Abstract
Background and purpose
Carotid intima-media thickness (CIMT) is a subclinical marker of cardiovascular disease (CVD). Recent studies suggest that shorter sleep duration is a risk factor for CVD, but there is limited evidence regarding this association using high-quality, objective assessments of sleep. The aim of this study is to determine whether sleep duration is associated with CIMT.
Methods
The study used an observational cohort consisting of 617 black and white middle-aged healthy participants (37–52 y; 58% female) in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Multivariable-adjusted linear regression analyses were performed. Sleep duration was measured using wrist actigraphy monitors. CIMT was calculated using the average of 20 measurements of the mean common carotid, bulb and internal CIMT, which was assessed using ultrasound images.
Results
After adjusting for covariates, one hour of longer sleep duration was associated with 0.026 mm less CIMT among men (p=0.02, 95% CI -0.047, -0.005), and 0.001 mm less CIMT among women (p=0.91, 95% CI -0.020, 0.022). Segment-specific analyses indicated that the carotid bulb was a key driver of the observed association.
Conclusions
Shorter objectively assessed sleep duration was associated with greater CIMT among men but not women.
Keywords: Sleep, carotid intima-media thickness, atherosclerosis, cardiovascular disease
INTRODUCTION
A growing body of evidence suggests that sleep duration may be a potential risk factor for cardiovascular disease (CVD).1–3 Findings have been somewhat inconsistent both as to whether there is a significant association and whether it differs by sex. Evidence suggests that “shorter sleepers,” those reporting sleeping <6 hours, and “longer sleepers,” those reporting sleeping >8 hours, have earlier CVD mortality compared to those sleeping 7–8 hours.1–3
One limitation of these studies is that most used self-reported sleep duration,4 which can introduce misclassification leading to biased estimates.5, 6 Studies using objective measures of sleep duration may provide better evidence regarding the association between sleep duration and CVD. Furthermore, given that there are sex differences in both sleep characteristics and in subclinical CVD,7, 8 studies that investigate the potential differences by sex will add to our understanding of the relationships between sleep duration and CVD risk. Recent studies found associations between sleep duration and risk factors for CVD such as blood pressure, lipids, metabolic syndrome and subclinical markers of coronary atherosclerosis, such as coronary artery calcification.3, 9–11 Carotid intima media thickness (CIMT) serves as a potential subclinical marker of CVD risk, and has been associated with increased risk of myocardial infarction and stroke.12–15 CIMT may be involved in the association between sleep duration and CVD, however evidence is needed using an objective assessment rather than self-reported sleep.
Consequently, the primary aim of this study was to evaluate associations between objectively assessed sleep duration (using actigraphy) and CIMT among participants from the Coronary Artery Risk Development in Young Adults (CARDIA) study, and determine whether the associations vary by sex.
METHODS
Study Sample
Participants included 617 middle-aged black and white adults from the CARDIA study, an ongoing, prospective cohort study (N=5115), who were initially recruited in 1985 from four study sites across the US (Chicago, IL, Minneapolis, MN, Birmingham, AL, Oakland, CA.) Additional details regarding methods, study design and recruitment can be found elsewhere.16 An ancillary sleep study at the year 15 CARDIA follow-up was conducted at the Chicago site, and all non-pregnant site participants (N=814) were invited to participate; 669 (82%) consented and completed the sleep monitoring. CIMT was measured among 3258 of the 3549 (92%) participants at the year 20 CARDIA visit (2005–2006). Of the 669 participants from the ancillary sleep study, 617 (76%) also had CIMT assessed, and 52 did not have CIMT assessed and were not included in the study. Findings from the CARDIA year 15 general sleep questionnaire indicated no significant differences in the self-reported sleep time between the ancillary sleep study participants and those who declined to participate.17 The Institutional Review Boards of Northwestern University and the University of Chicago approved the protocol, and all participants provided informed consent.
