 posteromedial fractures, which accounted for 9.3 %, 48.0 %, and 42.7 %, respectively. According to split or depression, there were three depression fractures, 16 split fractures, 39 split-depression fractures, and 17 comminuted fractures. The three pure depression fractures were anteromedial fractures. Twenty-seven split-depression fractures were posteromedial fractures, with a split fracture on the posteromedial plateau and a depression fracture on the posterolateral plateau. Seventeen comminuted fractures were of the total medial plateau fractures, which manifested by splitting the medial plateau into two separate fragments, anteromedial and posteromedial.
The mean MFA, SAP and MFH in three different fracture subtypes are shown in Table 1. For the three parameters, there were no significant differences between anteromedial and posteromedial fractures. However, the mean MFA, SAP and MFH in total medial plateau fractures were larger than those in anteromedial and posteromedial fractures, suggesting that total medial plateau fractures generally involved a larger region.
Table 1.
The values of MFA, SAP, and MFH in three fracture types
| Fracture type | MFA (n = 4, degrees) | SAP (n = 36, %) | MFH (n = 32, mm) |
|---|---|---|---|
| Anteromedial fracture | 47.5 ± 7.1 | 38.3 ± 10.4 | 41.3 ± 6.3 |
| Total medial fracture | 81.2 ± 6.9a,b | 53.9 ± 10.9a,b | 64.0 ± 19.5a,b |
| Posteromedial fracture | 42.5 ± 11.2 | 32.4 ± 9.2 | 44.8 ± 10.5 |
MFA major fracture angle, SAP surface area percentage, MFH medial fragment height
Data was expressed as mean ± SD. Three pure medial depression fractures in the anteromedial fracture group were excluded in statistical analysis. To eliminate the impact of fracture direction (positive or negative), absolute values were adopted to compare the differences of MFA in the three fracture types
aP < 0.05, when compared to anteromedial fracture
bP < 0.05, when compared to posteromedial fracture
Discussion
The results of this study showed Schatzker type IV tibial plateau fractures may be distributed at different locations on the medial plateau and their fracture lines may run in various directions. Therefore, different operative approach and fixation should be selected for different fracture type of medial plateau fractures.
In almost all schematic diagrams from textbooks, Schatzker type IV fractures are described as fractures in which the fracture line is along the anteroposterior axis. The placement of buttress plates through the medial approach has become the accepted method of treating this type of fracture. However, it seems that not all Schatzker type IV fractures are well managed with medially placed plates. Luo et al. [11] analysed 17 cases of failed medial plateau fracture treatment and found that seven fixations had failed due to improper placement of medial buttress plating. Among these, four were medial comminuted fractures and three were posteromedial shearing fractures. Displacement occurred in all cases.
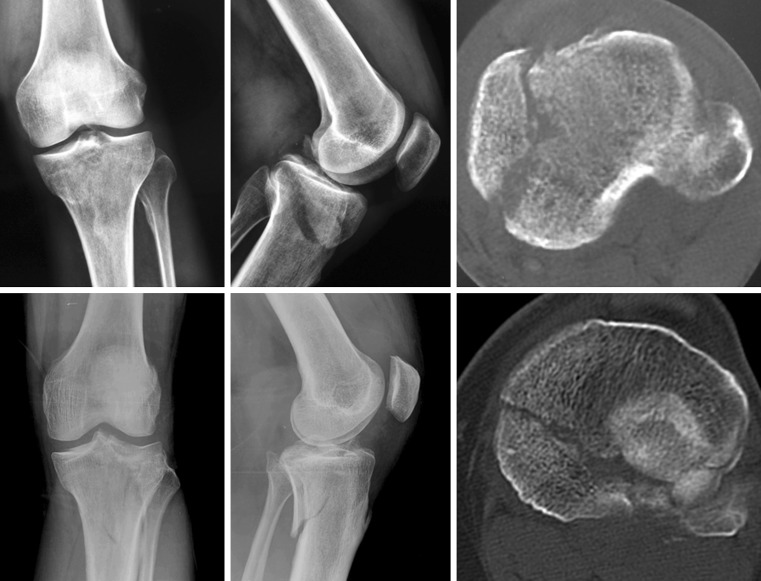
Because CT has been in use in medicine for less than 30 years, the evaluation and classification of fractures mainly relies on two-dimensional X-ray images. With great respect to the work of Dr. Schatzker, we find that it is not completely appropriate to classify all medial plateau fractures into one single type, especially now that CT has become a routine part of the diagnosis of intra-articular fractures. With the assistance of CT, we found Schatzker type IV fractures may be located on the anteromedial, posteromedial or entire medial plateau, even in some cases, the posterolateral plaeau may also be involved, though few differences in these fractures appear on anteroposterior view radiograph (Fig. 5).
Fig. 5.
Although few differences appeared on anteroposterior (AP) view radiograph, the location and direction of these two Schaztker type IV fractures are distinctly different on CT axial images. Different surgical approaches should be selected for these two fractures to stabilize the medial fragments
In this series, total medial plateau fractures are still the majority, and more than 50 % area of the plateau, on average, appears involved as indicated by CT axial images. This supported the previous view that Schatzker type IV fractures may cross the intercondylar eminence and may involve part of the lateral plateau. Anteromedial fractures are relatively uncommon, accounting for 9.3 % of the fractures in this population. It may be the reason why these fractures were not given too much attention previously. The posteromedial fractures were not uncommon, which accounted for 42.7 % in this series. Unlike previously reported, the fracture lines of posteromedial fractures were seldom located on the coronal plane, but were rather typically oblique along the anteromedial to posterolateral direction [9, 12]. As indicated by lateral radiograph or 3D CT reconstruction, 1/2 or 1/3 of the medial plateau was displaced posteriorly, and the distal end of the fragment was often located at the posteromedial aspect of the plateau.
