Abstract
Purpose
The purpose of this study was to evaluate the clinical outcomes of osteochondral autograft transplantation (OAT) for juvenile osteochondritis dissecans (JOCD) lesions of the knee, especially time to return to sports.
Methods
Twelve knee JOCD lesions with OCD grade 3 and 4 categorised by magnetic resonance imaging (MRI) were treated with OAT. Nine male and two female skeletally immature patients averaging 13.7 years old were included. The OCD lesions were assessed arthroscopically and then fixed in situ using multiple osteochondral plugs harvested under fluoroscopy from the distal femoral condyle without damaging the physis. International Cartilage Repair Society (ICRS) score and Lysholm score were assessed pre- and postoperatively.
Results
After a mean follow-up of 26.2 ± 15.1 months, the International Knee Documentation Committee (IKDC) subjective score significantly improved (p < 0.01). According to the IKDC score, objective assessment showed that ten of 12 (83 %) had excellent results (score: A) after OAT and significantly improved (p < 0.01). Based on ICRS criteria, results were satisfactory in all patients. No patients experienced complications at the graft harvest site. All patients returned to their previous level of athletic activity at an average of 5.7 months after the surgery.
Conclusions
OAT for JOCD of the knee provided satisfactory results in all patients at a mean follow-up of 26.2 months.
Introduction
Osteochondritis dissecans (OCD) was first described by Paget in 1870. OCD is defined as “a fragment of articular cartilage together with subchondral bone that has become separated partly or completely from a joint surface”. This classically occurs on the lateral aspect of the medial femoral condyle.
OCD of the knee is often subcategorised into juvenile osteochondritis dissecans (JOCD) and adult OCD. JOCD occurs most frequently in children who are athletically active between the age of ten and 20, with a mean age of 13.4 years at diagnosis [1, 2]. The difference between JOCD and adult OCD depends on skeletal maturity determined by whether the physis is closed. This categorisation is useful because JOCD has shown more spontaneous healing with conservative treatment than adult OCD [3–7]. In addition, the stability of the OCD is important, because stable fragments more frequently respond to conservative therapy [8, 9]. When JOCD is properly categorised, non-weight-bearing and immobilisation for six weeks followed by activity modification has reportedly led to successful healing by three to 12 months in up to 90 % of cases [2, 4, 6, 10]. However, patients failing to heal after conservative treatment require surgical interventions resulting in a long drawn out healing process. As unstable OCD lesions frequently fail to respond to conservative treatment and thus often require surgical intervention, correct assessment of JOCD stability prior to treatment selection is important.
When surgery is necessary, the optimum surgical treatment for unstable lesions remains controversial [2]. In general, unstable lesions require partial removal with debridement to remove fibrous tissue and restore vascularity, followed by drilling [11], screw fixation [12, 13], osteochondral autologous transplantation (OAT), autologous chondrocyte implantation [14] and a combination of them [15]. However, there have been a few reports of OAT used as surgical treatment for JOCD [16, 17].
The purpose of this study was to evaluate the clinical outcomes of OAT for JOCD lesions of the knee. In this paper we report the functional outcome of surgical treatment with OAT in 12 JOCD lesions, assessed as grade 3 or 4 by magnetic resonance imaging (MRI).