Sleep Assessment
Sleep duration was estimated using wrist actigraphy monitors, which are omnidirectional accelerometer devices that measured wrist movements in 30-second intervals (Actiwatch-16, Mini-Mitter Inc, Bend, Oregon). Data collection was conducted 24 hours per day for 3 consecutive days while participants carried out typical activities, including sleeping in their own home. Three-day measures were taken twice (approximately one year apart) between 2003 and 2005, and the average of six monitored nights was calculated to estimate mean sleep duration. The variation in the day-to-day sleep time did not affect the association between mean sleep duration and IMT, and no significant differences persisted in participants’ average sleep duration for year 1 and year 2 data collection (p=0.431). In addition, previous reports suggest that the variability in day-to-day and year-to-year sleep time was minimal.18 Additional information regarding scoring and interpretation of data collected with this device has been described elsewhere.19 Validation studies of actigraphy data indicate that these devices are highly valid and reliable, with a correlation of 0.81–0.90 compared to polysomnography for total sleep time.20
Carotid Intima Media Thickness Assessment
Carotid ultrasounds were performed by centrally-trained technicians using standard procedures and equipment (GE Logiq 700, Issaquoah, Ill.) and were read at a single center (Tufts Medical Center, Boston, MA). High-resolution B-mode ultrasound images were measured at 3 locations, the common carotid artery (CCA), the carotid artery bulb (bulb), and the internal carotid artery (ICA). The transducer operated at a frequency of 13 MHz for the CCA and 9MHz for the bulb and the ICA. The carotid ultrasound procedures were performed in the supine position, and magnified gray scale images of the far and near wall of distal CCA, the bulb and the proximal ICA were obtained on the right and left sides. The primary CIMT outcome variable used in this study represents an average of the mean CIMT measure that was calculated using 20 different measurements from the 3 CIMT segments (4 CCA, 8 bulb, 8 ICA). In a subanalysis, we also assessed the mean of the max CIMT measure, as well as the segment-specific associations. One image was acquired for each side of the CCA, and two images for each side of the bulb and ICA. The first image was taken at 45° to the horizontal, and the second image was taken at 20° to 25°. The certified reader reviewed images using validated image analysis algorithm software as an aid. Pearson correlation coefficients based on the 58 replicate studies were 0.86 for CCA, 0.72 for the bulb, and 0.88 for the ICA.21
Statistical Analysis
Multivariable-adjusted linear regression models were used to evaluate the cross-sectional associations between objectively assessed sleep duration and CIMT. The models were first adjusted for potential confounders, including age, sex and race. Next, additional plausible mechanisms were added to the model including BMI, depression, smoking, waist circumference, triglycerides, LDL cholesterol, HDL cholesterol, diabetes, systolic blood pressure, diastolic blood pressure, IL-6, CRP, physical activity, alcohol consumption, caffeine consumption, blood pressure and cholesterol medication, sleep fragmentation and snoring. Covariates were kept in the full model if they were significantly associated with CIMT in the full model (p<0.10), or were important to include for theoretical reasons. Variables excluded from the final model were IL-6, CRP, triglycerides, physical activity, alcohol consumption, medication, sleep fragmentation and snoring. The model for sleep duration was also tested for a deviance from linear trend to assure that multiple variable linear regression models were appropriate.
Effect modification by sex and race was assessed using formal statistical tests for two-way interactions. No significant interaction was observed by sleep duration and race (p=0.96), however a marginal interaction was observed by sex and sleep duration (p=0.07), and therefore sex-stratified linear regression analyses were conducted. In addition, subanalyses were conducted to address the association between objectively assessed sleep duration and the mean of the max CIMT, as well as the segment-specific IMT associations. All data were analyzed using SAS version 9.2 software (SAS Institute Inc, Cary, NC).
RESULTS
Characteristics of study participants are shown for men and women separately in Tables 1 and 2. CIMT measurements and sleep duration differed by sex. Men had significantly lower mean sleep duration compared to women (5.8 hours (SD 1.1) vs. 6.3 hours (SD 1.0), p<0.001). Men also had significantly greater CIMT compared to women (0.74 mm (SD 0.13) vs. 0.68 mm (SD 0.12), p<0.001). (TABLE 1, TABLE 2)
Table 1.