Fracture fixation should be based on the individual characteristics of each fracture, such as location, morphology, and mechanism of injury. According to the direction of fracture line and the location of the fracture, we deduce that the three subtypes may be due to three different types of mechanism of injury. Previously, it was generally believed that medial plateau fracture was caused by a varus force on knee joint. However, based on the results of our morphologic study, we propose that cause of medial plateau fractures is related to the position of the knee joint at injury, extension or flexion. A total medial plateau fracture may occur when the knee joint is at a near neutral position, and anteromedial and posteromedial fractures often occur when the knee joint is in extension or flexion. The direction of the fracture line and the involved region of these two subtypes of fractures may be related to the degree of knee joint flexion. Nevertheless, the true mechanism of injury for different types of fractures should be determined through further experimental investigation.
To our knowledge, there are few systems of classification that specially address medial plateau fractures. Wahlquist’s classification is based on the site of the fracture, the medial condyle, inter condyle or lateral condyle [13]. This classification system is recommended for evaluation of the injuries of cruciate ligament and neurovascular bundle. Although it provides considerable detail, the AO/OTA classification system is too complex to memorize, and it often fails to provide a clear guide for surgical planning. Luo proposed a three-column classification system based on CT, in which the posteromedial fractures were classified into the posterior column factures [14]. In this study, based on the morphological characteristics of fractures obtained from CT scans and reconstruction, we further divided medial plateau fractures into three subtypes. This can be used as a supplement to the Schatzker classification system, and it would help promote understanding the mechanism of injury and allow better development of surgical plans for the treatment of medial plateau fractures.
The present study has two potential limitations. First, the research institution is the leading trauma center in southern China for high-severity fractures; therefore, the ratio of the three subtypes of medial plateau fractures probably does not represent the true ratio in the general population. Second, only four split fractures among the anteromedial fractures were used for statistical analysis, so the results might be biased.
Footnotes
Guang Yang and Yi Zhu contributed equally to this study.
References
- 1.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 2.Moore TM. Fracture–dislocation of the knee. Clin Orthop Relat Res. 1981;156:128–140. [PubMed] [Google Scholar]
- 3.Bennett WF, Browner B. Tibial plateau fractures: a study of associated soft tissue injuries. J Orthop Trauma. 1994;8(3):183–188. doi: 10.1097/00005131-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Lowe JA, Tejwani N, Yoo B, Wolinsky P. Surgical techniques for complex proximal tibial fractures. J Bone Joint Surg Am. 2011;93(16):1548–1559. [PubMed] [Google Scholar]
- 5.Barei DP, O'Mara TJ, Taitsman LA, Dunbar RP, Nork SE. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma. 2008;22(3):176–182. doi: 10.1097/BOT.0b013e318169ef08. [DOI] [PubMed] [Google Scholar]
- 6.Higgins TF, Kemper D, Klatt J. Incidence and morphology of the posteromedial fragment in bicondylar tibial plateau fractures. J Orthop Trauma. 2009;23(1):45–51. doi: 10.1097/BOT.0b013e31818f8dc1. [DOI] [PubMed] [Google Scholar]
- 7.Zeng ZM, Luo CF, Putnis S, Zeng BF. Biomechanical analysis of posteromedial tibial plateau split fracture fixation. Knee. 2011;18(1):51–54. doi: 10.1016/j.knee.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Fakler JK, Ryzewicz M, Hartshorn C, Morgan SJ, Stahel PF, Smith WR. Optimizing the management of Moore type I postero-medial split fracture dislocations of the tibial head: description of the Lobenhoffer approach. J Orthop Trauma. 2007;21(5):330–336. doi: 10.1097/BOT.0b013e318055603c. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharyya T, McCarty LP, 3rd, Harris MB, Morrison SM, Wixted JJ, Vrahas MS, Smith RM. The posterior shearing tibial plateau fracture: treatment and results via a posterior approach. J Orthop Trauma. 2005;19(5):305–310. [PubMed] [Google Scholar]
- 10.Luo CF, Jiang R, Hu CF, Zeng BF. Medial double-plating for fracture dislocations involving the proximal tibia. Knee. 2006;13(5):389–394. doi: 10.1016/j.knee.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Luo CF, Rui J. Analysis of failed surgical treatment of the medial tibial plateau fractures. Chin J Orthop Trauma. 2006;8(7):642–646. [Google Scholar]
- 12.Boeck H, Opdecam P. Posteromedial tibial plateau fractures. Operative treatment by posterior approach. Clin Orthop Relat Res. 1995;320:125–128. [PubMed] [Google Scholar]
- 13.Wahlquist M, Iaguilli N, Ebraheim N, Levine J. Medial tibial plateau fractures: a new classification system. J Trauma. 2007;63(6):1418–1421. doi: 10.1097/TA.0b013e3181469df5. [DOI] [PubMed] [Google Scholar]
- 14.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24(11):683–692. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]