Materials and methods
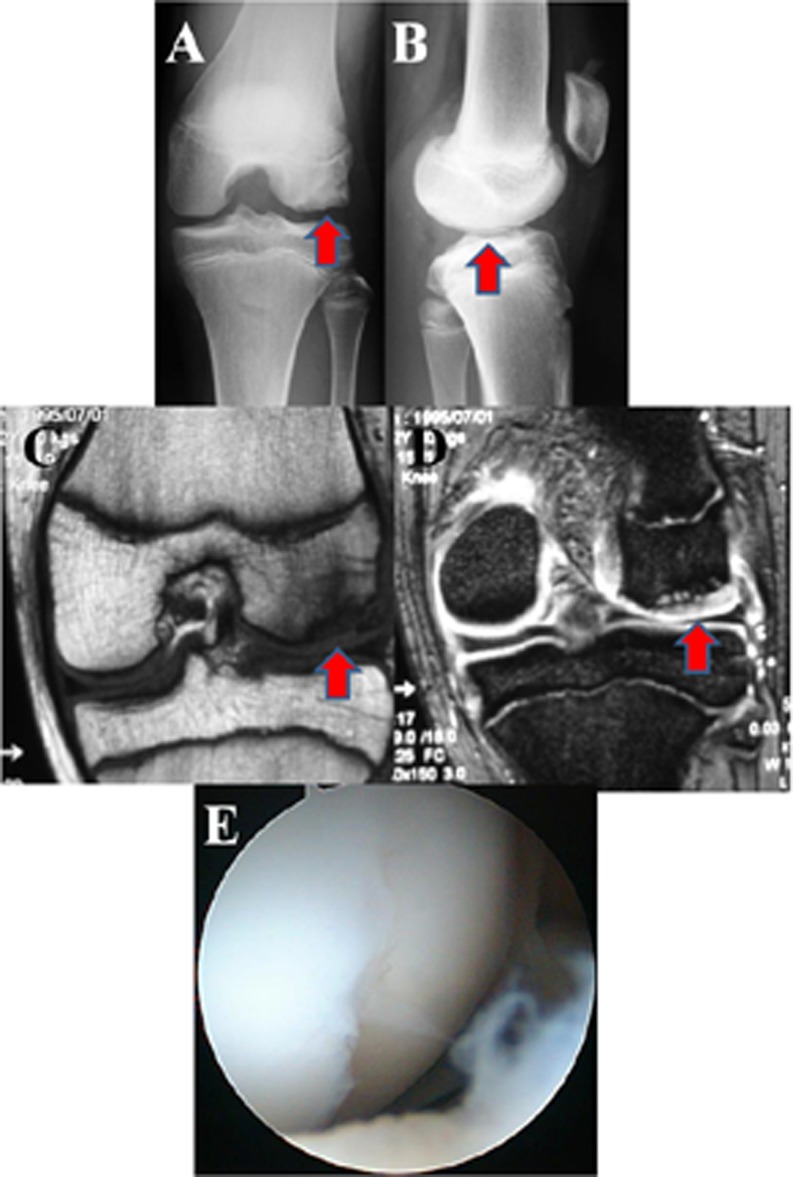
OAT was performed in 12 knees (nine boys and two girls, one boy was a bilateral case) for JOCD. All patients had open physes and persistent pain in their knees despite restrictions in their daily activities (Fig. 1a, b). Their OCD lesions were confirmed by radiography and MRI using the Nelson et al. classification [18] (Fig. 1c, d). The images were assessed based on T2-weighted images: grade 0, normal; grade 1, intact cartilage with signal changes; grade 2, a high-signal breach of the cartilage; grade 3, a thin, high-signal rim extending behind the osteochondral fragment, indicating synovial fluid around the fragment; and grade 4, mixed- or low-signal loose body, either in the centre of the lesion or free within the joint.
Fig. 1.
A 13-year-old girl with JOCD of the lateral femoral condyle who became asymptomatic after OAT (case 9). Anteroposterior radiograph reveals a lucent lesion (arrow) on the lateral femoral condyle (a). Lateral view (b). Coronal T1-weighted (c) and T2-weighted (d) MRI examinations of the knee performed before surgery showing a bone fragment in situ and high-signal intensity line between the bone and the fragment (grade 3) (arrow). Arthroscopic examination of the JOCD lesion of this case demonstrated a cartilage fissure in the lateral femoral condyle. The lesion was relatively stable on probing (e)
JOCD lesions with MRI grades of 3 or 4 were selected for treatment with OAT (grade 3, ten knees; grade 4, two knees). The patients desired an early return to previous activities.
The mean time from the onset to the operation was 13.5 months (range three to 36). All of them were primary operations. The mean age at surgery was 13.7 years (range 12–16 years old) and the mean follow-up was 26.2 months (range six to 60 months).