Distribution of Study Population by Sleep Duration and Carotid CIMT among Men
| Demographics | Overall (%) |
Mean Sleep Duration (hours) (SD) (N=260) |
P- value* |
Mean Carotid CIMT (mm) (SD) (N=260) |
P- value* |
|---|---|---|---|---|---|
| All male participants (N=260) | 5.8(1.1) | 0.74(0.13) | |||
| Age | |||||
| 37 – 41 years | 14.2 | 5.7(1.3) | 0.52 | 0.68(0.11) | <0.01 |
| 42 – 46 years | 30.8 | 5.7(1.2) | 0.74(0.11) | ||
| 47 – 52 years | 55.0 | 5.8(1.0) | 0.76(0.14) | ||
| Race | |||||
| Black | 36.5 | 5.2(1.1) | <0.01 | 0.75(0.12) | 0.32 |
| White | 63.5 | 6.1(0.9) | 0.73(0.14) | ||
| Education | |||||
| Less than high school degree | 7.0 | 5.1(1.3) | <0.01 | 0.79(0.10) | 0.01 |
| High school degree | 22.8 | 5.4(1.4) | 0.75(0.14) | ||
| Some college | 15.1 | 5.5(1.1) | 0.77(0.16) | ||
| College graduate | 55.2 | 6.1(0.9) | 0.72(0.12) | ||
| Covariates | |||||
| Body mass index | |||||
| ≥30 kg/m2 (obese) | 30.0 | 5.6(1.2) | 0.26 | 0.77(0.13) | <0.01 |
| 25 – 29.9 kg/m2(overweight) | 45.0 | 5.8(1.0) | 0.74(0.11) | ||
| <25 kg/m2(normal) | 25.0 | 5.8(1.2) | 0.70(0.15) | ||
| Waist circumference | |||||
| >90 cm | 63.9 | 5.8(1.1) | 0.53 | 0.76(0.12) | <0.01 |
| ≤90 cm | 36.2 | 5.7(1.2) | 0.71(0.14) | ||
| Systolic blood pressure | |||||
| >120 mmHg | 41.5 | 5.5(1.2) | <0.01 | 0.78(0.15) | <0.01 |
| ≤120 mmHg | 58.5 | 6.0(1.0) | 0.71(0.11) | ||
| Diastolic blood pressure | |||||
| >80 mmHg | 19.6 | 5.4(1.3) | <0.01 | 0.79(0.17) | <0.01 |
| ≤80 mmHg | 80.4 | 5.9(1.0) | 0.73(0.12) | ||
| High-density lipoprotein cholesterol | |||||
| <52 mg/dL (below median) | 70.7 | 5.8(1.1) | 0.67 | 0.74(0.13) | 0.53 |
| ≥52 mg/dL (above median) | 29.3 | 5.7(1.1) | 0.73(0.13) | ||
| Low-density lipoprotein cholesterol | |||||
| >109 mg/dL (above median) | 51.8 | 5.7(1.1) | 0.87 | 0.75(0.14) | 0.29 |
| ≤109 mg/dL (below median) | 48.2 | 5.8(1.1) | 0.73(0.12) | ||
| Diabetes | |||||
| Yes | 6.5 | 5.3(1.6) | 0.08 | 0.77(0.10) | 0.42 |
| No | 93.5 | 5.8(1.1) | 0.74(0.13) | ||
| Alcohol | |||||
| >7 drinks/week | 36.9 | 5.7(1.2) | 0.60 | 0.75(0.14) | 0.02 |
| 1–7 drinks/week | 42.8 | 5.9(0.9) | 0.74(0.14) | ||
| Non-drinker | 20.3 | 5.6(1.2) | 0.69(0.10) | ||
| Smoking | |||||
| Current smoker | 28.9 | 5.4(1.3) | 0.02 | 0.78(0.16) | 0.09 |
| Former smoker | 33.3 | 5.7(1.0) | 0.74(0.12) | ||
| Never smoker | 37.8 | 5.9(1.0) | 0.73(0.13) | ||
| Depression (mean CES-D) | |||||
| CES-D≥16 | 15.8 | 5.6(1.1) | <0.01 | 0.77(0.13) | 0.01 |
| CES-D<16 | 84.2 | 5.8(1.1) | 0.73(0.13) | ||
Abbreviations: CIMT, intima-media thickness
p-values reflect t-test or ANOVA test for those with 3 or more categories
Table 2.
Distribution of Study Population by Sleep Duration and Carotid CIMT among Women
| Demographics | Overall (%) | Mean Sleep Duratio n (hours) (SD) (N=357) |
P- value* |
Mean Carotid CIMT (mm) (SD) (N=357) |
P- value* |
|---|---|---|---|---|---|
| All participants (N=357) | 6.3(1.0) | 0.68(0.12) | |||
| Age | |||||
| 37 – 41 years | 21.3 | 6.2(1.0) | 0.76 | 0.64(0.09) | <0.01 |
| 42 – 46 years | 29.7 | 6.5(1.0) | 0.66(0.12) | ||
| 47 – 52 years | 49.0 | 6.3(0.9) | 0.70(0.13) | ||
| Race | |||||
| Black | 48.5 | 5.9(0.9) | <0.01 | 0.71(0.13) | <0.01 |
| White | 51.5 | 6.7(0.8) | 0.65(0.11) | ||
| Education | |||||
| Less than high school degree | 4.2 | 5.7(0.6) | <0.01 | 0.71(0.15) | <0.01 |
| High school degree | 17.7 | 6.2(1.1) | 0.70(0.14) | ||
| Some college | 27.5 | 6.1(1.0) | 0.71(0.14) | ||
| College graduate | 50.7 | 6.5(0.9) | 0.65(0.10) | ||
| Covariates | |||||
| Body mass index | |||||
| ≥30 kg/m2 (obese) | 36.2 | 6.1(0.9) | <0.01 | 0.72(0.13) | <0.01 |
| 25 – 29.9 kg/m2 (overweight) | 25.0 | 6.3(1.0) | 0.69(0.12) | ||
| <25 kg/m2 (normal) | 36.2 | 6.6(0.9) | 0.63(0.11) | ||
| Waist circumference | |||||
| >90 cm | 34.8 | 6.2(1.0) | 0.01 | 0.72(0.13) | <0.01 |
| ≤90 cm | 65.2 | 6.4(0.9) | 0.66(0.11) | ||
| Systolic blood pressure | |||||
| >120 mmHg | 25.8 | 6.2(1.0) | 0.04 | 0.73(0.12) | <0.01 |
| ≤120 mmHg | 74.2 | 6.4(0.9) | 0.66(0.12) | ||
| Diastolic blood pressure | |||||
| >80 mmHg | 21.4 | 6.09(1.0) | 0.02 | 0.72(0.12) | <0.01 |
| ≤80 mmHg | 78.7 | 6.37(1.0) | 0.67(0.12) | ||
| High-density lipoprotein cholesterol | |||||
| <52 mg/dL (below median) | 33.8 | 6.1(1.0) | 0.01 | 0.70(0.11) | 0.05 |