Surgical techniques
All patients underwent arthroscopic surgery with standard anterior portals (Fig. 1e). The JOCD lesion was assessed for congruity and stability of the chondral surface according to the International Cartilage Repair Society (ICRS) classification of OCD lesions [19]. For ICRS OCD II (partial discontinuity, stable on probing), the articular fissure was probed. For ICRS OCD III (complete discontinuity, “dead in situ”, not dislocated), when the fragment was relatively stable, debridement was not performed. When the lesion had an unstable fragment, it was gently debrided. For ICRS OCD IV (dislocated fragment, loose within the bed or empty defect), the lesion base was debrided. All patients with ICRS OCD IV had no large fragment or loose body. The diameter of the plugs was determined based on the defect size. The mean lesion size was 2.7 cm2.
Small cylindrical osteochondral plugs were retrieved via a small arthrotomy from the non-weight-bearing regions of the ipsilateral or contralateral knee and implanted into the holes well-prepared using an OAT device (OATS, Arthrex, Inc., Naples, FL, USA or Mosaicplasty, Smith & Nephew Endoscopy, Andover, MA, USA). To prevent damage to the epiphyseal plate, we harvested plugs from part of the femoral condyle distal from the physis. The size and number of the osteochondral grafts that would adequately cover the JOCD defects or fix the JOCD lesions were decided by using sizers before recipient holes were created in the JOCD lesions. To avoid damage to the physis, the osteochondral plugs were carefully harvested using fluoroscopy from the distal side of the physis. When the fragment of JOCD was stable (ICRS OCD II and III), the fragment was fixed by osteochondral plugs. In case of total loss of cartilage (ICRS OCD IV), we performed the original mosaicplasty technique to resurface the chondral defect [20–22].
Rehabilitation protocol
After surgery, the knee was immobilised for one week with a knee brace, and range of motion exercises were started from week two. Weight-bearing was not permitted during the first four weeks postoperatively. Full weight-bearing was allowed from seven weeks after surgery. After 12 weeks, patients gradually returned to their sports with a moderate level of athletic activity to the degree that their pain permitted.
Evaluation
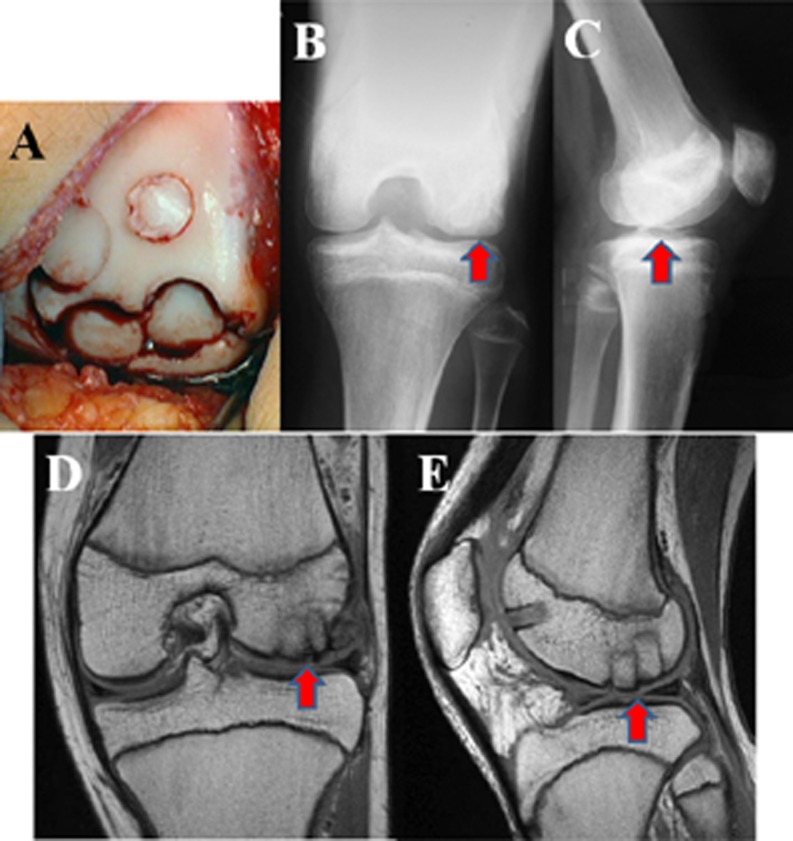
Radiographs were obtained at three and six months after surgery for evaluation of the cartilage surface and subchondral bone at the graft implant and harvest site (Fig. 2d, e).
Fig. 2.
Examination of case 9 revealed ICRS OCD III. The cartilage was fixed by four 6-mm diameter osteochondral plugs (13 mm length) harvested from the ipsilateral lateral condyle (a). Two-month postoperative radiographs of case 9 demonstrated apparently smooth joint congruity and an open physis (b, c). Coronal T1-weighted (d) and sagittal T1-weighted (e) MRI of the knee performed 2 months later showed that the intensity of the lesion was similar to that of the surrounding normal articular cartilage, but an interface still existed between the plugs and subchondral bone
The clinical outcome was analysed at three and six months after the operation using the International Knee Documentation Committee (IKDC) form.
Follow-up assessment also included the rating system described by Lysholm to evaluate clinical results [23]. In addition, we recorded when the patients returned to their previous levels of athletic activity.
Statistical analysis
Statistical analysis was performed using a paired t test and Wilcoxon signed rank test to determine the effect of OAT for JOCDs. The Wilcoxon signed rank test was used for comparison of preoperative and postoperative IKDC objective results. Significance was set at p < 0.05.
Results
The patients’ data are shown in Table 1. Eight of the chondral lesions were situated on the medial and four on the lateral femoral condyle. Arthroscopic findings and ICRS OCD classification showed grade II in nine knees, grade III in one knee and grade IV in two knees. The mean number of plugs was 2.3 ± 1.2. In three cases, one plug was used, and in five cases, two plugs were used. The reason we used more than three plugs in four cases was that the JOCD lesions were larger than the others. The diameter of the osteochondral plugs was between 3.5 and 10 mm.
Table 1.
Patient data
| Case no. | Age (years) | Sex | Location | Pre-op Lysholm score | Pre-op IKDC subjective | Pre-op IKDC surgeons | ICRS OCD classification | Lesion size (cm2) | Diameter and no. of osteochondral plugs | Post-op Lysholm score | Post-op IKDC subjective | Post-op IKDC surgeons | Follow-up (months) | Return to sports (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | M | LFC | 50 | 45.2 | C | IV | 1.3 | 3.5 mm ×1 | 80 | 83.5 | A | 60 | 12 |
| 2 | 15 | M | LFC | 67 | 63.9 | D | II | 1.8 | 4.5 mm ×1 | 100 | 94.9 | A | 18 | 6 |
| 3 | 15 | M | MFC | 62 | 60.9 | C | IV | 1 | 8.5 mm ×1 | 100 | 89.7 | A | 48 | 4.5 |
| 4 | 13 | M | MFC | 76 | 78.2 | C | II | 1.5 | 6 mm ×2 | 100 | 100 | A | 29 | 4 |
| 5 | 15 | M | MFC | 86 | 59 | C | II | 4.5 | 6 mm ×3, 8 mm ×2 | 100 | 60.2 | B | 32 | 8 |
| 6 | 12 | M | MFC | 67 | 58.7 | C | II | 3.8 | 6 mm ×2 | 94 | 89.5 | A | 24 | 6 |
| 7 | 16 | M | MFC | 87 | 64.6 | B | II | 4 | 8 mm ×2, 6 mm ×1 | 95 | 92 | A | 12 | 4 |
| 8 | 14 | M | MFC | 95 | 88 | C | II | 2.5 | 8 mm ×1, 10 mm ×1 | 100 | 100 | A | 22 | 3 |
| 9 | 13 | F | LFC | 77 | 58.6 | C | III | 5 | 8 mm ×3, 6 mm ×1 | 96 | 89.7 | A | 15 | 5 |
| 10 | 13 | M | MFC | 74 | 66.7 | C | II | 2.7 | 8 mm ×2 | 96 | 83.9 | A | 24 | 6 |
| 11 | 13 | M | MFC | 74 | 66.7 | C | II | 2.4 | 8 mm ×3 | 96 | 83.9 | A | 24 | 6 |
| 12 | 13 | M | LFC | 71 | 50.6 | C | II | 2 | 6 mm ×2 | 95 | 86.2 | B | 6 | 4 |
| Mean | 13.7 | 74.1 | 63.4 | 2.7 | No. of plugs 2 | 96.0* | 87.8* | 26.2* | 5.7 |
IKDC International Knee Documentation Committee, ICRS International Cartilage Repair Society, LFC lateral femoral condyle, MFC medial femoral condyle
*p < 0.01 in comparison with preoperative score