| ≥52 mg/dL (above median) | 66.2 | 6.4(0.9) | 0.67(0.13) | ||
| Low-density lipoprotein cholesterol | |||||
| >109 mg/dL (above median) | 47.3 | 6.4(0.9) | 0.23 | 0.70(0.13) | <0.01 |
| ≤109 mg/dL (below median) | 52.7 | 6.3(0.9) | 0.70(0.11) | ||
| Diabetes | |||||
| Yes | 8.4 | 6.2(0.9) | 0.10 | 0.76(0.15) | <0.01 |
| No | 91.6 | 6.3(1.0) | 0.67(0.12) | ||
| Alcohol | |||||
| >7 drinks/week | 19.5 | 6.7(0.9) | <0.01 | 0.67(0.13) | <0.01 |
| 1–7 drinks/week | 45.0 | 6.5(1.0) | 0.67(0.12) | ||
| Non-drinker | 35.5 | 6.2(0.9) | 0.70(0.13) | ||
| Smoking | |||||
| Current smoker | 30.6 | 6.0(1.0) | 0.01 | 0.71(0.14) | 0.01 |
| Former smoker | 44.6 | 6.4(0.9) | 0.70(0.13) | ||
| Never smoker | 24.9 | 6.6(0.9) | 0.64(0.11) | ||
| Depression (mean CES-D) | |||||
| CES-D≥16 | 22.0 | 6.0(1.1) | <0.01 | 0.68(0.12) | 0.19 |
| CES-D<16 | 78.0 | 6.4(0.9) | 0.68(0.12) | ||
Abbreviations: CIMT, intima-media thickness
p-values reflect t-test or ANOVA test for those with 3 or more categories
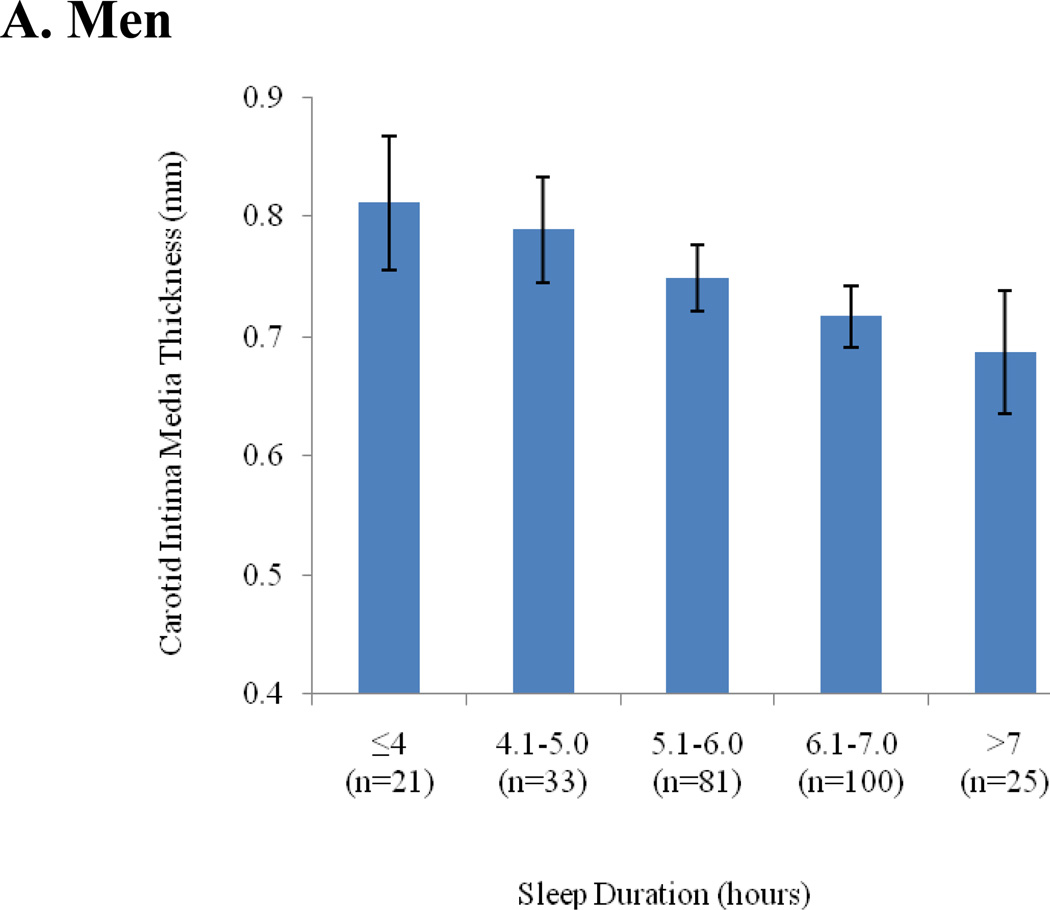
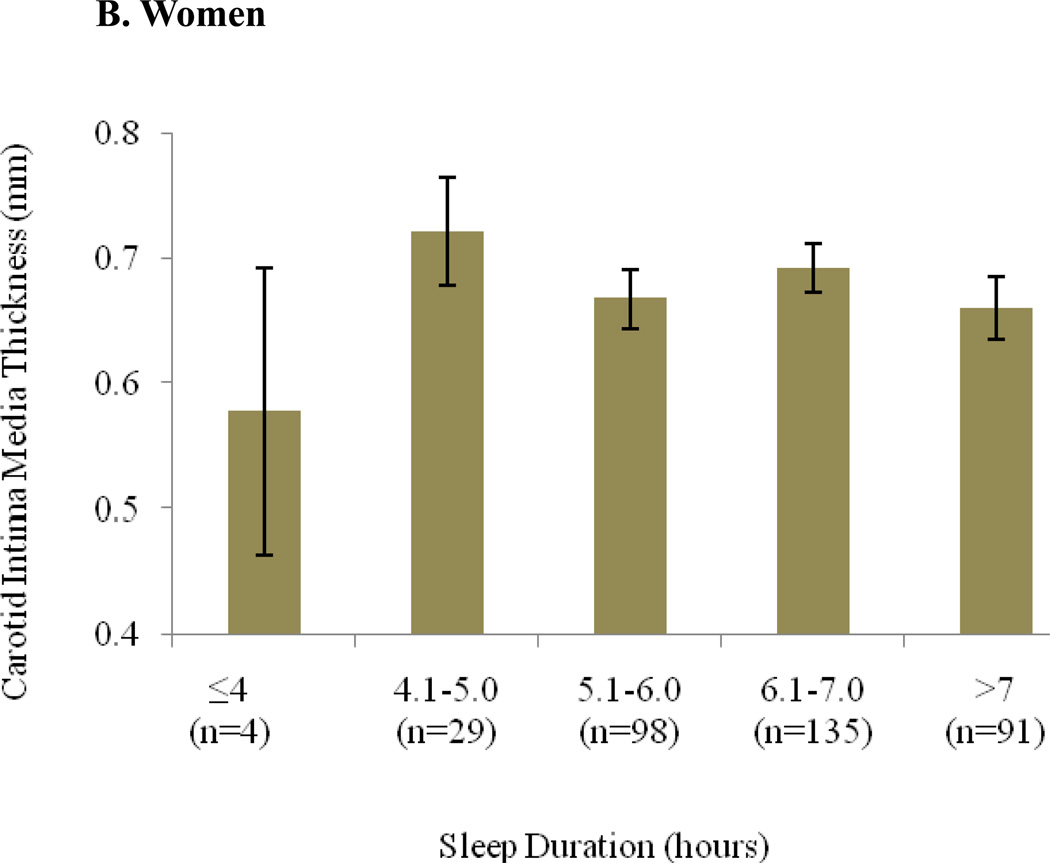
In sex-stratified regression analyses adjusted for age and race/ethnicity, sleep duration was significantly associated with CIMT (mean of 20 measurement sites) among men (β=-0.028 mm CIMT per 1 hour sleep duration; 95% CI -0.044,-0.013; p<0.001), but not among women (β=-0.005; 95% CI -0.019,-0.009; p=0.49) (TABLE 3, FIGURE 1). After further adjustment for additional covariates, including age, race, smoking, education, BMI, depression, systolic blood pressure, LDL cholesterol, HDL cholesterol, and diabetes, the association remained significant among men (β=-0.026; 95% CI -0.047, -0.005; p=0.02) (TABLE 3).