In the entire series, there were no infections. The preoperative IKDC subjective score for patients averaged 63.4 ± 11.3 points, and the score significantly increased to 87.8 ± 10.4 points at six months after surgery (p < 0.01). The preoperative IKDC objective scores, which were class B in one patient, class C in ten patients and class D in one patient, were significantly improved at six months after surgery with class A in ten patients and class B in two patients (p < 0.01).
The average Lysholm scores six months after the operation were significantly improved to 96.0 ± 5.6 points compared to the preoperative score of 74.1 ± 12.0 points (p < 0.01).
All patients returned to their previous level of athletic activity at an average of 5.7 ± 2.4 months after surgery.
Discussion
The most important finding of this study was that the use of OAT for JOCD of the knee was a potential strategy to provide good clinical outcome with earlier return to activities. In this study, OAT for JOCD of the knee provided satisfactory results in all 12 patients at a mean follow-up of 26.2 months.
JOCD and adult OCD are separate entities, differentiated by whether there is growth plate fusion. JOCD of the knee has a much better prognosis than adult OCD. When patients are properly selected, results of non-operative treatment for JOCD of the knee are very successful. In fact, a course of conservative therapy is proposed for skeletally immature patients with stable (grade 1 or 2) OCD lesions [7, 24–26]. However, even among these patients, if there are continued symptoms or healing failure confirmed by radiograph or MRI findings after six to 12 months, surgical treatment is indicated. Although conservative treatment by restricting daily activities and sporting activities is reasonable, many athletes do not want to stop sports activities for six to 12 months or have to change their activities. Such patients may also be candidates for earlier surgery.
To obtain successful clinical outcomes, monitoring the type and stage of OCD lesions is essential. Although Brückl et al. described a classification based on radiography, some researchers have encountered patients in whom the arthroscopic findings did not correspond with their radiographic classification [27]. Because of this, Nelson et al. reported on the classification of OCDs by MRI [18]. This classification is simple and useful for monitoring OCD lesions preoperatively and corresponds well to arthroscopic findings. Based on the classification, therefore, we performed OAT for JOCD in all patients with grade 3 or grade 4 lesions. Patient selection based on these criteria enabled us to obtain excellent results including significant improvement in objective and subjective IKDC scores. In addition, clinical results assessed by Lysholm score were also significantly improved postoperatively.
In our series, all patients returned to their previous levels of athletic activity as early as 5.7 months. There is no report that mentions the period of return to sports activity after OAT for JOCD. Gudas et al. reported superiority of OAT to microfracture [28]; 93 % of athletes receiving OAT for the treatment of articular cartilage defects (adult OCDs) returned to sports activities at their pre-injury levels at an average of 6.5 months after the operation (range four to eight months). On the other hand, 52 % of athletes after microfracture returned to their previous sports activities at the same time. Peterson et al. reported that patients who were treated for JOCD with autologous chondrocyte transplantation were able to return to work and athletic activity within 18 months after surgery [29]. Thus, when patients are appropriately selected, it seems OAT can promote successful outcomes in JOCD lesions of the knee.