Table 3.
Linear Regression for Sleep Duration on Carotid Intima-Media Thickness (mm) -Differences by sex
| Male (N=260) |
Female (N=357) |
|||||
|---|---|---|---|---|---|---|
| β | 95% CI | P- value |
β | 95% CI | P-value | |
| Sleep time (hrs) adjusted for age and race | −0.028 | −0.044,– 0.013 |
<0.01 | −0.005 | −0.019, 0.009 | 0.49 |
| Sleep time (hrs) adjusted for age, race, CHD risk markers* | −0.026 | −0.047,– 0.005 |
0.02 | −0.001 | −0.020, 0.022 | 0.91 |
Smoking, education, depression, BMI, systolic blood pressure, LDL cholesterol, HDL cholesterol, diabetes
Figure 1.
Objectively assessed sleep duration and carotid CIMT adjusted for age and race - presented by sex (includes 95% confidence intervals)
In a subanalysis we assessed the mean of the maximum CIMT for 20 measurements, which was consistent with the findings for the mean of the mean CIMT for 20 measurements. In the full models, adjusted for age, race/ethnicity, smoking, education, depression, obesity, systolic blood pressure, HDL cholesterol, LDL cholesterol, and diabetes status, the association between actigraphically assessed sleep duration and maximum CIMT was significant among men (β=-0.030, 95% CI -0.005, -0.014, p=0.02), but was not significant among women (β=-0.005, 95% CI -0.020, 0.030, p=0.69).
Site-specific CIMT locations were also evaluated as the outcome in linear regression analyses, and these segments included the bulb, the CCA, and the ICA. Findings among men suggested that the association of sleep duration with CIMT were primarily driven by associations with thickening of the bulb and not the CCA or ICA. Sleep duration was a strong and significant predictor of thickness of the bulb among men in models adjusted for age and race (β=-0.06, 95% CI -0.094,-0.025, p<0.01) as well the models adjusted for demographics and CVD risk factors (β=-0.07, 95% CI -0.125,-0.023, p<0.01). Adjusted models were not significant for the ICA or the CCA among men, or the ICA, CCA or bulb among women. (See supplement)
DISCUSSION
This study provides evidence that shorter objectively assessed sleep duration is associated with increased CIMT in men but not women after adjusting for demographics and CVD risk factors. A significant linear association was present such that among men, each additional hour of sleep per night was associated with a reduced level (0.026 mm) in CIMT (95% CI -0.047, -0.005, p-value=0.02) in fully adjusted models. Although there were few individuals with more than 8 hours of measured sleep (N=6), we did not observe a U-shaped association among either sex as has been found in other studies.
To the best of our knowledge, this is the first study addressing the association between sleep duration and CIMT using objective sleep measures rather than self-reported sleep. One study investigated the association between self-reported sleep duration and CIMT and found a strong J-shaped association among a population-based sample of 2437 individuals from the Study of Health in Pomerania (SHIP) cohort after adjusting for sex and age.4 A key limitation of the SHIP study was the self-reported sleep measure, especially given that other studies have suggested that self-reported sleep time is weakly correlated with that measured from polysomnography (r=0.18, p<0.001).5 Our findings provide novel evidence of this association using an objective assessment of sleep duration and CIMT, but suggest an association among men only.
CIMT serves as a reasonable surrogate measure of subclinical CVD. A recent meta-analysis by Lorenz et al. among 37,197 subjects suggested that for a CIMT difference of 0.10 mm, the future adjusted relative risk of MI increased by 15% (RR=1.15; 95% CI, 1.12, 1.17); and the adjusted relative risk of stroke increased by 18% (RR=1.18; 95% CI, 1.16, 1.21).15 In our study, a difference of 0.13 mm was observed among men in the lowest compared to the highest sleep category (4 hours vs. 7–8 hours).
The observed differences in segment-specific CIMT associations may be due to potential differences in underlying mechanisms relating to atherosclerosis and hypertension. Our findings suggested that the carotid bulb demonstrated significant independent associations with sleep duration, but the CCA and ICA alone were not significantly associated. Studies addressing this pathophysiology have indicated differences in CIMT segments, including that the CCA wall tends to have a higher prevalence of foam cells, but that the bifurcation tends to contain more complex plaques.22 Previous findings have also suggested that the CCA is most strongly associated with blood pressure and hypertension compared with other segments, and that the bulb and ICA tend to be associated with cholesterol and the atherosclerotic burden, as well as diabetes.21 Our findings on segment specific associations may provide some additional evidence regarding potential biologic pathways and suggest that sleep restriction may be less correlated with changes in the CCA, and may have more of an effect on mechanisms involving the carotid bulb.
A number of considerations must be addressed regarding the observed sex differences. One concern is that differences in cardiovascular physiology and pathology exist by sex, and men experience age-related atherosclerotic disease progression at younger ages than women.8, 23 Given that this is a middle-aged population, we may be capturing an association among men and not women due to the men’s elevated disease progression, and similar associations may perhaps be observed among women in this cohort at older ages. In addition, it could be argued that the findings may be due to an increased prevalence of sleep apnea, which tends to be more common among men, and has demonstrated to be causally linked to cardiovascular outcomes.24–26 A recent study from the Sleep Heart Health Study cohort, however, suggested that there was no meaningful association between sleep apnea and CIMT after controlling for cardiovascular risk factors.27 In a subanalysis our assessment of sleep apnea risk in this sample suggested no association between the apnea risk score, snoring or fragmentation and CIMT (see supplement). Furthermore, previous findings from the Northern Manhattan Study also indicated that snoring was not a significant predictor of CIMT (p=0.986) in multivariate linear regression analysis among a diverse cohort of men and women (N=1605).28
This study has a number of notable limitations. Because the study was limited to a cross-sectional design, it allows for limited understanding regarding causal associations. It is unclear how CIMT thickness could cause shorter sleep, but both may be due to a third factor or factors. When assessing the primary exposure, although sleep duration was assessed objectively using wrist actigraphy monitors, the data does not provide insight regarding sleep architecture, sleep disordered breathing or changes in blood oxygenation saturation. However, this objective assessment provides clear advantages over self-reported sleep, and alternative measures of apnea risk and fragmentation were considered. In addition, previous studies have demonstrated that actigraphy is correlated with polysomnography for total sleep time (r=0.88–0.90) among healthy adults, and is stable within this cohort from year to year.18, 20, 29, 30
CONCLUSIONS
In summary, our study found evidence of an association between decreased sleep duration and CIMT in men but not in women. It is important that future studies address this association prospectively to investigate whether these associations are causally related. In addition, it would be beneficial for future studies to have an objective measure of sleep-disordered breathing from an overnight polysomnography. Additional research is also needed to investigate the observed sex differences, and to strengthen the current understanding of biological mechanisms underlying the association between short sleep duration and subclinical CVD.
Supplementary Material
Acknowledgements
We are grateful for the contributions from the CARDIA study investigators and participants.
Funding Sources: The Coronary Artery Risk Development in Young Adults (CARDIA) study is supported by US Public Health Service contracts NO1-HC-48047, NO1-HC-48048, NO1-HC-48049, NO1-HC-48050, and NO1-HC-95095 from the National Heart, Lung, and Blood Institute. The Young Adult Longitudinal Trends in Antioxidants (YALTA) Ancillary Study is supported by R01HL053560 and the CARDIA Sleep and Weight Gain Ancillary Study is supported by P01AG011412.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: MRS none, DSL none, KL none, KLK none, KM none, CDL none, EBL none CBE none.