Recently, two studies introduced the use of OAT for JOCD, and both reported that biological fixation with cylindrical osteochondral autografts provided healing of the osteochondral fragment with promising results [16, 17]. However, to the best of our knowledge, this study is the first case series to show the clinical results of treatment with OAT for JOCD lesions. Although most patients with JOCD heal successfully with conservative treatment, in some patients, surgical treatment, especially by OAT, may be useful.
However, there are some limitations to this study. Although no abnormalities were noted in any patients at the final follow-up, long-term observation is necessary to monitor any unexpected long-term complications especially in lesions at the harvest site. Moreover, the utility of this operation should be further substantiated by a randomised study comparing it to another operative procedure.
In conclusion, we performed OAT for 12 JOCD lesions of the knee, MRI grades 3 or 4. All patients were subsequently symptom free and suffered no side effects such as infection or restriction of knee motion. Based on our study, we believe that OAT for JOCD is a useful choice for surgical treatment when patients are appropriately selected.
Acknowledgment
The authors thank Ms. Janina Tubby for help in preparing the manuscript.
References
- 1.Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am. 1984;66:1340–1348. [PubMed] [Google Scholar]
- 2.Robertson W, Kelly BT, Green DW. Osteochondritis dissecans of the knee in children. Curr Opin Pediatr. 2003;15:38–44. doi: 10.1097/00008480-200302000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Linden B. Osteochondritis dissecans of the femoral condyles: a long-term follow-up study. J Bone Joint Surg Am. 1977;59:769–776. [PubMed] [Google Scholar]
- 4.Pappas AM. Osteochondrosis dissecans. Clin Orthop Relat Res. 1981;158:59–69. [PubMed] [Google Scholar]
- 5.Twyman RS, Desai K, Aichroth PM. Osteochondritis dissecans of the knee. A long-term study. J Bone Joint Surg Br. 1991;73:461–464. doi: 10.1302/0301-620X.73B3.1670450. [DOI] [PubMed] [Google Scholar]
- 6.Williams JS, Jr, Bush-Joseph CA, Bach BR., Jr Osteochondritis dissecans of the knee. Am J Knee Surg. 1998;11:221–232. [PubMed] [Google Scholar]
- 7.Yoshida S, Ikata T, Takai H, Kashiwaguchi S, Katoh S, Takeda Y. Osteochondritis dissecans of the femoral condyle in the growth stage. Clin Orthop Relat Res. 1998;346:162–170. doi: 10.1097/00003086-199801000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Bonhdorf K. Osteochondritis (osteochondrosis) dissecans: a review and new MRI classification. Eur Radiol. 1998;8:103–112. doi: 10.1007/s003300050348. [DOI] [PubMed] [Google Scholar]
- 9.Dipaola J, Nelson DW, Colville M. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy. 1991;7:101–104. doi: 10.1016/0749-8063(91)90087-E. [DOI] [PubMed] [Google Scholar]
- 10.Garrett JC. Osteochondritis dissecans. Clin Sports Med. 1991;10:569–593. [PubMed] [Google Scholar]
- 11.Hayan R, Phillipe G, Ludovic S, Claude K, Jean-Michel C. Juvenile osteochondritis of femoral condyles: treatment with transchondral drilling. Analysis of 40 cases. J Child Orthop. 2009;4(1):39–44. doi: 10.1007/s11832-009-0225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson LL, Uitvlugt G, Austin MD, Detrisac DA, Johnson C. Osteochondritis dissecans of the knee: arthroscopic compression screw fixation. Arthroscopy. 1990;6:179–189. doi: 10.1016/0749-8063(90)90073-M. [DOI] [PubMed] [Google Scholar]
- 13.Kocher MS, Czarnecki JJ, Andersen JS, Micheli LJ. Internal fixation of juvenile osteochondritis dissecans lesions of the knee. Am J Sports Med. 2007;35:712–718. doi: 10.1177/0363546506296608. [DOI] [PubMed] [Google Scholar]
- 14.Micheli LJ, Moseley JB, Anderson AF, et al. Articular cartilage defects of the distal femur in children and adolescents: treatment with autologous chondrocyte implantation. J Pediatr Orthop. 2006;26:455–460. doi: 10.1097/01.bpo.0000224565.72762.eb. [DOI] [PubMed] [Google Scholar]
- 15.Steinhagen J, Bruns J, Deuretzbacher G, Ruether W, Fuerst M, Niggemeyer O. Treatment of osteochondritis dissecans of the femoral condyle with autologous bone grafts and matrix-supported autologous chondrocytes. Int Orthop. 2010;34:819–825. doi: 10.1007/s00264-009-0841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berlet GC, Mascia A, Miniaci A. Treatment of unstable osteochondritis dissecans lesions of the knee using autogenous osteochondral grafts (mosaicplasty) Arthroscopy. 1999;15:312–316. doi: 10.1016/S0749-8063(99)70041-1. [DOI] [PubMed] [Google Scholar]
- 17.Miura K, Ishibashi Y, Tsuda E, Sato H, Toh S. Results of arthroscopic fixation of osteochondritis dissecans lesion of the knee with cylindrical autogenous osteochondral plugs. Am J Sports Med. 2007;35:216–222. doi: 10.1177/0363546506294360. [DOI] [PubMed] [Google Scholar]
- 18.Nelson DW, DiPaola J, Colville M, Schmidgall J. Osteochondritis dissecans of the talus and knee: prospective comparison of MR and arthroscopic classifications. J Comput Assist Tomogr. 1990;14:804–808. doi: 10.1097/00004728-199009000-00026. [DOI] [PubMed] [Google Scholar]
- 19.ICRS Cartilage Injury Evaluation Package. Available via http://www.cartilage.org/_files/contentmanagement/ICRS_evaluation.pdf
- 20.Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003;85-A(Suppl 2):25–32. doi: 10.2106/00004623-200300002-00004. [DOI] [PubMed] [Google Scholar]
- 21.Hangody L, Kish G, Kárpáti Z, Udvarhelyi I, Szigeti I, Bély M. Mosaicplasty for the treatment of articular cartilage defects: application in clinical practice. Orthopedics. 1998;21:751–756. doi: 10.3928/0147-7447-19980701-04. [DOI] [PubMed] [Google Scholar]
- 22.Matsusue Y, Yamamuro T, Hama H. Arthroscopic multiple osteochondral transplantation to the chondral defect in the knee associated with anterior cruciate ligament disruption. Arthroscopy. 1993;9:318–321. doi: 10.1016/S0749-8063(05)80428-1. [DOI] [PubMed] [Google Scholar]
- 23.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 24.Smet AA, Ilahi OA, Graf BK. Untreated osteochondritis dissecans of the femoral condyles: prediction of patient outcome using radiographic and MR findings. Skeletal Radiol. 1997;26:463–467. doi: 10.1007/s002560050267. [DOI] [PubMed] [Google Scholar]
- 25.Glancy GL. Juvenile osteochondritis dissecans. Am J Knee Surg. 1999;12:120–124. [PubMed] [Google Scholar]
- 26.Sales de Gauzy J, Mansat C, Darodes PH, Cahuzac JP. Natural course of osteochondritis dissecans in children. J Pediatr Orthop B. 1999;8:26–28. doi: 10.1097/00009957-199901000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Brückl R, Rosemeyer B, Thiermann G. Results of operative treatment of osteochondrosis dissecans of the knee joint in juveniles. Z Orthop Ihre Grenzgeb. 1982;120:717–724. doi: 10.1055/s-2008-1051384. [DOI] [PubMed] [Google Scholar]
- 28.Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G, Smailys A. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21:1066–1075. doi: 10.1016/j.arthro.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 29.Peterson L, Minas T, Brittberg M, Lindahl A. Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am. 2003;85-A(Suppl 2):17–24. doi: 10.2106/00004623-200300002-00003. [DOI] [PubMed] [Google Scholar]