REFERENCES
- 1.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur Heart J. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 2.Gallicchio L, Kalesan B. Sleep duration and mortality: A systematic review and meta-analysis. J Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolff B, Volzke H, Schwahn C, Robinson D, Kessler C, John U. Relation of self-reported sleep duration with carotid intima-media thickness in a general population sample. Atherosclerosis. 2008;196:727–732. doi: 10.1016/j.atherosclerosis.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 5.Silva GE, Goodwin JL, Sherrill DL, Arnold JL, Bootzin RR, Smith T, et al. Relationship between reported and measured sleep times: The sleep heart health study (shhs) Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2007;3:622–630. [PMC free article] [PubMed] [Google Scholar]
- 6.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: How similar are they? Intra-individual daily and yearly variability in actigraphically recorded sleep measures: The cardia study. Epidemiology. 2008;19:838–845. [Google Scholar]
- 7.Krishnan V, Collop NA. Gender differences in sleep disorders. Current opinion in pulmonary medicine. 2006;12:383–389. doi: 10.1097/01.mcp.0000245705.69440.6a. [DOI] [PubMed] [Google Scholar]
- 8.Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, et al. Insights from the nhlbi-sponsored women's ischemia syndrome evaluation (wise) study: Part ii: Gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. Journal of the American College of Cardiology. 2006;47:S21–S29. doi: 10.1016/j.jacc.2004.12.084. [DOI] [PubMed] [Google Scholar]
- 9.Hall MH, Muldoon MF, Jennings JR, Buysse DJ, Flory JD, Manuck SB. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep. 2008;31:635–643. doi: 10.1093/sleep/31.5.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Calhoun DA, Harding SM. Sleep and hypertension. Chest. 138:434–443. doi: 10.1378/chest.09-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS. Short sleep duration and incident coronary artery calcification. JAMA. 2008;300:2859–2866. doi: 10.1001/jama.2008.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: The rotterdam study. Circulation. 1997;96:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 13.Fathi R, Haluska B, Isbel N, Short L, Marwick TH. The relative importance of vascular structure and function in predicting cardiovascular events. Journal of the American College of Cardiology. 2004;43:616–623. doi: 10.1016/j.jacc.2003.09.042. [DOI] [PubMed] [Google Scholar]
- 14.O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular health study collaborative research group. The New England journal of medicine. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 15.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: A systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 16.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, et al. Cardia: Study design, recruitment, and some characteristics of the examined subjects. Journal of clinical epidemiology. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 17.Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: The cardia study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 18.Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Intra-individual daily and yearly variability in actigraphically recorded sleep measures: The cardia study. Sleep. 2007;30:793–796. doi: 10.1093/sleep/30.6.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jean-Louis G, von Gizycki H, Zizi F, Spielman A, Hauri P, Taub H. The actigraph data analysis software: Ii. A novel approach to scoring and interpreting sleep-wake activity. Perceptual and motor skills. 1997;85:219–226. doi: 10.2466/pms.1997.85.1.219. [DOI] [PubMed] [Google Scholar]
- 20.Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–392. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- 21.Polak JF, Person SD, Wei GS, Godreau A, Jacobs DR, Jr, Harrington A, et al. Segment-specific associations of carotid intima-media thickness with cardiovascular risk factors: The coronary artery risk development in young adults (cardia) study. Stroke. 41:9–15. doi: 10.1161/STROKEAHA.109.566596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dalager S, Paaske WP, Kristensen IB, Laurberg JM, Falk E. Artery-related differences in atherosclerosis expression: Implications for atherogenesis and dynamics in intima-media thickness. Stroke. 2007;38:2698–2705. doi: 10.1161/STROKEAHA.107.486480. [DOI] [PubMed] [Google Scholar]
- 23.Orshal JM, Khalil RA. Gender, sex hormones, and vascular tone. Am J Physiol Regul Integr Comp Physiol. 2004;286:R233–R249. doi: 10.1152/ajpregu.00338.2003. [DOI] [PubMed] [Google Scholar]
- 24.Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, et al. Sleep apnea and cardiovascular disease: An american heart association/american college of cardiology foundation scientific statement from the american heart association council for high blood pressure research professional education committee, council on clinical cardiology, stroke council, and council on cardiovascular nursing. In collaboration with the national heart, lung, and blood institute national center on sleep disorders research (national institutes of health) Circulation. 2008;118:1080–1111. doi: 10.1161/CIRCULATIONAHA.107.189375. [DOI] [PubMed] [Google Scholar]
- 25.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009;373:82–93. doi: 10.1016/S0140-6736(08)61622-0. [DOI] [PubMed] [Google Scholar]
- 26.Parish JM, Somers VK. Obstructive sleep apnea and cardiovascular disease. Mayo Clin Proc. 2004;79:1036–1046. doi: 10.4065/79.8.1036. [DOI] [PubMed] [Google Scholar]
- 27.Wattanakit K, Boland L, Punjabi NM, Shahar E. Relation of sleep-disordered breathing to carotid plaque and intima-media thickness. Atherosclerosis. 2008;197:125–131. doi: 10.1016/j.atherosclerosis.2007.02.029. [DOI] [PubMed] [Google Scholar]
- 28.Ramos-Sepulveda A, Wohlgemuth W, Gardener H, Lorenzo D, Dib S, Wallace DM, et al. Snoring and insomnia are not associated with subclinical atherosclerosis in the northern manhattan study. International journal of stroke : official journal of the International Stroke Society. 2010;5:264–268. doi: 10.1111/j.1747-4949.2010.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification from wrist activity. Sleep. 1992;15:461–469. doi: 10.1093/sleep/15.5.461. [DOI] [PubMed] [Google Scholar]
- 30.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep. 1994;17:201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.